Abstract
Purpose:
The College of American Pathologists offers biannual proficiency testing for molecular analysis of fragile X syndrome. The purpose of this study was to analyze laboratory performance on the fragile X proficiency surveys from 2001 to 2009.
Methods:
Individual laboratory responses were analyzed for accuracy of genotype determination (normal, gray zone, premutation, or full mutation) and size analysis of the FMR1 trinucleotide repeat region. The analytical sensitivity and specificity of testing for fragile X were calculated, and laboratory performance for trinucleotide repeat sizing was evaluated.
Results:
Overall, laboratories demonstrated analytical sensitivity of 99% and 96% for detection of full mutations associated with fragile X syndrome in males and females, respectively; analytical sensitivity of 98% for detection of premutations; and analytical specificity of 99.9%. Size measurements of the CGG repeat region were acceptable from most laboratories, with an increase in the range of reported sizes observed for larger repeat expansions.
Conclusions:
Molecular genetic testing for fragile X syndrome demonstrated excellent sensitivity and specificity by laboratories participating in the College of American Pathologists (CAP) surveys. Allele sizing demonstrated good performance overall with improved accuracy over the study period. Participation in proficiency testing can aid laboratories in assessing individual performance and need for calibration of assays.
Genet Med 2012:14(3):306–312
Similar content being viewed by others
Introduction
The clinical phenotypes associated with expansion of the CGG trinucleotide repeats in the 5’ untranslated region (UTR) of the X-linked FMR1 gene (OMIM *309550) include fragile X–associated tremor/ataxia syndrome (FXTAS), premature ovarian insufficiency/failure (POI/POF), and fragile X syndrome.1 The normal size range of CGG repeats extends to 44 copies. The intermediate range (“gray zone”) is 45–54 repeats, for which expansion to a full mutation in the next generation has not been described, although there is increased instability compared with normal alleles and small, incremental expansions have been observed.2 The unstable, premutation range of 55–200 repeats is coupled with an increased risk of POI in females and the late-onset, progressive neurodegenerative condition FXTAS in males and, less often, females.3 In female premutation carriers, the risk of expansion to a full mutation in the next generation increases with the size of the premutation, with essentially 100% risk with greater than 100 repeats.4 Therefore, accurate diagnostic sizing in this range is essential for genetic counseling for risk of affected offspring. Triplet repeat expansions greater than 200 copies are classified as full mutations and are associated with transcriptional silencing of the FMR1 gene by methylation.5 Full mutations of FMR1 are associated with fragile X syndrome, the most prevalent inherited intellectual disability syndrome, affecting approximately 1:4,000 males and half as many females. The fragile X syndrome phenotype is characterized by typical but nonspecific manifestations including large ears and a long face, macro-orchidism after puberty, joint laxity, and a variety of cognitive and behavioral issues in the autism spectrum.6,7
Testing for fragile X–related disorders is performed using PCR-based methods and/or genomic Southern hybridization. These approaches are technically challenging because detection of alleles containing from tens to thousands of copies of CGG is difficult to achieve with a single analytical technique. With increasing CGG repeats, the DNA melting temperature also increases, thus limiting the efficiency of the PCR due to impaired DNA strand separation. Southern blot analysis can overcome this limitation but has limited resolution of accurate DNA fragment size. Triplet repeat expansions can demonstrate somatic variation within individual patients, and mosaicism of both size and methylation status may be present, particularly for the full-mutation alleles.5 Methylation status also affects the phenotypic expression of fragile X syndrome; therefore, laboratories must distinguish methylated from unmethylated alleles, usually by Southern blot analysis using methylation-sensitive restriction enzymes.
The College of American Pathologists (CAP) offers proficiency testing twice annually for fragile X–related phenotypes. Molecular diagnostic laboratories participate by performing the FMR1 molecular analyses routinely used in clinical diagnostic practice, either with laboratory-developed tests or commercial methods. The data are collected and summarized by the CAP with grading based on the accuracy of the genotype and the postanalytic interpretation. The CAP/American College of Medical Genetics (ACMG) Biochemical and Molecular Genetics Committee (BMGC) reviews the data and provides a summary of the results after each proficiency test. Any incorrect result is considered an unacceptable response by the laboratory. Laboratories that report an incorrect result in more than one consecutive survey receive a warning letter from the CAP and may lose CAP accreditation. The BMGC has performed a retrospective study over 9 years (2001–2009) to assess overall laboratory performance for this technically challenging test.
