Abstract
Study design:
Mixed-methods study using comprehensive survey and semi-structured interviews.
Objectives:
Compare the experiences of sexual education during rehabilitation for people with non-traumatic spinal cord dysfunction (SCDys) and traumatic spinal cord injury (SCI), determine preferences for the delivery of this information and provide recommendations for spinal rehabilitation professionals.
Setting:
Community, Australia.
Methods:
Adults completed survey (traumatic SCI n=115; SCDys=39) or were interviewed (SCDys: n=21). Survey included questions regarding sexual education during rehabilitation, participant satisfaction with this and preferred modes for receiving such information. These themes were also explored during interviews.
Results:
No difference between SCI and SCDys regarding satisfaction or preferred modes of presentation (all P>0.05). People with SCDys were less likely to report receiving sexuality education during rehabilitation (SCDys n=11, 30%; SCI n=61, 53%; P=0.03). Interviews suggested that this may be gendered, as only two women recalled receiving sexual education, whereas men often received this as part of continence management. Overall, only 18% were satisfied or very satisfied with sexual education and information received, and 36% were dissatisfied or very dissatisfied. Preferred modes for receiving sexuality information included sexuality counsellor (n=97), recommended internet sites (n=77), peer support workers (n=76), staff discussion (n=67), written information (n=67) and DVD (n=58). These preferences were confirmed during interviews, although women expressed a strong preference for written information sheets.
Conclusion:
There was very low satisfaction with sexuality education during rehabilitation. Our findings highlight the scope and directions for improving the sexual education and information given to people with both SCDys and SCI during rehabilitation.
Similar content being viewed by others
Introduction
Spinal cord damage from any cause, whether traumatic or non-traumatic, can result in sexuality changes that are commonly complex and confounding.1, 2 Sexual functioning is acknowledged as a key domain of general health that is important for well being and quality of life3 but is typically inadequately addressed in people with disability.4, 5
For people with spinal cord damage, it is a major priority that changes in sexuality are adequately addressed as part of their rehabilitation.6 Most studies of sexuality in people with spinal cord damage have focused on people with traumatic spinal cord injury (SCI). There is no internationally accepted term for the group of conditions that can cause non-traumatic spinal cord damage;7 hence, the term spinal cord dysfunction (SCDys) will be used to describe these conditions throughout this paper. Although some studies of sexuality have included people with non-traumatic SCDys,8 until recently no studies had been published that report specifically on the sexual changes in people with SCDys.9, 10 The demographic characteristics and functional outcomes for people with SCDys are different from SCI.11, 12 SCDys is more common in people of older age who are more likely to have chronic health issues that potentially influence sexuality generally13, 14, as well as further impact on sexual functioning following spinal cord damage. In addition, in many developed countries, the incidence of SCDys is higher than SCI,15, 16 and this difference is expected to increase markedly in the coming decades with population ageing.15 Therefore, studies that focus on sexuality issues in people with SCDys are very important.
It is well recognised that health-care professionals in the rehabilitation team have a key role in the education of the patient with spinal cord damage about possible changes to sexuality and strategies to adjust to these changes.17, 18, 19, 20 Some studies have examined patient satisfaction regarding the content and delivery of sexuality education within spinal rehabilitation services.17, 18, 19, 21 There are no published studies, however, regarding the experience of sexual education during rehabilitation for people with SCDys, their satisfaction with these services or what people with SCDys would like to have received during rehabilitation. This is important to address considering the older age profile and increased incidence of SCDys compared with SCI.
The aim of this project was to conduct a mixed-methods study of people with SCDys regarding their experience and satisfaction with sexual education during rehabilitation and determine their preferences for receiving this information. The primary objective was to provide recommendations for spinal rehabilitation professionals regarding the sexual education needs and preferences of people with SCDys. A secondary objective was to compare the survey responses from people with SCDys to those with SCI.
Methods
This was a mixed-methods study, with quantitative and qualitative components conducted concurrently. Eligible participants could participate in both components if they desired.
