Abstract
Study design:
Cross-section design.
Objectives:
The development of reliable screen technology for predicting those at risk of depression in the long-term remains a challenge. The objective of this research was to determine factors that classify correctly adults with spinal cord injury (SCI) with depressed mood and to develop a diagnostic algorithm that could be applied for prediction of depressed mood in the long-term.
Setting:
SCI rehabilitation unit, rehabilitation outpatient clinic and Australian community.
Methods:
Participants included 107 adults with SCI. The assessment regimen included demographic and injury variables, negative mood states, pain intensity, health-related quality of life and self-efficacy. Participants were divided into those with ‘normal’ mood versus those with elevated depressed mood. Discriminant function analysis (DFA) was then used to isolate factors that in combination, best classify the presence or absence of depressed mood.
Results:
At the time of assessment, 24 participants (22.4%) had elevated depressed mood. DFA identified six factors that discriminated between those with depressed mood (P<0.01) and those with normal mood, explaining 61% of the variance. Factors consisted of pain intensity, mental health, emotional and social functioning, self-efficacy and fatigue. DFA correctly classified 91.7% (n=22 of 24) of those with depressed mood and 95.2% (n=79 of 83) of those without. Demographic, injury and physical health function variables were not found to discriminate depressed mood.
Conclusion:
Clinical implications of applying a diagnostic algorithm for detecting depression in adults with SCI are discussed. Prospective research is needed to test the predictive efficacy of the algorithm.
Similar content being viewed by others
Introduction
Living with spinal cord injury (SCI) and its functional limitations, participation restriction and complications is associated with increased levels of psychological morbidity such as depression and post-traumatic stress disorder, leading to diminished well-being.1, 2, 3, 4, 5, 6, 7, 8, 9 Secondary conditions like chronic pain and chronic fatigue are also significant problems.10, 11, 12 Factors associated with increased risks of depressed mood in people with SCI include chronic pain, poor self-efficacy, inferior health, alcohol abuse, fewer functional improvements, greater frequency of pressure ulcers, chronic fatigue, elevated anxiety and greater number of days in bed.4, 5, 9, 13 Clearly, depression and its associated complications present a major challenge for many people with SCI.
Research has shown that depressed mood can be reliably assessed using screening instruments like the PHQ-9, though there has been scarce research conducted that has evaluated their ability to predict long-term depression in adults with SCI, despite calls for greater research efforts in the detection of depression in people with SCI.14, 15 Attempts to predict depression in adults with SCI have been limited.3, 4, 5, 9, 16 Factors that have been found to predict depressed mood in the long-term include chronic pain, poor self-efficacy, coping strategies and appraisals, declining health and unsafe use of alcohol.4, 5, 16 However, injury and demographic factors like age at injury, sex and level of injury have not been found to predict depression.5
There is a clinical consensus that early and reliable detection of depressed mood in people with SCI would be beneficial; however, additional research is required in this area.9, 14 The aim of this study was to isolate factors that discriminate between adults with SCI with elevated depressed mood and those with normal mood, and second, to develop an algorithm that correctly classifies those with depressed mood. It was hypothesized that psychosocial factors would correctly classify the presence of depressed mood whereas injury, demographic and physical health/physical role factors would poorly classify the presence of depressed mood.
Materials and methods
Participants
Participants included 107 adults with SCI living in the community. Adult people with SCI attending outpatient services or who were re-hospitalized in a Sydney SCI rehabilitation unit (n=32) were invited into the study. In addition, participants were approached using community contacts or by advertising in self-help newsletters (n=75). Inclusion criteria of the study consisted of: (a) the presence of an established SCI, that is, at least 6 months post-injury having returned to the community, (b) aged 18–75 years at the time of interview and (c) able to speak English.
Descriptive statistics for age, time since injury, age at injury and years of education are shown in Table 1. Of the total group, 87% (n=93) were male, 61% (n=65) had paraplegia and 49% (n=53) were assessed by a medical specialist to have an incomplete lesion, on the basis of International Standards for Neurological Classification of SCI (http://ais.emsci.org/). Most of the participants (73%, n=78) were on medications, the main types taken being analgesics, anticonvulsants, antispasmodics, hypnotics and anti-depressants.
