Abstract
Thromboxane A2 (TXA2) is an important lipid mediator whose function in apoptosis is the subject of conflicting reports. Here, a yeast two-hybrid screen for proteins that interact with the C-terminus of the TXA2 receptor (TP) identified Siva1 as a new TP-interacting protein. Contradictory evidence suggests pro- and anti-apoptotic roles for Siva1. We show that a cisplatin treatment induces TXA2 synthesis in HeLa cells. We demonstrate that endogenous TP stimulation promotes cisplatin-induced apoptosis of HeLa cells and that such modulation requires the expression of Siva1, as evidenced by inhibiting its endogenous expression using siRNAs. We reveal that, upon stimulation of TP, degradation of Siva1 is impeded, resulting in an accumulation of the protein, which translocates from the nucleus to the cytosol. Translocation of Siva1 correlates with its reduced interaction with Mdm2 (an inhibitor of p53 signalling), as well as with its increased interaction with TRAF2 and XIAP (known to enhance pro-apoptotic signalling). Our data provide a model that reconciles the pro- and anti-apoptotic roles that were reported for Siva1 and identify a new mechanism for promoting apoptosis by G protein-coupled receptors. Our findings may have implications in the use of cyclo-oxygenase inhibitors during cisplatin chemotherapy and might provide a target to reduce cisplatin toxicity on non-cancerous tissues.
Similar content being viewed by others
Main
Thromboxane A2 (TXA2) is a potent lipid mediator best known for its central role in platelet activation, although other functions are emerging as well.1 It is synthesized from arachidonic acid through sequential processing by the cyclo-oxygenase (COX) 1 or 2 and the thromboxane synthase – a cascade inhibited by non-steroidal anti-inflammatory drugs. TXA2 has been shown to function through its TXA2 receptor (TP), a G protein-coupled receptor that mainly signals through Gαq and Gα13.1 TP comes in two isoforms, TPα and TPβ, differing in their C-terminal cytoplasmic tails. We previously reported that TPβ, but not TPα, undergoes significant constitutive and agonist-induced endocytosis.2 We performed a yeast two-hybrid screen looking for proteins interacting with the C-terminal tail of TPβ.3 We report here that the Siva1 protein directly interacts with the C-tail of TPβ.
Siva1 is a 175 amino-acids protein known to induce apoptosis through multiple pathways.4, 5 Various studies demonstrated that Siva1 expression is upregulated in contexts where apoptosis is induced, such as ischemic insults6 and treatments with chemotherapeutic agents like cisplatin.7 Siva1 was shown to be a direct transcriptional target of p53 and E2F18 and suggested mechanisms of apoptosis induction include Siva1 interaction with and inhibition of Bcl-xL9 and binding to TRAF2 (Nakahata1) or XIAP10 to inhibit NFκB activity and promote sustained JNK activation. On the other hand, a recent study highlighted a powerful anti-apoptotic role for Siva1 where, by simultaneously binding to both p53 and Mdm2, Siva1 suppressed p53 signalling.11 To this day, this functional dichotomy remains unresolved. Interestingly, Siva1 interacts with five cell-surface receptors – three members of the TNF receptors family (CD27, GITR and OX-40,12 as well as the LPA2 and S1P4 receptors.13 Although Siva1 seemed instrumental in inducing pro-apoptotic signalling in the case of the TNF receptors, agonist stimulation of the LPA2 receptor, in contrast, appeared to enhance Siva1 degradation and protect from apoptosis.13, 14
Apoptosis modulation by TXA2 is a controversial subject and depending on the studied cell type, both apoptosis protection and promotion have been observed as an outcome of TP stimulation.15, 16, 17, 18 The aim of the present study was to assess the involvement of Siva1 in the modulation of apoptosis by TXA2. Our data reconcile, for the first time, the conflicting reports on Siva1 as a pro- or anti-apoptotic protein and provide insights as to how the outcome of TP signalling might be shifted as a result of changing Siva1 expression and localization.
Results
TP directly interacts with Siva1
We have previously shown that the C-terminus of TPβ (C-tail) contains regulatory domains responsible for the trafficking properties of the receptor.3 To identify putative proteins that interact with the receptor, we performed a yeast two-hybrid screen using the TPβ C-tail as bait. A total of 1.5 × 106 independent clones were screened, yielding over 300 positives, seven of which contained the full-length Siva1 coding sequence (data not shown). To confirm the interaction and map the domains involved on both proteins, constructs of the whole coding sequence and deletion mutants of Siva1 fused to a histidine repeat sequence were generated along with fragments of the C-tail and intra-cellular loops (ICL) of TPβ fused to the gluthatione-S transferase (Figures 1a and b). The constructs were expressed and purified from bacteria and in vitro pulldowns were performed. As shown in Figure 1c, full-length Siva1 directly interacted with the C-tail and ICLs of the receptor. The complete TPβ C-tail (C-tail A) was the most effective in pulling down Siva1. Pulldown of Siva1 was markedly decreased for the C-tail B and E constructs, suggesting the presence of an important interaction determinant between amino acids 334 and 345. Both ICL1 and ICL2 also showed significant interaction with full-length Siva1, indicating that TPβ-Siva1 binding is likely dependent upon multiple sites on the receptor. The binding site on Siva1, on the other hand, appeared to be dependent on the very C-terminal end of the protein (Figure 1d) with substantial loss of interaction seen when removing amino acids 138–175 and further loss of the residual interaction when removing amino acids 114–175, suggesting that this region of Siva1 is required for the binding of the multiple receptor domains. The interaction was further confirmed in HEK293 cells. As shown in Figure 1e, Siva1-HA co-immunoprecipitated with Flag-TPβ while the interaction between the receptor and Siva1ΔC-HA was greatly reduced, corroborating our in vitro interaction mapping on Siva1. The TP-Siva1 interaction was detected between the endogenous proteins in HeLa cervical cancer cells that endogenously express both TP1 and Siva114 (Supplementary Material 1). A 5-h stimulation of TP reduced the TP-Siva1 co-immunoprecipitation.