Study design and setting
A comprehensive survey was conducted between 1 August 2013 and 30 June 2014 of Australian adults (n=154) with spinal cord damage living in the community.9
To explore the complex and subjective psychosocial experience of sexuality for people with SCDys, a qualitative research design was also used. This enabled a deeper understanding of how people perceived and gave meaning to their experiences.22 Following an introductory telephone conversation (10–15 min) in which participants were given detailed information about this component the study, face-to-face semi-structured interviews were arranged and conducted between September 2013 and September 2014 by researchers trained in qualitative research methods.22 The participants were 11 women10 and 10 men with SCDys who lived within 200 km of Melbourne. Face-to-face interviews were selected as the preferred data-collection strategy in order to increase rapport, to allow for the full development of participants’ accounts, an important component of exploratory research, and to enable an immediate response to possible participant distress.23
Participants
Participants with SCDys were recruited from attendees at a spinal rehabilitation unit (SRU) review clinic by mailing those who had attended the clinic between 2010 and 2013. A notice was also placed in the clinic waiting area between 1 August 2013 and 30 June 2014. A number of State-based organisations that support people with spinal cord damage in the community (see Acknowledgements) also promoted the study through their websites, newsletters, emails and social media.9
The survey included people with both traumatic SCI and non-traumatic SCDys. The rationale for this was to compare the survey results between the different aetiologies of spinal cord damage. Only people with SCDys were eligible for the qualitative interview. This was justified by the lack of qualitative studies on this topic involving people with SCDys.
The following people were excluded from both components of this project: those residing in a nursing home or hospitalised (because these situations adversely impact on establishing and maintaining a sexual relationship and sexual functioning), those having a congenital cause of SCDys or multiple sclerosis (as cortical impairment can be a confounding influence on aspects of sexuality) and those with clinically significant psychiatric conditions or cognitive impairment, or insufficient English to complete the questionnaires or participate in an interview.
Outcome variables
The survey covered numerous patient-reported outcome measures (copy available upon request)9 that included clinical and demographic information, as well as questions regarding education participants received during their initial inpatient admission and the consequences of spinal cord damage for their sexuality. There were questions about whether participants recalled receiving education regarding sexuality during their inpatient rehabilitation, who gave this education, how satisfied they were with the sexual education they received and what would have been their preferred mode(s) for receiving sexuality information and education. Participants could indicate one or more of the modes that they would have preferred.
Individual face-to-face semi-structured interviews were guided by a series of questions exploring participants’ experiences in rehabilitation relating to sexuality and sexuality education during rehabilitation (copy available on request). Additional prompting questions were used in response to participants’ answers. Interviews lasted 1–1.5 h and were conducted in participants’ homes or other preferred meeting place. Interviews were digitally recorded and subsequently transcribed verbatim.
Sample size
As this was an exploratory study, there was no predetermined sample size for the survey.
Qualitative sample size was determined by the concept of theoretical saturation, which refers to the point at which no significant new information arises from subsequent interviews.22 Research suggests that this occurs at around 12 interviews, but preliminary saturation (when most themes are fully articulated) can occur after 6 interviews.24
Quantitative statistical analysis
Continuous variables not normally distributed were summarised using the median and interquartile range. The Wilcoxon rank-sum (Mann–Whitney) test was used to calculate differences in the population distribution between continuous variables. Categorical variables were compared using Pearson’s chi-square test, with the Fisher exact correction used when small numbers in subgroups indicated that this was appropriate.
P-values of less than 0.05 were deemed statistically significant. Stata 12 for Windows (StataCorp, College Station, TX, USA) was used for statistical analysis.
Qualitative data analysis
Thematic analysis was conducted to identify the prominent themes within the interview data using a six-stage thematic analysis.25 Initial familiarisation with data was achieved through the process of verbatim transcription and repeated readings with the key research questions in mind (stage 1). Codes (basic components of the raw data) were then formed and organised (stage 2) and categorised into potential overarching themes and sub-themes using a largely inductive analysis; deductive themes were also identified based on the literature (stage 3). A theme was identified by noting the frequency with which it occurred and/or the extent to which it related to the research questions. The themes were then refined, and data extracts reviewed to ensure that they adequately reflected the relevant themes (stage 4). The final two stages involved defining and naming each theme in the context of the overall data (stage 5) and reporting the findings (stage 6). All coding was undertaken by two of the authors trained in qualitative research (MS and CR), which was cross-checked by another member of the research team (NW) to ensure the fit and applicability of the themes. In the few instances where there was disagreement, discussion ensued and themes were either redefined or amended. To maintain anonymity, each participant was provided with a pseudonym for this manuscript.