Materials and Methods
Samples tested
CAP proficiency testing for molecular analysis of fragile X syndrome was offered twice per year through the CAP MGL1 Molecular Genetics Survey. The BMGC selected samples of human cell lines derived from patients with specific FMR1 genotypes from the Coriell Institute for Medical Research Human Genetic Cell Repository database for analysis. The Coriell Institute grew the selected cell lines and provided isolated genomic DNA to the CAP for distribution to participating laboratories.
Collation of survey results
Laboratory responses to the CAP fragile X proficiency surveys from 2001 to 2009 were submitted via written or electronic reporting to the CAP. Each laboratory was assigned a unique identifier number. Responses were collated by the CAP and entered into a Microsoft Access database (Microsoft, Redmond, WA). Data from multiple years were summarized by the unique identifier and provided to the BMGC in blinded fashion in an Excel spreadsheet (Microsoft).
Analysis of laboratory performance for genotype determination
The results reported by each laboratory for the genotype (normal, gray zone, premutation, or full mutation) and triplet repeat size of each of the proficiency survey samples were analyzed. In addition, the biannual participant summary reports provided by the CAP BMGC to participating laboratories were reviewed. The percentage of responding laboratories reporting the correct genotype result for each sample and the analytical sensitivity and specificity for detecting premutation and full-mutation alleles were calculated. The 95% binomial proportion confidence intervals (CIs) were calculated using the exact method.
Analysis of allele sizing
For each of the survey samples, the mean, median, and standard deviation of the reported triplet repeat sizes were calculated using Microsoft Excel. Absurd values, defined by results likely due to transcription or entry errors such as “1” or “7,200” instead of “>200,” were removed prior to statistical analysis. Laboratory performance for fragment sizing analysis was based on variance from the median value; typically, the median did not vary significantly from the mean.
Analysis of Fragile Xperts data
For comparison purposes, FMR1 allele sizing data published by the Fragile Xperts Working Group of the Association for Molecular Pathology Clinical Practice Committee8 were provided by Jean Amos Wilson in a Microsoft Excel spreadsheet. The mean, median, standard deviation, and range of allele sizes generated were calculated using Excel.
Results
Between 2001 and 2009, an average of 90 laboratories participated each year in the CAP proficiency surveys for fragile X molecular genetic testing. The laboratories consisted primarily of US laboratories and a few international laboratories. The CAP provided annual data to the BMGC for analysis, when at least 80% of laboratories had submitted results.
Detection of normal alleles
During the study period, 37 samples that were negative for the FMR1 triplet repeat expansion were included in the CAP fragile X proficiency surveys. A total of 43 FMR1 alleles from male and female individuals were included with triplet repeat sizes in the normal range of 20 to 33 CGG repeats. Not all laboratories reported a repeat size for normal alleles because some only perform sizing analysis of samples with evidence of triplet repeat expansion. Interlaboratory concordance for the reported sizes of normal alleles was very good, with >90% of laboratories reporting results within two repeat copies of the median/mean result and >95% of laboratories reporting results within five repeats of the median/mean for the majority of these samples ( Table 1 ). A normal Gaussian distribution was observed for each of the survey samples with repeat sizes in the normal range (see figure in Supplementary Figure S1 online).
In each survey, >98% of laboratories correctly reported a normal result for each of the normal-range samples, regardless of whether they measured repeat size. The overall analytical specificity of fragile X testing was 99.9% (95% CI 99.66–99.96%) for repeat sizes ranging from 20 to 33 CGG repeats, the typical size from population controls. In 3 of 18 surveys, one or two laboratories incorrectly reported a premutation or full-mutation-sized allele. Each of these false-positive results could be attributed to switching with another sample from the same survey rather than analytical error. For the majority of surveys, 100% of participating laboratories correctly reported a normal genotype, demonstrating excellent specificity of fragile X testing.
