Abstract
The central nervous system (CNS) has a limited capacity to spontaneously regenerate following traumatic injury or disease, requiring innovative strategies to promote tissue and functional repair. Tissue regeneration strategies, such as cell and/or drug delivery, have demonstrated promising results in experimental animal models, but have been difficult to translate clinically. The efficacy of cell therapy, which involves stem cell transplantation into the CNS to replace damaged tissue, has been limited due to low cell survival and integration upon transplantation, while delivery of therapeutic molecules to the CNS using conventional methods, such as oral and intravenous administration, have been limited by diffusion across the blood–brain/spinal cord-barrier. The use of biomaterials to promote graft survival and integration as well as localized and sustained delivery of biologics to CNS injury sites is actively being pursued. This review will highlight recent advances using biomaterials as cell- and drug-delivery vehicles for CNS repair.
Similar content being viewed by others
INTRODUCTION
The central nervous system (CNS), composed of the brain, spinal cord, and retina, has a limited capacity to spontaneously regenerate and this, coupled with few regenerative strategies available, provides few treatment options for patients with CNS injuries or diseases. With only pharmacological treatments available that delay the progression of CNS diseases, there is a critical need for regenerative medicine strategies that overcome disease progression and promote tissue regeneration. CNS diseases are complex, resulting in loss of sensory, motor, and cognitive functions, as is the case in Parkinson’s disease (Davie, 2008), Alzheimer’s disease (Citron, 2010), multiple sclerosis (Lassmann et al, 2012), traumatic injuries (Bruns and Hauser, 2003; Lo et al, 2003; Sekhon and Fehlings, 2001), and impaired vision for retinal diseases such as retinitis pigmentosa (RP) (Shintani et al, 2009) and age-related macular degeneration (AMD) (de Jong, 2006). A multitude of mechanisms may contribute to CNS injury, including apoptotic and necrotic death of neurons (including photoreceptors), astrocytes and oligodendrocytes, axonal injury, demyelination, excitotoxicity, ischemia, oxidative damage, and inflammation (Fitch and Silver, 2008). The lack of tissue regeneration is attributed to an overall absence of axon-growth promoting factors (eg, the local presentation of growth promoting factors and extracellular matrix (ECM) proteins) and presence of axonal growth inhibitory/repulsive molecules (eg, myelin-associated proteins, and the glial scar which constitutes a chemical and physical barrier) at and around the lesion site (Fitch and Silver, 2008), see Box 1.
Successful therapeutic strategies have been difficult to achieve due to the complexity of the CNS and an inhospitable environment in and around the lesion site for cell transplantation. Limited diffusion of drugs/biologics across the blood–brain barrier (BBB) further restricts the utility of common delivery methods (ie, oral and intravenous). This review will focus primarily on regenerative medicine strategies—that is cell transplantation and endogenous cell stimulation—with particular focus on the role of biomaterials to promote recovery following traumatic brain and spinal cord injuries, and degenerative diseases, such as AMD and RP, which cause degeneration of the photoreceptors and the retinal pigment epithelium (RPE).
Overview of Cell-Based Treatment Strategies
Several strategies to promote tissue regeneration after injury are currently being pursued including cell-based therapies and delivery of bioactive molecules such as small molecules, growth factors, and antibodies (Pakulska et al, 2012; Shoichet et al, 2008). Cell-based therapies aim to replace and/or promote the survival of damaged cells or alter the local environment to be more conducive for regeneration by, for example, providing trophic support. Treatment strategies include transplantation of mesenchymal stromal cells (MSCs) (Bang et al, 2005; Kode et al, 2009), neural stem/progenitor cells (NSPCs) (Kokaia et al, 2012), embryonic stem cells (ESCs) (Lerou and Daley, 2005), induced pluripotent stem cells (iPSCs) (Willerth, 2011) and their differentiated progeny into the injured/diseased CNS (Box 2). Such cells can act to regenerate damaged host tissue either by directly integrating into the tissue (ie, cell replacement) or indirectly by secreting factors, which promote neuroprotection or neurogenesis (Bliss et al, 2010). For the latter approach, cells are used that are known to produce a variety of factors that have been shown to be beneficial after injury including neurotrophic factors, such as nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), neurotrophin-3 (NT-3), ciliary neurotrophic factor (CNTF), glial cell-derived neurotrophic factor (GDNF), and leukemia inhibitory factor (LIF), and ECM proteins, such as laminin, fibronectin, collagen I/III and IV (Fortun et al, 2009; White and Jakeman, 2008; Wright et al, 2003). Early clinical trials showed that cell transplantation of MSCs (Bang et al, 2005) or an immortalized cell line of immature neurons derived from human teratocarcinomas (Kondziolka et al, 2005), into the stroke-injured brain of human patients had no adverse effects (Wechsler, 2009). Unfortunately, the clinical efficacy of cell transplantation techniques has been limited by poor cell survival, uncontrolled differentiation, and ineffective integration into the host tissue, primarily due to an inhospitable environment at and around the injury site. Biomaterial hydrogels, described in detail herein, are being investigated to enhance cell survival, host-tissue integration, and even attenuate the inflammatory response.
Overview of Drug/Biologics-Based Treatment Strategies
Bioactive molecules delivered to the CNS have been pursued to promote tissue regeneration—ie, neurogenesis, plasticity, axonal regeneration, and neuroprotection. For example, intraventricular sequential delivery of epidermal growth factor (EGF) and erythropoietin (EPO) into the stroke-injured rat brain showed enhanced migration of endogenous NSPCs (see Box 2) to the injury site, resulting in neurogenesis and improved functional recovery (Kolb et al, 2007). Likewise, growth factors such as interferon-γ (Victorio et al, 2010) and GDNF (Zhang et al, 2009) have been shown to be neuroprotective and promote axonal outgrowth, respectively, following SCI. However, the low permeability of the BBB and blood–spinal cord barrier limit diffusion of therapeutics using conventional delivery strategies (Pardridge, 2012), requiring either high systemic doses to reach therapeutic concentrations at the injury site, which often leads to systemic cytotoxicity, or local delivery strategies. Systemic administration leads to off-target distribution of therapeutic molecules, and can result in undesired side effects such as tumor formation and fibrosis (Lee et al, 2000). Several strategies are being pursued to enhance drug permeability across the BBB, including drug delivery via liposomes or nanoparticles (NPs) (Patel et al, 2009). Alternative strategies that circumvent the BBB, resulting in direct tissue delivery, include direct injection into the injury site or intraventricular injection, but these too are associated with possible risks such as cerebral edema and convulsions. Injections into the intrathecal space that surrounds the spinal cord can yield higher concentrations of the therapeutic molecule in the target tissue immediately following injection compared to systemic injections, but this approach is limited by the rapid distribution and elimination of the therapeutics by the cerebrospinal fluid (Groothuis, 2000).
Combination Treatment Strategies
Combination strategies involving cells, bioactive molecules and biomaterials have been pursued over the past several years as a means to both enhance cell survival and integration after cell transplantation and achieve local delivery to the brain, thereby circumventing the BBB and systemic side effects (Orive et al, 2009; Pakulska et al, 2012). Similar to drug delivery, cell transplantation also poses potential systemic side effects when the cells are injected intravenously and not directly into or adjacent to the injury (Quertainmont et al, 2012). Biomaterials can serve as delivery vehicles for therapeutic molecules such as growth factors, proteins, and small molecules to provide a sustained and tunable drug release profile, without the need for multiple, high-dosage treatments (Hoare and Kohane, 2008). They can also be used as cell delivery vehicles, where they can provide physical support for cells to ensure their retention and distribution at the site of transplantation. Hydrogels are water swollen materials, which are particularly compelling for transplantation into soft tissue, such as the CNS, because they can match the mechanical properties of the tissue, are non-cytotoxic and allow both facile migration of cells and diffusion of biomolecules out of the scaffold while maintaining a physical structure (Drury and Mooney, 2003; Tibbitt and Anseth, 2009; Zhu and Marchant, 2011).
We will focus on recent advances using biomaterial hydrogels to study cell–substrate interactions and their use in cell transplantation and bioactive molecule delivery to the injured CNS, with specific focus on the brain and spinal cord after traumatic injury, and the retina due to disease.
CELL–SUBSTRATE INTERACTIONS: DESIGNING HYDROGELS TO MIMIC THE ECM
Cells and their extracellular matrix (ECM) define the cellular microenvironment in terms of chemical, physical and mechanical properties. The CNS ECM comprises proteoglycans such as chondroitin sulfate proteoglycans (CSPGs), glycosaminoglycans such as hyaluronan (HA), and proteins such as laminin, collagen, and fibronectin (Zimmermann and Dours-Zimmermann, 2008). Hydrogels can mimic the chemical, physical, and mechanical properties of the ECM to promote cell adhesion, proliferation, and differentiation (see Box 3). A commonly used hydrogel is Matrigel; however, as it is derived from a mouse sarcoma, its composition is complex and variable (Kleinman and Martin, 2005), making well-defined studies difficult to achieve and reproduce. In order to mimic the native ECM, a hydrogel that provides a blank palette on which biomolecules can be painted is often used to promote specific cell–substrate interactions. Recent advances on neural cell–biomaterial interactions are highlighted below, including chemical signals (the role of cell-adhesive molecules, growth factors and other cells); mechanical cues; and physical cues (ie, architecture of the biomaterial) on neural cellular response (Figure 1).
Schematic representation of the multiple interactions of the cellular microenvironment, including: cell–cell and cell–substrate interactions where the ECM is defined by its chemical, physical, and mechanical properties: stiffness and elasticity, matrix degradability, permeability and density of ECM components. Figure adapted with permission Owen and Shoichet (2010); copyright 2010 Wiley Periodicals Inc.
Chemical Signals
ECM proteins represent key components in the cell niche that dictates cell fate. These proteins are recognized by cell surface receptors and are involved in cellular processes such as proliferation, differentiation, and migration. For example, fibronectin is a major component of the ECM that binds with cell surface receptors, known as integrins, to promote cell adhesion and viability (Prowse et al, 2011). Although the uninjured adult CNS contains limited fibronectin (DeQuach et al, 2011; Volpato et al, 2013), it has an important role in the developing CNS and has been shown to promote axonal regeneration of adult neurons (Tonge et al, 2012). Pierschbacher and Ruoslahti (1984) discovered that a short synthetic peptide, arginine–glycine–aspartate (RGD), derived from fibronectin also binds to integrins and promotes cell adhesion and viability (Hersel et al, 2003). Since this initial discovery, numerous other ECM-derived synthetic peptides have been identified to bind to integrin receptors. Given the importance of laminin in the neural ECM, laminin-derived peptides have been investigated: tyrosine–isoleucine–glycine–serine–arginine (YIGSR) (Graf et al, 1987) and isoleucine–lysine–valine–alanine–valine (IKVAV) (Tashiro et al, 1989) promote neural cell adhesion and neurite outgrowth, respectively, and similarly, the neural cell adhesion molecule (NCAM)-derived amino-acid sequence, EVYVVAENQQGKSKA, induces neurite outgrowth and increases neuronal survival (Neiiendam et al, 2004).
To take advantage of key cell–ECM interactions, these cell-adhesive peptides have been incorporated into biomaterial strategies. The conformation of the peptide is critical to its binding with the corresponding integrin receptor. For this reason, longer peptide chains (Beer et al, 1992; Craig et al, 1995), cyclic peptides (Haubner et al, 1996; Kato and Mrksich, 2004), and/or peptide pairs (Grant et al, 1997; Mardilovich et al, 2006) are often immobilized to biomaterial surfaces to optimize cellular interaction. Presentation of the immobilized peptide is also critical to its cellular interaction (Maheshwari et al, 2000; Massia and Hubbell, 1991) and thus careful attention has been devoted to the conjugation chemistry. Peptide adsorption and/or non-specific conjugation disrupts peptide conformation, resulting in poor receptor binding and irreproducible results. Bio-orthogonal, water-based reactions provide superb peptide immobilization strategies, as they rely on specific coupling chemistry yielding controlled biomolecule orientation, which are key in subsequent bioactivity studies (Azagarsamy and Anseth, 2013). For example, Silva et al (2012) used orthogonal Diels–Alder click chemistry to immobilize the GRGDS peptide to a chemically-modified gellan gum hydrogel and showed greater cell adhesion and viability of NSPCs (Silva et al, 2012). Similarly, increased dorsal root ganglia neurite outgrowth was observed on elastin-mimetic polypeptide hydrogels functionalized with RGD (Lampe et al, 2013) and acrylate-modified dextran hydrogels functionalized with thiolated YIGSR and IKVAV peptides (Levesque and Shoichet, 2006).
Growth factors represent another key component in the cell niche that dictates cell fate. These proteins have cellular receptors and are involved in intracellular signaling processes resulting in proliferation, differentiation, and migration. Site-specific conjugation of growth factors to hydrogels is also key to cellular recognition. Taking advantage of the bio-orthogonal, high-affinity binding between biotin and streptavidin, biotin-platelet-derived growth factor (PDGF-AA) was conjugated to streptavidin-containing hydrogels, such as agarose (Aizawa et al, 2008) or hyaluronan/methylcellulose (HAMC) (Tam et al, 2012), and shown to promote the differentiation of rat NSPCs into oligodendrocytes. Similarly, when biotin–interferon-γ was conjugated to streptavidin-modified chitosan hydrogels, NSPCs differentiated preferentially into neurons (Leipzig et al, 2010). In these examples, the immobilized growth factors were repeatedly shown to promote similar NSPC differentiation as soluble growth factor controls, thereby demonstrating the potential of the immobilized growth factor, not only for in vitro differentiation but also for use in cell transplantation studies.