Triangulation is a multi-method approach that was employed to ensure rigour and validity of the data and analysis and to facilitate an understanding of the complexity of the topic under study.22 In this study, triangulation occurred in several ways: (1) use of a mixed-methods study design; (2) interviews with multiple individuals with differing periods of time since onset of SCDys; and (3) the use of multiple researchers in data collection, analysis and interpretation.
NVivo 10 for windows (QSR International, Doncaster, Victoria, Australia) was used for qualitative data management.
Ethics
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Survey
There were 154 people with spinal cord damage who completed the survey, but two did not answer the questions regarding education received during inpatient rehabilitation about the consequences of spinal cord damage for sexuality. Those with SCI (n=115, 76%) were more likely to be male (72%), younger (median age 46, interquartile range 32–55) and have tetraplegia (48%) compared with those with SCDys (n=37, 24%; male=49%, P=0.008; median age 58, interquartile range 51–68, P=0.0001; tetraplegia 21%, P=0.003). The median time since onset of spinal cord damage was 11 years (interquartile range 4–20). Most (95%) respondents were exclusively heterosexual, and 5% were gay, lesbian or bisexual. Other demographic and clinical results regarding these participants have been reported previously.9
Participants’ responses regarding the education they reported receiving during their initial inpatient rehabilitation admission in relation to the consequences of spinal cord damage for sexuality, their satisfaction with this education and desire for more information are shown in Table 1. Gender (P>0.1) or relationship status (married or in a de facto relationship) at the time of spinal cord damage (P>0.1) did not influence whether participants received sexuality education during rehabilitation admission. Older participants, however, were less likely to report that they received sexuality education during rehabilitation (P=0.007).
Forty-four participants reported that they received sexuality education information from staff and 41 received written information. Of these, 15 received both education from staff and written information. There was no relationship between the aetiology of spinal cord damage and the source of sexuality information (from staff P=0.09; written P>0.1). Participants reported 16 other sources of information, including group discussions (n=3), movies or films (n=3), seminars (n=2), internet sources (n=2), books (n=1) and others not specified (n=5).
The preferred modes for receiving sexuality information during rehabilitation reported by participants were sexuality counsellor (n=97), recommended internet sites (n=77), peer support workers (n=76), written information (n=68), staff discussion (n=67) and DVD (n=58). There were no differences between the aetiologies of spinal cord damage regarding preferences for receiving the different types of information (all P-values >0.1). Other sources nominated were email (n=1) and other not specified (n=4). Two participants desired information on sexual experimentation, two requested that information should be provided for partners and two indicated that advice should have been provided on the sexuality support services available following discharge. Another very pertinent comment from the survey was that ‘each listed (option) may be helpful at certain times and depending on the person’.
Qualitative data
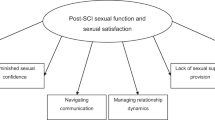
Information provided during interviews highlighted the complexity of sexual adjustment after SCDys, influenced by the interaction of physical, psychological and social factors. In particular, psychosocial factors, especially those related to gender roles, were seen as either inhibiting or facilitating sexual adjustment. The interview participants were exclusively heterosexual.
Sexual rehabilitation services: identifying needs
Participants overwhelmingly reported gaps in formal support provided by clinicians in relation to sexuality. These gaps were patterned by gender: only 2 of the 12 women interviewed recalled receiving any information about sexual pleasure or sexuality during rehabilitation:
It has been nil… At the beginning, I was so confused … that I might have had some that didn’t sink in. (Alice)
Both female participants who received such information reported dissatisfaction:
When I spoke about sex, the doctor wouldn’t even answer me. Whenever I brought it up, it was if I hadn’t said anything. (Iris)
In contrast, although male participants were given some information, they reported a need for more detailed, personalised information. All of the men interviewed could recall engaging in some level of discussion about sexuality – most often in terms of erectile function – as part of broader discussions about bladder and bowel continence and management. This typically gave little consideration to the bodily contingencies that could arise. Anthony, for example, experienced ongoing difficulties with bladder infection related to catheterisation and so received information on what he could and could not do sexually. However, this information did not extend to include the potential problems that could arise; as a result, his experience of bleeding when he did attempt intercourse left him unwilling to persist in his efforts:
My thinking about the sexual part is still there… But I’m not doing anything anymore because once, a couple of times, I tried to [have sex]… It scared me a little bit because, [although] you get sort of an erection, you start bleeding… so I stopped… [I] was thinking maybe… something happened in me, something has closed up… From then on, I forgot about [sexuality].
