Abstract
Background:
There is emerging literature demonstrating a relationship between the timing of feeding and weight regulation in animals. However, whether the timing of food intake influences the success of a weight-loss diet in humans is unknown.
Objective:
To evaluate the role of food timing in weight-loss effectiveness in a sample of 420 individuals who followed a 20-week weight-loss treatment.
Methods:
Participants (49.5% female subjects; age (mean±s.d.): 42±11 years; BMI: 31.4±5.4 kg m−2) were grouped in early eaters and late eaters, according to the timing of the main meal (lunch in this Mediterranean population). 51% of the subjects were early eaters and 49% were late eaters (lunch time before and after 1500 hours, respectively), energy intake and expenditure, appetite hormones, CLOCK genotype, sleep duration and chronotype were studied.
Results:
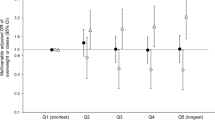
Late lunch eaters lost less weight and displayed a slower weight-loss rate during the 20 weeks of treatment than early eaters (P=0.002). Surprisingly, energy intake, dietary composition, estimated energy expenditure, appetite hormones and sleep duration was similar between both groups. Nevertheless, late eaters were more evening types, had less energetic breakfasts and skipped breakfast more frequently that early eaters (all; P<0.05). CLOCK rs4580704 single nucleotide polymorphism (SNP) associated with the timing of the main meal (P=0.015) with a higher frequency of minor allele (C) carriers among the late eaters (P=0.041). Neither sleep duration, nor CLOCK SNPs or morning/evening chronotype was independently associated with weight loss (all; P>0.05).
Conclusions:
Eating late may influence the success of weight-loss therapy. Novel therapeutic strategies should incorporate not only the caloric intake and macronutrient distribution—as is classically done—but also the timing of food.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
09 April 2013
This article has been corrected since online publication and a corrigendum is also printed in this issue
References
Corbalán MD, Morales EM, Canteras M, Espallardo A, Hernández T, Garaulet M . Effectiveness of cognitive-behavioral therapy based on the Mediterranean diet for the treatment of obesity. Nutrition 2009; 25: 861–869.
Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, Vieira PN et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity (Silver Spring) 2010; 18: 725–735.
Garaulet M, Sánchez-Moreno C, Smith CE, Lee YC, Nicolás F, Ordovás JM . Ghrelin sleep reduction and evening preference: relationships to CLOCK 3111 T/C SNP and weight loss. PLoS One 2011; 6: e17435.
Garaulet M, Esteban Tardido A, Lee YC, Smith CE, Parnell LD et al. SIRT1 and CLOCK 3111T>C combined genotype is associated with evening preference and weight loss resistance in a behavioral therapy treatment for obesity. Int J Obes (Lond) 2012; 36: 1436–1441.
Garaulet M, Corbalán-Tutau MD, Madrid JA, Baraza JC, Parnell LD, Lee YC et al. PERIOD2 variants are associated with abdominal obesity, psycho-behavioral factors, and attrition in the dietary treatment of obesity. J Am Diet Assoc 2010; 110: 917–921.
Oishi K, Shirai H, Ishida N . CLOCK is involved in the circadian transactivation of peroxisome-proliferator-activated receptor alpha (PPARalpha) in mice. Biochem J 2005; 386: 575–581.
Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science 2005; 308: 1043–1045.
Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH et al. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 2010; 466: 627–631.
Froy O . Metabolism and circadian rhythms-implications for obesity. Endocr Rev 2010; 31: 1–24.
Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW . Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring) 2009; 17: 2100–2102.
Sherman H, Genzer Y, Cohen R, Chapnik N, Madar Z, Froy O . Timed high-fat diet resets circadian metabolism and prevents obesity. FASEB J 2012; 26: 3493–3502.
Lowrey PL, Takahashi JS . Mammalian circadian biology: elucidating genome-wide levels of temporal organization. Annu Rev Genomics Hum Genet 2004; 5: 407–441.
Scheer FA, Hilton MF, Mantzoros CS, Shea SA . Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 2009; 106: 4453–4458.
Gómez-Abellán P, Madrid JA, Ordovás JM, Garaulet M . Chronobiological aspects of obesity and metabolic syndrome. Endocrinol Nutr 2012; 59: 50–61 (in Spanish).
Garaulet M, Ordovás JM, Gómez-Abellán P, Martínez JA, Madrid JA . An approximation to the temporal order in endogenous circadian rhythms of genes implicated in human adipose tissue metabolism. J Cell Physiol 2011; 226: 2075–2080.