Samples with 42 FMR1 CGG repeats (in the high-normal range) were included in several of the CAP proficiency surveys. These individuals are unaffected and do not have measurable risk for triplet repeat expansion in future generations. Triplet repeat sizing of samples with 42 CGG repeats produced a greater range of reported repeat sizes than for normal samples with smaller repeat sizes. Overall, 80–89% of responding laboratories reported repeat sizes within two repeats of the median value, and 89–98% reported repeat sizes within five repeats of the median value ( Table 1 ). Distribution plots of the repeat sizes reported by each laboratory demonstrated a normal Gaussian distribution for each of the 42-repeat samples, with a large range due to a few outlier laboratories that reported greater than five repeats outside the median values (see figure in Supplementary Figure S2 online). Specific laboratories that reported outlier sizing results differed among surveys, with the exception of two individual laboratories that were outliers in at least two separate surveys. Measurements of 42-repeat alleles appeared to improve over time, with an increasing percentage of laboratories reporting values within two repeats of the median result.
Most laboratories (average 82%, range 73–90%) correctly interpreted 42-repeat samples as within the normal range, but a significant percentage interpreted these samples as gray-zone (average 15%, range 0–26%) or premutation (average 3%, range 0–8%) alleles ( Figure 1 ). The overall clinical specificity of testing for samples with 42 repeats was 97%, with an average of 3% of laboratories reporting a false-positive premutation result. The reporting of a premutation decreased with time, from eight laboratories in 2002 to three in 2003, to one in 2005–2008 attributed to preanalytic sample switching. The false-positive rate was largely attributed to interpretive error rather than analytical error because only three (27%) laboratories that reported a premutation actually measured repeat size within the premutation range. The remaining laboratories either did not report repeat size (four laboratories) or reported sizes in the normal (two laboratories) or gray-zone (one laboratory) ranges. Laboratories that measured a repeat size in the premutation range decreased over the years analyzed, suggesting that outlier laboratories may have improved calibration for sizing analysis. In 2002, more laboratories chose “premutation” as a genotype response than in more recent years, during which “gray zone” was added as a response category.
Some laboratories (14–26%) interpreted samples with 42 repeats as gray-zone alleles ( Figure 1 ). These are not considered false-positive results in this analysis because alleles in the gray-zone range have no measurable risk of expansion to a full mutation in the next generation. The increased range of sizes reported for alleles with 42 repeats compared with those in the typical normal range contributed to an overcalling of the gray-zone category. However, most gray-zone results correlated with a repeat size measurement within the normal range (up to 44 repeats). This may represent confusion among laboratories with the definition of the gray-zone category, which has changed over time as more information regarding repeat instability and risk of expansion has been obtained.
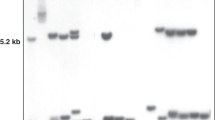
Diagnosis of fragile X syndrome
Affected males with fragile X syndrome typically have a single FMR1 allele with greater than 200 CGG repeats and complete methylation of the FMR1 promoter region. From 2001–2009, seven challenges included samples from affected males with FMR1 repeat sizes ranging from approximately 300 to 1,000 triplet repeats. Greater than 97% of participating laboratories (97–100% per survey, average 99%) correctly reported the presence of a full mutation for each of the samples from males with fragile X syndrome ( Figure 2 ). A small percentage (<3%) of laboratories reported an incorrect result (premutation or normal) in a single survey, with some errors attributed to sample switching rather than analytical error. Identification of full mutations in samples from females was not as good, with 96% (range 95–96%) of laboratories correctly determining the presence of a full mutation, 1.2–1.3% reporting a premutation, and 2.5–3.5% reporting a normal result ( Figure 2 ). The overall analytical sensitivity for detection of full mutations associated with fragile X syndrome was 99% in males (95% CI 98.1–99.7%) and 96% in females (95% CI 91.5–98.3%).