To understand cell–cell and cell–substrate interactions in the cell niche, defined biomimetic three-dimensional (3D) microenvironments can be created. The cytoarchitecture of the CNS is intricate and important for correct function. For example, the retina consists of seven cell types arranged in six layers, which are required for vision. Immobilization of specific growth factors and/or adhesion peptides within spatially defined volumes of a 3D hydrogel may promote preferential differentiation of retinal stem cells (RSCs) to a given phenotype in such spatially defined volumes, thereby providing a platform to study cellular interactions (and disease progression) in vitro (Figure 2). Bio-orthogonal chemistry is particularly compelling for selective and spatially controlled immobilization of biomolecules in 3D. For example, protein concentration gradients and protein patterns were created in 3D hydrogels using multi-photon irradiation to precisely bind a given protein (Wosnick and Shoichet, 2008). In this technique, a photo-labile molecule is conjugated to a reactive functional group (eg, thiol) of the hydrogel. Exposure of these photo-labile protecting groups to multi-photon irradiation can be achieved in a spatially defined manner in 3D with micrometer resolution, thereby cleaving the photo-labile groups in a specific region of the hydrogel; subsequent conjugation reactions with bioactive molecules modified with the complimentary bio-orthogonal functional group (eg, maleimide or acrylate) results in spatially controlled immobilization of bioactive molecules. Numerous growth factors, such as CNTF, sonic hedgehog (SHH) (Wylie et al, 2011), vascular endothelial growth factor-165 (VEGF165) (Aizawa et al, 2010), and EGF (Owen et al, 2013), as well as cell-adhesive RGD peptides (DeForest and Anseth, 2011) have been photopatterned into various hydrogels such as agarose, hyaluronan, and poly(ethylene glycol) (PEG). When a photopatterned concentration gradient of VEGF165 was immobilized in a GRGDS-modified agarose hydrogel, Aizawa et al (2010) demonstrated primary brain endothelial cell migration, resulting in tubule-like structures in 3D. Moreover, a symbiotic interaction between endothelial cells and retinal progenitor cells (RPCs) was observed in these gels: RPCs only grew into gels when cultured with endothelial cells, while endothelial tubules were stabilized by co-culture with RPCs (Aizawa and Shoichet, 2012). This may provide some insight into the RSC niche. Interestingly, Wylie et al (2011) reported the concomitant immobilization of multiple growth factors (CNTF and SHH) within distinct volumes of an agarose hydrogel in a spatially controlled fashion. NSPCs cultured on a GRGDS-modified agarose hydrogel migrated into the gel along a SHH concentration gradient (Wylie et al, 2011). These studies demonstrate that photopatterning can be used to control the spatial orientation of growth factors and peptides to create biomimetic 3D environments. The defined matrices can be used to study cell–cell and cell–substrate interactions, which may provide insight into disease progression, developmental biology, or drug screening.
Concept schematic for the spatial immobilization of growth factors that will preferentially and spatially differentiate retinal stem/progenitor cells to progeny of the retina in a layered structure.
The synergism between immobilized growth factors and cell adhesion molecules has been shown to influence cell receptor activation, resulting in improved signaling and bioactivity (Comoglio et al, 2003). Martino et al (2011) reported that by including growth factors (ie, PDGF, VEGF, and bone morphogenetic protein-2) on the same fibrin polymeric backbone as the integrin-binding domain, greater bioactivity was observed compared with binding them on separate polymer backbones. It was hypothesized that synergistic activation of integrins and receptor kinases occurs when the corresponding ligands of these receptors are in close spatial proximity to each other. This was further supported by Tam et al (2012) who demonstrated that co-conjugation of PDGF-A and the cell adhesive RGD peptide to the same polymer backbone promoted greater differentiation of NSPCs into oligodendrocytes compared with controls of each bioactive molecule alone or even both on separate polymeric backbones. Together, the studies demonstrate that cell–substrate interactions are influenced not only by the presence of specific ligands but also by their spatial orientation relative to each other. These are important considerations when designing biomaterials to promote specific cellular responses such as adhesion and/or differentiation whether for in vitro culture or in vivo transplantation.
Mechanical Cues
An effective biomimetic hydrogel will also emulate the physical and mechanical properties of the 3D environment. For example, Leipzig and Shoichet (2009) showed that gel stiffness affected the differentiation profile of rat neural stem cells. NSPCs cultured on softer (<1 kPa) methacrylamide chitosan hydrogels differentiated predominantly into astrocytes and neurons, whereas those cultured on hydrogels stiffer than 7 kPa differentiated largely into oligodendrocytes. Furthermore, NSPCs cultured on gels with an intermediate stiffness (3.5 kPa) exhibited the greatest amount of proliferation. Thus, even subtle differences in mechanical properties (while maintaining similar chemical properties) can influence cell fate. Recently, Sur et al (2013) reported that dissociated hippocampal cells derived from mouse embryos cultured on peptide amphiphile hydrogels (∼7 kPa) showed significantly increased neuronal differentiation, maturation, and synapse density compared with cells cultured on stiffer hydrogels (∼25 kPa). MSCs also responded differently to varying mechanical properties: on soft substrates, with moduli comparable to that of the brain (0.1–1 kPa), MSCs preferentially differentiated to neural-like cells; on intermediate stiffness substrates, MSCs differentiated to myogenic cells, and on bone-like stiffness substrates (25–40 kPa), MSCs differentiated to osteogenic cells (Engler et al, 2006). Moreover, cell viability was higher on softer hydrogels (Liu et al, 2010). Interestingly, Musah et al (2012) reported that the viability of human ESCs increased when cultured on stiff poly(acrylamide) hydrogels. These seemingly conflicting results demonstrate that each cell type responds differently to changes in their physical environment, and thereby provide valuable insight into their development, while at the same time informing effective bioengineered materials strategies for tissue repair.
Physical Topographical Cues
The architecture of the native ECM is formed by dynamic cell remodeling, whereby cells can secrete and degrade structural molecules such as hyaluronan to create 3D environments necessary for cellular functions (Kim et al, 2011b). The formation of ECM structures, such as fibers, pores, and ridges, provides important structural support for cellular organization, as well as physical cues for cellular interactions (Flemming et al, 1999; Hoffman-Kim et al, 2010). The size and shape of two-dimensional biomaterial substrates coated with purified ECM molecules has been shown to influence the fate and function of adherent cells such as endothelial cells (Chen et al, 1997, 1998; Singhvi et al, 1994). For example, relatively large islands of ECM molecules have been reported to promote proliferation, while in stark contrast small islands have been shown to induce apoptosis. Other studies have demonstrated that aligned ECM molecules, as well as the micron-scale topography of fibers or grooves, exert substantial effects on the guidance and orientation of neural cells and their processes (Lietz et al, 2006; Rajnicek et al, 1997; Schnell et al, 2007). This is of particular interest in the development of biomaterial-based scaffolds intended to promote the repair of nervous system tissues, which are highly organized, such as the retina or white matter tracts of the spinal cord (Suzuki and Raisman, 1992). In vitro studies have demonstrated the influence of fiber diameter on the orientation of process outgrowth. The greater surface curvature of small-diameter fibers prompted an increasing tendency for neurite outgrowth to follow the longitudinal axis of the fibers: small-caliber fibers promoted greater oriented process growth than large-caliber fibers (Smeal et al, 2005; Smeal and Tresco, 2008). Recent advances in nanotechnology and especially electrospinning have led to an interest in cell–substrate interactions in the sub-micron range (Schnell et al, 2007). The ability of fibers with diameters in the sub-micron range to affect the behavior of neural and non-neural cells (Bockelmann et al, 2011; Mo et al, 2004; Sun et al, 2005) has been demonstrated in vitro.
Studies into the role of biomaterial topography in the context of regenerative medicine and nerve repair include 3D scaffolds (Bozkurt et al, 2009). In vivo, Tsai et al (2004) demonstrated that poly(2-hydroxyethyl methacrylate-co-methylmethacrylate) hydrogel channels can be used to improve tissue regeneration of transected rat spinal cords. By inserting the transected cord stumps into the hydrogel nerve guidance channels, axonal regeneration was enabled by contact guidance cues while at the same time limiting the growth of scar tissue and maintaining alignment of both the cord stumps and migrating cells. Moore et al (2006) have synthesized multi-channelled scaffolds with tunable properties (ie, channel diameter, wall porosity) composed of poly(D,L-lactic-co-glycolic acid) (PLGA), which were designed to enable the use and guidance of multiple cell types within a single scaffold in a spatially defined manner. Such studies have made it increasingly clear that a better understanding of cell–substrate interactions, as well as cell–cell interactions within 3D scaffolds, is required for the optimal design of biomaterial- and cell-based treatment strategies intended to promote functional repair.
CELL DELIVERY
Cell transplantation is a promising therapeutic strategy to replace dead or damaged tissue in the CNS (Figure 3). Three major challenges need to be overcome to deliver the promise of cell transplantation in regenerative medicine: (1) cell distribution; (2) cell survival/viability; and (3) host-tissue integration. The distribution of exogenously transplanted cells using saline or media is non-ideal, often resulting in aggregated cells (even before injection), thereby reducing cell survival. Cell viability upon transplantation into the host tissue is necessary to permit the transplanted cells to perform their desired functions, such as cytokine and growth factor secretion or cell–cell contact to promote tissue regeneration. Moreover, cells are not easily tracked and are often dispersed and removed by immune cells, disabling host-tissue integration. The inhospitable environment of the injured tissue at the lesion site and the lack of cell adhesion and cell survival factors further limit cell viability. Cell integration with the host tissue must be rapid, but is often limited by chemical and physical barriers. Hydrogels are promising cell delivery vehicles as they allow facile migration of cells and molecular transport of nutrients and oxygen (Orive et al, 2009; Pettikiriarachchi et al, 2010). Moreover, they provide a physical scaffold for the retention of cells at the injection site upon transplantation, thereby overcoming the problem of cell dispersion, and injectable hydrogels facilitate minimally invasive surgery. Taking advantage of the chemistry described in the previous section, the hydrogel can be designed to promote cell survival with the inclusion of pro-survival factors, or to mimic the cell’s ECM by incorporating specific chemical cues that direct stem cell fate upon transplantation. This section will focus on recent advances in hydrogel cell delivery vehicles into the brain, spinal cord, and retina in an effort to promote tissue and functional repair after injury or disease.
Cell delivery with or without biomaterials to (a) the injured brain, (b) the injured spinal cord and (c) the subretinal space of the retina between the photoreceptors (rods and cones) and the retinal pigmented epithelium (RPE). (b) Image copyright (2005) by Michael Corrin.
Brain
Early studies by Evans and Kaufman (1981) showed that NSPCs transplanted into dysmyelinated shiverer mice brains were able to differentiate into myelin basic protein-expressing oligodendrocytes, remyelinate host axons, and decrease tremors in some engrafted animals (Yandava et al, 1999). However, low cell survival and integration resulted in high variability in behavioral outcomes (Snyder and Park, 2002). Park et al (2002) showed that using a poly(glycolic acid) biopolymer as a delivery vehicle for NSPCs into hypoxia-ischemia-injured mouse brains promoted tissue regeneration by decreasing cavity volume, and enhancing neurite outgrowth and integration of transplanted cells.
Recently, the use of biomaterials that can interact with transplanted cells and the host tissue has been of significant interest. Hyaluronan is a naturally occurring polysaccharide found in the ECM of the central nervous system. It has anti-inflammatory properties, and can interact with various HA-receptors (such as CD44 and hyaluronan-mediated motility receptor) present on different cell types to promote cell adhesion and survival (Jiang et al, 2007). Zhong et al (2010) used a blend of HA, gelatin, and heparin to deliver NSPCs into stroke-injured mouse brains (see Figure 3a for a schematic representation of cell injections into the injured brain). They observed greater cell survival and attenuated host immune response in the graft site compared with cells delivered in suspension alone. The hydrogel acted as a barrier for infiltrating microglia/macrophages and prevented their migration into the graft (Zhong et al, 2010). Similarly, Kauer et al (2012) demonstrated that HA-based hydrogels, relative to phosphate buffered saline, increase the cell viability (approximately a three-fold increase from 20 to 60% after 28 days in vivo) of mouse NSPCs upon transplantation into mouse brains. These studies underline the benefits (eg, attenuating immune response and promoting cell viability) of using naturally occurring biopolymers as delivery vehicles.
Incorporating bioactive molecules into cell delivery vehicles has been explored to both improve cell survival via enhanced exogenous cell–substrate interactions and promote host-tissue neuroprotection and/or neuroregeneration. Cheng et al (2013) developed injectable hydrogels composed of self-assembling peptides for NSPC delivery: a hydrogel consisting of repeating units of the tetrapeptide, Arg–Ala–Asp–Ala, poly(RADA) with a C-terminal IKVAV sequence vs saline alone promoted greater tissue repair in the rat brain after a resection-type injury when used to deliver NSPCs. The inclusion of the IKVAV peptide sequence with poly(RADA) significantly increased the differentiation of transplanted NSPCs into neurons compared with poly(RADA) alone. Moreover, transplantation into the rat brain of NSPCs in fibrous poly(ɛ-caprolactone) (PCL) scaffolds immobilized with GDNF significantly enhanced NSPC survival, proliferation, and differentiation into neurons and oligodendrocytes in vivo relative to transplantation of NSPCs in the absence of PCL (Wang et al, 2012a).
Vascularization of a transplanted graft is another important consideration for integration into the host tissue. To this end, Bible et al (2012) encapsulated VEGF within PLGA biodegradable microparticles coated with fibronectin to enhance NSPC adhesion. The authors demonstrated that release of VEGF recruited host endothelial cells into the graft site, resulting in the formation of primitive neurovascular units in the graft site. Interestingly, Matsuse et al (2011) reported that co-delivery of bone marrow-derived MSCs dispersed in collagen sponges with basic fibroblast growth factor (bFGF)-releasing gelatin microspheres improved cell viability, distribution, angiogenesis, and motor recovery following ischemic stroke. Together, these studies demonstrate that biomaterials can increase cell viability after transplantation into the brain, an effect that can be even further increased by incorporating bioactive molecules.
Spinal Cord
Attempts to replace lost cells and create a growth-promoting environment following spinal cord injury have included transplantation into the lesion site of: stem cells, such as NSPCs (Pfeifer et al, 2006), ESCs (McDonald et al, 1999), and iPSCs (Tsuji et al, 2010), peripheral cells (Bunge and Pearse, 2003) such as Schwann cells (Li and Raisman, 1994) and olfactory ensheathing glia (Ramon-Cueto et al, 1998), and central glia, such as oligodendrocytes (Nistor et al, 2005) and astrocytes (Davies et al, 2006). Such cell-based strategies promote some functional improvements in experimental animal models of spinal cord injury, but their mechanism(s) of action remain poorly defined, particularly due to poor cell survival following transplantation (Bradbury and McMahon, 2006). Furthermore, transplanted stem/progenitor cells differentiated uncontrollably, leading to negative side effects, such as allodynia (ie, hypersensitivity to normally non-painful stimuli) (Hofstetter et al, 2005). Delivery of the cells within hydrogels aims to improve cell survival. By incorporating peptides and/or growth factors, cell survival and/or controlled differentiation of stem/progenitor cells can be achieved. Although the approaches may ultimately be used for neurodegenerative diseases of the spinal cord, such as amyotrophic lateral sclerosis, we will focus solely on traumatic spinal cord injury in this review.
Itosaka et al (2009) found that fibrin-based hydrogels used to transplant MSCs into acute hemisected rat spinal cord lesions improved the survival of the transplanted cells and promoted functional recovery compared with saline or single-cell injections 4 weeks after injury. Delivery of oligodendrocyte precursor cells in hydrogels composed of HA and gelatin, crosslinked with PEG, in a demyelination lesion model of the spinal cord resulted in axon remyelination (Li et al, 2013); however, identification of transplanted vs host cells was ambiguous, and thus the effect of the hydrogel on the survival of transplanted cells was unclear.
