Key Points
-
With the creation of flexible ureteroscopes with reduced calibre and holmium lasers of increased power, management of upper-tract urinary stones has changed towards ureteroscopic treatment
-
The techniques of stone dusting or basketing both have advantages and disadvantages, but ultimately a number of factors including surgeon preference, stone size and composition determine which is used
-
Further clinical trials are needed to define the role of these two ureteroscopic techniques for upper-urinary-tract stones
-
Technological developments such as rendering fragments paramagnetic, focused ultrasonic propulsion and lasers with increased power should improve stone-free rates as well as patient satisfaction
Abstract
Over the past two decades, the management of upper-tract urinary stones has dramatically changed towards an increase in the use of ureteroscopic treatment. This change has been driven by technological advances such as the creation of flexible ureteroscopes with reduced calibre (which now have digital, disposable and dual flexion capability) and holmium lasers with increased power. Two basic principles exist when treating stones ureteroscopically: either creating stone dust and small fragments (<1–2 mm) to theoretically enable spontaneous passage of the small particles or stone fragmentation that enables safe extraction of the stone pieces with a basket or grasper in an efficient manner. Each method has unique advantages and disadvantages, but, ultimately, surgeon preference, stone size, composition, location and intrarenal and/or ureteral anatomy determine which technique is used. To date, clinical trials comparing these two techniques are lacking.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Matlaga, B., Jansen, J., Meckley, L., Byrne, T. & Lingeman, J. Treatment of ureteral and renal stones: a systematic review and meta-analysis of randomized, controlled trials. J. Urol. 188, 130–137 (2012).
Sofer, M. et al. Holmium:YAG laser lithotripsy for upper urinary tract calculi in 598 patients. J. Urol. 167, 31–34 (2002).
Preminger, G., Assimos, D. & Lingeman, J. AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J. Urol. 173, 1991–2000 (2005).
Kim, S., Kuo, R. & Lingeman, J. Percutaneous nephrolithotomy: an update. Curr. Opin. Urol. 13, 235–241 (2003).
Michel, M., Trojasn, L. & Rassweiler, J. Complications in percutaneous nephrolithotomy. Eur. Urol. 51, 899–906 (2007).
Hyams, E., Munver, R., Bird, V., Uberoi, J. & Shah, O. Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2 to 3 cm: a multi-institutional experience. J. Endourol. 24, 1583–1588 (2010).
Cohen, J., Cohen, S. & Grasso, M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. Br. J. Urol. Int. 111, 127–131 (2012).
Aboumarzouk, O., Monga, M., Kata, S., Traxer, O. & Somani, B. Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J. Endourol. 25, 1257–1263 (2012).
Marks, A. & Teichman, J. Lasers in clinical urology: state of the art and new horizons. World J. Urol. 25, 227–233 (2007).
Teichman, J., Vassar, G. & Glickman, R. Holmium:yttrium-aluminum-garnet lithotripsy efficiency varies with stone composition. Urology 52, 392–397 (1998).
Grasso, M. Experience with the holmium laser as an endoscopic lithotrite. Urology 48, 199–206 (1996).
Chan, K. et al. Holmium:YAG laser lithotripsy: a dominant photothermal ablative mechanism with chemical decomposition of urinary calculi. Lasers Surg. Med. 25, 22–37 (1999).
Pierre, S. & Preminger, G. Holmium laser for stone management. World J. Urol. 25, 235–239 (2007).
Patel, A. P. & Knudsen, B. E. Optimizing use of the holmium: YAG laser for surgical management of urinary lithiasis. Curr. Urol. Rep. 15, 397 (2014).
Hecht, S. L. & Wolf, J. Techniques for holmium laser lithotripsy of intrarenal calculi. Urology 81, 442–445 (2013).
Chawla, S. N., Chang, M. F., Chang, A., Lenoir, J. & Bagley, D. H. Effectiveness of high-frequency Holmium:YAG laser stone fragmentation: the “popcorn effect”. J. Endourol. 22, 645–649 (2008).
Sea, J. et al. Optimal power settings for Holmium: YAG lithotripsy. J. Urol. 187, 914–919 (2012).
Traxer, O. & Thomas, A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J. Urol. 189, 580–584 (2013).
Delvecchio, F. C. et al. Assessment of stricture formation with the ureteral access sheath. Urology 61, 518–522 (2003).
Rapoport, D., Perks, A. & Teichman, J. Ureteral access sheath use and stenting in ureteroscopy: effect on unplanned emergency room visits and cost. J. Endourol. 21, 993–997 (2007).
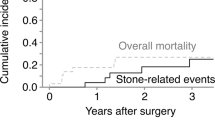
Rebuck, D., Macejko, A., Bhalani, V., Ramos, P. & Nadler, R. The natural history of renal stone fragments following ureteroscopy. Urology 77, 564–568 (2011).