Sizing analysis of full-mutation alleles demonstrated a greater range of reported sizes than for smaller sized alleles. This was not unexpected because Southern blot analysis, the technique most frequently employed for detection of full-mutation alleles, has lower resolution than PCR sizing of smaller alleles. Many laboratories reported that they do not routinely measure repeat size of full-mutation alleles. The reported triplet repeat sizes for full-mutation alleles demonstrated a normal Gaussian distribution with a large range, with larger alleles demonstrating the widest ranges (see figure in Supplementary Figure S3 online). Despite the large range in sizes, at least 83% of responding laboratories (average 88%, range 83–92%) reported results within two standard deviations from the median, and the majority of reported sizes were within 50 repeats of the median results.
Detection of premutation alleles
From 2001 to 2009, a total of eight premutation samples from male and female patients were distributed in the fragile X proficiency surveys ( Figure 3 ). Five of these surveys included samples with approximately 90 repeats, which is close to the upper limit of detection for most capillary electrophoresis PCR sizing techniques. For these samples, at least 95% of laboratories in each survey (average 98%, range 95–100%) correctly determined the presence of a premutation ( Figure 3 , top panel). The overall analytical sensitivity for detection of premutations with approximately 90 CGG repeats was 98% (95% CI 97.1–98.2%). The excellent detection rate indicates that laboratories participating in CAP proficiency testing can detect premutation alleles near the analytical limits of most FMR1 PCR assays, although some may use Southern blot analysis as a screening method.
Genotype results for premutation samples. The genotypes reported by participating laboratories for samples with a premutation-size allele are depicted. In the top panel, the bar graph represents the percentage of laboratories reporting each genotype result for the surveys that included a premutation sample with approximately 90 repeats. In the bottom panel, the percentage of laboratories reporting each genotype result is shown for the surveys that included unusual female premutation samples with either skewed methylation or an unusually large degree of size mosaicism.
Three of the proficiency surveys included unusual samples from female premutation carriers. One unusual sample was a premutation mosaic sample with reported repeat sizes ranging from 80 to over 200 repeats. This sample demonstrated an unusual extent of size mosaicism, which does not reflect typical clinical samples with premutation alleles in this size range and may have been an artifact generated through repeated in vitro cell passages. One limitation of a proficiency testing program of this scope is the use of cell line samples rather than primary specimens to produce a sufficient amount of DNA for large-scale distribution. The analytical sensitivity for detection of this premutation was good, with 90% of laboratories correctly reporting either a premutation or mosaic and 8% of laboratories reporting a full mutation, likely due to the detection of fragments in the >200 repeat range ( Figure 3 , bottom panel). Only two laboratories (2.2%) failed to detect the expansion and reported a normal result; this may have been due to failure to amplify the expanded allele by PCR and/or failure to identify the broad smear observed in Southern blot analysis as an expanded allele in this unusual mosaic sample.
Another challenging premutation sample used in two separate surveys was from a female carrier of an allele with approximately 78 repeats, which also demonstrated a skewed methylation pattern in which the expanded allele was almost completely methylated instead of demonstrating the typical ~50% methylation. Although some female premutation carriers may exhibit skewed or unequal methylation, this extreme skewed methylation for FMR1 is not typically observed. Most laboratories correctly reported the presence of a premutation. However, a significant percentage (18 and 28% in the two surveys) reported a normal result ( Figure 3 , bottom panel). This high false-negative rate may have been due to the unusual pattern observed using methylation-sensitive Southern blot analysis, which lacked the unmethylated, expanded DNA fragment typically seen in female premutation samples. More laboratories successfully detected this premutation in 2007 compared with 2002 (75 vs. 66%).