Siva1 interacts with the C-tail and intra-cellular loops (ICL) of TPβ through its domain spanning amino acids 138 through 175. (a) Various fragments of the TPβ C-tail were cloned into the pGEX-4T-1 vector to generate GST fusion proteins. (b) Full length and two deletion mutants of Siva1 with a C-terminal HA epitope were also cloned into the pRSETa vector, adding six in-frame histidines at the N-terminal end of the Siva1 insert. (c) Siva1 pulldowns. Purified full-length His-Siva1-HA was incubated with various GST-tagged TP ICLs and C-tail fragments. Siva1 was pulled-down by all TPβ constructs, but ICL1, ICL2 and the C-tail constructs containing amino-acids 334–345 were the most effective. (d) Truncation of the Siva1 C-terminal end prevented Siva1 pulldown by both the complete TPβ C-tail (Ctail A) and ICL1. (e) Formation of a TP/Siva1 complex in cellulo. Siva1-HA and FLAG-TPβ were co-expressed in HEK293 cells and immunoprecipitations were performed on the lysate using an anti-FLAG monoclonal antibody and protein G-coated agarose beads. Siva1-HA co-immunoprecipitated with FLAG-TPβ (lane 2), whereas truncation of the Siva1 C-terminal end severely diminished the interaction (lane 4). IB, immunoblotting; IP, immunoprecipitation
Endogenous TP stimulation promotes cisplatin-induced apoptosis in HeLa cells
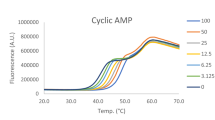
Because both pro- and anti-apoptotic roles for Siva1 had been reported,4, 11 we wondered if and how Siva1 could be involved in the modulation of apoptosis by TXA2. HeLa cells were treated overnight with the DNA-damaging agent cisplatin in order to induce a basal level of apoptosis. Concomitantly, the cells were stimulated with increasing concentrations of U46619 and apoptosis was assessed using two independent techniques, annexin V staining of externalized phosphatidylserines and western blotting of poly (ADP-ribose) polymerase (PARP), a caspase substrate cleaved during apoptosis. As shown in Figures 2a and b, U46619 dose-dependently promoted HeLa cells cisplatin-induced apoptosis with an EC50 of about 87 nM, similar to the 82 nM EC50 reported for human platelet aggregation.19 Promotion of apoptosis by U46619 was abolished by treatment with the TP antagonist SQ29548 (Figures 2c and d), further supporting that U46619 functions through TP to enhance cisplatin-induced apoptosis. Interestingly, U46619 could not induce apoptosis in the absence of cisplatin treatment (Figure 2a), indicating that co-stimulatory signals triggered by cisplatin are required for this TP phenotype.
Endogenous TP stimulation promotes cisplatin-induced apoptosis in HeLa cells as assessed by phosphatidylserine exposure and PARP cleavage. (a) HeLa cells were incubated for 5 h with various concentrations of U46619 and concomitantly treated with 50 or 100 μM cisplatin or vehicle for 5 h or overnight (O/N). Phosphatidylserine exposure was assessed by flow-cytometry analysis of a fluorescent annexin V staining 24 h following the start of the cisplatin treatment. U46619 dose-dependently induced phosphatidylserine exposure in cisplatin-treated HeLa cells (see three top curves), but not in untreated cells (lower curve). Mean calculated EC50 for U46619 was of 87 nM. Drawn in grey is the standard deviation from the mean, which spans from 34 nM to 224 nM. Each point in the scatter plot is the mean and S.E.M. of three identical conditions in a single experiment. The four independent experiments using various cisplatin treatments shown are representative of multiple experiments using each individual treatment. (b) Following flow-cytometry analysis, samples were lysed and SDS-PAGE and immunobloting using a monoclonal anti-PARP antibody were performed. U46619 dose-dependently induced PARP cleavage following cisplatin treatment. The blot shown here is that of a 50 μM overnight treatment, but is representative of the other 100 μM O/N and 50 μM 5 h treatments as well. (c and d) The effect of U46619 on phosphatidylserine exposure and PARP cleavage can be inhibited by a concomitant 10 μM treatment with the TP antagonist SQ29548
Cisplatin induces TXA2 production
While performing the EC50 calculations for the previous experiments, we noticed that, although U46619 consistently promoted cisplatin-induced apoptosis in HeLa cells, the EC50 of this effect appeared inversely correlated with the harshness of the cisplatin treatment. Indeed, in Figure 2a, the EC50 are ∼36 nM, ∼77 nM and ∼236 nM for the experiments where the cells were treated with 100 μM cisplatin overnight, 50 μM cisplatin overnight, or 50 μM for 5 h, respectively. This observation led us to believe that cisplatin might induce endogenous production of TXA2 by HeLa cells, which could change the actual agonist concentration in our culture medium, consequently shifting our apparent dose–response curve to the left. We thus measured the concentration of TXB2 – a stable TXA2 metabolite – as a proxy for TXA2 synthesis. As shown in Figure 3, cisplatin treatment increased TXB2 concentration in the culture medium by 5–10 folds to about 2.25 nM, up from 0.22 nM in untreated conditions, indicating that HeLa cells can synthetize TXA2 and secrete it in the culture medium during the DNA-damage response. This increased synthesis correlates with, and qualitatively explains, the apparent apoptosis EC50 reduction upon cisplatin treatment. However, since TXA2 production is likely to be underestimated due to detection limitations, it cannot quantitatively be linked to the shift in EC50 of cisplatin-induced apoptosis in Figure 2.
Cisplatin induces thromboxane production. HeLa cells were treated for 48 h with various concentrations of cisplatin. The culture medium was then collected and thromboxane B2 levels were assessed using a commercially available ELISA-based kit. Shown here is a representative result of five independent experiments
TP stimulation prevents Siva1 degradation
With the clear pro-apoptotic outcome of TP stimulation observed in our model, we next investigated how Siva1 function might be controlled by TXA2. To assess whether TPβ or its stimulation had any control over Siva1 expression, Siva1-HA and Flag-TPβ were expressed in HEK293 cells together or separately and treated with U46619 for up to 5 h. As shown in Figure 4a, agonist stimulation of TPβ for 2 and 5 h increased the amount of Siva1 protein that was detected. This effect was also observed with Siva1ΔC (data not shown). An increase in total expression can be the result of either enhanced synthesis or decreased degradation. Because the previous experiments were performed using expression constructs under the control of the constitutive CMV promoter, we conjectured that an augmentation in total Siva1 expression was most likely the result of a reduction in the degradation of the protein. A cycloheximide chase was performed in order to calculate the half-life of Siva1 in cellulo. Cells expressing TPβ and Siva1 were incubated with vehicle or U46619 for 3 h and then treated with the protein synthesis inhibitor cycloheximide for the indicated times (Figure 4b). In the most conservative experiment, Siva1 half-life was ∼18 min in cells treated with vehicle and increased to ∼29 min in cells stimulated with U46619 (Figures 4b and c), indicating that TP stimulation slowed Siva1 turnover by about 60%. Other experiments showed Siva1 half-life to be of 19, 26 or 31 min in basal condition, which increased to, respectively, 74, 65 or 106 min upon stimulation. We postulate that the high variability of the absolute half-life between each experiment might result from variations in passage number and/or cell confluence, as Siva1 expression is notoriously affected by these factors.20 In any case, statistical analysis of all four experiments using a two-way repeated measures ANOVA found the interaction between the two variables (TP stimulation and total Siva1 expression with time) to be extremely significant at P=0.0060, indicating that regardless of the initial absolute half-life, TP stimulation increased Siva1 stability. TP-induced increase in Siva1 expression was also confirmed in HeLa cells using endogenous proteins and found to be of similar magnitude to that induced by cisplatin treatment (Figure 4d). Concomitant treatment with both U46619 and cisplatin resulted in a further increase in Siva1 expression relative to either treatment alone. Together, these results indicate that TP stimulation increases total Siva1 expression by impeding its degradation and that the presence of cisplatin further elevates Siva1 levels, possibly through enhanced transcription, as described by others.7
TP increases total Siva1 expression by decreasing its degradation. (a) HEK293 cells were transfected with FLAG-TPβ and/or Siva1-HA. Two days later, cells were treated with 100 nM U46619 for 0.5, 2 or 5 h and then lysed. Western blot analysis demonstrates that U46619 treatment time-dependently induced an increase in Siva1-HA expression when Siva1 and TP were co-transfected (lanes 5–8), but not when Siva1 was transfected alone (lanes 9–12). (b and c) A time course of cycloheximide treatment was performed to evaluate Siva1 degradation kinetics. HEK293 cells were transfected with FLAG-TPβ and Siva1-HA. After 48 h, cells were treated for 3 h with 100 nM U46619. Cycloheximide was then added to the culture medium to reach a final concentration of 100 μg/ml and cells were harvested after the indicated times. Cells were then lysed and analysed by SDS-PAGE, western blotting and immunoblotting of transfected Siva1-HA using an HRP-coupled anti-HA antibody. Band intensity in (b) was quantified and plotted in (c) to calculate the in cellulo half-life of Siva1 in the presence or absence of TPβ stimulation. In the most conservative experiment (shown here), Siva1 was found to have an 18 min half-life in untreated cells, which increased by 60% to 29 min upon U46619 stimulation. A two-way repeated measures ANOVA performed using the results from all experiments found the half-lives increased seen upon stimulation to be extremely significant at P=0.0060. (d) Endogenous Siva1 expression also increased following U46619 stimulation of endogenous TP in HeLa cells. The increase was comparable to that induced by an overnight 50 μM cisplatin treatment and the combination of TP stimulation and cisplatin treatment had additive effect on Siva1 expression (lane 4). All blots shown are representative of at least three independent experiments
TP stimulation modulates the interaction of Siva1 with its known partners
Siva1 promotes apoptosis through various mechanisms, including the direct binding of XIAP10 and TRAF2.21 A recent report, however, highlighted that Siva1 could directly bind to both Mdm2 and p53 simultaneously and enhance p53 ubiquitination and degradation, thereby protecting against apoptosis.11 We thus wondered whether TP might be able to regulate those interactions, two of which are pro-apoptotic and one of which is anti-apoptotic. Co-immunoprecipitations of Siva1-HA with Myc-tagged Mdm2, XIAP or TRAF2 were performed following a 5-h FLAG-TP stimulation by U46619 or vehicle. As shown in Figure 5, TPβ stimulation enhanced the pro-apoptotic Siva1 interactions with XIAP and TRAF2 while decreasing the anti-apoptotic interaction between Siva1 and Mdm2 (see Supplementary Material 2 for detailed results analysis).
TP stimulation enhances the Siva1 interaction with XIAP and TRAF2 while diminishing the interaction between Siva1 and Mdm2. (a) HEK293 cells were co-transfected with Siva1-HA, FLAG-TPβ and Myc-Mdm2, Myc-XIAP or Myc-TRAF2. After 48 h, cells were treated or not with U46619 for 5 h before performing the co-immunoprecipitations. (b) The Siva1 increase upon U46619 stimulation shown in (a) was quantified in the lysate panels (white series) and in the co-immunoprecipitation panels (grey series) of three independent experiments. (c and d) Co-immunoprecipitation of endogenous XIAP or TRAF2 by goat anti-Siva antibodies was performed in HeLa cells and confirmed the results obtained in (a) and (b). Results shown in both histograms are the mean±S.D. of three independent experiments
TP stimulation induces translocation of Siva1 to the cytoplasm
Siva1 was reported to be predominantly located in the nucleus,4 although subpopulations have been described in the cytosol, plasma membrane and mitochondria.5, 7 Because Mdm2 is mostly nuclear22 while XIAP and TRAF2 are both cytosolic proteins,23, 24 we hypothesized that TP stimulation might induce a translocation of Siva1 from its nuclear location to the cytoplasm, thereby decreasing its interaction with Mdm2 and enhancing its association with XIAP and TRAF2. We thus performed live confocal microscopy imaging of HeLa cells expressing low levels of a Cherry-HA-Siva1 construct (Figure 6 and Supplementary Material 3). In accordance with our earlier demonstration of increased Siva1 expression following TP simulation, the Cherry-HA-Siva1 fluorescence markedly increased after 3 to 6 h of U46619 treatment. Progressive Siva1 translocation to the cytoplasm could be observed until about 12 h after receptor stimulation, where Siva1 appeared in equivalent proportions at the nucleus and the cytoplasm. Cytosolic staining was usually diffuse, but punctate accumulations could often be seen (Figure 6b), as reported by others.5 In some cells, apoptosis – as evidenced by blebbing seen in the differential interference contrast channel and Hoechst condensation – followed Siva1 translocation by 2 to 12 h (Figure 6a). Co-transfection of GFP-TPβ along with Cherry-HA-Siva1 appeared to accelerate and amplify all of the aforementioned processes (Figure 6b), with Siva1 translocation to the cytoplasm usually complete after 4–6 h and cell blebbing/contraction initiated after 6–8 h of receptor stimulation. Translocation and increase of expression of Siva1, as well as Siva1-induced apoptosis were also observed by immunostaining of the endogenous proteins (Figure 6e and Supplementary Material 4). However, in the absence of a transfection elevating total Siva1 expression, the apparition of apoptotic cells following U46619 stimulation required a concomitant treatment with sub-toxic doses of cisplatin, further supporting our dose–response results presented in Figure 2a. Finally, Siva1 translocation from the nucleus to the cytoplasm following endogenous TP stimulation was confirmed biochemically by performing cell fractionation experiments (Figures 6c and d).