Ron, too, felt that the challenges he experienced could have been foreshadowed or, at the very least, alleviated by better information and support from the health professionals involved in his care:
I would have liked to know more about [my sexuality]… Because it's a potential part of where I'm at and because I have had some difficulties in that regard, it would have been good to know more about it.
These examples highlight a lack of information given by health professionals about how to cope with the bodily changes associated with SCDys and how this contributed to participants’ difficulty communicating with others, including their intimate partners, about sexuality.
These differences in modes of information delivery led several (mostly) female participants to perceive bias in the lack of sexual rehabilitation services received. They signified that sexual rehabilitation services should be introduced and accessible to all irrespective of gender, age or perceived partnership. Sexual rehabilitation services should be uniformly offered to all patients, broached by rehabilitation staff, and not dependent on the judgment of a medical person or reliant on people to request it:
I think it needs to be initiated [by health professionals]… because they do give you awareness of all sorts of other different things when you’re there, about how you might be feeling bad about yourself, about looking after yourself… and what you might find difficult. (Rhonda)
For Rhonda, sexual education was an integral part of a holistic rehabilitation service. The majority of participants concurred, desiring sexual rehabilitation services to be presented in a similar way to other regular rehabilitation services.
Timing and extent of sexual rehabilitation services
The general view was that sexuality rehabilitation service should be introduced in rehabilitation or before this if surgery was anticipated. Although most participants experienced an initial period of sexual disinterest (latency) following the onset of SCDys, they did not believe that this was a barrier to sexual rehabilitation services. Indeed, most participants felt that they would have been better prepared for their changes in sexuality if they had received education about potential changes early in their rehabilitation process, before they re-engaged in sexual activities (which encompassed a wide range of practices, from massage to masturbation to coitus). For example, although he recognised that SCDys impacted people differently depending on the completeness and the level of injury, Daniel advocated for openness from health professionals in sexuality from the beginning, as he felt it prepared them better for different outcomes:
You've got to incorporate sexual education to [apply to different levels and completeness]. Each person's different… Tell people, this may work or it may not work. You may have feeling, or may not. Don't lie to people. Leave it so it's open, because in my case I was [mis]led.
Daniel’s experience following initial interactions with health professionals left him feeling cynical and without assistance when he experienced difficulties in maintaining an erection and being unable to achieve orgasm. These comments highlight the value of repeated and ongoing efforts by rehabilitation professionals to engage people with SCDys in conversations to this end.
Both male and female participants felt that their surgeon had an important role in raising the issue of potential changes in sexuality:
My thoughts are that the first point of call should be the surgeons, who actually perform the operations. They should be the first people who should advise me… in understanding it, being able to explain it, and then moving us onto people like physio[therapist]s and psychologists. (Ron)
Inpatient rehabilitation was seen to offer an important yet often underutilised opportunity for the delivery of sexual rehabilitation services. This was especially salient for women, who perceived that the failure to be offered information reflected discrimination against them because of being older, female or apparently single:
I’m assuming the reason that it was not mentioned to me was either that I didn’t have a regular male visitor... or my age. If you were young and you had a lovely partner who came to visit and young children, I’m sure the doctor looking after you would volunteer that. (Mary)
Concerns about possible discrimination also influenced many female participants to not request information on sexual adjustment during rehabilitation. Fears of embarrassment restricted three women from asking for sexual information, although they wanted it.
Because I’m older, I think ‘What will they think?’ (Josie).
Not having a current partner was also described as a reason for not asking for information while in rehabilitation, as Beryl described, ‘what’s the point. I haven’t got anyone.’ Male participants received sexual rehabilitation services in a more routine way (as a ‘programme’), although there were contrasting views on the role of such services during inpatient rehabilitation. Some participants valued inpatient sexual rehabilitation:
The physiotherapists and psychologists have a very useful role in [rehabilitation], overcoming it and dealing with [changes in sexuality]. (Ron)
In contrast, other participants felt that the timing was challenging because of the number of competing priorities during rehabilitation:
I went through rehabilitation, which basically covers most areas [and] we do programs which involve sexuality... [but] I don’t think there’s enough on that … I would like to have discussed [sexuality] a bit more at an earlier stage... When you do [rehabilitation], you’re in the middle of trying to cope with being in a wheelchair, trying to cope with a life in the wheelchair. You’re not really thinking sexuality at that stage. (Nathan)
Post-discharge sexuality services
Although many participants felt that there was a place for inpatient sexual rehabilitation services, a widespread need for ongoing access to sexual rehabilitation services after discharge as sexual interest was regained and problems were experienced was indicated: ‘[It] should be an ongoing thing’ (Alec). Alice reflected that regaining sexuality was part of the recovery process following SCDys: ‘Now that I am feeling more normal, more in control of my life… I want to be able to do what I can to be normal’. Nathan explained this further: ‘Once you get out of hospital, that’s where the support should be. Not [just] when you’re in the hospital.’