The co-delivery of stem cells with growth factors provides a strategy to control cell fate after transplantation. Johnson et al (2010a) transplanted mouse ESC-derived neural progenitor cells (ESC-derived NPCs) within fibrin scaffolds into a sub-acute, hemisected rat spinal cord lesion. The scaffolds were functionalized with heparin-binding peptides, which bind heparin and subsequently heparin-binding proteins (ie, PDGF-AA and NT-3) (Johnson et al, 2010b). The co-delivery of growth factors with ESC-NPCs significantly improved cell viability and neuronal differentiation after 2 weeks. However, by 8 weeks, the transplanted stem cells had formed tumors, clearly demonstrating the need for transplantation of defined and purified cell populations. An injectable hydrogel composed of HA and methyl cellulose (HAMC, which was first described by Gupta et al (2006), was used to successfully deliver both human umbilical derived stem cells and rat NSPCs into clip-compression injured rat spinal cords (Figure 3b) (Caicco et al, 2013b; Mothe et al, 2013). To promote the differentiation of transplanted rat NSPCs into oligodendrocytes, HAMC was functionalized with recombinant PDGF-A (Tam et al, 2012). Sub-acute transplantation of NSPCs in PDGF-functionalized HAMC into spinal cord injured rats, relative to conventional media controls, showed improved functional recovery on the ladder walk test, and increased host oligodendrocytes and host neurons. Furthermore, the combination of NSPCs and PDGF-A functionalized HAMC promoted the tissue sparing around the lesion site and a reduction in lesion volume (Mothe et al, 2013).
Synthetic hydrogels, such as poly(2-hydroxypropyl methacrylamide) (PHPMA) functionalized with RGD, have also been investigated for MSC transplantation into the chronic balloon compression injured spinal cord (Hejcl et al, 2010). Animals received implants 5 weeks after injury, and some cells were present within the hydrogel after 6 months. Animals that had PHPMA/RGD+MSC transplants showed greater behavioral functional repair compared with animals with injury alone, but not relative to animals that had hydrogel implants alone, obscuring the benefit of the MSCs. The tissue benefits observed in animals transplanted with the PHPMA/RGD+MSCs included: reduced tissue atrophy, migration of astrocytes and Schwann cells into the scaffold, accompanied by axons, and angiogenesis. Other synthetic hydrogels, such as poly(N-isopropylacrylamide)-g-PEG (PNIPAAm-g-PEG) and poly(N-isopropylacrylamide)-g-methylcellulose (PNIPAAm-g-MC) branched copolymers have also been transplanted in hemisection models of spinal cord injury (Conova et al, 2011). The authors investigated short survival times (1 and 2 weeks) after acute injections and demonstrated that the hydrogels did not contribute to the inflammatory response, the glial scar or demyelination, and were permissive to axonal growth when supplemented with BDNF. Although transplanted fibroblasts survived when transplanted within PNIPAAm-g-PEG, neither a detailed analysis nor comparison with cell injections without the hydrogel was included. Thus, natural and synthetic polymers, particularly when conjugated to other bioactive molecules, can function as effective cell delivery vehicles into the injured spinal cord.
Hydrogels with unique architectures, such as self-assembling peptide nanofiber scaffolds (SAPNS), have promoted repair in spinal cord lesions (Tysseling-Mattiace et al, 2008). The structure of the nanofibers facilitated neurite guidance across the lesion site (Zhan et al, 2013). SAPNS were used to transplant Schwann cells and NSPCs into acute lesions of dorsal column transections of the spinal cord (Guo et al, 2007). Both the cell types survived up to 6 weeks after transplantation, the longest time point investigated. The combination of hydrogel with Schwann cells promoted the greatest axonal ingrowth of motor and sensory neurons. Furthermore, host cells infiltrated and blood vessels extended into the scaffold. Therefore, cell- and axon guidance in the injured spinal cord can be achieved by controlling the topology of biomaterials.
Interestingly, pre-differentiation of NSPCs to neurons was shown to enhance cell survival and functional repair after transplantation in a full transection spinal cord injury rat model relative to animals receiving in situ differentiated NSPCs (Kim et al, 2011a). Cells were transplanted using fibrin-filled chitosan hydrogel guidance channels that matched the modulus of spinal cord tissue (Freier et al, 2005). NSPCs that had been pre-differentiated to neurons with dibutyryl cyclic AMP (dbcAMP) before transplantation survived significantly (by 80%) better than cells that were differentiated in situ, by local, sustained release of dbcAMP. Moreover, synapse formation and behavioral repair were evident only in animals transplanted with dbcAMP pre-differentiated neural cells. These studies demonstrate the importance of the differentiated progeny coupled with the biomaterial for greater survival of transplanted cells.
Retina
The first cell transplantation experiment in the eye was performed in the late 1950s, when Royo and Quay (1959) isolated a whole retinal sheet from a dog fetus, and implanted it in the anterior chamber of the mother’s eye. Numerous subsequent studies have since transplanted cells into the retina in an attempt to regenerate damaged photoreceptors (Gouras et al, 1984; Gouras et al, 1985; Li and Turner, 1988). However, it was later realized that cell transplantation in solution suffered from significant drawbacks such as cell reflux from the injection site, cell aggregation, cell death, and lack of integration into the host tissue (MacLaren et al, 2006; Wongpichedchai et al, 1992). Interestingly, retinal pigmented epithelia (RPE) and whole-fetal retinal cells that were transplanted as a sheet survived better than cell suspensions (Seiler and Aramant, 1998, 2012; Turner et al, 1988) as the continuous adherence to their matrix protected them from anchorage-dependent cell death, known as anoikis (Taddei et al, 2012). In addition, cell polarity was maintained, and greater immune tolerance was observed compared with cells transplanted in suspension (Ghosh et al, 2008; Wenkel and Streilein, 2000). Transplanting cells with biomaterials, in a defined cellular microenvironment, is advantageous for graft-cell survival and integration. Materials provide an adhesion surface for the cells, and afford more uniform cell distribution, thereby decreasing cell aggregation (Ballios et al, 2010). They can also be used as vehicles for the incorporation of additional chemical factors that can enhance cell survival, differentiation, and integration.
Early studies of cell transplantation into the retina focused on biomaterial biocompatibility. Bhatt et al (1994) reported no gross evidence of rejection using sheets of collagen I to transplant human RPE into the rabbit subretinal space. Moreover, transplantation of biodegradable gelatin membranes containing neural retina sheets into the eyes of rabbits did not elicit an inflammatory response (Hsiue et al, 2002). Degradation of the biomaterial was also investigated in order to prevent persistent retinal detachment at the transplantation site, which could lead to complications such as photoreceptor degeneration, gliosis, and proliferative vitreoretinopathy (Lewis and Fisher, 2003; Lo et al, 2011; Pastor et al, 2002). These early reports demonstrated the feasibility of biomaterials for cell transplantation into the retina.
The mechanical properties of biomaterials used for cell transplantation are key to ensure minimal retinal tissue damage after transplantation. For example, Lavik et al (2005) demonstrated that scaffolds composed of a blend of PLGA and poly(lactic acid) (PLA), prepared via solid–liquid phase separation, resulted in reduced elastic modulus and increased maximum strain at failure compared with PLA alone (Lavik et al, 2005). The reduced elasticity of the scaffolds means that they are more compliant to the sensitive retinal tissue (ie, the scaffolds can more readily alter their conformation to match the structure of the retina), and thus reduces the physical damage to the retina upon transplantation. In addition, the increased maximum strain at failure means that the scaffolds are less likely to break during the transplantation procedure. Mouse retinal progenitor cells (RPCs) were efficiently and uniformly dispersed along the surface of PLGA/PLA scaffolds. RPCs adhered to the scaffolds, differentiated into Müller glia, and were implanted into the rat subretinal space. However, no evidence of photoreceptor or other neuronal differentiation is shown, which would have been preferable for transplantation into animal models of retinal degeneration. Müller glia transplantation has not been shown to have a regenerative effect in the retina, and usually impedes transplanted cell integration in the retina (West et al, 2008). Thus, the authors suggest that future studies should also utilize chemical cues delivered in these PLGA/PLA scaffolds to promote differentiation into functional photoreceptors. Using the PLGA/PLA scaffolds, ∼50% of transplanted cells were estimated to be alive after 14 days, which is significantly greater than that achieved by bolus injections, where typically ∼1–2% of cells survive (MacLaren et al, 2006); however, a direct comparison is difficult because different cells were delivered in these two studies (Lavik et al, 2005; MacLaren et al, 2006). Importantly, a subsequent study demonstrated that biomaterials increase cell survival after retinal transplantation compared with bolus injections (Tomita et al, 2005a). Transplantation of RPCs into the subretinal space with laminin-coated PLGA-PLA scaffolds promoted a 10-fold increase in cell survival over bolus injection. At 2 and 4 weeks after transplantation, RPC differentiation was observed, as evidenced by the expression of neurofilament 200 (NF-200, a neuronal marker), PKC-α (a bipolar cell marker), recoverin and rhodopsin (photoreceptor markers). Some cell migration into the retinal layers was also observed. Probing the mechanism of increased survival conferred by the biomaterial, the authors showed that EGF, which is used in the culture medium of the RPCs, had adsorbed to the biomaterial and may have contributed to the increased survival observed in the biomaterial group. An advantage of this particular approach is that the biomaterial allows for more precise control over the placement of the transplanted cells in the host tissue such that it can be positioned at the site of the degenerated area (for example, in the macula for AMD patients). A potential caveat is that although PLGA-PLA scaffolds promote cell survival and differentiation upon transplantation, the implantation surgery is highly invasive and the biomaterial, although degradable, is still present after 4 weeks, and thus may lead to retinal detachment. Even though the molar mass and shape of the biomaterial and implantation site influence its degradation rate, PLGA is known to be a slowly-degrading material within the eye. For example, PLGA microspheres have been detected in the eye 6 months after transplantation (Giordano et al, 1995). These studies demonstrated that cells transplanted with biomaterials showed increased cell survival and integration into the retina; however, there were still shortcomings that needed to be overcome.
A significant obstacle to promoting functional recovery following cell transplantation is the successful migration of cells out of the biomaterial and integration into the host tissue. To enhance cell migration out of the biomaterial, Tucker et al (2010) transplanted RPCs using a scaffold consisting of PLGA encapsulated with matrix metalloproteinase-2 (MMP2). MMP2 is known to degrade neurocan, a CSPG, and CD44, a hyaluronan-binding protein (Zhang et al, 2007b). Neurocan and CD44 can form fibrous networks in the degenerating retina (and in other CNS regions), and have been shown to impede neurite outgrowth, ultimately causing cell death (Chaitin and Brun-Zinkernagel, 1998; Inatani et al, 2000; Krishnamoorthy et al, 2000; Moon et al, 2003). RPCs that were delivered from PLGA-MMP2 scaffolds exhibited greater migration into the host outer nuclear layer of the retina compared to PLGA-bovine serum albumin (BSA) scaffolds. Furthermore, the migrating RPCs differentiated into photoreceptors as determined by the expression of the photoreceptor markers recoverin or rhodopsin. Importantly, the presence of MMPs did not negatively affect retinal morphology. This study shows that functionalization of biomaterials with factors that neutralize inhibitory clues of the host microenvironment can improve the integration of RPCs into the retina.
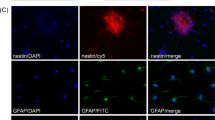
Another technique to promote the survival, migration, and integration of transplanted RPCs into the retina was developed by Tao et al (2007), who used microelectromechanical system technology to create ultrathin (6 μm) poly(methyl methacrylate) (PMMA) sheets with or without pores of defined sizes. The survival and proliferation of murine RPCs cultured on porous and non-porous PMMA sheets in vitro were comparable to cells cultured on tissue culture polystyrene. Interestingly, RPC transplantation with porous PMMA sheets into the mouse subretinal space demonstrated significantly more surviving cells after 4 weeks compared with non-porous PMMA sheets. The difference was hypothesized to be due to an inferior retention of the RPCs in the non-porous PMMA during the transplantation process, leading to increased cell reflux. Substantive cell migration into the host retina was also observed with the porous scaffolds; migrated donor cells expressed glial fibrillary acidic protein (GFAP), NF-200, or recoverin as evidence of differentiation towards Müller glia, neurons, and photoreceptors, respectively. The retinal detachment created during transplantation appeared to resolve itself within 4 days, possibly due to the thin, porous material used; however, although PMMA is biocompatible and has been used as a lens replacement for many years (DeVore, 1991), it is a stiff, non-degradable material (Yamanaka et al, 1985). Therefore, it would either ultimately require a second surgery for its removal or, if left within the eye indefinitely, would likely result in a long-term immune response or other complications associated with the intraocular use of PMMA (Amon and Menapace, 1994; Rowe et al, 2004; Tognetto et al, 2003).
The use of materials that cause the least amount of damage to the eye during the transplantation procedure is a significant consideration, and has led to the development of injectable biomaterials. All of the aforementioned materials were transplanted in the subretinal space through a 5-mm scleral incision, using forceps, which entails significant trauma to the eye. In an effort to resolve this issue, Redenti et al (2009) used microfabricated poly(glycerol sebacate) (PGS) scaffolds that were 45 μm thick with 50 μm diameter pores, and coated them with laminin. Mouse RPCs cultured on PGS showed increased adhesion and proliferation compared with those cultured on glass. This highly elastic material was injected through a 25-gauge needle, requiring only a 1–2 mm scleral incision. (see Figure 3c for a schematic representation of subretinal injections). PGS is biocompatible and degrades within ∼1 month after subretinal transplantation. Subretinal transplantation of mouse RPCs in PGS showed that mouse RPCs migrated into the inner and outer nuclear layers of the host retina, with few differentiating into photoreceptor and bipolar cells; however, the efficacy of this matrix for cell delivery in vivo is unclear, as no control group consisting of cells in the absence of PGS was included. Interestingly, Ballios et al (2010) studied the injectable HAMC hydrogel for RSC transplantation, first showing its benefit in vitro and then in vivo. Importantly, the HAMC hydrogel was injected through an even finer (than the PGS scaffold), 34 gauge needle with fast gelation after injection. An in vivo degradation assay in the subretinal space demonstrated resorption of the gel after 7 days, thereby minimizing risks of adverse retinal detachment while maximizing cell migration and host-tissue integration. After subretinal injection in mice, RPCs delivered in HAMC were evenly distributed along the Bruch’s membrane, whereas RPCs delivered in conventional saline controls were aggregated. Importantly, the retinal architecture was not affected by the hydrogel injection. Together these data demonstrate that this is a compelling biomaterial for cell delivery to the retina while obviating the complicated surgery associated with transplanting biomaterial sheets.