Siva1 is predominantly nuclear but translocates to the cytoplasm upon TP stimulation. (a) Live confocal microscopy of Cherry-Siva1-transfected HeLa cells. Before stimulation, Siva1 mostly co-localizes with the Hoechst 33342-stained nucleus. After a 6 h U46619 stimulation of endogenous TP, Cherry-Siva1 fluorescence is noticeably increased, enabling the visualization of a cytosolic population. This population progressively increases until the nucleus is undistinguishable from the cytoplasm, at about 12 h of receptor stimulation. At this point in time, apoptosis hallmarks such as DNA condensation and cell contraction can be seen, culminating in extensive blebbing after 18 h of TP stimulation. (b) Co-transfection of GFP-TPβ with Cherry-Siva1 accelerates the process, with complete loss of nuclear demarcation on the Siva1 channel by 4 h and apparition of apoptosis hallmarks by 8 h of receptor stimulation. (e) Confocal microscopy of fixed HeLa cells stained for endogenous Siva1 reveals similar results. Initially low, Siva1 signal is increased upon a 16 h 1 mM U46619 stimulation where a cytoplasmic population also appears. As reported in Figure 2, concomitant sub-toxic 50 μM 16 h cisplatin treatment is required to visualize apoptosis in non-transfected cells. Scale bar is 10 μm. LUT table for all channels is shown on the left. (c) Fractionation experiments in HeLa cells show transfected Siva1-HA to be mainly localized to the nucleus, although, as with the confocal experiments, a cytosolic population can be seen. Upon endogenous TP stimulation, signal from the cytosolic fraction is increased relative to the nuclear fraction. Immunoblotting of GAPDH and lamin A/C show the adequate separation of the cytosolic and nuclear fractions, respectively. (d) Quantification of Siva1 found in the cytosolic fraction relative to that detected in the nuclear fraction
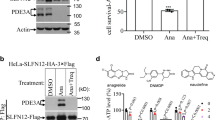
Siva1 is required for TP-mediated modulation of apoptosis
We next evaluated whether Siva1 expression was required for the modulation of apoptosis by TP. Two different FITC-labelled siRNAs targeting exon 2 and 4 of human Siva1 were transfected into HeLa cells (Figure 7a and Supplementary Material 4). Twenty-four hours after siRNA tranfections, cells were treated overnight with cisplatin and concomitantly stimulated with 1 μM U46619, the agonist concentration that maximally promoted the cisplatin-induced apoptosis in Figure 2a. Apoptosis assessment by annexin V staining and PARP cleavage demonstrated that the promotion of cisplatin-induced apoptosis by TP stimulation was severely compromised in cells transfected with the siRNAs targeting Siva1 compared with cells transfected with the control scrambled siRNA (Figure 7), confirming the importance of Siva1 in the modulation of apoptosis by TP.
Siva1 is required for apoptosis modulation by TP in HeLa cells. (a) Knockdown efficacy of siRNAs targeting exon 2 (siSiva A) and exon 4 (siSiva B) of Siva1 was assessed by western blotting of endogenous Siva. (b) Quantification of (a). (c and d) Cells were transfected with FITC-labeled siRNAs and treated with 1 μM U46619 or vehicle for 5 h, concomitant with an overnight 50 μM cisplatin treatment. Annexin V staining of transfected cells (c) and PARP cleavage (d) analysis show that Siva1 knockdown by both siRNAs significantly reduced promotion of apoptosis by U46619. Statistical analysis performed using unpaired t-test. *P<0.05 and **P<0.01
Discussion
When trying to sum up the results of various studies on the role of TXA2 in the modulation of apoptosis, one striking element that emerges is that most studies performed in primary cell cultures reported TP as a pro-apoptotic receptor (e.g., T lymphocytes,18 cardiomyocytes,17 platelets16), whereas the majority of studies reporting TXA2 as a pro-proliferative mediator were performed using either cancer cells (e.g., human bladder cancer specimens,25 pulmonary cancer cell line NCI-H23,26 or thromboxane synthase inhibitors.25, 27 In the latter case, deducing the outcome of TP signalling by using synthase inhibitors is challenging because, by blocking TXA2 synthesis, those inhibitors also drive the balance of eicosanoids towards other mediators such as prostacyclin28 that itself possesses pro-apoptotic properties.29 As for studies performed in cancerous cells, one must keep in mind that one of their most important features is their ability to evade apoptosis. To that end, the preponderance of cancerous cells show impaired p53 function.30 It is tempting to speculate that the outcome of TP signalling might shift from pro-apoptotic in ‘healthy cells’ to proliferative in cancer cells. Here, we demonstrated that siRNA-mediated knockdown of Siva1 severely reduced the promotion of apoptosis by TP. Because Siva1 is a direct transcriptional target of p53,7 we suggest that impaired p53 function might prevent Siva1 expression and therefore the promotion of apoptosis by TP. In support of this hypothesis, promotion of apoptosis by TXA2 required a concomitant cisplatin treatment in HeLa cells (Figure 2). Because Siva1 induction by U46619 and cisplatin is additive (Figure 4d), we believe that the co-treatment might be required to elevate Siva1 levels past the threshold required for TP signalling towards apoptosis – a situation that might not happen in p53-deficient cells.
In addition, we showed that the cisplatin treatment induced TXA2 production by HeLa cells. This suggests the presence of a positive feedback loop in which the DNA-damage-response in one cell might sensitize itself or neighbouring cells to DNA-damage-induced apoptosis. To the best of our knowledge, ours is the first in vitro demonstration of TXA2 production upon cisplatin treatment. Clinically, it was reported that urinary excretion of TXB2 was increased 4.5–fold during and immediately after cisplatin infusion in patients treated for various malignancies.31 TXA2 production was also observed following treatment with other cytotoxic drugs such as gentamicin32 and cyclosporine.33 This further supports the clinical relevance of our findings and implies that not only might a defective TP-Siva axis contribute to apoptosis resistance in tumours, but a functional TP-Siva axis in surrounding normal tissues and organs might also contribute to the toxicity of the chemotherapeutic treatment.
Whether Siva1 is pro- or anti-apoptotic has recently been the subject of debate,4, 11 which could be resolved in part by our data. Although Siva1 was mainly known to induce apoptosis through extrinsic, intrinsic and caspases-independent pathways,4, 5 an elegant study by Du et al.11 revealed that, by simultaneously binding p53 and Mdm2, Siva1 potentiated p53 ubiquitination and proteasomal degradation, effectively inhibiting apoptosis. Here, we demonstrate that following TP stimulation, Siva1 translocates from the nucleus to the cytosol where it progressively accumulates because of hindered degradation. As others reported that Siva1 stability could be decreased by LPA2-induced ubiquitination,34 we tried to assess whether the opposite would hold true with TP, where U46619 might decrease Siva1 ubiquitination. However, we found basal Siva1 ubiquitination levels to be so low that no further decrease could be observed (data not shown), suggesting that Siva1 stabilization by TP might occur through mechanisms other than regulation of protein ubiquitination, which might include phosphorylation, other ubiquitin-like modifiers or the N-end rule pathway. Aside from Siva1 stabilization, we also showed that TP stimulation enhances both pro-apoptotic Siva1/TRAF2 and Siva1/XIAP interactions while reducing the anti-apoptotic Siva1/Mdm2 interaction. With regard to the Siva1/Mdm2 interaction, the bearing of the residual co-immunoprecipitation signal observed following stimulation (Figure 5a) remains to be ascertained. It could be that some level of this anti-apoptotic interaction is actually maintained, but overrun by the stabilized cytoplasmic Siva1 interacting with XIAP and TRAF2. Another possibility would be that in cells destined to enter apoptosis, the anti-apoptotic Siva1/Mdm2 interaction is completely lost and that the impression of its conservation results from the fact that western blots study an unsynchronized cell population. Whatever the case, we do suggest that the Siva1 function at the nucleus might indeed be anti-apoptotic through the reported p53-Mdm2 scaffold and that its pro-apoptotic properties might appear once it has translocated to the cytoplasm where it can access not only TRAF2 and XIAP, but also the mitochondria5 where Bcl-2 and Bcl-xL are located. We believe this is the first model unifying the pro- and anti-apoptotic roles of Siva1 and showcasing a live modulation of Siva1 localization and function by agonist stimulation of a receptor. A schematic representation of our proposed mechanism is illustrated in Figure 8.