Ongoing support was also required when new partners were found, as Mary explained.
I haven‘t met anybody since I’ve have my urethral catheter and my bowel problem and I definitely have to get some counselling and advice [but] I don’t know who I would go to.
In the case of partnerships developing after SCDys, ongoing sexual rehabilitation services would allow both partners to have realistic expectations around sexual pleasure.
The problem is you have to take [the condom drainage] off to be intimate and then you don't know if you're gonna pass urine or get the required result. It became an issue for my wife, so that started diminishing the intimacy side of things.
To this end, some participants suggested a need for both members of a couple to receive support from sexual rehabilitation services, in order to ‘not only tell them… this is what’s happening to your partner but affirming their emotions as well’ (Alice).
Modes of delivery of sexual rehabilitation services
All participants believed that sexual rehabilitation services should be provided by appropriately qualified sexual health professionals who have specific knowledge in sexuality and an appropriate attitude so that participants could speak openly: ‘Someone you could ask anything of and they would be totally matter of fact and not make you feel embarrassed’ (Alice). Yet, the precise strategy for this information delivery varied by gender, with male participants preferring more active ways of engagement with the material.
In particular, they expressed a preference for audio-visual material, such as instructional videos, which would allow them to diversify their sexual repertoires and become aware of non-hegemonic expressions of sexuality:
I think it would be good if someone could make a DVD… For the partners, it would say ‘this is how you could approach your partner now who has erectile dysfunction and can't ejaculate quickly.’ And [it should contain] ideas on keeping the spice in the relationship, rather than it falling apart because of that issue… I think it's just suggesting to people rather than having to discuss [that] there's still a way [to experience pleasure] if people are willing to find a solution. (James)
Indeed, James described how he had sought out information on YouTube in order to develop a new sexual repertoire; this was not only about being sexually active but was also an important aspect of maintaining the relationship with his partner.
Several other men discussed their desire for peer support group sessions, where they could discuss their experiences with others who had encountered, and potentially developed strategies to overcome, the challenges they faced:
You could place them in a group therapy session, but it would have to be a little bit jocular, so that every person in the group session could bounce ideas off each other, and the person leading it could ask things like ‘well… how many of you have ever tried oral sex?’ (Eddie)
In contrast, women described different preferences around finding solutions to enhance their sexual pleasure. In addition to a sexual counsellor, there was a strong preference for printed material, as this was seen as egalitarian and presenting information in a thought-provoking, non-confrontational way: ‘I think that written information would be non-threatening in the first instance and then maybe … someone to talk to further’ (Alice). Several suggested that a resource list of whom to contact for different types of information would be valuable.
Several women indicated that the type of information they would most value was broad progression-related information and commonly experienced sexual challenges around restricted mobility, lack of genital sensation and continence management: ‘I would have liked to have the opportunity to find out what other people have experienced, am I the only one who feels like this?’ (Jeanette)
There was little support among the women for online resources, as most did not have internet access and those who did said that they did not find great value in it. In addition, limited value was seen in peer support groups, with the majority expressing concerns about the deeply personal nature of sexuality and the possibility of being judged.
Discussion
There were no differences between SCI and SCDys regarding satisfaction or preferred modes of presentation of sexuality education; however, people with SCDys were less likely to report receiving sexuality education during rehabilitation. Overall, a low proportion of survey respondents reported receiving education during inpatient rehabilitation about the consequences of spinal cord damage for their sexuality. There was very low satisfaction among all people with spinal cord damage regarding the education that was received. Most people with spinal cord damage would have liked more sexuality-related education during inpatient rehabilitation. This information was reflected during qualitative interviews, which also found a perception among some people with SCDys of a staff bias against providing sexuality information to females, those without a partner and older-aged people. The survey findings confirmed a bias in the provision of this information to younger people over those of an older age. A variety of modalities for presenting education about the consequences of spinal cord damage for sexuality during inpatient rehabilitation need to be available, and these options also need to be available after discharge into the community. These findings highlight the importance of taking gender into account when planning the delivery of sexual rehabilitation services.
