Abstract
Purpose
To document the etiology, clinical presentation, and visual prognosis of optic neuritis in Taiwanese children.
Methods
Retrospectively reviewed children younger than 18 years old with optic neuritis in Chang Gung Memorial Hospital and Chang Gung Children’s Hospital from 1998 to 2009.
Results
There were 24 children (38 eyes) with optic neuritis in that period. Overall, 14 patients (58.3%) were female and 10 patients (41.7%) were male. In total, 14 patients (58.3%) had bilateral involvement, and 10 patients (41.7%) had unilateral involvement. Out of 38 eyes, 24 (63.2%) had disc swelling. Out of 24 patients, 21 (87.5%) underwent intravenous steroid therapy (10 to 30 mg/kg/day) for 3–5 days, and followed by an oral taper. Out of 24 patients, 20 (83.3%) achieved final visual acuity (VA) of 20/40 or better. However, a poor visual outcome (four patients) (VA<20/40) was correlated with pale disc at presentation (P=0.002, Pearson χ2-test) and age older than 10 years (P=0.012, Fisher’s exact test). Five patients were diagnosed with acute disseminated encephalomyelitis (ADEM) (21%), and three patients were diagnosed with multiple sclerosis (MS) (12.5%). Patients with ADEM did not have a better visual outcome than patients with MS (P=0.643, Fisher’s exact test).
Conclusions
Visual recovery from optic neuritis was favorable in Taiwanese children. A poor visual outcome was correlated with pale disc at presentation and patients’ age older than 10 years. ADEM is the most common associated systemic disease; MS is relatively rare.
Similar content being viewed by others
Introduction
The visual prognosis of patients with optic neuritis has been well studied by the Optic Neuritis Treatment Trial (ONTT).1, 2, 3 Benefit from treatment with intravenous steroid in prevention from multiple sclerosis (MS) has also been extensively analyzed.4, 5, 6, 7 However, these studies were mostly confined to young adults. Optic neuritis in children is considered to be a totally different entity in contrast to adults. Children with optic neuritis usually experience better visual recovery, they also have more bilateral involvement and optic disc swelling, and carry a relatively low risk of subsequent MS as well.8, 9, 10 However, there have been accumulating reports with different clinical characteristics of optic neuritis and MS in Europe,11, 12 North America,8, 9, 13 and Asia.14, 15, 16, 17 Herein we report a retrospective study to evaluate the clinical characteristics of children with optic neuritis in Taiwan. Meanwhile, the specific aim of this study was to statistically document the factors relevant to visual prognosis in optic neuritis in children.
Patients and methods
The medical records of all patients younger than 18 years old, who came to Linkou Chang Gung Memorial Hospital and Chang Gung Children’s Hospital from 1998 to 2009, with a diagnosis of optic neuritis were retrospectively reviewed. This study was approved by the Institutional Review Board at Chang Gung Memorial Hospital. The diagnosis of optic neuritis was made on the basis of history of visual loss and some of the clinical findings including afferent pupillary defect, visual field defect, optic disc appearance, color vision defect, and abnormal visual-evoked potentials. Patients with hereditary optic neuropathy, systemic vascular diseases, compressive optic neuropathy, and malignancy were excluded from this study. Optic neuritis was recorded as unilateral or bilateral. Bilateral simultaneous disease was defined as both eyes being affected within 1 month of each other, and bilateral recurrent disease was defined as one or both eyes being affected more than once.
Information about the sex, age of onset, laterality (unilateral or bilateral), initial visual acuity (VA), final VA, cerebrospinal fluid (CSF) findings, therapy, recent infections and immunizations, image study including computer tomography (CT) or magnetic resonance imaging (MRI), and associated systemic diseases such as MS or acute disseminated encephalomyelitis (ADEM) was obtained.
For statistical analysis, the initial VA and final VA were taken as best-corrected VA (BCVA). A logarithmic transformation of decimal VA was used a scattergram. Eyes without formed vision were classified into one of four low-vision categories, which were assigned decimal equivalents as follows: counting fingers=0.00500; hand motion=0.00250; light perception=0.00125; and no light perception=0.00100.18 The logarithm of reciprocal decimal VA was used to approximate the logarithm of minimal angle of resolution (log MAR). All statistical analyses were conducted using SPSS software (Standard Windows version 15.0, SPSS, Chicago, IL, USA). All P-values quoted were two-tailed and were considered statistically significant when they were less than 0.05.