Proposed schematic model of Siva1 regulation. Siva1 is expressed at low levels in normal cells and is mainly localized at the nucleus, where it can bind Mdm2 and suppress p53 activity, thus promoting cell survival. TP stimulation induces a translocation of Siva1 to the cytoplasm, where it accumulates and interacts with Bcl-xL, XIAP and TRAF2 to promote apoptosis. Cisplatin treatment induces thromboxane A2 production and p53 activity through its DNA-damaging action, resulting in an induction of Siva1 transcription. Finally, Siva1 is required for the promotion of apoptosis by TP. We postulate that this prerequisite might not be met in cancerous cell lines with impeded p53 activity, possibly explaining why, to the best of our knowledge, TP was only ever shown to induce apoptosis in primary cell cultures
Lastly, we demonstrated that Siva1 directly interacts with the C-tail and intracellular loops of TPβ. Interestingly, total expression and localization of Siva1ΔC, which displayed significantly reduced interaction with TPβ, could be modulated by TP stimulation similarly to full-length Siva1 (data not shown). This could suggest that (1) the interaction is not involved in those two processes that would be triggered by other receptor signalling pathways; or (2) that the residual TPβ-Siva1 interaction is sufficient for TPβ to mediate its effects on Siva1. The fact that receptor stimulation decreased the co-immunoprecipitation with Siva1 suggests that the association might be constitutive, where TP could sequester a small cytoplasmic Siva1 fraction existing at the basal state and release it upon stimulation. This could further contribute to the TP-induced cytoplasmic Siva1 accumulation and enhanced interaction with pro-apoptotic partners. The correlation between TP-Siva1 dissociation and Siva1 stabilization would also support the observations reported for the anti-apoptotic LPA2 receptor where an agonist-induced stabilization of the LPA2-Siva1 interaction lead to increased Siva1 ubiquitination and degradation.34 In any case, ours is the first report of Siva1 interacting with a pro-apoptotic GPCR and the first to demonstrate that Siva1 expression is required to couple the receptor to apoptosis modulation. Whether the direct interaction between TP and Siva1 is required for this effect to occur or rather serve a distinct unknown function remains to be seen, but our data does reveal a completely new mechanism of GPCR-mediated apoptosis modulation that had never been appreciated before.
Better understanding of apoptosis regulation is critical not only to cancer research, but also to our comprehension of inflammatory and hypoxia responses. With its proven involvement in cardiovascular diseases, immune regulation and cancer,1 TXA2 is at the crossroads of all of those processes. We showed here that a DNA-damaging cisplatin treatment induced TXA2 synthesis in HeLa cells. In turn, stimulation of TP promoted cisplatin-induced apoptosis, which required Siva1 expression. We demonstrated that TP stimulation caused Siva1 to accumulate by inhibiting its degradation and provoked its translocation from the nucleus to the cytoplasm. This translocation resulted in decreased interaction with Mdm2, and enhanced association with XIAP and TRAF2. The model derived from our data explains, at least in part, the dual pro- and anti-apoptotic roles that were reported for Siva1. Together, our findings may have clinical implications in the use of COX inhibitors during cisplatin chemotherapy and provide mechanistic insight required to improve treatment effectiveness35 and alleviate some of its complications.36
Materials and Methods
Reagents
Anti-GST polyclonal anti-body (cat. A190-122A) was from Bethyl Laboratories (Montgomery, TX, USA). Rat monoclonal HRP-coupled anti-HA antibody (clone 3F10) was from Roche Diagnostics (Rothkreuz, Switzerland). Anti-PARP monoclonal antibody (cat. 556494) was from BD Pharmingen (Franklin Lakes, NJ, USA). Anti-GAPDH (FL-335), anti-Lamin A/C (H-110) anti-c-Myc (A-14) and anti-Siva (FL-175, C-20 and N-19) polyclonal antibodies, anti-Mdm2 (SMP14) monoclonal antibody and protein G PLUS-agarose were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Anti-FLAG monoclonal (M2) and polyclonal (F7425) antibodies were obtained from Sigma-Aldrich (St-Louis, MO, USA). Anti-human TP receptor polyclonal antibody (cat. 10004452) was from Cayman Chemical Company (Ann Arbor, MI, USA). XIAP (3B6) and TRAF2 (C192) polyclonal antibodies were from Cell Signalling Technology (Danvers, MA, USA). HRP-linked anti-Myc polyclonal antibody (ab1261) was from Abcam (Cambridge, UK). HRP-linked anti-rabbit (NA934V) and anti-mouse (NA931V) secondary antibodies were from GE Healthcare (Little Chalfont, UK). Alexa Fluor 546 goat anti-rabbit (cat. A-11035) secondary antibody was from Life Technologies (Grand Island, NY, USA). Cisplatin (cis-Diammineplatinum(II) dichloride, cat. P4394) and cycloheximide (cat. C4859) were from Sigma-Aldrich. U46619 (cat. 16450) and SQ29548 (cat. 19025) were from Cayman Chemical Company.
Plasmid constructs
The full-length open reading frame of Siva1 was cloned by RT-PCR using template RNA extracted from HeLa cells. The HA-tagged Siva1 constructs were generated by PCR using the Phusion High-Fidelity PCR system (New England Biolabs, Ipswich, MA, USA) and with primers containing the HA epitope in-frame with the C terminus of the Siva1 open reading frame. The PCR products were inserted into either the pcDNA3 expression vector (Life Technologies) to yield the Siva1-HA and Siva1ΔC-HA constructs or into the pRSETa expression vector (Invitrogen) to yield the 6 × His-Siva1-HA, 6 × His-Siva1ΔC-HA and 6 × His-Siva1ΔΔC-HA constructs. The Cherry-HA-Siva1 construct was generated by inserting the HA-tagged Siva1 ORF in the pmCherry plasmid (cat. 632522, Clontech, Mountain View, CA, USA). Generation of the TP constructs in the pGEX-4T-1 vector (GE Healthcare) was described previously.3 Myc-Mdm2, Myc-TRAF2 and Myc-XIAP were all cloned by RT-PCR from HeLa cells mRNA and inserted into the pcDNA3 expression vector (Invitrogen).
Cell culture, transfection and stimulation
HEK293 and HeLa cells were maintained in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (Invitrogen) at 37°C in a 5% CO2 humidified atmosphere. Transfections of both cell types were performed at 50–70% confluence using TransIT-LT1 Reagent (Mirus, Madison, WI, USA) according to the manufacturer's protocol. Whenever agonist or antagonist treatments were required, the culture medium was changed to medium containing the relevant compound (DMEM 0.5% BSA, 20 mM Hepes) 30 min before stimulation start and kept for the remaining of the experiment.
