Abstract
Both chronic heart failure (CHF) and cancer are among the most frequent causes of death in developed countries. Given that CHF activates neurohumoral factors, such as cytokines, the pathophysiology of CHF could prime the onset or progression of cancer. We consecutively enrolled 5238 patients with CHF who had been hospitalized in the Department of Cardiovascular Medicine in our institute between 2001 and 2013. We followed these patients until April 2015. We examined the cohort of patients from our hospital and compared it with a control cohort derived from the 2008 cancer database ‘Monitoring of Cancer Incidence in Japan’ from the National Cancer Center, Japan. The incidence of cancer in CHF patients (198 cases out of the 5238 patients) was approximately four times higher than that in control patients (2.27% vs 0.59%, P<0.0001; 95% confidence interval, 1.89–2.71). When we omitted the patients whose cancer diagnosis occurred prior to their diagnosis of CHF, we still observed a significantly higher incidence of cancer in patients with CHF than in controls. Based on our results, we suggest that there is a strong correlation between the pathophysiology of CHF and cancer. Given that CHF could prime the onset of cancers, we recommend that clinicians should be vigilant regarding cancer comorbidity in patients with CHF.
Similar content being viewed by others
Introduction
Chronic heart failure (CHF), one of the major causes of mortality and morbidity worldwide,1 is the end-stage outcome of many cardiovascular diseases.2, 3 The pathophysiology of CHF includes the upregulation of: (1) neurohumoral factors, such as sympathetic nerves, the renin–angiotensin–aldosterone system4 and the growth hormone and cytokine systems;5 (2) the Klotho/FGF23 system;6 and (3) signal transduction proteins, such as the mammalian target of rapamycin.7 These diverse axes can independently influence the proliferative functions of their target organs. The most common cause of death in Western countries8 as well as in Japan9 is cancer; however, there has been no clear evidence that CHF is related to this disease. Intriguingly, recent reports have suggested that the pathophysiology and treatment of heart failure (HF) cause cancer,10, 11, 12, 13, 14, 15 and a retrospective cohort study demonstrated that the risk of CHF increased in patients with breast cancer after anthracycline and trastuzumab treatment.16 Furthermore, the causes of CHF and cancer can overlap; for example, diabetes mellitus can cause both cardiovascular disease17 and cancer.18 This indicates that there might be a cause and effect relationship between CHF and cancer, although this association remains unclear; it is also unknown whether CHF induces cancer or whether cancer precedes CHF. Interestingly, a recent report showed that atrial natriuretic peptide, a potential biomarker of CHF,19 decreased both cancer metastasis and the incidence of cancer.20, 21 Therefore, there is a need to investigate whether the pathophysiology of CHF induces or reduces the incidence of cancer and what types of cancer might be involved.
To investigate these issues, we consecutively enrolled patients with CHF in a retrospective study and examined the clinical profiles of and prevalence of cancer in these patients. Furthermore, we investigated the time of onset of each cancer and CHF and examined the prevalence of CHF preceding cancer onset.
Methods
Study design
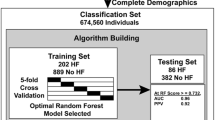
This study was a retrospective, single-center, cohort study. We consecutively enrolled 5238 CHF patients who were hospitalized in the Department of Cardiovascular Medicine in our institute between 2001 and 2013, and we followed these patients until April 2015. We also obtained data from the 2008 cancer database ‘Monitoring of Cancer Incidence in Japan’ from the National Cancer Center, Japan. The patients in this database comprised the control group (controls). This study was approved by the National Cerebral and Cardiovascular Center Research Ethics Committee (M27-077). The Committee decided that, according to the Japanese Clinical Research Guidelines, the acquisition of informed consent from the subjects was not required because it was a retrospective observational study. Instead, a public announcement was made in accordance with the Ethics Committee’s request and the Japanese Clinical Research Guidelines.