Results
As shown in Table 1, 24 patients (38 eyes) were included in this study; their ages ranged from 5 to 17 years. The mean age at presentation was 10.08±4.15 years. Follow-up period ranged from 1 week to 12 years, with a mean of 14.01 months (median: 2.5 months). There were 14 female patients (58.3%) and 10 male patients (41.7%). Fourteen patients (58.3%) had bilateral disease, and ten patients (41.7%) had unilateral disease. In addition, 14 patients (58.3%) had afferent pupillary defect, and 24 eyes (63.2%) had disc swelling. Of 16 eyes (42.1%) performed visual field examination, 14 eyes had visual field defect, and generalized suppression was the most common type. Of 21 eyes (55.3%) performed color vision test, 19 eyes had color vision defect. Of 23 eyes (60.5%) performed visual evoked potential test, 19 eyes had abnormal visual evoked potential. Out of 24 patients, 21 (87.5%) underwent intravenous steroid therapy. Of these 21 patients, 19 patients received methylprednisolone therapy (10–30 mg/kg/day) for 3–5 days, and followed by oral prednisolone 1 mg/kg/day for 2–4 weeks, the other 2 patients received dexamethasone therapy (5 mg, q6 h for 7 days, followed by tapering from q8 h, q12 h to qd). Of 10 patients (41.7%) performed CSF analysis, 8 patients had normal CSF findings. Of seven patients further tested for oligoclonal band in CSF and calculated IgG index, none had oligoclonal band. One patient had IgG index over 0.66 (0.792) and developed MS. In addition, two patients diagnosed with ADEM had proof of recent viral infection by CSF study and by serological test, respectively. These details of patients’ information are summarized in Table 2.
Effect of initial VA on final VA
There was a significant difference between initial VA (logMAR) and final VA (logMAR) in our patients (P≤0.001, Wilcoxon signed-ranks test), indicating good visual recovery in pediatric patients with optic neuritis. Initial VA ranged from 20/20 to no light perception. Out of 38 eyes, 19 (50%) had initial VA better than 20/4000 (above counting fingers) at presentation, and 19 of 38 eyes (50%) had initial VA worse than 20/4000 (counting fingers or below) at presentation. Eyes with initial VA better than 20/4000 did not have better final VA (VA ≥20/40) than those with initial VA worse than 20/4000 (P=1.00, Fisher’s exact test).
Effect of gender on final VA
In this study, 20 of 24 patients (83.3%) achieved final VA of 20/40 or better. Of the 20 patients with final VA of 20/40 or better, 12 patients were female and 8 patients were male. Statistical analysis for final visual outcome in female group vs male group did not demonstrate a significant difference (P=0.563, Fisher’s exact test).
Effect of laterality on final VA
Out of 14 patients, 12 (85.7%) in the bilateral group attained final VA of 20/40 or better, 8 of 10 patients (80%) in the unilateral group achieved final VA of 20/40 or better. The statistical analysis revealed no significant difference in visual outcome between patients with bilateral diseases and unilateral diseases (P=0.563, Fisher’s exact test).
Effect of disc appearance on final VA
The values of final VA (logMAR) in the three groups were significantly different (P=0.025, Kruskal–Wallis test). Non-parametric post-hoc comparisons indicated that final VA in the pale disc group was significantly poorer than that in the swelling disc group (P=0.016) and normal disc group (P=0.022). There was no difference in final VA between the swelling disc group and normal disc group (P=0.352) (Mann–Whitney U-test). Out of 24 eyes, 20 (83.3%) with swelling disc at presentation achieved final VA of 20/40 or better, 9 of 11 eyes (81.8%) with normal disc at presentation achieved final VA of 20/40 or better, and none of 3 eyes (0%) with pale disc at presentation attained final VA of 20/40 or better. There was a statistically significant trend toward a poorer visual outcome in eyes with pale disc at presentation (P=0.005, Pearson χ2-test).
Effect of age at presentation on final VA
Subgroup analysis was performed on the visual outcome in patients 10 years of age or younger and those 11 years of age or older at presentation. All of the 15 patients (100%) who were 10 years of age or younger achieved final VA of 20/40 or better; five of nine patients (55.6%) who were 11 years of age or older achieved final VA of 20/40 or better. There was a statistically significant better visual outcome in children younger than 10 years of age (P=0.012, Fisher’s exact test).