The findings of our study are generally consistent with those of previous studies that focused on people with traumatic SCI. In particular, the low rate of receiving education during inpatient rehabilitation about the consequences of spinal cord damage for sexuality and the low satisfaction with the education provided appears to have progressed little in the past two decades.17 That these low levels of education and satisfaction are no better in our study is extremely disappointing. In keeping with previous studies, a multitude of modalities are recommended for addressing the education needs of people with spinal cord damage regarding the consequences of this damage for their sexuality.17, 19, 20
Numerous barriers to the provision of sexuality rehabilitation to patients have been reported.18, 19, 20, 26, 27 These include staff discomfort, limited staff knowledge, perception of expertise elsewhere, readiness on the part of the patient for receiving the information and discriminatory or misinformed staff attitudes. The qualitative interview findings from our SCDys patients mirror many of these.
The qualitative findings highlight the importance of taking gender into account when planning the delivery of sexual rehabilitation services. In contrast, the survey results found no influence on whether participants received sexuality education during rehabilitation according to gender or whether they had a partner at the time of spinal cord damage. This may be partly explained by the differences in aetiology between the two samples. However, the perception of interviewees that there was a bias against older participants was corroborated by the survey.
Coalescing the findings of the current study with those of previous studies,3, 9, 17, 18, 19, 20, 21, 28, 29, 30, 31, 32, 33, 34, 35 we make a number of recommendations for rehabilitation professionals regarding the sexual education needs and preferences of people with SCDys in Table 2. We also make the following suggestions regarding the content of sexuality rehabilitation programs for people with spinal cord damage of any aetiology. Topics (in no specific order) should include reproductive biology; birth control, sexuality transmitted infections and safe sex practices; assertiveness training (to assist in dealing with unwanted advances); facilitating communication about changes in sexual function and needs; self-esteem training; relationship goals; information about specific issues related to spinal cord damage such as fertility changes, erection and ejaculation issues for men, lubrication, childbirth and menstruation for women; erogenous zones and options of non-intercourse sexual activity, and practical issues regarding intercourse, including those related to continence, skin care, mobility and transferring issues affecting positioning, and spasticity.
The main strength of this project is that it is the first to comprehensively study people with SCDys regarding the sexuality rehabilitation services they received during inpatient rehabilitation and their preferences for what services they would have liked to receive. Another strength of this project is the use of a mixed-methods methodology, using qualitative face-to-face semi-structured interviews and a quantitative survey, which added to the robustness of the findings and provided a detailed exploration of participants’ experiences. The inclusion of a sample of people with traumatic SCI in the survey provided an important contrast and reinforcement of the results from those with SCDys.
The limitations of this study include the responder bias to surveys, which is reported to be greater in studies of sexuality.36 However, alternative study approaches are not readily available. The lower numbers of females and people with SCDys in the survey also need to be noted. A more detailed discussion of the limitations of the survey has been presented previously.9 Self-report bias may have occurred in the face-to-face interviews; however, alternative data-collection strategies such as audio-assisted computer self-interviews37 were not adopted because of the perceived poor computer literacy of our SCDys sample. During interviews, questions were presented in a range of ways in order to minimise the self-report bias, and multiple modes of triangulation were implemented in order to enhance the credibility of the qualitative analysis.38, 39 Furthermore, interviews possibly reduced bias because of the use of probing questions to clarify understanding.
The study findings highlight key areas of concern for people following SCDys in Australia, which are likely to be generalisable to other Anglo-Western cultures. We are unable to comment on the generalisability to cultures that differ markedly in attitudes to sexuality. All participants who took part in interviews were recruited through a single spinal rehabilitation service and were required to reside within the greater metropolitan area. It is possible that, given rural–urban disparities in health service delivery particularly in terms of disability-specific health care, our findings do not fully reflect the challenges faced by some people following SCDys. Nonetheless, the findings identify key domains for further health service research in this under-served population.
Conclusion
Our findings highlight the considerable scope for improving the sexual education and information given to people with SCDys and SCI during rehabilitation and provide valuable guidance for this. Although perceptions of gender, age and disablement have an important role in how clinicians and consumers understand sexuality following spinal cord damage, these socially learned constructs are amenable to reconstruction. Using insights gained regarding factors facilitating sexual adjustment, such as broadening understanding of sexual norms, effective interventions can be developed for the improvement of sexual rehabilitation services post SCDys. In this way, sexual rehabilitation services can respond to an important opportunity to enhance well being of those with whom they work.