BIOMOLECULE DELIVERY TO THE CNS VIA HYDROGEL AND NP VEHICLES
Delivery of bioactive molecules to the CNS is currently being pursued to promote neuroprotection and plasticity, modulate the inflammatory response, and stimulate endogenous stem cells to proliferate and migrate to the injured tissue (Figure 4) (Dibajnia and Morshead, 2013). However, CNS treatment is challenging as many CNS disorders are characterized by a multifactorial pathophysiology (ie, expression of growth inhibitory molecules, genetic alterations, inflammation, altered immunoresponse, excitotoxicity, and oxidative stress) making successful single drug development difficult (Rossi et al, 2013). Furthermore, delivery of therapeutics into the CNS is limited by the low permeability of the blood–brain/spinal cord barrier to many of these molecules (Groothuis, 2000; Pardridge, 2012). Efforts to overcome this issue have included using high doses of therapeutics delivered to the intrathecal space of the spinal cord by either bolus injection or prolonged infusion with osmotic minipumps. These techniques are non-ideal, resulting in either uneven, short-lived exposure to the delivered drug (with bolus) or possible infection/blockage (with external minipump/catheter systems). Intraventricular injections into the brain bypass the BBB, but are highly invasive and result in significant tissue damage with cannula insertion through brain tissue. More recent strategies involve chemical or electromagnetic disruption of the barrier coupled with functionalized NPs or liposomes that have limited capacity to cross the blood–brain/spinal cord barrier (Rossi et al, 2013).
Schematics of hydrogel-based drug delivery system to (a) the injured brain, and (b) the injured spinal cord. (a) The drug-containing hydrogel (HAMC) is placed on top of the cortex, permitting diffusion into the brain. The black arrows in the horizontal cross-section indicate diffusion in all directions. (b) Hydrogel injection into the space between the spinal cord and the dura mater, termed intrathecal space. Fast gelling hydrogels enable local release at the injection site. Figures adapted with permission from (a) Cooke et al (2011); copyright 2011 Elsevier. (b) Image copyright (2005) by Michael Corrin.
Biomaterials as drug delivery systems can offer localized and sustained delivery. Furthermore, they provide a physical scaffold or depot for sustained release while at the same time protecting the therapeutic biomolecule from degradation in vivo. The properties of these biomaterials can be altered to tune the release rate of the biomolecule into the target tissue. Prolonged release is important because it obviates the need for multiple injections to sustain a constant dosage. This section will highlight some of the recent advances using biomaterials to deliver therapeutic molecules to the brain and spinal cord.
Brain
Several growth factors have been shown to promote the proliferation (Erlandsson et al, 2011; Popa-Wagner et al, 2010; Sun et al, 2003; Teramoto et al, 2003; Tureyen et al, 2005), migration (Kolb et al, 2007; Ohab et al, 2006; Schabitz et al, 2007), and differentiation (Kolb et al, 2007; Popa-Wagner et al, 2010; Schabitz et al, 2007) of endogenous stem cells, and improve functional recovery (Erlandsson et al, 2011; Kolb et al, 2007; Ohab et al, 2006; Popa-Wagner et al, 2010) in experimental animal models. However, some of these studies used either invasive delivery techniques such as intraventricular injections, which can lead to further damage, or systemic injection, which can result in off-target, cytotoxic or non-specific effects due to the very high dosage required to cross the BBB before systemic degradation and circulation.
Efforts to increase the bioavailability of drugs delivered into the brain via systemic delivery have resulted in the use of various drug carriers, such as polymeric NPs, which are described in detail elsewhere (Orive et al, 2009). Polymeric NPs comprise natural or synthetic polymers (eg, PLA and PLGA) and are between 10–1000 nm in diameter. These particles enhance drug circulation and can be designed to target and cross (to a limited extent) the BBB following systemic injection. Liu et al (2013a, 2013b) recently reported the use of PEG-PLA NPs to deliver the neuroprotective peptide NAP (NAPVSIPQ) into the brain via tail-vein or intranasal injections. To promote NAP transport across the BBB, the authors covalently conjugated a transferrin-mimetic peptide (B6: CGHKAKGPRK) (Liu et al, 2013a) or lactoferrin (Liu et al, 2013b), a glycoprotein in the transferrin family, to PEG-PLA NPs. Transferrin receptors are located on the surface of endothelial cells of the BBB and are involved in receptor-mediated transcytosis to transport bound-ligands across the BBB. Tail-vein injections of these NPs resulted in greater accumulation of the B6-PEG-PLA and lactoferrin-PEG-PLA NPs in the brain compared with PEG-PLA NPs alone. Behavioral experiments (Morris water maze) showed that animals treated with NAP-laden B6-PEG-PLA or lactoferrin-PEG-PLA NPs preserved hippocampal function in animal models of Alzheimer’s disease. These studies show that systemic delivery of therapeutic molecules can be used to permeate the BBB and preserve functional benefits using the appropriately designed carriers.
Nakaguchi et al (2012) recently reported local delivery of insulin-like growth factor-1 and hepatocyte growth factor using gelatin microspheres to promote proliferation and neuronal differentiation of endogenous brain NSPCs (Nakaguchi et al, 2012). The microspheres were injected into the striatum of mouse brains to reach the NSPC niche in the subventricular zone (SVZ). Increased neurogenesis (defined by the number of doublecortin-positive (DCX+) cells) was observed with growth factor releasing microspheres relative to vehicle controls 7 days post-injection.
An alternative strategy for drug delivery to the NSPC niche was developed by Cooke et al (2011), who demonstrated that epi-cortical implants of EGF-containing HAMC hydrogels (Figure 4a) can provide sustained delivery to the SVZ. Furthermore, Cooke et al (2011) and Wang et al (2012b) reported deep brain tissue penetration of two factors, EGF and EPO, respectively, previously shown to stimulate endogenous stem cells and promote tissue repair in an animal model of stroke (Kolb et al, 2007). Interestingly, chemical modification of EGF with PEG enhanced its tissue penetration depth, while preserving its bioactivity, relative to EGF alone (Cooke et al, 2011). EGF-PEG induced significantly more Ki67+ proliferating cells than EGF or vehicle controls. EPO, similarly delivered from the epi-cortically-placed HAMC hydrogel, was also shown to stimulate the migration of DCX+ neuroblasts from the SVZ. Another molecule that has been shown to promote neurogenesis following stroke in animal models is cyclosporine A (CsA) (Erlandsson et al, 2011). Recently, Caicco et al (2013a) demonstrated sustained local release of CsA to the brain using epi-cortical implants of CsA encapsulated in PLGA microspheres dispersed in HAMC. CsA was shown to be released for 25 days into the brain and to reach the NSPC niche in the SVZ, which is key to stimulating neurogenesis of endogenous NSPCs (Caicco et al, 2013a; Erlandsson et al, 2011). Together, these studies show that therapeutic molecules can be delivered into the brain using an epi-cortical delivery approach, thereby circumventing the BBB and invasive injections.
Regeneration of injured tissue is critical to functional recovery and this is enhanced by re-vascularization. To enhance angiogenesis, Zhang et al (2007a) encapsulated VEGF165 in poly(dimethylsiloxane–tetraethoxysilane) (PDMS-TEOS) that was then injected into a brain cavity. The PDMS-TEOS biomaterial filled the brain cavity and restored the brain shape compared with the distorted shape that remained without biomaterial injection. Furthermore, delivery of VEGF165 significantly increased the number of endothelial cells and astrocytes in the scaffold compared with delivery of PDMS-TEOS alone (Zhang et al, 2007a). Alginate hydrogels used to deliver VEGF165 into stroke-injured rat brains also resulted in significant improvement in locomotor activity compared with vehicle controls (Emerich et al, 2010). Interestingly, sustained VEGF165 release resulted in significantly better behavioral recovery and reduced lesion volume compared with bolus delivery of VEGF165, thereby demonstrating the beneficial effects of sustained delivery strategies.
Spinal Cord
Intrathecal delivery via minipumps has been used as an alternative to systemic and oral administration. Unfortunately, direct injections into the CSF show only a poor distribution of the drug into the spinal cord parenchyma (Rossi et al, 2013). Furthermore, possible side effects include obstruction, leakage, breakage and dislodgment of the catheter, hemorrhage, CSF leaks and infections (Belverud et al, 2008). More recently, NPs and hydrogels have been investigated as an alternative way to deliver drugs to the injured spinal cord. NPs typically have a short half-life in vivo, and are often coated with PEG to increase their half-life in the bloodstream and prevent macrophage uptake. They have been used to deliver methylprednisolone (Kim et al, 2009), prostaglandin E1 (Takenaga et al, 2010), and mixtures of different neurotrophic factors (BDNF, GDNF, NGF, CNTF, and other peptide fragments) (Menon et al, 2012) to the injured spinal cord. However, injected NPs often leave the zone of injection as they are not confined by any support, and easily extravasate into the circulatory system, where they are distributed all over the body, including the liver and spleen (Kim et al, 2009). Therefore, local delivery of drugs/biomolecules with hydrogels (Figure 4b) or NPs dispersed in hydrogels have been suggested to provide a targeted therapy that is able to maximize the efficacy of bioactive agents while minimizing their side effects.
Localized drug delivery into the injured spinal cord using biomaterials has focused significantly on axonal regeneration to promote motor function repair. One of the earliest studies investigating the potential of combinations of hydrogels and bioactive molecules was done by Goldsmith and de la Torre (1992) where collagen scaffolds were supplemented with 4-aminopyridine (a potassium channel blocker), laminin, beta-glia maturation factor, or omental lipid angiogenic factor. Implantation of these hydrogels into completely transected spinal cords of cats promoted the growth of dense bundles of neurites into the collagen matrix and into the distal spinal cord. These fibers showed a maximal outgrowth of 90 mm below the transection site upon addition of 4-aminopyridine into the collagen matrix. Unfortunately behavioral analysis was not included in this investigation.
Jain et al (2006) used agarose gels and lipid microtubes to deliver BDNF to dorsal hemisection injuries of the spinal cord. BDNF reduced both the reactivity of astrocytes and the production of CSPGs at the lesion site, leading to more regenerating fibers entering the implanted hydrogel at 6 weeks after injury. However, the functional benefits of this strategy were not described and the complications associated with having to cool the agarose solution during its delivery make this strategy impractical. NT-3, in the same neurotrophic family as BDNF, was delivered via PLA-PEG hydrogels to dorsal hemisection injuries, and detected at the lesion site for up to 14 days (Piantino et al, 2006). Remarkably, NT-3-treated animals showed greater axonal regeneration and improved functional recovery relative to vehicle controls. Taylor et al (2006) also delivered NT-3, but into a suction ablation model of spinal cord injury, using fibrin hydrogels with a heparin binding system (Johnson et al, 2010b). They observed greater axonal ingrowth into the lesion compared with control scaffolds (without NT-3) 9 days after injury. Furthermore, reduced GFAP immunoreactivity was detected at the white matter border of the lesion with fibrin scaffolds compared with saline injections. However, animals treated with or without fibrin scaffolds and NT-3 did not show functional improvement over saline controls.
Experimental treatment strategies to promote neuroprotection and tissue sparing aim to reduce the loss of cells at and around the lesion site. Jimenez Hamann et al (2005) injected concentrated collagen solutions into the intrathecal space to deliver EGF and bFGF to the spinal cord after clip compression injury. They observed that EGF diffused deep into the tissue, but the signal was lost after 7 days, whereas bFGF could still be detected adjacent to the hydrogel after 7 days. After 56 days, collagen solutions containing EGF and bFGF improved white matter sparing and showed the lowest cavitational volume and the greatest ependymal cell proliferation relative to controls; despite these promising results, no functional benefits were observed.
The inflammatory response after spinal cord injury is thought to have beneficial and detrimental properties, depending on the type, severity, and time after injury (Chan, 2008; Kwon et al, 2004). Several studies have demonstrated that both inhibition and promotion of the inflammatory response can have beneficial effects (Ghirnikar et al, 2000; Hauben et al, 2000; Rapalino et al, 1998; Wamil et al, 1998). Kang et al (2010) delivered minocycline, an antibiotic, to lateral hemisection injuries via tetronic-oligolactide hydrogels. The implantation of the hydrogel alone allowed blood vessel formation in the lesion cavities, and in combination with minocycline, macrophage infiltration, and CSPG deposition decreased while axon growth through the lesion area increased in a dose-dependent manner 7 weeks after injury. As no behavioral analysis was reported, it is not clear whether this strategy results in functional improvements.
The two most prominent and extensively investigated regenerative agents are chondroitinase ABC (ChABC), which has been shown to degrade the growth inhibitory CSPGs at the glial scar, and anti-NOGO antibodies, which neutralize the myelin-associated inhibitory molecule NOGO-A (Chen et al, 2000; Zuo et al, 1998). ChABC is relatively unstable at 37 °C (Tester et al, 2007) and requires sustained local delivery to the spinal cord for efficacy. Thus, hydrogel-based delivery systems must not only achieve desirable sustained release profiles, but also protect ChABC against enzymatic and hydrolytic degradation in vivo.
Agarose microtubes were used to deliver ChABC to dorsally hemisected spinal cords (Lee et al, 2010). ChABC was stabilized with trehalose in the formulation to retain its biological activity. Thermostabilized ChABC remained active at 37 °C in vitro for up to 4 weeks using a non-quantitative bioassay. The delivery system reduced CSPG levels at the injury site for up to 6 weeks post-SCI with delivery of the thermostabilized ChABC. Co-delivery of NT-3 with ChABC promoted axonal regeneration and demonstrated some functional benefit at 6 weeks after injury compared with animals receiving agarose gels without NT-3 (Lee et al, 2010). In a separate study, Hyatt et al (2010) used pre-gelled fibrin hydrogels to stabilize and deliver ChABC to dorsal transection injuries. Compared with simple intraspinal injections of ChABC, the fibrin delivery system contained more bioactive ChABC at the lesion site (as determined by zymography) at 3 weeks after injury and led to a 37% reduction of CSPGs. Recently, an affinity-based controlled release system was designed for ChABC where bioactive release was quantified over a 7-day period (Pakulska et al, 2013). These studies demonstrate that biomaterials are able to stabilize ChABC in vivo and maintain its bioactivity for a longer period of time compared with simple injections.