Effect of systemic association on final VA
Five patients were diagnosed with ADEM, and four of these five patients (80%) achieved final VA of 20/40 or better. Three patients were diagnosed with MS, and two of these three patients (66.7%) attained final VA of 20/40 or better. Statistical analysis for visual outcome in ADEM vs MS group, and patients with ADEM vs patients without ADEM demonstrated that there were no significant difference (P=0.643, and 0.635, respectively, Fisher’s exact test).
Regression analysis for final VA
We further divided patients into unilateral and bilateral groups for assessment of all above factors in final VA. In the unilateral group, there is a significant relationship between age and final VA, with a 1-year increase in age being associated with an increase of 0.034 log MAR in final VA (P=0.013, multiple linear regression analysis) after adjusting for initial VA. Meanwhile, the relationship between disc appearance at presentation and final VA is highly significant in the bilateral group, with a decrease of 1.646 log MAR in final VA in normal disc group (P=0.001) and a decrease of 1.489 log MAR in final VA in swelling disc group (P=0.002), after adjusting for initial VA (multiple linear regression analysis).
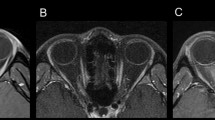
Neuroimaging
Of 24 patients, MRI of the brain was performed in 19 patients. Computed tomography of the brain was performed in three patients. Out of 19 patients, 11 (57.89%) had abnormal MRI findings, including only optic nerve enhancement in 2 patients, combined optic nerve enhancement with cerebral white matter lesion in 2 patients, and multiple cortical white matter lesions in the brain or spinal cord in 7 patients. In eight patients with normal MRI of the brain, the images all revealed well visualization of bilateral optic nerve and optic pathway without definite abnormal signal intensity or contrast enhancement. Interestingly, of these eight patients with normal optic nerve appearance in MRI, five patients (62.5%) had disc swelling, and the other three patients (37.5%) had normal optic disc. In contrast, of four patients having abnormal enhancement of optic nerve in MRI in this study, two patients (50%) had disc swelling and the other two patients (50%) had normal optic disc. Taken together, it indicated that appearance of optic disc might not correlate well with optic nerve appearance in image study. Of 11 patients having abnormal MRI findings, 8 patients (72.7%) achieved final VA of 20/40 or better. All three patients performing CT of the brain had normal findings. Of a total 11 patients having normal image study (MRI or CT), 10 patients (90.9%) achieved final VA of 20/40 or better. There was a trend toward better visual outcome in children with normal image study, but there was no statistically significant difference (P=0.586, Fisher’s exact test). The factors for visual prognosis in pediatric optic neuritis in this study are summarized in Table 3.
Discussion
The visual prognosis and clinical features of pediatric optic neuritis has been described previously.8, 11, 12, 14, 15, 17, 19 According to these reports, 77–90% of patients attained final VA of 20/40 or better. In addition, optic neuritis in childhood had more bilateral, female involvement, disc swelling at presentation, and was frequently associated with preceding viral infection. In our study, 83.3% of our patients achieved final VA of 20/40 or better, suggesting favorable visual recovery in Taiwanese children. Our study further confirms previous clinical features of optic neuritis in children such as more bilateral, female involvement and disc swelling at presentation (Table 4). However, older mean age, lower preceding febrile illness, and a relatively lower development rate of MS were noted in Taiwanese children. ADEM is the most common associated systemic disease in current study.
Accumulating evidences have reported some factors relevant to better visual outcome in pediatric optic neuritis. For instance, unilateral involvement,9 normal MRI of the brain, and children 6 years of age or younger appeared to have a better visual prognosis.8 Compared with a previous study, there was no significant difference in visual outcome between children with unilateral involvement and bilateral involvement in our study. Although we also found a trend toward children with normal image study seeming to have a better visual outcome, there was no statistically significant difference. Nevertheless, we demonstrated that children younger than 10 years old significantly had a better visual prognosis. Furthermore, the younger the age, the better the final VA was in children with unilateral involvement as shown by regression analysis.