Yeast two-hybrid screen
The yeast two-hybrid screen was performed as described previously.3 Briefly, a plasmid containing the C-terminus of TPβ (pAS2-1–TPβCT) was transformed into the yeast strain pJ69-4a according to the lithium yeast transformation protocol. This stably transformed clone was then transformed with a Human HeLa MATCHMAKER cDNA Library or with the empty pGad424 plasmid (Clontech). Positive clones were initially selected for growth in the absence of histidine. Clones showing positive interactions were then isolated, and these interactions were confirmed by growth on quadruple selective media (Trp−, Leu−, His− and Ade−). pGADGH plasmids containing the library inserts from positive colonies were isolated and transformed into the DH10B bacterial strain. Plasmids were extracted from DH10B cells and transformed once more into yeast with either the bait (pAS2-1/TPβCT) or the negative control (pAS2-1) and plated on quadruple selective medium (Trp−, Leu−, His− and Ade−) to confirm the interaction. The selected plasmids were then sequenced by dideoxy sequencing, and the identities of the clones were determined by using the NCBI BLAST alignment tool.
Recombinant protein production and binding assays
His- and GST-tagged fusion proteins were produced in OverExpress C41(DE3) Escherichia coli strain (Avidis, St-Beauzire, France) according to the manufacturer's instructions. His-tagged recombinant proteins were purified using nickel-nitrilotriacetic acid-agarose resin (cat. 1018244 Qiagen, Hilden, Germany), while GST-tagged recombinant proteins were purified using glutathione-Sepharose 4B (cat. 17–0756–01, GE Healthcare) as per the manufacturers’ instructions. Purified recombinant proteins were analyzed by SDS-PAGE followed by Coomassie Brilliant Blue R-250 staining. Glutathione-Sepharose bound GST-tagged fusion protein was incubated with purified histidine protein in binding buffer (10 mM Tris, pH 7.4, 150 mM NaCl, 1 mM EDTA, 10% glycerol, and 0.5% Igepal) supplemented with protease inhibitors (9 mM pepstatin, 9 mM antipain, 10 mM leupeptin, and 10 mM chymostatin) and 2 mM DTT overnight at 4°C. The binding reactions were then washed four times with binding buffer. SDS sample buffer was added to the binding reactions, and the tubes were boiled for 5 min. The binding reactions were analyzed by SDS-PAGE, and immunoblotting was performed with the indicated specific antibodies.
Immunoprecipitations
HEK293 cells were transiently transfected with the indicated constructs and maintained as described above for 48 h in 60 mm petri dishes. Immunoprecipitations of endogenous proteins were performed in HeLa cells. Where indicated, cells were then stimulated with TP agonist U46619 at a 100 nM concentration for 5 h. Cells were subsequently washed with ice-cold phosphate-buffered saline (PBS) and harvested in 200 μl of lysis buffer (150 mM NaCl, 50 mM Tris, pH 8, 1% Igepal, 0.5% Sodium-deoxycholate, 0.1% SDS, 10 mM Na4P2O7, and 5 mM EDTA) supplemented with protease inhibitors (9 nM pepstatin, 9 nM antipain, 10 nM leupeptin, and 10 nM chymostatin (Sigma-Aldrich). After incubation in lysis buffer for 60 min at 4°C, the lysates were cleared by centrifugation for 20 min at 14 000 r.p.m. at 4°C. Lysates were brought to equal protein concentration following protein dosage with the DC protein assay kit (cat. 500–0112, Bio-Rad, Hercules, CA, USA) and 1 μg of specified antibody was added to between 500 and 900 μg of supernatant, depending on the experiment. After an overnight incubation at 4°C, 30 μl of 50% protein G-agarose was added, followed by a 1 h incubation at 4°C. Samples were then centrifuged for 1 min and washed three times with 1 ml of lysis buffer. Immunoprecipitated proteins were eluted by the addition of 25 μl of Laemmli buffer followed by a 30-min incubation at 37°C. Initial lysates and immunoprecipitated proteins were analyzed by SDS-PAGE and immunoblotting using specific antibodies.
Apoptosis induction and assessment
HeLa cells were harvested to 50% confluence. Culture medium was then changed for stimulation medium (DMEM 0.5% BSA, 20 mM Hepes) containing cisplatin at the specified concentration, along with the indicated agonists or antagonists. If siRNAs were to be transfected, cells were allowed to reach 80–90% confluence and transfection occurred one day before the start of the cisplatin treatment. Sixteen to twenty-four hour following the start of the cisplatin treatment, cells were washed with 1 ml of room temperature PBS and trypsinized for 15 min. Trypsinization was stopped by the addition of DMEM 10% FBS culture medium and cells collected in 15 ml tubes using polystyrene pipettes. During this procedure, initial culture medium and washing buffer were collected along with the trypsinized cells to ensure that cells floating before trypsinization were included in the experiment. Pipette ‘up and downs’ were avoided as much as possible. Cells were pelleted by centrifugation at no more than 300 g and washed in 1 ml of annexin V binding buffer (150 mM NaCl, 10 mM Hepes, 2.5 mM CaCl2), before being finally resuspended in 100 μl of annexin V binding buffer containing 3 μl of Alexa fluor 647–conjugated annexin V (cat. 640912, BioLegend, San Diego, CA, USA) and 1 μM propidium iodide (Molecular Probes). Cells were incubated 15 min on ice before being read on a FACSCalibur (BD Biosciences, Franklin Lakes, NJ, USA) flow cytometer using appropriate lasers and filter sets. BD's CellQuest Pro 5.2.1 software was used to acquire and analyze 30 000 events. If siRNAs were transfected, the green FL-1 channel was used to assess transfection efficiency (usually about 60–70%) and non-transfected cells were excluded from the analysis. Remaining cells after the FACS reading were then pelleted and lysed in 50 μl of a highly denaturating lysis buffer (100 mM NaCl, 50 mM Tris, pH 8, 1 mM EDTA, 1% Igepal, 0.5% sodium-deoxycholate, 1% SDS and 4 M urea) for 60 min. Lysates were cleared by centrifugation, dosed using the DC protein assay kit (cat. 500–0112, Bio-Rad) and SDS-PAGE and immunobloting were performed using 50 μg to reveal PARP cleavage.
Thromboxane production assay
HeLa cells harvested to 50% confluence were treated with various concentrations of cisplatin for 48 h. Culture medium was collected and analyzed using the TXB2 EIA kit (cat. 519031) from Cayman Chemical Company, as per the manufacturer's instructions.