Antibodies against the myelin inhibitory molecule NOGO-A (ie, anti-NOGO-A) have been shown to improve functional recovery in experimental animal models when delivered by an intrathecal catheter (Freund et al, 2006; Liebscher et al, 2005) and have been studied in a phase I clinical trial (Hawryluk et al, 2008). To achieve sustained release, anti-NOGO-A is typically delivered by osmotic minipumps; however, as external minipumps are susceptible to infection, patients enrolled in the clinical trial received repeated injections of anti-NOGO-A into the intrathecal space. In a complimentary approach, the delivery of an antibody that acts as a competitive antagonist for the native receptor of NOGO-A (NOGO-66 receptor, NgR) has also been reported to promote axonal regeneration (Wei et al, 2010), as activation of NgR by NOGO-A inhibits neurite outgrowth (Domeniconi et al, 2002; Liu et al, 2002). To avoid multiple injections, Wei et al (2010) immobilized NgR antibodies (anti-NgR) to HA-poly(L-lysine) hydrogels, which were directly implanted after lateral hemisection of the spinal cord (Wei et al, 2010). Anti-NgR diffusion out of the hydrogel was slow and immunohistochemical analysis showed that most of the NgR antibodies were still present within the scaffold 2 weeks after implantation, thereby competitively inhibiting NgR from activation with NOGO-A. However, at 4 weeks, more antibody diffused out of the hydrogel and was detected within the tissue; anti-NgR was still detected in the tissue at 8 weeks, albeit in lower concentrations. The antibodies had no effect on angiogenesis, and blood vessels were found in both hydrogel-antibody and hydrogel vehicle control groups within the lesion site. Both groups showed decreased GFAP immunoreactivity compared with untreated controls, likely due to the anti-inflammatory effects of hyaluronan. Anti-NgR delivery promoted greater axonal regeneration compared with untreated controls, suggesting that the sustained diffusion of anti-NgR from HA hydrogels is a promising strategy to promote regeneration of the injured spinal cord. The challenge of this study is translation to the patient as the hemi-section model is not as clinically relevant as compression models.
FUTURE RESEARCH DIRECTIONS
The use of hydrogels, and especially injectable hydrogels, for local and controlled drug and cell delivery to the CNS is a new and rapidly expanding discipline in the field of regenerative medicine. The injectability and resorbability of the hydrogel obviate the need for both invasive surgical procedures associated with transplants and removal of non-degradable materials. Yet, there is no magic bullet for the treatment of CNS disorders, requiring a combined strategy of biomaterial, cell and biomolecule to achieve therapeutic benefit. The resulting clinical translation of such combination strategies will be inherently more complicated; however, there is precedence in other diseases such as the use of drug eluting stents for occluded blood vessels or antibody–drug conjugates for cancer treatment.
Future hydrogels must provide a delivery system for both sustained biomolecule and cell delivery. Although conceptually attractive, cell transplantation often suffers from low cell survival (Cooke et al, 2010). Whether in an immunoprotective barrier (Cheung and Anseth, 2006; Su et al, 2010) or an injectable hydrogel, cell survival and integration remain key challenges to the field. Both the biomaterial design and the differentiated cell progeny will influence cell survival and integration. These factors are intimately related as cells need to survive sufficiently long to integrate and at the same time they need to integrate with the host tissue to survive. Thus, host-tissue integration has to occur rapidly after transplantation. This can be promoted with angiogenesis or by overcoming the chemical or physical barriers to cell integration, such as the glial scar, which forms after CNS injury. Each injury type will require a specific, optimized delivery system, with different cell–biomolecule combinations.
Diffusion of bioactive substances is largely dependent on the physical properties of molecule. Modification of EGF with PEG (Cooke et al, 2011) has previously been shown to increase its depth of penetration in rodent brains; however, the challenge is to demonstrate that biomolecules can penetrate sufficiently deep into the brain of larger animals after intrathecal or epi-cortical delivery. Furthermore, prolonged exposure of certain molecules may be problematic as this may result in the over-proliferation of normal cells. This illustrates the need to precisely control the kinetics of drug release from polymers, whereby a potential strategy would be to fine tune the interaction between the drug and the biomaterial, such as by using protein binding partners with varying binding affinities to conjugate the drug to the biomaterial (Vulic and Shoichet, 2012). Other disadvantages of current hydrogel delivery systems include the low loading capacity for hydrophobic drugs and the difficulties in controlling the diffusion of small molecules that have low steric hindrances (Perale et al, 2012). This can be overcome by either derivatizing drugs with a hydrophilic molecule, such as PEG, or encapsulation in polymeric NPs. The latter approach has also been used to prolong the delivery of protein therapeutics; however, the encapsulation process itself can degrade the protein and the amount of protein/polymer delivered is usually less than 5–10%, resulting in more polymer than therapeutic being delivered.
An appropriate cytoarchitecture may be required for optimal cellular response, but this will inherently complicate the surgical procedure. In addition to chemical and cellular strategies of regeneration, combination strategies with rehabilitation and enriched environment will pave the way of the future, taking advantage of multiple stimuli to regenerate the brain. There is already some evidence of this potential (Garcia-Alias et al, 2009; MacLellan et al, 2011), which will be expanded upon in the future.
With defined 3D culture systems, where the mechanical, chemical, and biological milieu is controlled, our understanding of the stem cell niche and disease progression will be enhanced and this knowledge should lead to better defined hydrogels for greater success in vivo in the future. Research into the development of dynamic, ‘smart’ materials that can respond to changes in external stimuli such as pH, temperature, and the presence of specific ligands (de Las Heras Alarcon et al, 2005; Han et al, 2013) is growing, and these new materials provide exciting possibilities to not only study the dynamic nature of cell–cell and cell–matrix interactions, but also for use as stimuli-sensitive drug delivery vehicles. (Roy et al, 2010)
Although biomaterials demonstrated beneficial effects in experimental animal models, new biotechnological- and/or chemical processes may need to be developed before clinical translation. For example, the purification of biomaterials is imperative for safe use in human patients, therefore requiring them to be rigorously tested and void of cytotoxic components (eg, endotoxins and toxic reagents used during chemical modifications) (Rietschel et al, 1994). In addition, biomaterials that have undergone chemical modifications (eg, conjugation of bioactive molecules) may require different chemical procedures to produce large quantities of biomaterials and bioactive molecules, as the same chemistry used for small-scale synthesis may be impractical for large-scale production (Milne, 2011; Ranjan et al, 2012). Nonetheless, the ability to create reproducible and well-defined biomaterial systems for delivery of therapeutic biomolecules and cells into the CNS in a non-invasive manner should advance translational applications to the clinic.
FUNDING AND DISCLOSURE
The authors acknowledge that a composition of matter patent has been issued for HAMC and additional patents are under review for cell and drug delivery with HAMC.
References
Aizawa Y, Leipzig N, Zahir T, Shoichet M (2008). The effect of immobilized platelet derived growth factor AA on neural stem/progenitor cell differentiation on cell-adhesive hydrogels. Biomaterials 29: 4676–4683.
Aizawa Y, Shoichet MS (2012). The role of endothelial cells in the retinal stem and progenitor cell niche within a 3D engineered hydrogel matrix. Biomaterials 33: 5198–5205.
Aizawa Y, Wylie R, Shoichet M (2010). Endothelial cell guidance in 3D patterned scaffolds. Adv Mater 22: 4831-+.
Amon M, Menapace R (1994). In-vivo documentation of cellular reactions on lens surfaces for assessing the biocompatibility of different intraocular implants. Eye 8: 649–656.
Azagarsamy MA, Anseth KS (2013). Bioorthogonal click chemistry: an indispensable tool to create multifaceted cell culture scaffolds. ACS Macro Lett 2: 5–9.
Ballios BG, Cooke MJ, van der Kooy D, Shoichet MS (2010). A hydrogel-based stem cell delivery system to treat retinal degenerative diseases. Biomaterials 31: 2555–2564.
Bang OY, Lee JS, Lee PH, Lee G (2005). Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol 57: 874–882.
Becker AJ, Mc CE, Till JE (1963). Cytological demonstration of the clonal nature of spleen colonies derived from transplanted mouse marrow cells. Nature 197: 452–454.
Beer JH, Springer KT, Coller BS (1992). Immobilized Arg-Gly-Asp (RGD) peptides of varying lengths as structural probes of the platelet glycoprotein IIb/IIIa receptor. Blood 79: 117–128.
Belverud S, Mogilner A, Schulder M (2008). Intrathecal pumps. Neurotherapeutics 5: 114–122.
Bhatt NS, Newsome DA, Fenech T, Hessburg TP, Diamond JG, Miceli MV et al (1994). Experimental transplantation of human retinal-pigment epithelial-cells on collagen substrates. Am J Ophthalmol 117: 214–221.
Bible E, Qutachi O, Chau DY, Alexander MR, Shakesheff KM, Modo M (2012). Neo-vascularization of the stroke cavity by implantation of human neural stem cells on VEGF-releasing PLGA microparticles. Biomaterials 33: 7435–7446.
Bliss TM, Andres RH, Steinberg GK (2010). Optimizing the success of cell transplantation therapy for stroke. Neurobiol Disease 37: 275–283 Detailed review of cell transplantation strategies in the stroke-injured brain.
Bockelmann J, Klinkhammer K, von Holst A, Seiler N, Faissner A, Brook GA et al (2011). Functionalization of electrospun poly(epsilon-caprolactone) fibers with the extracellular matrix-derived peptide GRGDS improves guidance of schwann cell migration and axonal growth. Tissue Eng A 17: 475–486.
Bongso A, Richards M (2004). History and perspective of stem cell research. Best Pract Res Clin Obstet Gynaecol 18: 827–842.
Bozkurt A, Deumens R, Beckmann C, Olde Damink L, Schugner F, Heschel I et al (2009). In vitro cell alignment obtained with a Schwann cell enriched microstructured nerve guide with longitudinal guidance channels. Biomaterials 30: 169–179.
Bradbury EJ, McMahon SB (2006). Opinion—Spinal cord repair strategies: why do they work? Nat Rev Neurosci 7: 644–653.
Bruns TJ, Hauser WA (2003). The epidemiology of traumatic brain injury: a review. Epilepsia 44: 2–10.
Bunge MB, Pearse DD (2003). Transplantation strategies to promote repair of the injured spinal cord. J Rehabil Res Dev 40: 55–62.
Caicco MJ, Cooke MJ, Wang Y, Tuladhar A, Morshead CM, Shoichet MS (2013a). A hydrogel composite system for sustained epi-cortical delivery of Cyclosporin A to the brain for treatment of stroke. J Control Release 166: 197–202.
Caicco MJ, Zahir T, Mothe AJ, Ballios BG, Kihm AJ, Tator CH et al (2013b). Characterization of hyaluronan-methylcellulose hydrogels for cell delivery to the injured spinal cord. J Biomed Mater Res A 101: 1472–1477.
Chaitin MH, Brun-Zinkernagel AM (1998). Immunolocalization of CD44 in the dystrophic rat retina. Exp Eye Res 67: 283–292.
Chan CC (2008). Inflammation: beneficial or detrimental after spinal cord injury? Recent Pat CNS Drug Discov 3: 189–199.
Chen CS, Mrksich M, Huang S, Whitesides GM, Ingber DE (1997). Geometric control of cell life and death. Science 276: 1425–1428.
Chen CS, Mrksich M, Huang S, Whitesides GM, Ingber DE (1998). Micropatterned surfaces for control of cell shape, position, and function. Biotechnol Prog 14: 356–363.
Chen MS, Huber AB, van der Haar ME, Frank M, Schnell L, Spillmann AA et al (2000). Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature 403: 434–439 First report showing that inhibition of myelin-associated neurite outgrowth inhibitor, Nogo-A, with a monoclonal antibody results in increased dorsal root ganglion neurite outgrowth when cultured on CNS myelin.
Cheng TY, Chen MH, Chang WH, Huang MY, Wang TW (2013). Neural stem cells encapsulated in a functionalized self-assembling peptide hydrogel for brain tissue engineering. Biomaterials 34: 2005–2016.
Cheung CY, Anseth KS (2006). Synthesis of immunoisolation barriers that provide localized immunosuppression for encapsulated pancreatic islets. Bioconjug Chem 17: 1036–1042.
Citron M (2010). Alzheimer’s disease: strategies for disease modification. Nat Rev Drug Discov 9: 387–398.
Clarke L, van der Kooy D (2011). The adult mouse dentate gyrus contains populations of committed progenitor cells that are distinct from subependymal zone neural stem cells. Stem Cells 29: 1448–1458.
Comoglio PM, Boccaccio C, Trusolino L (2003). Interactions between growth factor receptors and adhesion molecules: breaking the rules. Curr Opin Cell Biol 15: 565–571.
Conova L, Vernengo J, Jin Y, Himes BT, Neuhuber B, Fischer I et al (2011). A pilot study of poly(N-isopropylacrylamide)-g-polyethylene glycol and poly(N-isopropylacrylamide)-g-methylcellulose branched copolymers as injectable scaffolds for local delivery of neurotrophins and cellular transplants into the injured spinal cord. J Neurosurg Spine 15: 594–604.
Cooke MJ, Vulic K, Shoichet MS (2010). Design of biomaterials to enhance stem cell survival when transplanted into the damaged central nervous system. Soft Matter 6: 4988–4998.
Cooke MJ, Wang YF, Morshead CM, Shoichet MS (2011). Controlled epi-cortical delivery of epidermal growth factor for the stimulation of endogenous neural stem cell proliferation in stroke-injured brain. Biomaterials 32: 5688–5697 Report demonstrating that the PEGylation of EGF increases penetration into the brain when delivered via an epi-cortically-placed hydrogel for delivery into the stroke-injured brain.
Craig WS, Cheng S, Mullen DG, Blevitt J, Pierschbacher MD (1995). Concept and progress in the development of RGD-containing peptide pharmaceuticals. Biopolymers 37: 157–175.
Davie CA (2008). A review of Parkinson’s disease. Brit Med Bull 86: 109–127.
Davies JE, Huang C, Proschel C, Noble M, Mayer-Proschel M, Davies SJ (2006). Astrocytes derived from glial-restricted precursors promote spinal cord repair. J Biol 5: 7.
de Jong PT (2006). Age-related macular degeneration. N Engl J Med 355: 1474–1485.
de Las Heras Alarcon C, Pennadam S, Alexander C (2005). Stimuli responsive polymers for biomedical applications. Chem Soc Rev 34: 276–285.
DeForest CA, Anseth KS (2011). Cytocompatible click-based hydrogels with dynamically tunable properties through orthogonal photoconjugation and photocleavage reactions. Nat Chem 3: 925–931.
DeQuach JA, Yuan SH, Goldstein LSB, Christman KL (2011). Decellularized porcine brain matrix for cell culture and tissue engineering scaffolds. Tissue Eng Pt A 17: 2583–2592.
DeVore DP (1991). Long-term compatibility of intraocular lens implant materials. J Long Term Eff Med Implants 1: 205–216.