Accurate sizing of premutation alleles is important in determining the risk for expansion to a full mutation in the offspring of female carriers. For the five premutation samples with 90 repeats, repeat sizes were reported by only 80–90% of laboratories, although >95% of laboratories reported detection of a premutation allele. Overall, the range of sizes reported for premutation alleles was broader than the range demonstrated for normal alleles ( Table 1 ). Interlaboratory results for sizing premutation alleles with 90 repeats demonstrated a normal distribution, with the majority of laboratories (average 86%, range 74–91%) reporting a repeat size within 10 repeats of the median result and more than half of respondents (average 69%, range 54–78%) reporting a result within 5 repeats of the median result (see figure in Supplementary Figure S4 online). Sizing of the premutation allele with skewed methylation demonstrated similar accuracy, with 77–80% of reported results within 10 repeats of the median and 63% of results within 5 repeats of the median (data not shown). Premutations of other sizes have not been tested systematically, in part, because there are very few available cell lines with well-characterized premutation alleles. In addition, this large, interlaboratory proficiency testing program limits the number of samples that can be distributed for each challenge at a reasonable cost. The recent addition of well-characterized samples of known repeat size to a readily available cell repository collection may support proficiency testing of other premutation alleles in the future.8
Sizing performance for the 90-repeat premutation alleles improved over time, with the percentage of laboratories reporting results within five repeats of the median value increasing from 54% in 2003 to 78% in 2008 ( Table 1 ). Over the time period analyzed, an increased percentage of laboratories using PCR for allele sizing reported using capillary electrophoresis rather than a gel-based method to measure repeat size (from 7% in 2001 to 80% in 2009), which may account in part for the observed improvement in overall sizing performance. However, there was no direct correlation between reported method(s) and poor sizing performance by individual laboratories, indicating that laboratory error or poor assay calibration was likely a major source of inaccurate allele sizing. There was no significant difference in sizing performance between US and non-US laboratories (data not shown).
Fragile Xperts data
A recent publication by the Fragile Xperts Working Group of the Association for Molecular Pathology Clinical Practice Committee reported the results of ten laboratories experienced in fragile X testing, with a goal to determine a consensus repeat size for several cell line samples to be available as resources for laboratories to calibrate their sizing assays.8 For comparison purposes, the sizing of FMR1 triplet repeats by the Fragile Xperts group was analyzed in the same manner as the CAP survey data. The Fragile Xperts sizing results were similar to the CAP proficiency surveys, with an increased range of sizes reported for larger repeat sizes, although the interlaboratory concordance for sizing premutation alleles was somewhat better than that of the survey sites. Analysis of the raw data generated by the Fragile Xperts indicated that ~90% of results were within two repeats of the mean/median for normal alleles with 20–31 repeats, within three repeats of the mean for alleles with 41–46 repeats, and within five repeats of the mean for a 54-repeat allele (data not shown). For premutation-size alleles, >90% of results were within five repeats of the mean for four samples with 73–87 repeats and within ten repeats of the mean for four samples with 98–118 repeats. The interlaboratory concordance for sizing was better when each of these laboratories used the same commercially available PCR reagents.
Discussion
Molecular genetic testing for fragile X–related disorders is complicated due to the CG-rich DNA sequence of the triplet repeat region, the large variation in the size of CGG expansions, and the need for accurate sizing of triplet repeats in the premutation range in order to predict the risk of expansion to a full mutation. Overall performance by laboratories participating in the CAP fragile X proficiency challenges between 2001 and 2009 was very good. The analytical sensitivity for detection of full mutations associated with fragile X syndrome was 99% in males (95% CI 98.1–99.7%) and 96% in females (95% CI 91.5–98.3%). The analytical sensitivity for detection of premutations was 98% (95% CI 97.1–98.2%), and the analytical specificity of testing was 99.9% (95% CI 99.66–99.96%).
The lower analytical sensitivity for detection of full mutations in females was primarily due to the reporting of a normal result by 2–3% of laboratories, indicating that a small percentage of laboratories failed to detect the expanded FMR1 allele in females. Molecular diagnosis of fragile X syndrome in females is more challenging than in males due to the presence of a normal FMR1 allele on one X chromosome. A single allele identified by PCR analysis in a female patient could be explained by the presence of two alleles homozygous for the same repeat number or of an expanded allele that is too large to be efficiently amplified by available PCR assays. Thus, detection of only one normal allele by PCR in a full-mutation carrier female could be incorrectly characterized as a normal male (or normal female) due to failure to identify the second, expanded allele. False-negative results in females could be minimized by Southern blot analysis of all samples or of any female samples with only one DNA fragment detected by PCR. For most of the CAP survey challenges, the gender of the patients was not indicated. As most clinical laboratories request patient demographic information prior to testing, this error rate might be lower in actual laboratory practice. As more laboratories adopt newer PCR techniques capable of amplifying full-mutation alleles, it is possible that false-negative results in females will be further minimized.9,10,11
Accurate sizing of the FMR1 trinucleotide repeat region has implications for risk assessment of premutation carriers and for determination of the correct genotype, particularly for alleles at the borders of the genotype (normal, gray zone, premutation, full mutation) categories. Measurement of FMR1 repeat size by PCR amplification is typically performed utilizing primers that flank the CGG triplet repeat region and evaluation of the size of the resulting PCR products by gel or capillary electrophoresis with fragment-size standards. However, accurate sizing by PCR amplification of the FMR1 triplet repeat region is inherently difficult due to the high melting temperature of CG-rich regions and the repetitive sequence of the region, which may produce expansions or deletions during PCR amplification. The larger the repeat region, the more difficult accurate sizing becomes. Direct DNA sequence analysis to determine the number of repeats is technically difficult for the same reasons, especially for larger premutation and full-mutation samples. Thus, the accuracy of FMR1 repeat analysis is challenging to measure in the absence of a robust, gold standard assay.