Chew, B. et al. Natural history, complications and re-Intervention rates of asymptomatic residual stone fragments after ureteroscopy: a report from the EDGE Research Consortium. J. Urol. 195, 982–986 (2016).
Ito, H. et al. Preoperative factors predicting spontaneous clearance of residual stone fragments after flexible ureteroscopy. Int. J. Urol. 22, 372–377 (2015).
Hyams, E. S., Bruhn, A., Lipkin, M. & Shah, O. Heterogeneity in the reporting of disease characteristics and treatment outcomes in studies evaluating treatments for nephrolithiasis. J. Endourol. 24, 1411–1414 (2010).
Schatloff, O., Lindner, U., Ramon, J. & Winkler, H. Randomized trial of stone fragment active retrieval versus spontaneous passage during holmium laser lithotripsy for ureteral stones. J. Urol. 183, 1031–1035 (2010).
Shah, O. & Humphreys, M. R. Dusting versus basketing during ureteroscopic lithotripsy—what is more efficacious? Interim analysis from a multi-centre prospective trial from the EDGE Research Consortium. AUA News 20, (2015).
Chew, B. H. et al. Dusting versus basketing during ureteroscopic lithotripsy—what is more efficacious? Interim analysis from a multi-centre prospective trial from the EDGE Research Consortium [abstract]. J. Urol. 193, 261–262 (2015).
Portis, A., Laliberte, M., Drake, S., Rosenberg, M. & Bretzke, C. Intraoperative fragment detection during percutaneous nephrolithotomy: evaluation of high magnification rotational fluoroscopy combined with aggressive nephroscopy. J. Urol. 175, 162–165 (2006).
Cloutier, J. et al. The glue-clot technique: a new technique description for small calyceal stone fragments removal. Urolithiasis 42, 441–444 (2014).
Tracy, C. R. et al. Rendering stone fragments paramagnetic with iron-oxide microparticles improves the efficiency and effectiveness of endoscopic stone fragment retrieval. Urology 76, 1266–1270 (2010).
Sorensen, M. D. et al. Focused ultrasonic propulsion of kidney stones: review and update of preclinical technology. J. Endourol. 27, 1183–1186 (2013).
Bailey, M. et al. Acoustic radiation force to reposition kidney stones. J. Acoust. Soc. Am. 133, 3279 (2013).
Harper, J. et al. Focused ultrasound to expel calculi from the kidney: safety and efficacy of a clinical prototype device. J. Urol. 190, 1090–1095 (2013).
Shah, A. et al. Focused ultrasound to expel calculi from the kidney. J. Urol. 187, 739–743 (2012).
Shah, A. et al. Novel ultrasound method to reposition kidney stones. Urol. Res. 38, 491–495 (2010).
Wang, Y. et al. Determination of tissue injury thresholds from ultrasound in a porcine kidney model. J. Acoust. Soc. Am. 133, 3411 (2013).
Bailey, M. et al. Ultrasonic propulsion of kidney stones: preliminary results of human feasibility study. IEEE Int. Ultrason. Symp. 511–514 (2014).
Morhardt, D. R., Tracey, J., Wolf, J. & Ghani, K. R. The new Stone Age: outcomes of ureteroscopic stone dusting using a 120-watt Holmium laser [abstract]. J. Urol. 193, 580–581 (2015).
Author information
Authors and Affiliations
Contributions
Both authors researched data for, discussed content for, wrote, reviewed and edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
O.S. has been a consultant and lecturer and served on the scientific advisory board for Boston Scientific. He is an Assistant Editor for the Journal of Urology and has served on the Guidelines Committee for Surgical Management of Stone Disease for the American Urological Association. He is also the Editor of a textbook for Elsevier and is a Special Government Employee for the Food and Drug Administration, USA. B.W. declares no competing interests.
Rights and permissions
About this article
Cite this article
Weiss, B., Shah, O. Evaluation of dusting versus basketing — can new technologies improve stone-free rates?. Nat Rev Urol 13, 726–733 (2016). https://doi.org/10.1038/nrurol.2016.172
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2016.172
This article is cited by
-
Temperature changes of renal calyx during high-power flexible ureteroscopic Moses holmium laser lithotripsy: a case analysis study
International Urology and Nephrology (2023)
-
Initial experience with the graphical user interface for laser parameters setting of a new thulium fibre laser source device for urinary pathologies treatment
World Journal of Urology (2023)
-
Femtosecond laser lithotripsy: a novel alternative for kidney stone treatment? Evaluating the safety and effectiveness in an ex vivo study
Urolithiasis (2023)
-
Initial clinical experience with the pulsed solid-state thulium YAG laser from Dornier during RIRS: first 25 cases
World Journal of Urology (2023)
-
Initial clinical experience with the new thulium fiber laser: first 50 cases
World Journal of Urology (2021)