Study population
We verified the presence of CHF in the 5238 patients who were hospitalized in the Department of Cardiovascular Medicine in our institute from 2001 to 2013. The patient characteristics are shown in Table 1. The diagnosis of CHF was confirmed by an expert team of cardiologists using the Framingham Heart Failure Diagnostic Criteria.22 We also assessed the existence and severity of CHF using echocardiograms and plasma B-type natriuretic peptide (brain natriuretic peptide (BNP)) levels.23 In addition, careful medical histological analysis, physical examination, laboratory testing, chest X-rays, electrocardiography, complete Doppler echocardiography, coronary angiography, right heart catheterization, cardiac scintigraphy, cardiovascular magnetic resonance imaging, cardiopulmonary exercise testing and polysomnography were performed in all patients to diagnose the causes of CHF. By contrast, the cancers in the CHF patient cohort had been diagnosed by researchers who specialized in the diagnosis and treatment of cancers. We confirmed the evidence of cancer in the medical records of the relevant patients. We also examined the time of onset of CHF and cancer, defined as the time of the first diagnosis of CHF and cancer, respectively, at National Cerebral and Cardiovascular Center or at other specialized hospitals.
We also obtained data pertaining to the prevalence of cancer in Japan from the 2008 Cancer Registry and Statistics, collected and collated legally by the Cancer Information Service of the National Cancer Center, Japan. This registry is based on the results of a nationwide survey of cancer patients (Monitoring of Cancer Incidence in Japan) that aimed to ascertain the actual rate of cancer incidence and acquire data for cancer countermeasures in Japan. We used the data from 2008 as our control group because this was the median year of the 2001–2015 timeframe of our study.
Study protocol
We determined the prevalence of cancer in the CHF patient cohort and compared it with that in all Japanese cancer patients. We also determined the prevalence of individual cancers, such as lung cancer, in these two populations. Finally, we compared the prevalence of cancer in patients whose cancer originated after the onset of CHF with that in the cancer patient control group.
Primary outcome measure
The primary outcome measure was defined as the prevalence of all cancers and the comparison of cancer incidence in CHF patients and the cancer patient control group.
Secondary outcome measure
The secondary outcome measures were defined as the prevalence of each cancer, the comparison of the incidence of each cancer in CHF patients and in the cancer patient control group. We also investigated the characteristic of CHF such as causes of CHF, plasma BNP levels, left ventricular ejection fraction (LVEF) and LV dimensions in CHF patients.
Statistical analysis
Descriptive statistics of continuous variables are presented as the mean and s.d. or as medians with the 25th and 75th percentiles, depending on the distribution of the variables. Categorical variables are presented as frequencies and percentages. The overall prevalence of cancer in patients with CHF and the prevalence for each cancer type were calculated with the 95% confidence interval (CI). To compare the prevalence rates in the CHF and non-CHF populations, the prevalence rates were adjusted for age and sex, the most common variables used for standardization, using published data from the National Cancer Center database ‘Monitoring of Cancer Incidence in Japan’. All P-values were two-sided, and a P-value <0.05 was considered statistically significant. All statistical analyses were performed using the SAS Statistical Software version 9.3 for Windows (SAS Institute, Cary, NC, USA).
Results
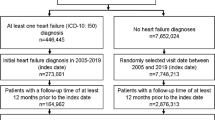
Table 1 shows the characteristics of the 5238 CHF patients. The severity of CHF was characterized by BNP levels, and LV systolic and diastolic diameters (LVDs and LVDd, respectively) and LVEF, which were determined by echocardiography at discharge. Table 2 shows that the incidence of cancer in CHF patients was higher than that in controls (overall: 2.27% vs 0.59%, P<0.0001; men: 2.12% vs 0.71%, P<0.0001; and women: 2.40% vs 0.47%, P<0.0001) after matching for sex and age. Furthermore, the incidences of stomach cancer, lung cancer, prostate cancer, breast cancer and colon cancer were higher in CHF patients than in controls. There was no correlation between the incidence of cancer and CHF etiology, although cancer incidence appeared to be higher in CHF patients with valvular heart diseases (Table 3). Table 4 shows the relationship between the incidence of cancer and CHF severity according to plasma BNP levels and LVEF; the results showed that the incidence of cancer increased as the BNP level increased but not as LVEF decreased. Intriguingly, the incidence of cancer increased as LVDd decreased. Progression of the severity of cardiovascular damage with smaller LV volume could be a clinical characteristic of CHF patients with cancer. We further examined the characteristics of CHF patients with and without cancer and found that those with cancer were older and that the prevalence of hemoglobin A1c >6.4% in CHF patients with and without cancer was 18.7% and 16.7%, respectively (P=0.464).