Siva1 expression
HEK293 cells were plated on day 1, transfected as indicated on day 2 and stimulated on day 4. For experiments assessing the expression of endogenous proteins, stimulations were performed in HeLa cells upon achievement of desired confluency. Cells were then washed with ice-cold PBS and harvested in 50 μl of lysis buffer (150 mM NaCl, 50 mM Tris, pH 8, 1% Igepal, 0.5% Sodium-deoxycholate, 0.1% SDS, 10 mM Na4P2O7, and 5 mM EDTA) supplemented with protease inhibitors (9 nM pepstatin, 9 nM antipain, 10 nM leupeptin, and 10 nM chymostatin (Sigma-Aldrich). After incubation in lysis buffer for 60 min at 4°C, the lysates were cleared by centrifugation for 20 min at 14 000 r.p.m. at 4°C. Lysate concentration was assessed with the DC protein assay kit (cat. 500–0112, Bio-Rad) and 30–50 μg of proteins were denaturated using Laemmli sample buffer and submitted to SDS-PAGE, western blotting on nitrocellulose membranes (BA85 Protran, Whatman, Kent, UK) and immunolabelling using the specified antibodies. When multiple immunolabelings were required, membranes were striped by two sequential 7 min room-temperature incubations in water 0.2 M NaOH. After extensive washing to remove residual NaOH, membranes were immunolabeled again.
Cycloheximide chase assay
HEK293 cells were transfected with FLAG-TPβ and Siva1-HA. After 48 h, culture medium was changed for the stimulation medium and cells were treated for 3 h with 100 nM U46619. Cycloheximide was then added to reach a final concentration of 100 μg/ml and cells were harvested for 15, 30, 60, 120 or 180 min. At the required times, cells were washed with ice-cold PBS, collected, pelleted and flash-frozen in liquid nitrogen. Once all samples were frozen, cells were lysed as described for the Siva1 expression experiment and 30–50 μg of lysate proteins were analyzed by SDS-PAGE, western blotting and immunolabelling using the specified antibodies.
Confocal microscopy
Live confocal microscopy was performed in HeLa cells plated and transfected with appropriate plasmids in Lab-Tek II chambered coverglass (cat. 155379, Thermo Fischer Scientific, Waltham, MA, USA). The day following transfection, the cell culture medium was changed to stimulation medium containing 1 μg/ml Hoechst 33342 (cat. H21492, Life Technologies) and cells were serum-starved for 4 h. The slide was then loaded on a H117 ProScan II (Prior Scientific, Cambridge, UK) high-precision motorized stage coupled to a FV1000 confocal microscope (Olympus, Richmond Hill, ON, Canada). Environmental control systems from Solent Scientific (Segensworth, UK) were used to maintain a 37°C temperature and constant CO2 and moisture levels throughout the experiment. Five to six fields containing 3–10 transfected cells were selected in each of the two chambers and their coordinates were entered as a multi-area time-lapse protocol in the FV10-ASW 2.1.3.10 software (Olympus). Five-layers Z-stack acquisitions were performed using a 63 × oil immersion objective. Each field was imaged once before stimulation and then once per hour for 18 h after the addition of agonist in one of the two chambers. To minimize laser exposure, the confocal aperture was set to 300 μM and, in addition to the differential interference contrast signal, no more than two fluorescence channels were acquired in a single experiment. Hoechst and Cherry channels were acquired simultaneously, but a sequential acquisition was favoured for the GFP and Cherry combination because of fluorescence spectrum overlay concerns. ZDC focus drift compensation was used throughout the experiment. For fixed-cells confocal microscopy, HeLa cells were plated onto coverslips and grown overnight in DMEM 10% FBS. Cells were fixed with 3% paraformaldehyde in PBS, washed with PBS, permeabilized with 0.1% Triton X-100 (cat. ICN807423, Thermo Fisher Scientific) in PBS, and blocked with 0.1% Triton X-100 in PBS containing 5% nonfat dry milk. Cells were then incubated with primary antibodies diluted in blocking solution, washed twice with PBS, blocked again with 0.1% Triton X-100 in PBS containing 5% nonfat dry milk, and incubated with appropriate secondary antibodies diluted in blocking solution. The cells were washed twice with permeabilization buffer, incubated 5 min in a Hoechst 33342-containing PBS solution and washed thrice with PBS. Coverslips were finally mounted using ProLong Gold antifade reagent (cat. P36934, Molecular Probes). Confocal acquisitions were performed sequentially for each channel and every microscope slides within a single experiment were read on the same day and using the same settings. Following acquisition, images were pseudocolored using the FV10-ASW 2.0.1.0 viewer software (Olympus).
Cell fractionation
Fractionation was performed according to the Rapid, Efficient And Practical method.37 Briefly, HeLa cells transfected with the Siva1-HA construct were stimulated 5 h with 100 nM U46619, washed in ice-cold PBS and resuspended in 900 μl of PBS 0.1% Igepal to permeate the plasma membrane. After a 10-s pop-spin, 300 μl of the supernatant was collected and considered the cytosolic fraction, which was then denaturated using 100 μl of 4 × Laemmli sample buffer. The remaining pellet was then washed with 1 ml of PBS 0.1% Igepal and resuspended in 180 μl of Laemmli sample buffer to become the nuclear fraction. The nuclear fraction was sonicated and both fractions were boiled for 5 min before being loaded for SDS-PAGE, western blotting and immunolabelling.
siRNA knockdown
Custom FITC-labeled Stealth siRNAs were purchased from Invitrogen. The siSiva A (sense: 5′-AGUGCUGUGCACCAGCUGUTT-3′ anti-sense: 5′-ACAGCUGGUGCACAGCACUTT-3′) was targeted at exon 2, while the siSiva B (sense: 5′-GACCAAGCGACUCCUGUUCTT-3′, anti-sense: 5′-GAACAGGAGUCGCUUGGUCTT-3′) was targeted at exon 4. A scrambled version of siSiva A was also ordered (sense: 5′-GUGCUCUGCGACGUUGACATT-3′ anti-sense: 5′-UGUCAACGUCGCAGAGCACTT-3′) and used as a control. siRNAs were transfected in HeLa cells using Lipofectamine 2000 (Invitrogen) following the manufacturer's HeLa cell specific protocol.
Image densitometry
Western blot quantification was meticulously performed using a procedure we developed based on the recommendations of Gassmann et al.38 Specifically, all quantified immunoblots were revealed using the same type of films (X-OMAT Blue XB, cat. 1776699, PerkinElmer, Waltham, MA, USA) and carefully exposed to avoid saturation. Films were scanned using a dual lens Epson Perfection v700 Photo scanner (Epson, Markham, ON, Canada) and the EPSON Scan Ver. 3.25A (Universal) software. Acquisition was performed at 400 dpi in 16-bits grayscale with auto-exposure and colour-correction options turned off. Images were analyzed using the ImageJ 1.42q software. Lanes were selected and plotted using the ‘Gel analyzer’ functions with only the central third of the lanes width being included by the lane selection rectangle. Peaks on the plots were individually closed to the background level of each lane using the ‘Straight line’ tool and the enclosed area was measured using the ‘Wand’ tool. Results were compiled in Microsoft Excel for Mac 2011 v14.1.0 (Microsoft Corporation, Bellevue, WA, USA) and reported as the mean of all quantified experiments with standard deviation.
Statistical analysis
EC50 and half-life calculations were performed in Prism 5.0b. (GraphPad Software, La Jolla, CA, USA) using, respectively, the ‘log (agonist) versus response (three parameters)’ and the ‘One phase decay’ pre-set analyses and reported accordingly. Statistical analysis were also performed in Prism 5.0b using the test and parameters mentioned in the figure legends.