The survey results illustrate the increased difficulty of size analysis for larger alleles. Sizing of triplet repeats demonstrated good interlaboratory concordance overall, with a significant increase in interlaboratory size range observed with increasing repeat size. The range of repeat sizes reported for premutation-size alleles has implications for genetic counseling of premutation carriers. For premutation carriers with 90 repeats, results varying from 80 to 100 repeats would be associated with a predicted 58% to 100% risk of expansion.4 These risk estimates are based on the average incidence of expansion in female carriers with varying repeat sizes in 10-repeat increments and were generated in a single laboratory; interlaboratory variability in repeat size determination may challenge these generalizations. In addition, the increased risk of expansion associated with increasing repeat size in premutation carriers is not stepwise, but a continuum. For example, female carriers with 80 repeats have a significantly increased risk of expansion over those with 69 repeats, whereas those with 70 repeats likely have no increased risk over those with 69 repeats, despite the higher published risk estimates for individuals with 70–79 repeats compared with 60–69 repeats. Individuals interpreting and providing counseling to patients for fragile X testing should recognize the inexact nature of triplet repeat sizing in the premutation range and convey the inexact nature of risk estimates for premutation-size categories.
Ideally, the interlaboratory concordance of triplet repeat measurement in the premutation range would be better than currently observed. Quantitative testing of any analyte is challenging to standardize in clinical laboratories, and historically there has been much effort to standardize quantitative assays using calibration standards and controls. The Fragile Xperts project demonstrated better interlaboratory sizing concordance when each of the laboratories used the same commercially available platform. Therefore, the overall concordance of FMR1 triplet repeat sizing may improve with the recent increase in commercially available standardized fragile X PCR assays, although the availability of multiple commercial reagents and different interlaboratory assay configurations may contribute to interlaboratory variability.10,11 Premutation repeat fragment sizing has improved over time, with a smaller range of repeat sizes reported and a smaller percentage of laboratories reporting outlier results, suggesting that many laboratories may have gained more experience and improved or recalibrated their assays. The overall improvement in allele sizing may be a result of participation in proficiency testing, the increased use of capillary electrophoresis over gel electrophoresis for PCR analysis, and/or the recent availability of characterized cell lines and of standard reference materials from the National Institute of Standards and Technology.8,12 However, some laboratories still report outlier size values for premutation alleles. Laboratories performing diagnostic molecular fragile X testing are highly encouraged to calibrate their FMR1 PCR sizing assays using controls of known repeat size.
Due to the decreased resolution of sizing by Southern blot analysis, measurement of repeat sizes larger than can be detected by PCR (typically 90–100 repeats) is inherently less accurate than for smaller alleles. This is demonstrated by the increased range of sizes measured by participating laboratories for full-mutation samples. The difficulty of sizing large CGG repeats underscores the importance of analyzing methylation status to determine the presence of a full mutation, especially for samples at the threshold of the premutation to full-mutation range. Interpretation can be complicated by the presence of size and methylation mosaicism, which may be differentially represented in the peripheral blood and the central nervous system. More accurate measurement than can be achieved by Southern blot analysis is not clinically relevant for greater than 100 repeats because virtually all premutation alleles over this size will expand to a full mutation when transmitted from a female carrier, and full mutations (>200 repeats) with complete methylation are associated with fragile X syndrome regardless of size.