Table 5 shows the characteristics of CHF patients diagnosed with CHF before cancer and CHF patients diagnosed with cancer before CHF. After eliminating those cancer patients in whom cancer was diagnosed prior to CHF, we still found a higher incidence of cancer in CHF patients than in controls (0.99% vs 0.59%, P<0.001). We found that these cancers were diagnosed at a mean duration of 8.8 years after the diagnosis of CHF.
Discussion
In the present study, we demonstrated a higher prevalence of cancer in patients with CHF compared with an age- and sex-matched cancer patient control group, particularly for cancers of the stomach, lung, prostate, breast and colon; thus, we propose that there is a strong correlation between the pathophysiology of CHF and cancer. To our knowledge, this is the first report of such a correlation; however, we need to consider several issues and plausible mechanisms before reaching any firm conclusions.
Issues regarding the results and conclusions of the present study
The first issue that we need to consider is the diagnostic accuracy for CHF and cancer. If the diagnosis of either CHF or cancer were not accurate, the current results would be incorrect. For CHF, we used many modalities to reach the diagnosis, such as echocardiograms, imaging with radioisotope, computed tomography and magnetic resonance imaging tests, cardiac catheterization with myocardial biopsies, physical examinations and blood examinations, which strongly indicate the very high accuracy of the diagnoses and the efficacy of CHF treatments in Japan. The cancer diagnoses in patients with CHF were also made by professionals who specialized in both the diagnosis and treatment of cancers; we checked the medical records of all patients to verify their accuracy. In addition, the diagnosis of cancer in the general Japanese population is also very accurate. A database of registered patients with cancer was created under the Cancer Control Act (Act No. 98 2006), which came into force on 1 April 2007. As a result of this Act, all cancers are precisely diagnosed in Japan and registered into the National Cancer Center database. Therefore, both the cancer and CHF databases were reliable sources to use for the present study.
The second issue was that the Japanese cohort for the control group in the present study already included patients with CHF. As a control for the CHF cohort, it would have been preferable to investigate the incidence of cancer in non-CHF subjects. Unfortunately, that particular cohort has not yet been created for the investigation of cancer incidence. In Japan, the population of CHF patients is considered to be between 0.2 and 1 million people, which corresponds to approximately 0.2–1% of the general Japanese population. Given that the incidence of cancer was higher in CHF patients than in the general Japanese population, the incidence of cancer in the non-CHF subjects should be marginally lower than the value we obtained (0.59%); this further increases the difference in the prevalence of cancer between the CHF and non-CHF populations. Thus it would be appropriate to conclude that CHF increased the incidence of cancer >3.85 times in our study population (2.27/0.59).
The third issue pertains to other comorbidities that can cause cancer in patients with CHF. Given that diabetes mellitus can cause cardiovascular disease17 and cancer,18 we checked plasma hemoglobin A1c levels; however, we found no differences in plasma hemoglobin A1c levels between CHF patients with and without cancer. Several drugs for CHF have been reported to induce cancer13, 14, 15; however, all drugs used to treat our CHF patient cohort have been approved for safety. Additionally, the rate of carcinogenesis should be too low to account for the differences between CHF patients with and without cancer and to provoke cancer over an average of 4 years (Table 5).
Finally, we found that the incidence of cancer in the stomach, lung, prostate, breast and colon was increased in the CHF cohort; however, we were unable to confirm that CHF pathophysiology was the reason why these organs were more likely to develop cancer. CHF causes low perfusion and edema in all organs, which can cause carcinogenesis. In this study, because: (1) the number of cancer patients was small; (2) the species of cancer were heterogeneous; and (3) we did not check the blood levels of neurohumoral factors, such as cytokines, that can facilitate the development and progression of each individual cancer, we hypothesize that the neurohumoral factors elevated during HF generally increase carcinogenesis. Furthermore, we only examined the cancer groups that contained more than five patients; thus, we cannot exclude the possibility that low-frequency cancers, such as ovarian cancer, are influenced by CHF.