Dibajnia P, Morshead CM (2013). Role of neural precursor cells in promoting repair following stroke. Acta Pharmacol Sin 34: 78–90 Recent detailed review describing the delivery of therapeutics into the stroke-injured brain for endogeneous stem cell stimulation.
Domeniconi M, Cao Z, Spencer T, Sivasankaran R, Wang K, Nikulina E et al (2002). Myelin-associated glycoprotein interacts with the Nogo66 receptor to inhibit neurite outgrowth. Neuron 35: 283–290.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D et al (2006). Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8: 315–317.
Drury JL, Mooney DJ (2003). Hydrogels for tissue engineering: scaffold design variables and applications. Biomaterials 24: 4337–4351.
Emerich DF, Silva E, Ali O, Mooney D, Bell W, Yu SJ et al (2010). Injectable VEGF hydrogels produce near complete neurological and anatomical protection following cerebral ischemia in rats. Cell Transplant 19: 1063–1071.
Engler AJ, Sen S, Sweeney HL, Discher DE (2006). Matrix elasticity directs stem cell lineage specification. Cell 126: 677–689 Early example showing the effect of a substrate’s mechanical properties on mesechymal stem cell differentiation.
Erlandsson A, Lin CHA, Yu FG, Morshead CM (2011). Immunosuppression promotes endogenous neural stem and progenitor cell migration and tissue regeneration after ischemic injury. Experimen Neurol 230: 48–57.
Evans MJ, Kaufman MH (1981). Establishment in culture of pluripotential cells from mouse embryos. Nature 292: 154–156.
Fitch MT, Silver J (2008). CNS injury, glial scars, and inflammation: inhibitory extracellular matrices and regeneration failure. Exp Neurol 209: 294–301.
Flemming RG, Murphy CJ, Abrams GA, Goodman SL, Nealey PF (1999). Effects of synthetic micro- and nano-structured surfaces on cell behavior. Biomaterials 20: 573–588.
Fortun J, Hill CE, Bunge MB (2009). Combinatorial strategies with Schwann cell transplantation to improve repair of the injured spinal cord. Neurosci Lett 456: 124–132.
Freier T, Montenegro R, Shan Koh H, Shoichet MS (2005). Chitin-based tubes for tissue engineering in the nervous system. Biomaterials 26: 4624–4632.
Freund P, Schmidlin E, Wannier T, Bloch J, Mir A, Schwab ME et al (2006). Nogo-A-specific antibody treatment enhances sprouting and functional recovery after cervical lesion in adult primates. Nat Med 12: 790–792.
Friedenstein AJ, Chailakhjan RK, Lalykina KS (1970). The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet 3: 393–403.
Garcia-Alias G, Barkhuysen S, Buckle M, Fawcett JW (2009). Chondroitinase ABC treatment opens a window of opportunity for task-specific rehabilitation. Nat Neurosci 12: 1145–1151 Report demonstrating the necessity for both therapeutic treatment and physical rehabitation for functional recovery following spinal cord injury.
Ghirnikar RS, Lee YL, Eng LF (2000). Chemokine antagonist infusion attenuates cellular infiltration following spinal cord contusion injury in rat. J Neurosci Res 59: 63–73.
Ghosh F, Rauer O, Arner K (2008). Neuroretinal xenotransplantation to immunocompetent hosts in a discordant species combination. Neuroscience 152: 526–533.
Giordano GG, Chevezbarrios P, Refojo MF, Garcia CA (1995). Biodegradation and tissue reaction to intravitreous biodegradable Poly(D,L-lactic-co-glycolic) acid microspheres. Curr Eye Res 14: 761–768.
Goldsmith HS, de la Torre JC (1992). Axonal regeneration after spinal cord transection and reconstruction. Brain Res 589: 217–224 Early report demonstrating the potential for using hydrogels with bioactive molecules to regenerate the injured spinal cord.
Gouras P, Flood MT, Kjeldbye H (1984). Transplantation of cultured human retinal cells to monkey retina. An Acad Bras Cienc 56: 431–443 The first report of cell transplantation into the retina.
Gouras P, Flood MT, Kjeldbye H, Bilek MK, Eggers H (1985). Transplantation of cultured human retinal epithelium to bruchs membrane of the owl monkeys eye. Curr Eye Res 4: 253–265.
Graf J, Ogle RC, Robey FA, Sasaki M, Martin GR, Yamada Y et al (1987). A pentapeptide from the laminin-B1 chain mediates cell-adhesion and binds the 67000-laminin receptor. Biochemistry 26: 6896–6900.
Grant RP, Spitzfaden C, Altroff H, Campbell ID, Mardon HJ (1997). Structural requirements for biological activity of the ninth and tenth FIII domains of human fibronectin. J Biol Chem 272: 6159–6166.
Groothuis DR (2000). The blood-brain and blood-tumor barriers: a review of strategies for increasing drug delivery. Neuro-Oncology 2: 45–59.
Guo J, Su H, Zeng Y, Liang YX, Wong WM, Ellis-Behnke RG et al (2007). Reknitting the injured spinal cord by self-assembling peptide nanofiber scaffold. Nanomed Nanotechnol Biol Med 3: 311–321.
Gupta D, Tator CH, Shoichet MS (2006). Fast-gelling injectable blend of hyaluronan and methylcellulose for intrathecal, localized delivery to the injured spinal cord. Biomaterials 27: 2370–2379 First report that describes the feasibility of using HAMC for local delivery to the spinal cord for tissue regeneration.
Han LH, Lai JH, Yu S, Yang F (2013). Dynamic tissue engineering scaffolds with stimuli-responsive macroporosity formation. Biomaterials 34: 4251–4258.
Hauben E, Butovsky O, Nevo U, Yoles E, Moalem G, Agranov E et al (2000). Passive or active immunization with myelin basic protein promotes recovery from spinal cord contusion. J Neurosci 20: 6421–6430.
Haubner R, Gratias R, Diefenbach B, Goodman SL, Jonczyk A, Kessler H (1996). Structural and functional aspects of RGD-containing cyclic pentapeptides as highly potent and selective integrin alpha(v)beta(3) antagonists. J Am Chem Soc 118: 7461–7472.
Hawryluk GW, Rowland J, Kwon BK, Fehlings MG (2008). Protection and repair of the injured spinal cord: a review of completed, ongoing, and planned clinical trials for acute spinal cord injury. Neurosurg Focus 25: E14.
Hejcl A, Sedy J, Kapcalova M, Toro DA, Amemori T, Lesny P et al (2010). HPMA-RGD hydrogels seeded with mesenchymal stem cells improve functional outcome in chronic spinal cord injury. Stem Cells Dev 19: 1535–1546.
Hersel U, Dahmen C, Kessler H (2003). RGD modified polymers: biomaterials for stimulated cell adhesion and beyond. Biomaterials 24: 4385–4415 Detailed review about biomaterials conjugated with synthetic RGD peptides derivatives, and their effects on cellular bioactivity.
Hoare TR, Kohane DS (2008). Hydrogels in drug delivery: progress and challenges. Polymer 49: 1993–2007.
Hoffman-Kim D, Mitchel JA, Bellamkonda RV (2010). Topography, cell response, and nerve regeneration. Annu Rev Biomed Eng 12: 203–231.
Hofstetter CP, Holmstrom NAV, Lilja JA, Schweinhardt P, Hao JX, Spenger C et al (2005). Allodynia limits the usefulness of intraspinal neural stem cell grafts; directed differentiation improves outcome. Nat Neurosci 8: 346–353.
Hofstetter CP, Schwarz EJ, Hess D, Widenfalk J, El Manira A, Prockop DJ et al (2002). Marrow stromal cells form guiding strands in the injured spinal cord and promote recovery. Proc Natl Acad Sci USA 99: 2199–2204.
Hsiue GH, Lai JY, Lin PK (2002). Absorbable sandwich-like membrane for retinal-sheet transplantation. J Biomed Mater Res 61: 19–25.
Hyatt AJ, Wang D, Kwok JC, Fawcett JW, Martin KR (2010). Controlled release of chondroitinase ABC from fibrin gel reduces the level of inhibitory glycosaminoglycan chains in lesioned spinal cord. J Control Release 147: 24–29.
Inatani M, Tanihara H, Oohira A, Honjo M, Kido N, Honda Y (2000). Upregulated expression of neurocan, a nervous tissue specific proteoglycan, in transient retinal ischemia. Invest Ophth Vis Sci 41: 2748–2754.
Itosaka H, Kuroda S, Shichinohe H, Yasuda H, Yano S, Kamei S et al (2009). Fibrin matrix provides a suitable scaffold for bone marrow stromal cells transplanted into injured spinal cord: A novel material for CNS tissue engineering. Neuropathology 29: 248–257.
Jain A, Kim YT, McKeon RJ, Bellamkonda RV (2006). In situ gelling hydrogels for conformal repair of spinal cord defects, and local delivery of BDNF after spinal cord injury. Biomaterials 27: 497–504.
Jiang D, Liang J, Noble PW (2007). Hyaluronan in tissue injury and repair. Annu Rev Cell Dev Bi 23: 435–461.
Jimenez Hamann MC, Tator CH, Shoichet MS (2005). Injectable intrathecal delivery system for localized administration of EGF and FGF-2 to the injured rat spinal cord. Exp Neurol 194: 106–119.
Johnson PJ, Tatara A, McCreedy DA, Shiu A, Sakiyama-Elbert SE (2010a). Tissue-engineered fibrin scaffolds containing neural progenitors enhance functional recovery in a subacute model of SCI. Soft Matter 6: 5127–5137.
Johnson PJ, Tatara A, Shiu A, Sakiyama-Elbert SE (2010b). Controlled release of neurotrophin-3 and platelet-derived growth factor from fibrin scaffolds containing neural progenitor cells enhances survival and differentiation into neurons in a subacute model of SCI. Cell Transplant 19: 89–101.
Kang YM, Hwang DH, Kim BG, Go DH, Park KD (2010). Thermosensitive polymer-based hydrogel mixed with the anti-inflammatory agent minocycline induces axonal regeneration in hemisected spinal cord. Macromol Res 18: 399–403.
Kato M, Mrksich M (2004). Using model substrates to study the dependence of focal adhesion formation on the affinity of integrin-ligand complexes. Biochemistry 43: 2699–2707.
Kauer TM, Figueiredo JL, Hingtgen S, Shah K (2012). Encapsulated therapeutic stem cells implanted in the tumor resection cavity induce cell death in gliomas. Nat Neurosci 15: 197–204.
Kelley MW, Turner JK, Reh TA (1995). Regulation of proliferation and photoreceptor differentiation in fetal human retinal cell cultures. Invest Ophthalmol Vis Sci 36: 1280–1289.
Kim H, Zahir T, Tator CH, Shoichet MS (2011a). Effects of dibutyryl cyclic-amp on survival and neuronal differentiation of neural stem/progenitor cells transplanted into spinal cord injured rats. PLoS ONE 6: e21744.
Kim SH, Turnbull J, Guimond S (2011b). Extracellular matrix and cell signalling: the dynamic cooperation of integrin, proteoglycan and growth factor receptor. J Endocrinol 209: 139–151.
Kim YT, Caldwell JM, Bellamkonda RV (2009). Nanoparticle-mediated local delivery of methylprednisolone after spinal cord injury. Biomaterials 30: 2582–2590.
Klassen H, Schwartz MR, Bailey AH, Young MJ (2001). Surface markers expressed by multipotent human and mouse neural progenitor cells include tetraspanins and non-protein epitopes. Neurosci Lett 312: 180–182.
Kleinman HK, Martin GR (2005). Matrigel: basement membrane matrix with biological activity. Semin Cancer Biol 15: 378–386.
Kode JA, Mukherjee S, Joglekar MV, Hardikar AA (2009). Mesenchymal stem cells: immunobiology and role in immunomodulation and tissue regeneration. Cytotherapy 11: 377–391.
Kokaia Z, Martino G, Schwartz M, Lindvall O (2012). Cross-talk between neural stem cells and immune cells: the key to better brain repair? Nat Neurosci 15: 1078–1087.
Kolb B, Morshead C, Gonzalez C, Kim M, Gregg C, Shingo T et al (2007). Growth factor-stimulated generation of new cortical tissue and functional recovery after stroke damage to the motor cortex of rats. J Cerebr Blood F Met 27: 983–997.
Kondziolka D, Steinberg GK, Wechsler L, Meltzer CC, Elder E, Gebel J et al (2005). Neurotransplantation for patients with subcortical motor stroke: a Phase 2 randomized trial. J Neurosurg 103: 38–45.
Krishnamoorthy R, Agarwal N, Chaitin MH (2000). Upregulation of CD44 expression in the retina during the RDS degeneration. Brain Res Mol Brain Res 77: 125–130.
Kwon BK, Tetzlaff W, Grauer JN, Beiner J, Vaccaro AR (2004). Pathophysiology and pharmacologic treatment of acute spinal cord injury. Spine J 4: 451–464.
Lampe KJ, Antaris AL, Heilshorn SC (2013). Design of three-dimensional engineered protein hydrogels for tailored control of neurite growth. Acta Biomaterialia 9: 5590–5599.
Lassmann H, van Horssen J, Mahad D (2012). Progressive multiple sclerosis: pathology and pathogenesis. Nat Rev Neurol 8: 647–656.
Lavik EB, Klassen H, Warfvinge K, Langer R, Young MJ (2005). Fabrication of degradable polymer scaffolds to direct the integration and differentiation of retinal progenitors. Biomaterials 26: 3187–3196.
Lee H, McKeon RJ, Bellamkonda RV (2010). Sustained delivery of thermostabilized chABC enhances axonal sprouting and functional recovery after spinal cord injury. Proc Natl Acad Sci USA 107: 3340–3345.
Lee RJ, Springer ML, Blanco-Bose WE, Shaw R, Ursell PC, Blau HM (2000). VEGF gene delivery to myocardium: deleterious effects of unregulated expression. Circulation 102: 898–901.
Leipzig ND, Shoichet MS (2009). The effect of substrate stiffness on adult neural stem cell behavior. Biomaterials 30: 6867–6878.
Leipzig ND, Xu CC, Zahir T, Shoichet MS (2010). Functional immobilization of interferon-gamma induces neuronal differentiation of neural stem cells. J Biomed Mater Res A 93A: 625–633.
Lerou PH, Daley GQ (2005). Therapeutic potential of embryonic stem cells. Blood Rev 19: 321–331.
Levesque SG, Shoichet MS (2006). Synthesis of cell-adhesive dextran hydrogels and macroporous scaffolds. Biomaterials 27: 5277–5285.