Loboda A, Kraft WK, Fine B, Joseph J, Nebozhyn M, Zhang C et al. Diurnal variation of the human adipose transcriptome and the link to metabolic disease. BMC Med Genomics 2009; 2: 7.
Ptitsyn AA, Zvonic S, Conrad SA, Scott LK, Mynatt RL, Gimble JM . Circadian clocks are resounding in peripheral tissues. PLoS Comput Biol 2006; 2: e16.
Tu BP, Kudlicki A, Rowicka M, McKnight SL . Logic of the yeast metabolic cycle: temporal compartmentalization of cellular processes. Science 2005; 310: 1152–1158.
Garaulet M, Madrid JA . Chronobiological aspects of nutrition, metabolic syndrome and obesity. Adv Drug Deliv Rev 2010; 62: 967–978.
Garaulet M, Corbalán MD, Madrid JA, Morales E, Baraza JC, Lee YC et al. CLOCK gene is implicated in weight reduction in obese patients participating in a dietary programme based on the Mediterranean diet. Int J Obes (Lond) 2010; 34: 516–523.
Garaulet M, Pérez-Llamas F, Zamora S, Tebar FJ . Weight loss and possible reasons for dropping out of a dietary/behavioural programme in the treatment of overweight patients. J Human Nutr Diet 1999; 12: 219–227.
Serra-Majem L, Aranceta J . SENC Working Group on Nutritional Objectives for the Spanish Population. Spanish Society of Community Nutrition. Nutritional objectives for the Spanish population. Consensus from the Spanish Society of Community Nutrition. Public Health Nutr 2001; 4: 1409–1413.
Cooper Z, Fairburn CG, Hawker DM . Cognitive-Behavioral treatment of obesity. A Clinician’s Guide. New York: The Guilford Press, 2003.
Ferrario VF, Sforza C, Schmitz JH, Miani A, Taroni G . Fourier analysis of human soft tissue facial shape: sex differences in normal adults. J Anat 1995; 187: 593–602.
Mataix J, Mañas M, Llopis J, Martínez E . (Table of Composition of Spanish Foods) Tabla De Composición De Alimentos Españoles (in Spanish). Instituto de Nutrición y Tecnología, Universidad de Granada: Granada, Spain, 1995.
Moreiras O, Carvajal A, Cabrera L . (Table of Composition of Spanish Foods) Tablas De Composición De Alimentos (In Spanish) In: Pirámide SA, ed. Madrid, Spain, 1995.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et alInternational Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis. Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645.
Pérez-Llamas F, Garaulet M, Herrero F, Palma JT, Pérez de Heredia F, Marín R et al. (Multivalent informatics application for studies of the nutritional status of the population. Assessment of food intake). Nutr Hosp 2004; 19: 160–166 (in Spanish).
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395.
Roman-Viñas B, Serra-Majem L, Hagstrom M, Ribas-Barba L, Sjostrom M, Segura-Cardona R . International Physical Activity Questionnaire: reliability and validity in a Spanish population. Eur J Sport Sci 2010; 10: 297–304.
Horne JA, Ostberg O . A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 1976; 4: 97–110.
Taillard J, Philip P, Chastang JF, Bioulac B . Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J Biol Rhythms 2004; 19: 76–86.
Garaulet M, Lee YC, Shen J, Parnell LD, Arnett DK, Tsai MY et al. CLOCK genetic variation and metabolic syndrome risk: modulation by monounsaturated fatty acids. Am J Clin Nutr 2009; 90: 1466–1475.
Garaulet M, Lee YC, Shen J, Parnell LD, Arnett DK, Tsai MY et al. Genetic variants in human CLOCK associate with total energy intake and cytokine sleep factors in overweight subjects (GOLDN population). Eur J Hum Genet 2010; 18: 364–369.
Sookoian S, Gemma C, Gianotti TF, Burgueño A, Castaño G, Pirola CJ . Genetic variants of Clock transcription factor are associated with individual susceptibility to obesity. Am J Clin Nutr 2008; 87: 1606–1615.
Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, Haim A et al. Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci USA 2010; 107: 18664–18669.
Hatori M, Vollmers C, Zarrinpar A, DiTacchio L, Bushong EA, Gill S et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab 2012; 15: 848–860.
Jakubowicz D, Froy O, Wainstein J, Boaz M . Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids 2012; 77: 323–331.
Sensi S, Capani F . Chronobiological aspects of weight loss in obesity: effects of different meal timing regimens. Chronobiol Int 1987; 4: 251–261.