Several possibilities that the onset of CHF may be followed by the onset of cancer
There are various mechanisms by which CHF pathophysiology could affect the onset or progression of cancer. The first is that the activation of neurohumoral factors, such as cytokines and endothelin, could affect oncogenesis. Endothelin has been reported to activate the transcription factor nuclear factor-κB,24 and the GATA-4 transcription factor25 can affect oncogenesis in remote organs via mitogen-activated protein kinase-mediated phosphorylation. Second, cancer drugs can cause HF. Indeed, trastuzumab, a drug for breast cancer, has been found to be toxic to the heart and can cause CHF.26 It has been reported that survivors of young adult cancer were at increased risk of developing cardiovascular disease.27 However, we observed an increased incidence of cancer in patients with CHF, even after excluding those patients in whom the onset of cancer preceded the onset of CHF; this suggested that the pathophysiology of CHF primed oncogenesis. This was in agreement with the results of Hasin et al.,10 who prospectively observed the onset of cancer in 961 CHF and non-CHF subjects and found a 68% increase in cancer in the CHF patients. We also observed a 68% increase in the onset of cancer in patients with CHF ((0.99–0.59)/0.59=0.68). The third possibility is the existence of common risk factors between CHF and cancer. Indeed, smoking and diabetes mellitus have been reported to be risk factors for both CHF and cancer.28 However, the percentages for comorbidity with diabetes mellitus were similar between patients with and without CHF. Conversely, there might be unknown common risk factors for both CHF and cancer. The fourth possibility is that there might be genes or foods that are related to both cancer and CHF. The fifth possibility is that, because hospitalized CHF patients undergo examinations for both cardiac function and general physical condition, cancers are diagnosed incidentally, which could contribute to the increased incidence of cancer diagnosis in CHF patients. However, even in the general population, the Japanese Government has budgeted money to examine cancer onset, suggesting that we may also accidently find cancer in non-CHF subjects as well as in CHF patients. Taken together, because we could not identify the specific mechanisms through which cancer might be primed by the pathophysiology of CHF, there is a need for further investigation.
Clinical importance
First, when we examine patients with CHF, we usually focus not only on cardiac function but also on the general condition of the patients. However, we typically only assess general conditions associated with CHF, such as renal dysfunction, pulmonary dysfunction or hepatic dysfunction. The current observation strongly supports the idea that these examinations are not sufficient and that we need to be vigilant regarding possible cancer onset in patients with CHF. Second, we hypothesize that CHF patients with cancer are likely to have more severe cardiovascular damage and a small LV. Interestingly, LVEF did not affect the incidence of cancer, suggesting that cancers could be observed in patients with HF with preserved EF. Third, we observed that the incidence of cancer in CHF patients increased as LVDd decreased, although LVEF was not significantly different between CHF patients with and without cancer. These results suggest that HF with preserved EF is associated with cancer. Although the reasons for this coincidence are not clear, one possible explanation is that modifiers of HF with preserved EF and cancers, such as aging, are similar. Finally, when we investigate CHF pathophysiology, we may also be taking a step forward in the identification of unknown oncogenesis mechanisms.
Social impacts
Although we have noted that cancer is related to the pathophysiology of CHF and that we need to be vigilant about concurrent cancer when examining CHF patients, we need to consider the present results in terms of their social impact. First, the present study could be interpreted as suggesting that cancer screening in CHF patients would be useful. However, the present retrospective study does not provide such evidence, and a prospective study is warranted because cancer screening in CHF patients might not find early-stage cancers. Second, we note that cancer screening in CHF patients might not improve the prognosis for all-cause mortality. Third, the improved prognosis that might be attributable to cancer screening in patients with CHF would not help in reducing the social burden, because such cancer screenings are not generally recommended at present. Instead, we emphasize that clinicians should always consider the possibility of cancer when examining CHF patients. Finally, before the prospective investigation of the cost-effectiveness of cancer screening in CHF patients, the conclusion of this study should not be extrapolated as a recommendation for the general practice of cancer screening in CHF patients under the present Japanese medical insurance system.