Study design and procedure
A cross-sectional design was employed and data were collected from participants during a 2-h interview in which participants completed a number of standardized questionnaires. Depending on mobility, assessment was conducted in either the participant’s home or a dedicated room in a research institution.
Assessment
Participants were asked to rate their average pain intensity over the past week using a 0–10 numerical rating scale,17 with 0=‘no pain’ and 10=‘pain as bad as can be imagined.’ Numerical pain-rating scales of this variety have been shown to have good test-retest reliability and validity.17, 18 The Profile of Mood States (POMS) was used to measure mood states.19 The POMS is a 65-Likert item measure of six mood states and a total POMS score. The six mood states include anxiety, depressive mood, anger, vigor, fatigue and confusion. High scores indicate elevated negative mood states except for vigor where high scores indicate increased vigor. The POMS was chosen to assess mood states in the SCI sample because it requests participants to rate themselves over a period of one week on descriptors such as ‘tired’, ‘tense’ and ‘worthless’ (0=not at all and 4=extremely), thereby reducing risks of false-positive detection of depressed mood. The POMS has acceptable validity and a high internal reliability.19
Health-related quality of life was assessed by the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), that has acceptable reliability and validity.20 The SF-36 questionnaire was scored by summing and transforming raw data for each of the eight domains as per the formula in the SF-36 manual.20 Higher scores on the eight domains suggest a higher quality of life. The SF-36 measures eight health-related dimensions including: (a) physical functioning, (b) role limitations due to physical health problems, (c) pain interference with daily activities; (d) general health status (e) vitality, (f) social functioning, (g) role limitations due to emotional problems and (h) mental health. Self-efficacy was assessed by the Moorong Self-Efficacy Scale (MSES) which has acceptable reliability and validity.21 The MSES is scored by summing all 16 items on a 7-point Likert scale ranging from 1 (very uncertain) to 7 (very certain).21 High scores on the MSES suggest high self-efficacy.
Statistical methods
Descriptive statistical analyses were conducted and participants were divided into two sub-groups on the basis of their POMS depressed mood score. The cut-off score was composed of the POMS depressed mood community norm of 8.0 plus one s.d. (s.d.=9), resulting in a split score of 17.19 The first sub-group (low depressed mood) were those with depressed mood scores of <17, whereas the second sub-group (high depressed mood) were those with scores ⩾17. After the split, 77.5% (n=83) were classified as having low depressed mood and 22.5% (n=24) having elevated depressed mood. The limitations of employing a split to demonstrate the impact of a factor upon another are understood.13 These include reduced statistical power and the under-utilization of data that falls close to the split. However, post-hoc power analyses confirmed statistical power was adequate after the split of the sample occurred.
Discriminant function analysis (DFA) was used to identify factors that differentiate participants with high depressed mood from participants with low depressed mood. The categorical/dependent variable used was low versus high depressed mood. Four sets of continuous or categorical independent variables were used to determine the most efficient classification of depressed mood. Choice of factors for each set was on the basis of measures available from the assessment tools used. Final combinations were a result of experimentation with available factors. Predictor sets included: (i) a demographic/injury set including five variables: age at injury, time since injury, years of education, level of lesion (paraplegia/tetraplegia) and completeness of lesion (complete/incomplete); (ii) SF-36 variables physical function, physical role, health and pain, and taking medications (yes or no); (iii) SF-36 variables emotional function and mental health function; (iv) six variables including three SF-36 variables social function, emotional function and mental health, as well as MSES self-efficacy, POMS fatigue and pain intensity.