Data archiving
There were no data to deposit.
References
Elliott S. Sexual dysfunction in women with spinal cord injury. In: Lin VW (ed.). Spinal Cord Medicine: Principles and Practice, 2nd edn. Demos Medical Publishing: New York, New York, 2010, p. 429–437.
Elliott S. Sexual dysfunction in men with spinal cord injury. In: Lin VW (ed.). Spinal Cord Medicine: Principles and Practice, 2nd edn. Demos Medical Publishing: New York, New York, 2010, p. 409–428.
World Health Organization. Defining Sexual Health: Report of a Technical Consultation on Sexual Health. Geneva, 2006.
Shakespeare T . Disabled sexuality: toward rights and recognition. Sex Disabil 2000; 18: 159–166.
Mall S, Swartz L . Sexuality, disability and human rights: Strengthening healthcare for disabled people. S Afr Med J 2012; 102: 792–793.
Simpson L, Eng J, Hsieh J, Wolfe D Spinal Cord Injury Rehabilitation Evidence (SCIRE) Research Team. The Health and Life Priorities of Individuals with Spinal Cord Injury: a systematic review. J Neurotrauma 2012; 29: 1548–1555.
New PW, Delafosse V . What to call spinal cord damage not due to trauma? Implications for literature searching. J Spinal Cord Med 2012; 35: 89–95.
Kreuter M, Taft C, Siösteen A, Biering-Sørensen F . Women’s sexual functioning and sex life after spinal cord injury. Spinal Cord 2011; 49: 154–160.
New PW, Currie KE . Development of a comprehensive survey of sexuality issues including a self-report version of the International Spinal Cord Injury sexual function basic data sets. Spinal Cord 2016; 54: 584–591.
Seddon M, Warren N, New PW . “I don’t get a climax any more at all”: pleasure and non-traumatic spinal cord damage. Sexualities 2016 (in press).
New PW . Functional outcomes and disability after nontraumatic spinal cord injury rehabilitation: results from a retrospective study. Arch Phys Med Rehabil 2005; 86: 250–261.
New PW, Simmonds F, Stevermuer T . A population-based study comparing traumatic spinal cord injury and non-traumatic spinal cord injury using a National rehabilitation database. Spinal Cord 2011; 49: 397–403.
McInnes RA . Chronic illness and sexuality. Med J Aust 2003; 179: 263–266.
Schover LR, Jensen SB . Sexuality and Chronic Illness - A Comprehensive Approach. The Guilford Press: New York. 1988.
New PW, Sundararajan V . Incidence of non-traumatic spinal cord injury in Victoria, Australia: a population-based study and literature review. Spinal Cord 2008; 46: 406–411.
Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG et al. The incidence and prevalence of SCI in Canada: a national perspective. Neuroepidemiology 2012; 38: 219–226.
Tepper MS . Sexual education in spinal cord rehabilitation: current trends and recommendations. Sex Disabil 1992; 10: 15–31.
McAlonan S . Improving sexual rehabilitation services: the patient's perspective. Am J Occup Ther 1996; 50: 826–834.
Esmail S, Knox H, Scott H . Sexuality and the Role of the Rehabilitation Professional. Center for International Rehabilitation Research Information and Exchange: Buffalo, NY. 2010, p. 1–18.
Ducharme S. Sexuality and spinal cord injury. In: Stone JH, Blouin M (eds). International Encyclopedia of Rehabilitation. Center for International Research and Exchange: Buffalo, NY, 2010.
Leibowitz RQ . Sexual rehabilitation services after spinal cord injury: what do women want? Sex Disabil 2005; 23: 81–107.
Liamputtong P . Qualitative Research Methods. Oxford University Press: South Melbourne, Victoria, Australia. 2013.
Irvine A, Drew P, Sainsbury R . ‘Am I not answering your questions properly?’ Clarification, adequacy and responsiveness in semi-structured telephone and face-to-face interviews. Qual Res 2013; 13: 87–106.
Guest G, Bunce A, Johnson L . How many interviews are enough? Field Methods 2006; 18: 59–82.
Braun V, Clarke V . Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101.