Study limitations
The present study has some limitations. First, because this study was a single-center study, the number of patients was limited, particularly, in the CHF cohort. Our hospital is a leading hospital with a high volume of CHF patients, and we have a database of >8000 CHF patients with precise information on the etiology and severity of their CHF. Nevertheless, we cannot analyze the incidence of rare cancers in our database of CHF patients. To resolve this, we suggest testing the present hypothesis using larger multicenter trials. Second, although most of our patients came from the area near Osaka, where our hospital is located, we also enrolled patients from all over Japan because our hospital is the only institution that specializes in cardiovascular diseases and HF. By contrast, the cancer database comprised subjects from all over the country. These differences in residency could also affect the quantitative results of the present study. However, we Japanese are relatively homogenous in terms of our living style and genetics. In addition, we were not able to exclude the data of CHF patients who were also diagnosed with cancer from the 2008 Japanese cancer database, which might have underestimated but not overestimated the number of patients in our cohort who had cancer with concurrent CHF. Finally, based on the data in this study, we were unable to determine the cause and effect relationship between CHF and cancer; thus further research is required to this end.
Clinical perspectives
We observed increased cancer onset in patients with CHF, which suggests that the pathophysiology of CHF primes the oncogenesis process.
Given that CHF might prime the onset of cancers, we should be vigilant regarding cancer comorbidity in patients with CHF.
Translational perspectives
Both CHF and cancer are among the most frequent causes of death in developed countries. Given that CHF modulates the activation of neurohumoral factors, such as cytokines, the pathophysiology of CHF could prime the onset or progression of cancer. We found that the incidence of cancer in CHF patients was approximately four times higher than that in control patients after adjustments for age and sex. The most frequent cancers in CHF patients were stomach, lung, prostate, breast and colon cancers. Thus we propose that there is a strong correlation between the pathophysiology of CHF and cancer.
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Giliespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Maqid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Tumer MB, American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014; 129: e28–e292.
Braunwald E, Bristow MR . Congestive heart failure: fifty years of progress. Circulation 2000; 102: Iv14–Iv23.
Jessup M, Brozena S . Heart failure. N Engl J Med 2003; 348: 2007–2018.
Dzau V . The cardiovascular continuum and renin-angiotensin-aldosterone system blockade. J Hypertens Suppl 2005; 23: S9–S17.
Torre-Amione G . Immune activation in chronic heart failure. Am J Cardiol 2005; 95: 3C–8C discussion 38C–40C.
Hu MC, Shi M, Cho HJ, Adams-Huet B, Peak J, Hill K, Shelton J, Amaral AP, Faul C, Taniguchi M, Wolf M, Brand M, Takahashi M, Kuro-O M, Hill JA, Moe OW . Klotho and phosphate are modulators of pathologic uremic cardiac remodeling. J Am Soc Nephrol 2015; 26: 1290–1302.
Sciarretta S, Volpe M, Sadoshima J . Mammalian target of rapamycin signaling in cardiac physiology and disease. Circ Res 2014; 114: 549–564.
Siegel R, Ma J, Zou Z, Jemal A . Cancer statistics, 2014. CA Cancer J Clin 2014; 64: 9–29.
Matsuda A, Matsuda T, Shibata A, Katanoda K, Sobue T, Nishimoto H . Cancer incidence and incidence rates in Japan in 2008: a study of 25 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clim Oncol 2014; 44: 388–396.
Hasin T, Gerber Y, McNallan SM, Weston SA, Kushwaha SS, Nelson TJ, Cerhan JR, Roger VL . Patients with heart failure have an increased risk of incident cancer. J Am Coll Cardiol 2013; 62: 881–886.
Deswal A, Basra SS . Incident cancer in patients with heart failure: causation or mere association? J Am Coll Cardiol 2013; 62: 887–888.
Ather S, Chan W, Bozkurt B, Aquilar D, Ramasubbu K, Zachariah AA, Wehrens XH, Deswal A . Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol 2012; 59: 998–1005.
Wright JL, Hansten PD, Stanford JL . Is digoxin use for cardiovascular disease associated with risk of prostate cancer? Prostate 2014; 74: 97–102.