Lewis GP, Fisher SK (2003). Up-regulation of glial fibrillary acidic protein in response to retinal injury: its potential role in glial remodeling and a comparison to vimentin expression. Int Rev Cytol 230: 263-+.
Li LX, Turner JE (1988). Inherited retinal dystrophy in the rcs rat—prevention of photoreceptor degeneration by pigment epithelial-cell transplantation. Exp Eye Res 47: 911–917.
Li X, Liu X, Cui L, Brunson C, Zhao W, Bhat NR et al (2013). Engineering an in situ crosslinkable hydrogel for enhanced remyelination. FASEB J 27: 1127–1136.
Li Y, Raisman G (1994). Schwann-cells induce sprouting in motor and sensory axons in the adult-rat spinal-cord. J Neurosci 14: 4050–4063.
Liebscher T, Schnell L, Schnell D, Scholl J, Schneider R, Gullo M et al (2005). Nogo-A antibody improves regeneration and locomotion of spinal cord-injured rats. Ann Neurol 58: 706–719.
Lietz M, Dreesmann L, Hoss M, Oberhoffner S, Schlosshauer B (2006). Neuro tissue engineering of glial nerve guides and the impact of different cell types. Biomaterials 27: 1425–1436.
Liu BP, Fournier A, GrandPre T, Strittmatter SM (2002). Myelin-associated glycoprotein as a functional ligand for the Nogo-66 receptor. Science 297: 1190–1193.
Liu SQ, Tian QA, Hedrick JL, Hui JHP, Ee PLR, Yang YY (2010). Biomimetic hydrogels for chondrogenic differentiation of human mesenchymal stem cells to neocartilage. Biomaterials 31: 7298–7307.
Liu Z, Gao X, Kang T, Jiang M, Miao D, Gu G et al (2013a). B6 Peptide-modified PEG-PLA nanoparticles for enhanced brain delivery of neuroprotective peptide. Bioconjug Chem 24: 997–1007.
Liu ZY, Jiang MY, Kang T, Miao DY, Gu GZ, Song QX et al (2013b). Lactoferrin-modified PEG-co-PCL nanoparticles for enhanced brain delivery of NAP peptide following intranasal administration. Biomaterials 34: 3870–3881.
Lo AC, Woo TT, Wong RL, Wong D (2011). Apoptosis and other cell death mechanisms after retinal detachment: implications for photoreceptor rescue. Ophthalmologica 226 (Suppl 1): 10–17.
Lo EH, Dalkara T, Moskowitz MA (2003). Mechanisms, challenges and opportunities in stroke. Nat Rev Neurosci 4: 399–415.
MacLaren RE, Pearson RA, MacNeil A, Douglas RH, Salt TE, Akimoto M et al (2006). Retinal repair by transplantation of photoreceptor precursors. Nature 444: 203–207 The first report of vision improvement after purified photoreceptor transplantation in an animal model.
MacLellan CL, Keough MB, Granter-Button S, Chernenko GA, Butt S, Corbett D (2011). A critical threshold of rehabilitation involving brain-derived neurotrophic factor is required for poststroke recovery. Neurorehabil Neural Repair 25: 740–748.
Maheshwari G, Brown G, Lauffenburger DA, Wells A, Griffith LG (2000). Cell adhesion and motility depend on nanoscale RGD clustering. J Cell Sci 113 (Pt 10): 1677–1686.
Mardilovich A, Craig JA, McCammon MQ, Garg A, Kokkoli E (2006). Design of a novel fibronectin-mimetic peptide-amphiphile for functionalized biomaterials. Langmuir 22: 3259–3264.
Martino MM, Tortelli F, Mochizuki M, Traub S, Ben-David D, Kuhn GA et al (2011). Engineering the growth factor microenvironment with fibronectin domains to promote wound and bone tissue healing. Sci Translation Med 3: 100.
Massia SP, Hubbell JA (1991). An RGD spacing of 440 nm is sufficient for integrin alpha V beta 3-mediated fibroblast spreading and 140 nm for focal contact and stress fiber formation. J Cell Biol 114: 1089–1100.
Matsuse D, Kitada M, Ogura F, Wakao S, Kohama M, Kira J et al (2011). Combined transplantation of bone marrow stromal cell-derived neural progenitor cells with a collagen sponge and basic fibroblast growth factor releasing microspheres enhances recovery after cerebral ischemia in rats. Tissue Eng A 17: 1993–2004.
McCulloch EA, Till JE (2005). Perspectives on the properties of stem cells. Nat Med 11: 1026–1028.
McDonald JW, Liu XZ, Qu Y, Liu S, Mickey SK, Turetsky D et al (1999). Transplanted embryonic stem cells survive, differentiate and promote recovery in injured rat spinal cord. Nat Med 5: 1410–1412.
Menon PK, Muresanu DF, Sharma A, Mossler H, Sharma HS (2012). Cerebrolysin, a mixture of neurotrophic factors induces marked neuroprotection in spinal cord injury following intoxication of engineered nanoparticles from metals. CNS Neurol Disord Drug Targets 11: 40–49.
Milne JJ (2011). Scale-up of protein purification: downstream processing issues. In: Walls D, Loughran ST (eds) Protein Chromatography: Methods and Protocols. Springer Science+Business Media: Hatfield. pp 73–85.
Mo XM, Xu CY, Kotaki M, Ramakrishna S (2004). Electrospun P(LLA-CL) nanofiber: a biomimetic extracellular matrix for smooth muscle cell and endothelial cell proliferation. Biomaterials 25: 1883–1890.
Moon LD, Asher RA, Fawcett JW (2003). Limited growth of severed CNS axons after treatment of adult rat brain with hyaluronidase. J Neurosci Res 71: 23–37.
Moore MJ, Friedman JA, Lewellyn EB, Mantila SM, Krych AJ, Ameenuddin S et al (2006). Multiple-channel scaffolds to promote spinal cord axon regeneration. Biomaterials 27: 419–429.
Mothe AJ, Tam RY, Zahir T, Tator CH, Shoichet MS (2013). Repair of the injured spinal cord by transplantation of neural stem cells in a hyaluronan-based hydrogel. Biomaterials 34: 3775–3783.
Musah S, Morin SA, Wrighton PJ, Zwick DB, Jin S, Kiessling LL (2012). Glycosaminoglycan-binding hydrogels enable mechanical control of human pluripotent stem cell self-renewal. ACS Nano 6: 10168–10177.
Nakaguchi K, Jinnou H, Kaneko N, Sawada M, Hikita T, Saitoh S et al (2012). Growth factors released from gelatin hydrogel microspheres increase new neurons in the adult mouse brain. Stem Cells Int 2012: 915160.
Neiiendam JL, Kohler LB, Christensen C, Li SZ, Pedersen MV, Ditlevsen DK et al (2004). An NCAM-derived FGF-receptor agonist, the FGL-peptide, induces neurite outgrowth and neuronal survival in primary rat neurons. J Neurochem 91: 920–935.
Nistor GI, Totoiu MO, Haque N, Carpenter MK, Keirstead HS (2005). Human embryonic stem cells differentiate into oligodendrocytes in high purity and myelinate after spinal cord transplantation. Glia 49: 385–396.
Nowak JZ (2006). Age-related macular degeneration (AMD): pathogenesis and therapy. Pharmacol Rep 58: 353–363.
Ohab JJ, Fleming S, Blesch A, Carmichael ST (2006). A neurovascular niche for neurogenesis after stroke. J Neurosci 26: 13007–13016.
Orive G, Anitua E, Pedraz JL, Emerich DF (2009). Biomaterials for promoting brain protection, repair and regeneration. Nat Rev Neurosci 10: 682–U647 Detailed review describing the use of biomaterials for drug and cell delivery into the brain.
Owen SC, Fisher SA, Tam RY, Nimmo CM, Shoichet MS (2013). Hyaluronic acid click hydrogels emulate the extracellular matrix. Langmuir 29: 7393–7400.
Owen SC, Shoichet MS (2010). Design of three-dimensional biomimetic scaffolds. J Biomed Mater Res A 94A: 1321–1331.
Pakulska MM, Ballios BG, Shoichet MS (2012). Injectable hydrogels for central nervous system therapy. Biomed Mater 7: 024101.
Pakulska MM, Vulic K, Shoichet MS (2013). Affinity-based release of Chondroitinase ABC from a modified methylcellulose hydrogel. J Control Release 171: 11–16.
Pardridge WM (2012). Drug transport across the blood-brain barrier. J Cerebr Blood F Met 32: 1959–1972.
Park KI, Teng YD, Snyder EY (2002). The injured brain interacts reciprocally with neural stem cells supported by scaffolds to reconstitute lost tissue. Nat Biotechnol 20: 1111–1117 Early report describing that delivery of NSPCs encapsulated in PLGA scaffolds into the brain promotes tissue regeneration.
Pastor JC, de la Rua ER, Martin F (2002). Proliferative vitreoretinopathy: risk factors and pathobiology. Prog Retinal Eye Res 21: 127–144.
Patel MM, Goyal BR, Bhadada SV, Bhatt JS, Amin AF (2009). Getting into the brain: approaches to enhance brain drug delivery. CNS Drugs 23: 35–58.
Perale G, Rossi F, Santoro M, Peviani M, Papa S, Llupi D et al (2012). Multiple drug delivery hydrogel system for spinal cord injury repair strategies. J Control Release 159: 271–280 Interesting study demonstrating the diffusion of molecules of different sizes out of hydrogels when transplanted into the spinal cord.
Pettikiriarachchi JTS, Parish CL, Shoichet MS, Forsythe JS, Nisbet DR (2010). Biomaterials for brain tissue engineering. Aust J Chem 63: 1143–1154.
Pfeifer K, Vroemen M, Caioni M, Aigner L, Bogdahn U, Weidner N (2006). Autologous adult rodent neural progenitor cell transplantation represents a feasible strategy to promote structural repair in the chronically injured spinal cord. Regen Med 1: 255–266.
Piantino J, Burdick JA, Goldberg D, Langer R, Benowitz LI (2006). An injectable, biodegradable hydrogel for trophic factor delivery enhances axonal rewiring and improves performance after spinal cord injury. Exp Neurol 201: 359–367.
Pierschbacher MD, Ruoslahti E (1984). Cell Attachment activity of fibronectin can be duplicated by small synthetic fragments of the molecule. Nature 309: 30–33 First report describing that the short fibronectin-derived peptide sequence Arg-Gly-Asp promotes cell adhesion.
Popa-Wagner A, Stocker K, Balseanu AT, Rogalewski A, Diederich K, Minnerup J et al (2010). Effects of granulocyte-colony stimulating factor after stroke in aged rats. Stroke 41: 1027–1031.
Prowse ABJ, Chong F, Gray PP, Munro TP (2011). Stem cell integrins: implications for ex-vivo culture and cellular therapies. Stem Cell Res 6: 1–12.
Quertainmont R, Cantinieaux D, Botman O, Sid S, Schoenen J, Franzen R (2012). Mesenchymal stem cell graft improves recovery after spinal cord injury in adult rats through neurotrophic and pro-angiogenic actions. PLoS One 7: e39500.
Rajnicek AM, Britland S, McCaig CD (1997). Contact guidance of CNS neurites on grooved quartz: influence of groove dimensions, neuronal age and cell type. J Cell Sci 110: 2905–2913.
Ramon-Cueto A, Plant GW, Avila J, Bunge MB (1998). Long-distance axonal regeneration in the transected adult rat spinal cord is promoted by olfactory ensheathing glia transplants. J Neurosci 18: 3803–3815.
Ranjan AP, Mukerjee A, Helson L, Vishwanatha JK (2012). Scale up, optimization and stability analysis of Curcumin C3 complex-loaded nanoparticles for cancer therapy. J Nanobiotechnol 10: 38.
Rapalino O, Lazarov-Spiegler O, Agranov E, Velan GJ, Yoles E, Fraidakis M et al (1998). Implantation of stimulated homologous macrophages results in partial recovery of paraplegic rats. Nat Med 4: 814–821.
Redenti S, Neeley WL, Rompani S, Saigal S, Yang J, Klassen H et al (2009). Engineering retinal progenitor cell and scrollable poly(glycerol-sebacate) composites for expansion and subretinal transplantation. Biomaterials 30: 3405–3414 The first report of an injectable biomaterial for cell transplantation into the retina.
Reynolds BA, Weiss S (1992). Generation of neurons and astrocytes from isolated cells of the adult mammalian central-nervous-system. Science 255: 1707–1710 First report showing that cells (NSPCs) found in the mouse lateral ventricles of the subventricular zone can divide and differentiate into neurons and astrocytes when treated with EGF.
Rietschel ET, Kirikae T, Schade FU, Mamat U, Schmidt G, Loppnow H et al (1994). Bacterial endotoxin: molecular relationships of structure to activity and function. FASEB J 8: 217–225.
Rossi F, Perale G, Papa S, Forloni G, Veglianese P (2013). Current options for drug delivery to the spinal cord. Expert Opin Drug Deliv 10: 385–396.
Rowe NA, Biswas S, Lloyd IC (2004). Primary IOL implantation in children: a risk analysis of foldable acrylic vs PMMA lenses. Br J Ophthalmol 88: 481–485.
Roy D, Cambre JN, Sumerlin BS (2010). Future perspectives and recent advances in stimuli-responsive materials. Prog Polym Sci 35: 278–301.
Royo PE, Quay WB (1959). Retinal transplantation from fetal to maternal mammalian eye. Growth 23: 313–336.
Schabitz WR, Steigleder T, Cooper-Kuhn CM, Schwab S, Sommer C, Schneider A et al (2007). Intravenous brain-derived neurotrophic factor enhances poststroke sensorimotor recovery and stimulates neurogenesis. Stroke 38: 2165–2172.
Schnell E, Klinkhammer K, Balzer S, Brook G, Klee D, Dalton P et al (2007). Guidance of glial cell migration and axonal growth on electrospun nanofibers of poly-epsilon-caprolactone and a collagen/poly-epsilon-caprolactone blend. Biomaterials 28: 3012–3025.
Schwab ME, Bartholdi D (1996). Degeneration and regeneration of axons in the lesioned spinal cord. Physiol Rev 76: 319–370.
Seiler MJ, Aramant RB (1998). Intact sheets of fetal retina transplanted to restore damaged rat retinas. Invest Ophth Vis Sci 39: 2121–2131.
Seiler MJ, Aramant RB (2012). Cell replacement and visual restoration by retinal sheet transplants. Prog Retin Eye Res 31: 661–687.
Sekhon LHS, Fehlings MG (2001). Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 26: S2–S12.
Shintani K, Shechtman DL, Gurwood AS (2009). Review and update: current treatment trends for patients with retinitis pigmentosa. Optometry 80: 384–401.