Optic atrophy has been identified in 85% of pediatric optic neuritis and does not have a strict correlation with VA.20 In our study, we found that children with pale disc at presentation significantly had a poorer visual outcome than children with normal or swelling optic disc at presentation. In addition, we also found that disc changes at presentation in bilateral disease were more important for predicting final VA. Patients with pale disc at presentation significantly had poor final VA; it is possible that pale disc at presentation might result from a previous unknown episode of optic neuropathy or delayed diagnosis of optic neuritis. In this study, one patient (number 18) experienced three episodes of optic neuritis in each eye. This patient ended up with pale optic disc and showed less favorable visual recovery compared with the other two patients (number 6 and 7) who experienced two episodes of optic neuritis. Therefore, the number of attacks of optic neuritis might be also an important factor for less favorable visual recovery. However, significant improvement of final vision was noted in most of our patients, regardless of initial vision, indicating the nature of better visual recovery in pediatric optic neuritis.
ADEM is a monophasic, multifocal, inflammatory disease of the central nervous system, and is considered to be a demyelinating illness of probable autoimmune etiology. It often occurs after recent viral infections or vaccination,21 but it can also develop without an apparent preceding condition.22 The acute neurological signs and symptoms may include headache, fever, vomiting, altered level of consciousness, seizures, motor and/or sensory deficits, cerebellar ataxia, and cranial nerve palsy.23, 24 Of five patients with ADEM in our study, two patients (40%) had fever, one patient (20%) had seizure, and two patients (40%) had preceding viral infection.
Optic neuritis is not uncommon in children with ADEM.25, 26 Optic neuritis in children with ADEM often is bilateral and associated with optic disc edema.27, 28 Meanwhile, the efficacy of intravenous steroid therapy was proved to be beneficial for ADEM.23, 24, 26, 29 Excellent response to steroid therapy in visual improvement and reduction of demyelinating lesions on MRI without recurrence in children with ADEM have also been reported.27, 28, 30 In our study, disc swelling at presentation was noted in three of five patients (60%) with ADEM, and bilateral optic neuritis was noted in two of five patients (40%) with ADEM. In addition, all of the patients with ADEM received steroid pulse therapy. Four of five patients (80%) with ADEM achieved final VA of 20/20, and the other one patient achieved a final VA of 20/50. Our results seem to be comparable to previous reports. However, the limitation of our study was that most of our patients received intravenous steroid pulse therapy and there was no control group for comparison. It is still unknown whether intravenous steroid pulse therapy had a beneficial effect on visual recovery in pediatric optic neuritis, and in pediatric optic neuritis with ADEM.
The risk for developing MS after optic neuritis in children has been well studied. Lucchinetti et al31 reported that 13% of the patients with isolated optic neuritis had progressed to clinically or laboratory-supported definite MS by 10 years of follow-up, 19% by 20 years, 22% by 30 years, and 26% by 40 years. Meanwhile, the presence of bilateral sequential or recurrent optic neuritis increased the risk of developing MS. In addition, the presence of HLA-DR2 antigens,11 and unilateral disease have also been reported to be the other risk factors.9, 11 However, the rate of developing MS after pediatric optic neuritis also varied with race (Table 4). In comparison with other Asian countries, the rate of developing MS was 12.5% in our study, which was higher than Korean (4%),15 and Thai (9.1%),14 but was much lower than that reported in Japanese (31.7%),17 and another recent Korean study (25%).19 One of the reasons for wide range of conversion rate in each study might be due to different follow-up period. Two of three patients who developed MS in our study had concurrent bilateral papillitis, the third patient had bilateral sequential and recurrent retrobulbar optic neuritis. Our finding was compatible with the observation from previous reports.8, 31 In this study, all these three patients with MS had bilateral optic neuritis, indicating that a bilateral disease might be a risk factor for developing MS.
The differentiation between MS and ADEM has an important prognostic implication, but is sometimes difficult. MS frequently recurs and results in progressive deterioration over many years, whereas ADEM is usually a monophasic disease from which there is generally complete recovery. In addition, MS is rarely associated with a preceding viral infection.32 MRI is the imaging of choice in diagnosis of ADEM, and is beneficial in the distinction from MS.33 In our study, the visual outcome in the ADEM group was not different from that in the MS group, which might be due to too small a number of patients in these two groups to achieve a statistically significant difference. Further investigation for collecting more patient number in these two groups and a prospective data collection for a considerable length of time should be needed.