DFA processes participants’ scores in these sets of variables to determine which sub-group the individuals belong to. Wilk’s λ and χ2 were used to establish the significance of how effective the variables were at discriminating between the two sub-groups. Structure matrix correlations were calculated to show contribution of the independent variables to the discriminant function. DFA presents the proportion of correct classifications comparing predicted group membership with actual group membership. DFA classifies actual cases (that is, into low versus high depressed mood) and then compares with the classification of predicted cases into low versus high depressed mood. If a large proportion of misclassifications occurs, then the predictive capacity of that set is considered poor. For the most effective set isolated by DFA, canonical unstandardized DFA coefficients were generated, and an algorithm was developed to indicate the partial contribution of each variable to the presence of depressed mood. Each variable’s unique contribution to the discriminate function was also calculated. One-way analysis of variances were performed for the most efficient classification set to indicate significant differences between sub-groups. Eta-squared (η2) values are provided for some analyses as an indication of the size of the difference between the two samples. An η2of around 0.03 is considered small, 0.13 is considered a medium difference and over 0.2 is considered a large difference. Post-hoc statistical power of the test is also provided. All analyses were performed using Statistica Software (Version 12, Statsoft, http://www.statsoft.com).
Research ethics
We certify that all applicable institutional regulations concerning the ethical use of human volunteers were followed during the course of this research. Approval was granted by the local institutional human research ethics committee. Written consent was obtained prior to participation in the study.
Results
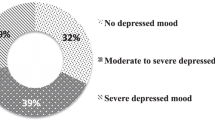
Table 1 shows detail for demographic and injury variables. No significant differences occurred between the two sub-groups for any demographic or injury variable (Wilks’ λ =0.92, F4, 101, P=NS). The low depressed mood sub-group (n=83) had a mean depressed mood score of 5.2 (s.d.=4.9; 95% confidence interval: 4.1–6.2) whereas the high depressed mood sub-group (n=24) had an elevated mean depressed mood score of 28.2 (s.d.=9.3; 95% confidence interval: 24.3–32.1). This difference was significant: F1, 105=64.5, P<0.01, η2=0.38, power=100%. Using the POMS depressed mood score of 17, 22.4% of the SCI sample had clinically elevated levels of depressed mood.
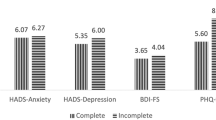
The demographic and injury variable set was not found to discriminate between the sub-groups: Wilks’ λ=0.91, χ210=9.7, P=0.46. Only 4.1% (n=1) of the high depressed mood sub-group were correctly classified as having high depressed mood and 91% of the variance remained unexplained. The physical health, pain and medication variable set discriminated significantly between the two sub-groups: Wilks’ λ=0.80, χ24=23.1, P<0.05; however, only 29% (n=7) of the high depressed mood sub-group were correctly classified and 80% of the variance remained unexplained. The third set, comprised of the two SF-36 emotional and mental health variables discriminated significantly between the two sub-groups: Wilks’ λ=0.53, χ22=66.2, P<0.01; however, the correct classification rate of high depressed mood was still too low at 70% (n=17) whereas 53% of the variance remained unexplained.
The fourth set was found to discriminate significantly between the two sub-groups: Wilks’ λ=0.38, χ26=98.1, P<0.01. DFA correctly classified almost 92% (n=22) of the high depressed mood sub-group, and it correctly classified 95.2% (n=79) of the low depressed mood sub-group. Only 38% of the variance remained unexplained. Table 2 shows descriptive statistics for the sub-groups for these six variables. Multivariate analysis of variance indicated the sub-groups are significantly different: Wilks’ λ=0.38, F6, 100=26.9, P<0.01. Table 2 also shows one-way analysis of variance results for differences between the sub-groups, indicating the six factors may be effective discriminators. Table 3 shows Pearson correlation coefficients between the six factors. Table 4 shows the factor structure loadings/correlations for the six independent variables with the absence or presence of depressed mood. Conventionally, in DFA, associations greater than ±0.3 are considered to be of interest.22 Table 4 shows the six factors correlated above ±0.3 to the discriminant function. Table 5 shows the DFA test of equality of sub-group means for the six variables. Emotional function, mental health and fatigue were found to be significantly different between the two sub-groups, self-efficacy approached significance, whereas social function and pain intensity were non-significant. Unstandardized (raw) canonical discriminant function coefficients for each the six variables were calculated from the DFA to develop an algorithm capable of detecting depressed mood. Higher levels in mental health, emotional health, self-efficacy and social function indicate reduced risk of depressed mood whereas higher levels of pain intensity and fatigue indicate greater risk of depressed mood. The algorithm that could be applied to predicting depression is shown below:

Discussion
On the basis of the POMS depressed mood cut-off score, 22.4% of the participants had elevated levels of depressed mood or probable depression. This rate of probable depression in people with SCI is similar to rates of 21–23% found by prior research.5, 9 The rate of probable depression found in the current study is high compared with rates of around 3–5% found in the adult Australian population.23 This finding provides grounds for increased resources to be directed into research and treatment of depression in adults with SCI.