Shoichet MS, Tate CC, Baumann MD, LaPlaca MC (2008). Strategies for Regeneration and Repair in the Injured Central Nervous System. In WM R (ed) Indwelling Neural Implants: Strategies for Contending with the In Vivo Environment. CRC Press: Boca Raton, FL, USA.
Silva NA, Cooke MJ, Tam RY, Sousa N, Salgado AJ, Reis RL et al (2012). The effects of peptide modified gellan gum and olfactory ensheathing glia cells on neural stem/progenitor cell fate. Biomaterials 33: 6345–6354.
Siminovitch L, McCulloch EA, Till JE (1963). The distribution of colony-forming cells among spleen colonies. J Cell Physiol 62: 327–336.
Singhvi R, Kumar A, Lopez GP, Stephanopoulos GN, Wang DI, Whitesides GM et al (1994). Engineering cell shape and function. Science 264: 696–698.
Smeal RM, Rabbitt R, Biran R, Tresco PA (2005). Substrate curvature influences the direction of nerve outgrowth. Ann Biomed Eng 33: 376–382.
Smeal RM, Tresco PA (2008). The influence of substrate curvature on neurite outgrowth is cell type dependent. Exp Neurol 213: 281–292.
Snyder EY, Park KI (2002). Limitations in brain repair. Nat Med 8: 928–930.
Su J, Hu BH, Lowe WL Jr., Kaufman DB, Messersmith PB (2010). Anti-inflammatory peptide-functionalized hydrogels for insulin-secreting cell encapsulation. Biomaterials 31: 308–314.
Sun T, Mai S, Norton D, Haycock JW, Ryan AJ, MacNeil S (2005). Self-organization of skin cells in three-dimensional electrospun polystyrene scaffolds. Tissue Eng 11: 1023–1033.
Sun YJ, Jin KL, Xie L, Childs J, Mao XO, Logvinova A et al (2003). VEGF-induced neuroprotection, neurogenesis, and angiogenesis after focal cerebral ischemia. J Clin Invest 111: 1843–1851.
Sur S, Newcomb CJ, Webber MJ, Stupp SI (2013). Tuning supramolecular mechanics to guide neuron development. Biomaterials 34: 4749–4757.
Suzuki M, Raisman G (1992). The glial framework of central white matter tracts: segmented rows of contiguous interfascicular oligodendrocytes and solitary astrocytes give rise to a continuous meshwork of transverse and longitudinal processes in the adult rat fimbria. Glia 6: 222–235.
Taddei ML, Giannoni E, Fiaschi T, Chiarugi P (2012). Anoikis: an emerging hallmark in health and diseases. J Pathol 226: 380–393.
Takahashi K, Yamanaka S (2006). Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126: 663–676 Important study that demonstrated that adult mouse cells can be transformed into induced pluripotent stem cells using a variety of transcription factors (ie Oct3/4, Sox2, c-Myc and Klf4).
Takenaga M, Ishihara T, Ohta Y, Tokura Y, Hamaguchi A, Igarashi R et al (2010). Nano PGE1 promoted the recovery from spinal cord injury-induced motor dysfunction through its accumulation and sustained release. J Control Release 148: 249–254.
Tam RY, Cooke MJ, Shoichet MS (2012). A covalently modified hydrogel blend of hyaluronan-methyl cellulose with peptides and growth factors influences neural stem/progenitor cell fate. J Mater Chem 22: 19402–19411.
Tao S, Young C, Redenti S, Zhang YQ, Klassen H, Desai T et al (2007). Survival, migration and differentiation of retinal progenitor cells transplanted on micro-machined poly(methyl methacrylate) scaffolds to the subretinal space. Lab Chip 7: 695–701.
Tashiro K, Sephel GC, Weeks B, Sasaki M, Martin GR, Kleinman HK et al (1989). A synthetic peptide containing the ikvav sequence from the a-chain of laminin mediates cell attachment, migration, and neurite outgrowth. J Biol Chem 264: 16174–16182.
Taylor SJ, Rosenzweig ES, McDonald JW, Sakiyama-Elbert SE (2006). Delivery of neurotrophin-3 from fibrin enhances neuronal fiber sprouting after spinal cord injury. J Control Release 113: 226–235.
Teramoto T, Qu JH, Plumier JC, Moskowitz MA (2003). EGF amplifies the replacement of parvalbumin-expressing striatal interneurons after ischemia. J Clin Invest 111: 1125–1132.
Tester NJ, Plaas AH, Howland DR (2007). Effect of body temperature on chondroitinase ABC’s ability to cleave chondroitin sulfate glycosaminoglycans. J Neurosci Res 85: 1110–1118.
Tibbitt MW, Anseth KS (2009). Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol Bioeng 103: 655–663.
Till JE, McCulloch EA (1961). A direct measurement of the radiation sensitivity of normal mouse bone marrow cells. Radiat Res 14: 213–222.
Tognetto D, Toto L, Minutola D, Ballone E, Di Nicola M, Di Mascio R et al (2003). Hydrophobic acrylic versus heparin surface-modified polymethylmethacrylate intraocular lens: a biocompatibility study. Graefes Arch Clin Exp Ophthalmol 241: 625–630.
Tomita M, Lavik E, Klassen H, Zahir T, Langer R, Young MJ (2005a). Biodegradable polymer composite grafts promote the survival and differentiation of retinal progenitor cells. Stem Cells 23: 1579–1588 The first comparison of cell transplantation with a biomaterial vs bolus injection into the eye.
Tonge DA, de Burgh HT, Docherty R, Humphries MJ, Craig SE, Pizzey J (2012). Fibronectin supports neurite outgrowth and axonal regeneration of adult brain neurons in vitro. Brain Res 1453: 8–16.
Tropepe V, Coles BL, Chiasson BJ, Horsford DJ, Elia AJ, McInnes RR et al (2000). Retinal stem cells in the adult mammalian eye. Science 287: 2032–2036 First report of retinal stem cells found in the adult mouse eye can proliferate and differentiate into retinal-specific cell types (eg, photoreceptors, bipolar neurons and Muller glia).
Tsai EC, Dalton PD, Shoichet MS, Tator CH (2004). Synthetic hydrogel guidance channels facilitate regeneration of adult rat brainstem motor axons after complete spinal cord transection. J Neurotrauma 21: 789–804.
Tsuji O, Miura K, Okada Y, Fujiyoshi K, Mukaino M, Nagoshi N et al (2010). Therapeutic potential of appropriately evaluated safe-induced pluripotent stem cells for spinal cord injury. Proc Natl Acad Sci USA 107: 12704–12709.
Tucker BA, Redenti SM, Jiang CH, Swift JS, Klassen HJ, Smith ME et al (2010). The use of progenitor cell/biodegradable MMP2-PLGA polymer constructs to enhance cellular integration and retinal repopulation. Biomaterials 31: 9–19.
Tureyen K, Vemuganti R, Bowen KK, Sailor KA, Dempsey RJ (2005). EGF and FGF-2 infusion increases post-ischemic neural progenitor cell proliferation in the adult rat brain. Neurosurgery 57: 1254–1262.
Turner JE, Seiler M, Aramant R, Blair JR (1988). Embryonic retinal grafts transplanted into the lesioned adult rat retina. Prog Brain Res 78: 131–139.
Tysseling-Mattiace VM, Sahni V, Niece KL, Birch D, Czeisler C, Fehlings MG et al (2008). Self-assembling nanofibers inhibit glial scar formation and promote axon elongation after spinal cord injury. J Neurosci 28: 3814–3823.
Victorio SCS, Havton LA, Oliveira ALR (2010). Absence of IFN gamma expression induces neuronal degeneration in the spinal cord of adult mice. J Neuroinflamm 7: 77–90.
Volpato FZ, Fuhrmann T, Migliaresi C, Hutmacher DW, Dalton PD (2013). Using extracellular matrix for regenerative medicine in the spinal cord. Biomaterials 34: 4945–4955.
Vulic K, Shoichet MS (2012). Tunable growth factor delivery from injectable hydrogels for tissue engineering. J Am Chem Soc 134: 882–885.
Wamil AW, Wamil BD, Hellerqvist CG (1998). CM101-mediated recovery of walking ability in adult mice paralyzed by spinal cord injury. Proc Natl Acad Sci USA 95: 13188–13193.
Wang TY, Forsythe JS, Nisbet DR, Parish CL (2012a). Promoting engraftment of transplanted neural stem cells/progenitors using biofunctionalised electrospun scaffolds. Biomaterials 33: 9188–9197.
Wang YF, Cooke MJ, Morshead CM, Shoichet MS (2012b). Hydrogel delivery of erythropoietin to the brain for endogenous stem cell stimulation after stroke injury. Biomaterials 33: 2681–2692.
Wechsler LR (2009). Clinical trials of stroke therapy which cells, which patients? Stroke 40: S149–S151.
Wei YT, He Y, Xu CL, Wang Y, Liu BF, Wang XM et al (2010). Hyaluronic acid hydrogel modified with nogo-66 receptor antibody and poly-L-lysine to promote axon regrowth after spinal cord injury. J Biomed Mater Res B Appl Biomater 95: 110–117.
Weiss S, Dunne C, Hewson J, Wohl C, Wheatley M, Peterson AC et al (1996). Multipotent CNS stem cells are present in the adult mammalian spinal cord and ventricular neuroaxis. J Neurosci 16: 7599–7609 First report describing the presence of neural stem cells in the spinal cord of adult mammals.
Wenkel H, Streilein JW (2000). Evidence that retinal pigment epithelium functions as an immune-privileged tissue. Invest Ophth Vis Sci 41: 3467–3473.
Werner C, Engelhard K (2007). Pathophysiology of traumatic brain injury. Br J Anaesth 99: 4–9.
West EL, Pearson RA, Tschernutter M, Sowden JC, MacLaren RE, Ali RR (2008). Pharmacological disruption of the outer limiting membrane leads to increased retinal integration of transplanted photoreceptor precursors. Exp Eye Res 86: 601–611.
White RE, Jakeman LB (2008). Don’t fence me in: harnessing the beneficial roles of astrocytes for spinal cord repair. Restor Neurol Neurosci 26: 197–214.
Willerth SM (2011). Neural tissue engineering using embryonic and induced pluripotent stem cells. Stem Cell Res Ther 2: 17.
Wongpichedchai S, Weiter JJ, Weber P, Dorey CK (1992). Comparison of external and internal approaches for transplantation of autologous retinal pigment epithelium. Invest Ophthalmol Vis Sci 33: 3341–3352.
Wosnick JH, Shoichet MS (2008). Three-dimensional chemical patterning of transparent hydrogels. Chem Mater 20: 55–60.
Wright LS, Li J, Caldwell MA, Wallace K, Johnson JA, Svendsen CN (2003). Gene expression in human neural stem cells: effects of leukemia inhibitory factor. J Neurochem 86: 179–195.
Wylie RG, Ahsan S, Aizawa Y, Maxwell KL, Morshead CM, Shoichet MS (2011). Spatially controlled simultaneous patterning of multiple growth factors in three-dimensional hydrogels. Nat Mater 10: 799–806.
Yamanaka A, Nakamae K, Takeuchi M, Momose A, Fukado Y, Oshima K et al (1985). Scanning electron microscope study on the biodegradation of IOL and suturing materials. Trans Ophthalmol Soc UK 104 (Pt 5): 517–521.
Yandava BD, Billinghurst LL, Snyder EY (1999). ‘Global’ cell replacement is feasible via neural stem cell transplantation: Evidence from the dysmyelinated shiverer mouse brain. Proc Natl Acad Sci USA 96: 7029–7034.
Zhan X, Gao M, Jiang Y, Zhang W, Wong WM, Yuan Q et al (2013). Nanofiber scaffolds facilitate functional regeneration of peripheral nerve injury. Nanomed Nanotechnol Biol Med 9: 305–315.
Zhang HZ, Hayashi T, Tsuru K, Deguchi K, Nagdhara M, Hayakawa S et al (2007a). Vascular endothelial growth factor promotes brain tissue regeneration with a novel biomaterial polydimethylsiloxane-tetraethoxysilane. Brain Res 1132: 29–35.
Zhang LQ, Ma ZW, Smith GM, Wen XJ, Pressman Y, Wood PM et al (2009). GDNF-enhanced axonal regeneration and myelination following spinal cord injury is mediated by primary effects on neurons. Glia 57: 1178–1191.
Zhang Y, Klassen HJ, Tucker BA, Perez MTR, Young MJ (2007b). CNS progenitor cells promote a permissive environment for neurite outgrowth via a matrix metalloproteinase-2-dependent mechanism. J Neurosci 27: 4499–4506.
Zhong J, Chan A, Morad L, Kornblum HI, Fan GP, Carmichael ST (2010). Hydrogel matrix to support stem cell survival after brain transplantation in stroke. Neurorehab Neural Re 24: 636–644.
Zhu J, Marchant RE (2011). Design properties of hydrogel tissue-engineering scaffolds. Expert Rev Med Devices 8: 607–626.
Zimmermann DR, Dours-Zimmermann MT (2008). Extracellular matrix of the central nervous system: from neglect to challenge. Histochem Cell Biol 130: 635–653 Detailed review describing the composition of the extracellular matrix of the CNS.
Zuo J, Neubauer D, Dyess K, Ferguson TA, Muir D (1998). Degradation of chondroitin sulfate proteoglycan enhances the neurite-promoting potential of spinal cord tissue. Exp Neurol 154: 654–662 Early report describing the role of ChABC in degrading chondroitin sulfate and promoting neurite outgrowth in the injured spinal cord.
Acknowledgements
We acknowledge the Natural Sciences and Engineering Research Council of Canada (MSS), Canadian Institutes of Health Research (MSS), and the IBBME International Scholars’ Fellowship (NM) for their financial support. We also thank Dr Michael J. Cooke for helpful discussions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tam, R., Fuehrmann, T., Mitrousis, N. et al. Regenerative Therapies for Central Nervous System Diseases: a Biomaterials Approach. Neuropsychopharmacol 39, 169–188 (2014). https://doi.org/10.1038/npp.2013.237
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2013.237
Keywords
This article is cited by
-
Self-healing hydrogel as an injectable implant: translation in brain diseases
Journal of Biomedical Science (2023)
-
Magnetothermal-based non-invasive focused magnetic stimulation for functional recovery in chronic stroke treatment
Scientific Reports (2023)
-
An Insight of Nanomaterials in Tissue Engineering from Fabrication to Applications
Tissue Engineering and Regenerative Medicine (2022)
-
Comparison of systemic and localized carrier-mediated delivery of methylprednisolone succinate for treatment of acute spinal cord injury
Experimental Brain Research (2021)
-
Delivery of transcription factors as modulators of cell differentiation
Drug Delivery and Translational Research (2021)