Tepper M . Providing comprehensive sexual health care in spinal cord injury rehabilitation: implementation and evaluation of a new curriculum for healthcare professionals. Sex Disabil 1997; 15: 131–165.
Herson L, Hart KA, Gordon MJ, Rintala DH . Identifying and overcoming barriers to providing sexuality information in the clinical setting. Rehabil Nurs 1999; 24: 148–151.
Annon JS . Behavioural Treatment of Sexual Problems: Brief Therapy. Harper & Row: Hagerstown, MD. 1976.
Weerakoon P, Stiernborg M . Sexuality education for health care professionals: a critical review of the literature. Annu Rev Sex Res 1996; 7: 181–217.
Fisher TL, Laud PW, Byfield MG, Brown TT, Hayat MJ, Fiedler IG . Sexual health after spinal cord injury: a longitudinal study. Arch Phys Med Rehabil 2002; 83: 1043–1051.
Booth S, Kendall M, Fronek P, Miller D, Geraghty T . Training the interdisciplinary team in sexuality rehabilitation following spinal cord injury: a needs assessment. Sex Disabil 2003; 21: 249–261.
Burch A . Health care providers' knowledge, attitudes, and self-efficacy for working with patients with spinal cord injury who have diverse sexual orientations. Phys Ther 2008; 88: 191–198.
Abramson C, McBride K, Konnyu K, Elliott S . Sexual health outcome measures for individuals with a spinal cord injury: a systematic review. Spinal Cord 2008; 46: 320–324.
Lombardi G, Del Popolo G, Macchiarella A, Mencarini M, Celso M . Sexual rehabilitation in women with spinal cord injury: a critical review of the literature. Spinal Cord 2010; 48: 842–29.
World Health Organization World Report on Disability. Geneva, Switzerland. 2011.
Strassberg DS, Lowe K . Volunteer bias in sexuality research. Arch Sex Behav 1995; 24: 369–382.
Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ . Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sex Transm Infect 2005; 81: 421–425.
Seale C . Quality in qualitative research. Qual Inq 1999; 5: 465–478.
Mays N, Pope C . Qualitative research: rigour and qualitative research. BMJ 1995; 311: 109.
World Health Organization Education and Treatment in Human Sexuality. The Training of Health Professional: Geneva. 1975.
Acknowledgements
The following people with spinal cord damage are thanked for their assistance with the development of the survey: Lynne Panayiotis, Georgina Fiorentino, Mark Hanson, Mike Short and anonymous. Vanessa Hamilton (previously Sexual Health Nurse Consultant, Austin Health, Melbourne, Australia) is thanked for providing helpful comments and suggestions. The following organisations are thanked for their assistance with distribution of the survey: AQA (Victoria), Spinal Injuries Association (Queensland), Spinal Cord Injuries Australia (New South Wales), Paraplegic–Quadriplegic Association of WA, ParaQuad NSW, Paraplegic and Quadriplegic Association of South Australia, Spinal Cord Injury Network (Australia). Dr Daniel E Rohe, Mayo Clinic Rochester, MN, USA is thanked for providing helpful suggestions on an earlier draft of this manuscript. We also thank all the participants who completed the survey or participated in an interview. Some of the information in this manuscript was presented at the Australian and New Zealand Spinal Cord Society 21st Annual Scientific Meeting, 19–21 November 2014, Auckland, New Zealand.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
New, P., Seddon, M., Redpath, C. et al. Recommendations for spinal rehabilitation professionals regarding sexual education needs and preferences of people with spinal cord dysfunction: a mixed-methods study. Spinal Cord 54, 1203–1209 (2016). https://doi.org/10.1038/sc.2016.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.62
This article is cited by
-
A Scoping Review of Literature on Sexual Health and Wellness in Women with Spinal Cord Injury
Sexuality and Disability (2024)
-
“You feel a bit unsexy sometimes”: The psychosocial impact of a spinal cord injury on sexual function and sexual satisfaction
Spinal Cord (2023)
-
The contribution of bio-psycho-social dimensions on sexual satisfaction in people with spinal cord injury and their partners: an explorative study
Spinal Cord Series and Cases (2022)
-
A Survey of Latin American Rehabilitation Professionals on Addressing Sexuality-Related Concerns After Spinal Cord Injury
Sexuality and Disability (2022)
-
Sex, support and society: a journey to reclaiming sexuality for individuals living with paraplegia in Cape Town, South Africa
Spinal Cord (2021)