Mistlberger RE, Lukman H, Nadeau BG . Circadian rhythms in the Zucker obese rat: assessment and intervention. Appetite 1998; 30: 255–267.
Lowden A, Moreno C, Holmbäck U, Lennernäs M, Tucker P . Eating and shift work—effects on habits, metabolism and performance. Scand J Work Environ Health 2010; 36: 150–162.
Ma Y, Bertone ER, Stanek EJ, Reed GW, Hebert JR, Cohen NL et al. Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol 2003; 158: 85–92.
Colles SL, Dixon JB, O’Brien PE . Night eating syndrome and nocturnal snacking: association with obesity, binge eating and psychological distress. Int J Obes (Lond) 2007; 31: 1722–1730.
Corbalán-Tutau MD, Madrid JA, Garaulet M . Timing and duration of sleep and meals in obese and normal weight women. Association with increase blood pressure. Appetite 2012; 59: 9–16.
Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L, Manios Y et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes (Lond) 2011; 35: 1308–1317.
Taheri S, Lin L, Austin D, Young T, Mignot E . Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004; 1: e62.
Baron KG, Reid KJ, Kern AS, Zee PC . Role of sleep timing in caloric intake and BMI. Obesity (Silver Spring) 2011; 19: 1374–1381.
Bienertová-Vasků J, Bienert P, Forejt M, Tomandl J, Brázdová Z, Vasků A . Genotype x nutrient association of common polymorphisms in obesity-related genes with food preferences and time structure of energy intake. Br J Nutr 2010; 103: 352–359.
Scheer FA, Morris CJ, Shea SA . The Internal Circadian Clock Increases Hunger and Appetite in the Evening Independent of Food Intake and Other Behaviors. Obesity (In Press).
Corbalán-Tutau MD, Madrid JA, Ordovás JM, Smith CE, Nicolás F, Garaulet M . Differences in daily rhythms of wrist temperature between obese and normal-weight women: associations with metabolic syndrome features. Chronobiol Int 2011; 28: 425–433.
Corbalán-Tutau D, Madrid JA, Nicolás F, Garaulet M . Daily profile in two circadian markers ‘melatonin and cortisol’ and associations with metabolic syndrome components. Physiol Behav 2012. e-pub ahead of print 15 June 2012.
Zhao Y, Zhang Y, Zhou M, Wang S, Hua Z, Zhang J . Loss of mPer2 increases plasma insulin levels by enhanced glucose-stimulated insulin secretion and impaired insulin clearance in mice. FEBS Lett 2012; 586: 1306–1311.
Konturek PC, Brzozowski T, Konturek SJ . Gut clock: implication of circadian rhythms in the gastrointestinal tract. J Physiol Pharmacol 2011; 62: 139–150.
Acknowledgements
This study was supported by grants from Tomás Pascual and Pilar Gómez-Cuétara Foundations, Spanish Government of Science and Innovation (BFU2011-24720), Séneca Foundation from the Government of Murcia (15123/PI/10). National Heart, Lung, and Blood Institute grants HL-54776, National Institute of Diabetes and Digestive and Kidney Diseases, grant number DK075030, and by contracts 53-K06-5-10 and 58-1950-9-001 from the US Department of Agriculture Research, and by National Heart, Lung, and Blood Institute grant R01 HL094806, and by National Institute of Diabetes and Digestive and Kidney Diseases, grant R21 DK089378.
Author contributions
MG, FAJLS designed the research; MG, PGA, JJAB, YCL, JMO conducted the research; MG, FAJLS analyzed data; MG, FAJLS wrote the paper; MG had primary responsibility for final content. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Garaulet, M., Gómez-Abellán, P., Alburquerque-Béjar, J. et al. Timing of food intake predicts weight loss effectiveness. Int J Obes 37, 604–611 (2013). https://doi.org/10.1038/ijo.2012.229
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.229
Keywords
This article is cited by
-
A genomics perspective of personalized prevention and management of obesity
Human Genomics (2024)
-
The role of insufficient sleep and circadian misalignment in obesity
Nature Reviews Endocrinology (2023)
-
Is time of eating associated with BMI and obesity? A population-based study
European Journal of Nutrition (2023)
-
Isocaloric diet is as effective as the hypocaloric diet in ameliorating symptoms in PCOS patients
International Journal of Diabetes in Developing Countries (2023)
-
Position statement on nutrition therapy for overweight and obesity: nutrition department of the Brazilian association for the study of obesity and metabolic syndrome (ABESO—2022)
Diabetology & Metabolic Syndrome (2023)