Although the nature of depression following SCI has been studied extensively,4, 5, 9, 16 our ability to predict adults with SCI at risk of depression is uncertain. To resolve this situation, DFA was used to determine the most effective combinations of injury, demographic, health or psychosocial factors that could discriminate the presence or absence of depressed mood. Injury and demographic variables did not discriminate well. This is consistent with earlier research that has not found impairment-related or demographic factors to be predictive of depression.9 The DFA was significant for the second set comprising physical role, physical function, general health, pain and taking medications; however, it classified the presence of high levels of depressed mood poorly, and again this has been suggested previously.4, 5, 9
The third set was employed to determine whether core symptoms of depression could accurately detect the presence of depressed mood. Although the DFA was significant, only 70% of the high depressed mood sub-group were correctly identified. This finding demonstrates that the etiology of depression is more complex than its core symptoms. Arguably then, attempts at predicting depression will require the use of a broader combination of factors that have potential to accurately classify participants with elevated depressed mood. The fourth set of psychosocial factors, only mildly related to each other (see Table 3), had an evidence base suggesting they could be promising predictors of depressed mood.4, 5, 6, 9, 16 These factors significantly contributed to the presence of depressed mood, and almost 92% (n=22) were correctly classified as having elevated depressed mood. Further, the high depressed mood sub-group had significantly higher risks on all six psychosocial factors (see Table 2), and the DFA loadings shown in Table 4 were all ⩾0.3, suggesting all factors contributed to the discriminate function. This finding is strengthened by prior research which has found factors like poor self-efficacy (or perceived helplessness), coping appraisals, chronic pain and chronic fatigue to be associated with elevated depressed mood following SCI.1, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 16 Furthermore, this DFA analytic approach complements work done to validate tools like the PHQ-9 and the many studies examining correlates/covariates of depression in the SCI population.3, 4, 5, 6, 9, 16
Given the above, it is timely that additional resources be invested in the development of psychosocial strategies that can detect/predict long-term depression following SCI. As stated earlier, it is desirable to predict risk of long-term depression so as to prevent the diminished well-being that accompanies depressive mood, especially as effective psychosocial-based treatments are available that can reduce risk of depression.4, 5, 9 The psychosocial set algorithm provides a feasible approach for predicting depressed mood in adults with SCI. Clearly, however, additional work is required before confidence in this approach is established. Limitations require discussion. The algorithm requires refinement in terms of its components ensuring assessment is easily applied in a clinical or research setting. Further, six factors may not be required for the algorithm to be predictive, given pain intensity and social function did not contribute significantly. However, at this stage it may be prudent to leave all factors in the algorithm for future development, as all six have strong associations with depressed mood.4, 5, 16 Given the sample was cross-sectional, a further limitation of the current research is the problem of generalizability, requiring prospective research in a SCI cohort testing the predictive capacity of this algorithm. However, research is ongoing that will evaluate the effectiveness of this algorithm at predicting people with a SCI who are at risk of developing depressed mood.
Data Archiving
There were no data to deposit.
References
Middleton J, Tran Y, Craig A . Relationship between quality of life and self-efficacy in persons with spinal cord injuries. Arch Phys Med Rehabil 2007; 88: 1643–1648.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ . A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Bombardier CH, Richards JS, Krause JS, Tulsky D . Symptoms of major depression in people with spinal cord injury: implications for screening. Arch Phys Med Rehabil 2004; 85: 1749–1756.
Craig A, Tran Y, Middleton J . Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009; 47: 108–114.
Fann R, Bombardier CH, Richards JS, Tate DG, Wilson CS, Temkin N . Depression after spinal cord injury: comorbidities, mental health service use, and adequacy of treatment. Arch Phys Med Rehabil 2011; 92: 352–360.