In summary, overall performance by laboratories participating in the CAP proficiency surveys for molecular fragile X testing demonstrated excellent analytical sensitivity and specificity. Sizing of the FMR1 triplet repeat region demonstrated good performance overall for quantitative measurement of a complex CG-rich repeat region and improved over the time frame analyzed. Some laboratories are performing sizing analyses poorly, which is most clinically relevant in the premutation range. With well-characterized calibration materials, interlaboratory concordance for sizing premutation alleles may improve, which would help provide more accurate risk assessment for patients. Participation in proficiency testing is useful for laboratories to compare individual performance with other laboratories and to identify need for recalibration of assays.
Disclosure
The authors declare no conflict of interest.
References
Hagerman PJ, Hagerman RJ . The fragile-X premutation: a maturing perspective. Am J Hum Genet 2004;74:805–816.
Fernandez-Carvajal I, Lopez Posadas B, Pan R, Raske C, Hagerman PJ, Tassone F . Expansion of an FMR1 grey-zone allele to a full mutation in two generations. J Mol Diagn 2009;11:306–310.
Hagerman RJ, Leavitt BR, Farzin F, et al. Fragile-X-associated tremor/ataxia syndrome (FXTAS) in females with the FMR1 premutation. Am J Hum Genet 2004;74:1051–1056.
Nolin SL, Brown WT, Glicksman A, et al. Expansion of the fragile X CGG repeat in females with premutation or intermediate alleles. Am J Hum Genet 2003;72:454–464.
Maddalena A, Richards CS, McGinniss MJ, et al. Technical standards and guidelines for fragile X: the first of a series of disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics. Quality Assurance Subcommittee of the Laboratory Practice Committee. Genet Med 2001;3:200–205.
Hagerman RJ . Lessons from fragile X regarding neurobiology, autism, and neurodegeneration. J Dev Behav Pediatr 2006;27:63–74.
Jacquemont S, Hagerman RJ, Hagerman PJ, Leehey MA . Fragile-X syndrome and fragile X-associated tremor/ataxia syndrome: two faces of FMR1. Lancet Neurol 2007;6:45–55.
Amos Wilson J, Pratt VM, Phansalkar A, et al.; Fragile Xperts Working Group of the Association for Molecular Pathology Clinical Practice Committee. Consensus characterization of 16 FMR1 reference materials: a consortium study. J Mol Diagn 2008;10:2–12.
Strom CM, Huang D, Li Y, et al. Development of a novel, accurate, automated, rapid, high-throughput technique suitable for population-based carrier screening for Fragile X syndrome. Genet Med 2007;9:199–207.
Lyon E, Laver T, Yu P, et al. A simple, high-throughput assay for Fragile X expanded alleles using triple repeat primed PCR and capillary electrophoresis. J Mol Diagn 2010;12:505–511.
Chen L, Hadd A, Sah S, et al. An information-rich CGG repeat primed PCR that detects the full range of fragile X expanded alleles and minimizes the need for southern blot analysis. J Mol Diagn 2010;12:589–600.
National Institute of Standards and Technology. Fragile X Human DNA Triplet Repeat Standard Reference Material. https://www-s.nist.gov/srmors/view_detail.cfm?srm=2399. Accessed 24 August 2011.
Acknowledgements
We thank Rodrigo Ranola and Jacques Mobille from the College of American Pathologists for providing collated data from the CAP fragile X proficiency surveys and Jean Amos Wilson for providing data from the Fragile Xperts Working Group of the Association for Molecular Pathology Clinical Practice Committee.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Weck, K., Zehnbauer, B., Datto, M. et al. Molecular genetic testing for fragile X syndrome: laboratory performance on the College of American Pathologists proficiency surveys (2001–2009). Genet Med 14, 306–312 (2012). https://doi.org/10.1038/gim.2011.11
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2011.11
Keywords
This article is cited by
-
Some economics on personalized and predictive medicine
The European Journal of Health Economics (2015)