There are some drawbacks in this study. First, the follow-up period was very wide. Overall, 13 patients (54.2%) were followed up within 3 months, 18 patients (75%) were followed up within 12 months, and 21 patients (87.5%) were followed up within 24 months. Of 13 patients with a follow-up period less than 3 months, 12 patients had final VA better than 20/40. We found that children with better visual recovery seemed to be prone to loss of follow-up. Insufficient follow-up time could lead to under estimation of the development of MS. Second, the type of treatment administered and the duration of time given were different between ophthalmologists and neurologists. The ophthalmologist usually followed the recommendations from the ONTT study to treat children with optic neuritis; however, the pediatric neurologist might not manage children in ways consistent with the ophthalmologist in clinical practice, which was also reported in a previous study.34 The main reason might be because of no standard guidelines from evidence-based research like the ONTT study in treating pediatric patients with optic neuritis. Nevertheless, intravenous methylprednisolone (10–30 mg/kg/day × 3–5 days) then taper from oral prednisolone for at least 4 weeks is still recommended to hasten visual recovery in children with optic neuritis.20 Finally, MRI of the brain is the gold standard imaging procedure for optic neuritis because it is much more powerful in predicting the risk of progression to MS compared with the presence of HLA-DR2 or CSF oligoclonal IgG band.35 However, CT of the brain was still performed in three patients because of the limitation of the facility in our hospital.
In conclusion, visual recovery in Taiwanese children with optic neuritis is favorable; a poor visual outcome was associated with age older than 10 years and pale disc at presentation. In addition, relatively lower rate of developing MS and not uncommon association with ADEM were also noted in Taiwanese children with optic neuritis.

Change history
10 November 2011
This article has been corrected since Advance Online Publication and an erratum is also printed in this issue
References
Beck RW, Cleary PA, Anderson Jr MM, Keltner JL, Shults WT, Kaufman DI et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The optic neuritis study group. N Engl J Med 1992; 326: 581–588.
Beck RW, Cleary PA . Optic neuritis treatment trial. One-year follow-up results. Arch Ophthalmol 1993; 111: 773–775.
Visual function 15 years after optic neuritis: a final follow-up report from the optic neuritis treatment trial. Ophthalmology 2008; 115: 1079–1082.
Beck RW, Cleary PA, Trobe JD, Kaufman DI, Kupersmith MJ, Paty DW et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. The Optic Neuritis Study Group. N Engl J Med 1993; 329: 1764–1769.
Beck RW, Gal RL . Treatment of acute optic neuritis: a summary of findings from the optic neuritis treatment trial. Arch Ophthalmol 2008; 126: 994–995.
Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Arch Neurol 2008; 65: 727–732.
Trobe JD . High-dose corticosteroid regimen retards development of multiple sclerosis in optic neuritis treatment trial. Arch Ophthalmol 1994; 112: 35–36.
Brady KM, Brar AS, Lee AG, Coats DK, Paysse EA, Steinkuller PG . Optic neuritis in children: clinical features and visual outcome. J AAPOS 1999; 3: 98–103.
Morales DS, Siatkowski RM, Howard CW, Warman R . Optic neuritis in children. J Pediatr Ophthalmol Strabismus 2000; 37: 254–259.
Cassidy L, Taylor D . Pediatric optic neuritis. J AAPOS 1999; 3: 68–69.
Riikonen R, Donner M, Erkkila H . Optic neuritis in children and its relationship to multiple sclerosis: a clinical study of 21 children. Dev Med Child Neurol 1988; 30: 349–359.
Kriss A, Francis DA, Cuendet F, Halliday AM, Taylor DS, Wilson J et al. Recovery after optic neuritis in childhood. J Neurol Neurosurg Psychiatry 1988; 51: 1253–1258.
Kennedy C, Csarroll FD . Optic neuritis in children. Arch Ophthalmol 1960; 63: 747–755.
Visudhiphan P, Chiemchanya S, Santadusit S . Optic neuritis in children: recurrence and subsequent development of multiple sclerosis. Pediatr Neurol 1995; 13: 293–295.
Hwang JM, Lee YJ, Kim MK . Optic neuritis in Asian children. J Pediatr Ophthalmol Strabismus 2002; 39: 26–32.
Hwang JS, Kim SJ, Yu YS, Chung H . Clinical characteristics of multiple sclerosis and associated optic neuritis in Korean children. J AAPOS 2007; 11: 559–563.
Mizota A, Niimura M, Adachi-Usami E . Clinical characteristics of Japanese children with optic neuritis. Pediatr Neurol 2004; 31: 42–45.