Kennedy P, Rogers B . Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000; 81: 932–937.
Ullrich PM, Smith BM, Poggensee L, Evans CT, Stroupe KT, Weaver FM et al. Pain and post-traumatic stress disorder symptoms during inpatient rehabilitation among operation enduring freedom/ operation Iraqi freedom veterans with spinal cord injury. Arch Phys Med Rehabil 2013; 94: 80–85.
Kennedy P, Evans MJ . Evaluation of post traumatic distress in the first 6 months following SCI. Spinal Cord 2001; 39: 381–386.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Wijesuriya N, Tran Y, Middleton J, Craig A . The impact of fatigue on the health related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil 2012; 93: 319–324.
Craig A, Tran Y, Wijesuriya N, Middleton J . Fatigue and tiredness in people with spinal cord injury. J Psychosom Res 2012; 73: 205–210.
Lidal IB, Jensen AE, Larsen TW, Stanghelle JK . Fatigue in persons who have lived with spinal cord injury for >20 years. Spinal Cord 2013; 51: 103–108.
Craig A, Tran Y, Siddall P, Wijesuriya N, Lovas L, Bartrop R et al. Developing a model of associations between chronic pain, depressive mood, chronic fatigue and self-efficacy in people with spinal cord injury. J Pain 2013; 14: 911–920.
Graves DE, Bombadier CH . Improving the efficiency of screening for major depression in people with spinal cord injury. J Spinal Cord Med 2008; 31: 177–184.
Mitchell MC, Burns NR, Dorstyn DS . Screening for depression and anxiety in spinal cord injury with DASS-21. Spinal Cord 2008; 46: 547–551.
Elfström ML, Rydén A, Kreuter M, Persson LO, Sullivan M . Linkages between coping and psychological outcome in the spinal cord lesioned: development of SCL-related measures. Spinal Cord 2002; 40: 23–29.
Widerstrom-Noga E, Biering-Sorensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP et al. The International Spinal Cord Injury Pain Basic Data Set. Spinal Cord 2008; 46: 818–823.
Jensen MP, Turner JA, Romano JM, Fisher LD . Comparative reliability and validity of chronic pain intensity measures. Pain 1999; 83: 157–162.
McNair DM, Lorr M, Droppleman LF, POMS Profile Of Mood States Manual. MHS: New York. 2005.
Ware JE, Snow KK, Kosinski M, Gandek B . Sf-36 Health Survey: Manual & Interpretation Guide. The Health Institute, New England Medical Centre: Boston. 1993.
Middleton JW, Tate RL, Geraghty TJ . Self-efficacy and spinal cord injury: psychometric properties of a new scale. Rehabil Psychol 2003; 48: 281–288.
Tabachnick BG, Fidell LS . Using Multivariate Statistics 2nd Ed. Harper & Row: New York. 1989.
Wilhelm K, Mitchell P, Slade T, Brownhill S, Andrews G . Prevalence and correlates of DSM-IV major depression in an Australian national survey. J Affect Dis 2003; 75: 155–162.
Acknowledgements
We acknowledge the financial support of the Lifetime Care Support Authority (NSW, Australia), the Australian Research Council (LP0560590) and the Australian Rotary Health. We also acknowledge the contribution of Drs Judy Lovas and Nirupama Wijesuriya to the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Craig, A., Rodrigues, D., Tran, Y. et al. Developing an algorithm capable of discriminating depressed mood in people with spinal cord injury. Spinal Cord 52, 413–416 (2014). https://doi.org/10.1038/sc.2014.25
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.25
Keywords
This article is cited by
-
Depressive mood in adults with spinal cord injury as they transition from an inpatient to a community setting: secondary analyses from a clinical trial
Spinal Cord (2017)
-
Perceived effectiveness and mechanisms of community peer-based programmes for Spinal Cord Injuries—a systematic review of qualitative findings
Spinal Cord (2017)
-
Factors predicting resilience in people with spinal cord injury during transition from inpatient rehabilitation to the community
Spinal Cord (2015)