Singh A, Bangalore S . Which, if any, antihypertensive agents cause cancer? Curr Opin Cardiol 2012; 27: 374–380.
Mackenzie IS, Macdonald TM, Thompson A, Morant S, Wei L . Spironolactone and risk of incident breast cancer in women older than 55 years: retrospective, matched cohort study. BMJ (Clin Res Ed.) 2012; 345: e4447.
Bowles EJ, Wellman R, Feigelson HS, Onitilo AA, Freedman AN, Delate T, Allen LA, Nekhlyudov L, Goddard KA, Davis RL, Habel LA, Yood MU, McCarty C, Magid DJ, Wagner EH, Pharmacovigilance Study Team. Risk of heart failure in breast cancer patients after anthracycline and trastuzumab treatment: a retrospective cohort study. J Natl Cancer Inst 2012; 104: 1293–1305.
Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, Deanfield J, Smeeth L, Timmis A, Hemingway H . Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinology 2015; 3: 105–113.
Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL, Wolff AC, Brancari FL . Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis. JAMA 2008; 300: 2754–2764.
Yoshimura M, Yasue H, Okumura K, Ogawa H, Jougasaki M, Mukoyama M, Nakao K, Imura H . Different secretion patterns of atrial natriuretic peptide and brain natriuretic peptide in patients with congestive heart failure. Circulation 1993; 87: 464–469.
Nojiri T, Hosoda H, Tokudome T, Miura K, Ishikane S, Otani K, Kishimoto I, Shintani Y, Inoue M, Kimura T, Sawabata N, Minami M, Nakahiri T, Funaki S, Takeuchi Y, Maeda H, Kidoya H, Kiyonari H, Shioi G, Arai Y, Hasegawa T, Takakura N, Hori M, Ohno Y, Miyazato M, Mochizuki N, Okumura M, Kangawa K . Atrial natriuretic peptide prevents cancer metastasis through vascular endothelial cells. Proc Natl Acad Sci USA 2015; 112: 4086–4091.
Serafino A, Pierimarchi P . Atrial natriuretic peptide: a magic bullet for cancer therapy targeting Wnt signaling and cellular pH regulators. Curr Med Chem 2014; 21: 2401–2409.
McKee PA, Castelli WP, McNamara PM, Kannel WB . The natural history of congestive heart failure: the Framingham Study. N Engl J Med 1971; 285: 1441–1446.
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecher S, McDonagh T, Sechtem U, Bonet LA, Avraamides P, Ben Lamin HA, Brignole M, Coca A, Cowburm P, Dargie H, Elliott P, Flachskampg FA, Guida GF, Hardman S, Iung B, Merkely B, Mueller C, Nanas JN, Nielsen OW, Orn S, Parissis JT, Ponikowski P, ESC Committee for Practive Guidelines. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2012; 14: 803–869.
Pikkarainen S, Tokola H, Kerkela R, Majalahti-Palviainen T, Vuolteenaho O, Ruskoaho H . Endothelin-1-specific activation of B-type natriuretic peptide gene via p38 mitogen-activated protein kinase and nuclear ETS factors. J Biol Chem 2003; 278: 3969–3975.
Kerkela R, Pikkarainen S, Majalahti-Palviainen T, Tokola H, Ruskoaho H . Distinct roles of mitogen-activated protein kinase pathways in GATA-4 transcription factor-mediated regulation of B-type natriuretic peptide gene. J Biol Chem 2002; 277: 13752–13760.
Wu YY, Huang TC, Tsai TN, Chen JH, Dai MS, Chang PY, Ho CL, Ye RH, Chung TR, Chen YC, Chao TY . The clinical efficacy and cardiotoxicity of fixed-dose monthly trastuzumab in HER2-positive breast cancer: a single institutional analysis. PLoS ONE 2016; 11: e0151112.
Chao C, Xu L, Bhatia S, Cooper R, Brar S, Wong FL, Armenian SH . Cardiovascular disease risk profiles in survivors of adolescent and Young Adult (AYA) cancer: The Kaiser Permanente AYA Cancer Survivors Study. J Clin Oncol 2016; 34: 1626–1633.