Takihara Y, Inatani M, Fukushima M, Iwao K, Iwao M, Tanihara H . Trabeculectomy with mitomycin C for neovascular glaucoma: prognostic factors for surgical failure. Am J Ophthalmol 2009; 147: 912–918.
Jo DH, Kim SJ, Chae JH, Yu YS . The clinical characteristics of optic neuritis in Korean children. Korean J Ophthalmol 2011; 25: 116–120.
Boomer JA, Siatkowski RM . Optic neuritis in adults and children. Semin Ophthalmol 2003; 18: 174–180.
Murphy J, Austin J . Spontaneous infection or vaccination as cause of acute disseminated encephalomyelitis. Neuroepidemiology 1985; 4: 138–145.
Lee WT, Wang PJ, Liu HM, Young C, Tseng CL, Chang YC et al. Acute disseminated encephalomyelitis in children: clinical, neuroimaging and neurophysiologic studies. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 1996; 37: 197–203.
Schwarz S, Mohr A, Knauth M, Wildemann B, Storch-Hagenlocher B . Acute disseminated encephalomyelitis: a follow-up study of 40 adult patients. Neurology 2001; 56: 1313–1318.
Tenembaum S, Chamoles N, Fejerman N . Acute disseminated encephalomyelitis: a long-term follow-up study of 84 pediatric patients. Neurology 2002; 59: 1224–1231.
Hung KL, Liao HT, Tsai ML . Postinfectious encephalomyelitis: etiologic and diagnostic trends. J Child Neurol 2000; 15: 666–670.
Hynson JL, Kornberg AJ, Coleman LT, Shield L, Harvey AS, Kean MJ . Clinical and neuroradiologic features of acute disseminated encephalomyelitis in children. Neurology 2001; 56: 1308–1312.
Kotlus BS, Slavin ML, Guthrie DS, Kodsi SR . Ophthalmologic manifestations in pediatric patients with acute disseminated encephalomyelitis. J AAPOS 2005; 9: 179–183.
Toker E, Yenice O, Yilmaz Y . Isolated bilateral optic neuropathy in acute disseminated encephalomyelitis. J Pediatr Ophthalmol Strabismus 2003; 40: 232–235.
Straub J, Chofflon M, Delavelle J . Early high-dose intravenous methylprednisolone in acute disseminated encephalomyelitis: a successful recovery. Neurology 1997; 49: 1145–1147.
Farris BK, Pickard DJ . Bilateral postinfectious optic neuritis and intravenous steroid therapy in children. Ophthalmology 1990; 97: 339–345.
Lucchinetti CF, Kiers L, O′Duffy A, Gomez MR, Cross S, Leavitt JA et al. Risk factors for developing multiple sclerosis after childhood optic neuritis. Neurology 1997; 49: 1413–1418.
Dale RC, de SC, Chong WK, Cox TC, Harding B, Neville BG . Acute disseminated encephalomyelitis, multiphasic disseminated encephalomyelitis and multiple sclerosis in children. Brain 2000; 123 (Part 12): 2407–2422.
Kesselring J, Miller DH, Robb SA, Kendall BE, Moseley IF, Kingsley D et al. Acute disseminated encephalomyelitis. MRI findings and the distinction from multiple sclerosis. Brain 1990; 113 (Part 2): 291–302.
Biousse V, Calvetti O, Drews-Botsch CD, Atkins EJ, Sathornsumetee B, Newman NJ . Management of optic neuritis and impact of clinical trials: an international survey. J Neurol Sci 2009; 276: 69–74.
Morrissey SP, Miller DH, Kendall BE, Kingsley DP, Kelly MA, Francis DA et al. The significance of brain magnetic resonance imaging abnormalities at presentation with clinically isolated syndromes suggestive of multiple sclerosis. A 5-year follow-up study. Brain 1993; 116 (Part 1): 135–146.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sun, MH., Wang, HS., Chen, KJ. et al. Clinical characteristics of optic neuritis in Taiwanese children. Eye 25, 1457–1464 (2011). https://doi.org/10.1038/eye.2011.196
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.196
Keywords
This article is cited by
-
Intravenous immunoglobulin treatment for steroid-resistant optic neuritis: a multicenter, double-blind, randomized, controlled phase III study
Japanese Journal of Ophthalmology (2021)
-
Paediatric Multiple Sclerosis: Update on Diagnostic Criteria, Imaging, Histopathology and Treatment Choices
Current Neurology and Neuroscience Reports (2016)