Ayanian JZ, Cleary PD . Perceived risks of heart disease and cancer among cigarette smokers. JAMA 1999; 281: 1019–1021.
Acknowledgements
This study was supported by Grants-in-aid for Human Genome, Tissue Engineering and Food Biotechnology (H13-Genome-011), Health and Labour Sciences Research Grants, Comprehensive Research on Aging and Health (H13-21seiki(seikatsu)-23), Health and Labour Sciences Research Grants from the Ministry of Health, Labour and Welfare in Japan and a Grant from the Japanese Cardiovascular Research Foundation. The sponsors of the present study had no role in the study design, data collection, data analysis, data interpretation or writing of the report. There are no additional disclosures of contributions, names, degrees, affiliations and indications (all persons who have made substantial contributions to the work but who are not authors have been compensated).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
TH reports personal fees from Takeda Pharmaceutical Company, Daiichi Sankyo Company, Otsuka Pharmaceutical, Bayer Yakuhin, Mitsubishi Tanabe Pharma Corporation, Abbott Vascular Japan and Shionogi & Co. during the conduct of the study; MA reports having received grants from the Japanese Government during the conduct of the study as well as personal fees and non-financial support from Pfizer, personal fees from Boehringer-Ingelheim, personal fees from Tanabe-Mitsubishi, personal fees from Kowa and personal fees from Takeda, which were unrelated to the submitted work; HT reports having received grants from The Bayer Scholarship for Cardiovascular Research and from the Japanese Ministry of Education, Culture, Sports, Science and Technology, which were unrelated to the submitted work; MA reports having received grants from the Japan Heart Foundation/Bayer Yakuhin Research Grant Abroad, grants from the Suzuken Memorial Foundation, non-financial support from Abbott Vascular Japan and non-financial support from the Takeda Pharmaceutical Company, which were unrelated to the submitted work; MK reports having received grants and personal fees from Takeda during the conduct of the study as well as grants from the Japanese Government, the Japan Heart Foundation and the Japanese Cardiovascular Research Foundation, grants and personal fees from Asteras, grants and personal fees from Sanofi, personal fees from Daiichi-Sankyo, grants and personal fees from Pfizer, grants and personal fees from Ono, personal fees from Bayer, grants and personal fees from Novartis, personal fees from Boehringer, grants and personal fees from Tanabe-Mitubishi, personal fees from Kowa, grants and personal fees from Kyowa-Hakko-Kirin, personal fees from Dainihon-Sumitomo, personal fees from Sawai, personal fees from MSD, grants and personal fees from Abbott, grants and personal fees from Otsuka, grants from Calpis, grants from Nihon Kohden, personal fees from Shionogi, personal fees from AstraZeneca, personal fees from Asahikasei Med., personal fees from Novo Nordisk, personal fees from Fuji-film RI and personal fees from Japan Medical Data, which were unrelated to the submitted work. The other authors declare no conflict of interest.
Additional information
Author contributions
All co-authors of this manuscript have read and approved the submission of the manuscript. All the authors made an important contribution to the study and are thoroughly familiar with the original data.
Rights and permissions
About this article
Cite this article
Sakamoto, M., Hasegawa, T., Asakura, M. et al. Does the pathophysiology of heart failure prime the incidence of cancer?. Hypertens Res 40, 831–836 (2017). https://doi.org/10.1038/hr.2017.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.45
Keywords
This article is cited by
-
KRAS, MYC, and ARF6: inseparable relationships cooperatively promote cancer malignancy and immune evasion
Cell Communication and Signaling (2023)
-
New-Onset Cancer in the HF Population: Epidemiology, Pathophysiology, and Clinical Management
Current Heart Failure Reports (2021)
-
Cancer Risk in the Heart Failure Population: Epidemiology, Mechanisms, and Clinical Implications
Current Oncology Reports (2021)
-
Elevated plasma endocan and BOC in heart failure patients decrease after heart transplantation in association with improved hemodynamics
Heart and Vessels (2020)
-
Prevalence of extracardiac findings in patients undergoing coronary computed tomography and additional low-dose whole-body computed tomography
Japanese Journal of Radiology (2020)