Abbreviations
- BSA:
-
bovine serum albumin
- C-tail:
-
C-terminal tail
- CMV:
-
cytomegalovirus
- COX:
-
cyclo-oxygenase
- DMEM:
-
Dulbecco's modified Eagle's medium
- GAPDH:
-
glyceraldehydes-3-phosphate dehydrogenase
- GFP:
-
green fluorescent protein
- GPCR:
-
G protein-coupled receptor
- GST:
-
glutathione transferase
- HA:
-
haemagglutinin
- HEK-293 cell:
-
human embryonic kidney cell
- His6:
-
hexahistidine
- HRP:
-
horseradish peroxidise
- IB:
-
immunoblot
- ICL:
-
intracellular loop
- IP:
-
immunoprecipitation
- JNK:
-
c-jun N-terminal kinase
- LPA:
-
lysophosphatidic acid
- Mdm2:
-
murine double minute 2
- NSAIDs:
-
non-steroidal anti-inflammatory drugs
- PARP:
-
poly (ADP-ribose) polymerase
- PBS:
-
phosphate-buffered saline
- siRNA:
-
small inhibitor RNA
- S1P:
-
sphingosine-1-phosphate
- TBS:
-
Tris-buffered saline
- TNF:
-
tumour necrosis factor
- TP:
-
thromboxane A2 receptor
- TRAF:
-
TNF receptor-associated factor
- TX:
-
thromboxane
- XIAP:
-
X-linked inhibitor of apoptosis protein
References
Nakahata N . Thromboxane A2: physiology/pathophysiology, cellular signal transduction and pharmacology. Pharmacol Ther 2008; 118: 18–35.
Parent JL, Labrecque P, Orsini MJ, Benovic JL . Internalization of the TXA2 receptor alpha and beta isoforms. Role of the differentially spliced cooh terminus in agonist-promoted receptor internalization. J Biol Chem 1999; 274: 8941–8948.
Parent A, Laroche G, Hamelin E, Parent J-L . RACK1 regulates the cell surface expression of the G protein-coupled receptor for thromboxane A(2). Traffic 2008; 9: 394–407.
Py B, Slomianny C, Auberger P, Petit PX, Benichou S . Siva-1 and an alternative splice form lacking the death domain, Siva-2, similarly induce apoptosis in T lymphocytes via a caspase-dependent mitochondrial pathway. J Immunol 2004; 172: 4008–4017.
Singaravelu K, Padanilam BJ . p53 target Siva regulates apoptosis in ischemic kidneys. Am J Physiol Renal Physiol 2011; 300: F1130–F1141.
Padanilam BJ, Lewington AJ, Hammerman MR . Expression of CD27 and ischemia/reperfusion-induced expression of its ligand Siva in rat kidneys. Kidney Int 1998; 54: 1967–1975.
Barkinge JL, Gudi R, Sarah H, Chu F, Borthakur A, Prabhakar BS et al. The p53-induced Siva-1 plays a significant role in cisplatin-mediated apoptosis. J Carcinog 2009; 8: 2.
Fortin A, MacLaurin JG, Arbour N, Cregan SP, Kushwaha N, Callaghan SM et al. The proapoptotic gene SIVA is a direct transcriptional target for the tumor suppressors p53 and E2F1. J Biol Chem 2004; 279: 28706–28714.
Chu F, Borthakur A, Sun X, Barkinge J, Gudi R, Hawkins S et al. The Siva-1 putative amphipathic helical region (SAH) is sufficient to bind to BCL-XL and sensitize cells to UV radiation induced apoptosis. Apoptosis 2004; 9: 83–95.
Resch U, Schichl YM, Winsauer G, Gudi R, Prasad K, de Martin R . Siva1 is a XIAP-interacting protein that balances NFkappaB and JNK signalling to promote apoptosis. J Cell Sci 2009; 122 (Pt 15): 2651–2661.
Du W, Jiang P, Li N, Mei Y, Wang X, Wen L et al. Suppression of p53 activity by Siva1. Cell Death Differ 2009; 16: 1493–1504.
Spinicelli S, Nocentini G, Ronchetti S, Krausz LT, Bianchini R, Riccardi C . GITR interacts with the pro-apoptotic protein Siva and induces apoptosis. Cell Death Differ 2002; 9: 1382–1384.
E S, Lai Y-J, Tsukahara R, Chen C-S, Fujiwara Y, Yue J et al. Lysophosphatidic acid 2 receptor-mediated supramolecular complex formation regulates its antiapoptotic effect. J Biol Chem 2009; 284: 14558–14571.
Prasad KV, Ao Z, Yoon Y, Wu MX, Rizk M, Jacquot S et al. CD27, a member of the tumor necrosis factor receptor family, induces apoptosis and binds to Siva, a proapoptotic protein. Proc Natl Acad Sci USA 1997; 94: 6346–6351.
Ekambaram P, Lambiv W, Cazzolli R, Ashton AW, Honn KV . The thromboxane synthase and receptor signaling pathway in cancer: an emerging paradigm in cancer progression and metastasis. Cancer Metastasis Rev 2011; 30: 397–408.
Lin KH, Chang HC, Lu WJ, Jayakumar T, Chou HC, Fong TH et al. Comparison of the relative activities of inducing platelet apoptosis stimulated by various platelet-activating agents. Platelets 2009; 20: 575–581.
Shizukuda Y, Buttrick PM . Protein kinase C-zeta modulates thromboxane A(2)-mediated apoptosis in adult ventricular myocytes via Akt. Am J Physiol Heart Circ Physiol 2002; 282: H320–H327.
Remuzzi G, Noris M, Benigni A, Imberti O, Sayegh MH, Perico N . Thromboxane A2 receptor blocking abrogates donor-specific unresponsiveness to renal allografts induced by thymic recognition of major histocompatibility allopeptides. J Exp Med 1994; 180: 1967–1972.
Liel N, Mais DE, Halushka PV . Binding of a thromboxane A2/prostaglandin H2 agonist [3H]U46619 to washed human platelets. Prostaglandins 1987; 33: 789–797.
Severino A, Abbruzzese C, Manente L, Valderas ÁA, Mattarocci S, Federico A et al. Human papillomavirus-16 E7 interacts with Siva-1 and modulates apoptosis in HaCaT human immortalized keratinocytes. J Cell Physiol 2007; 212: 118–125.
Gudi R, Barkinge J, Hawkins S, Prabhakar B, Kanteti P . Siva-1 promotes K-48 polyubiquitination of TRAF2 and inhibits TCR-mediated activation of NF-kappaB. J Environ Pathol Toxicol Oncol 2009; 28: 25–38.
Brown DR, Thomas CA, Deb SP . The human oncoprotein MDM2 arrests the cell cycle: elimination of its cell-cycle-inhibitory function induces tumorigenesis. EMBO J 1998; 17: 2513–2525.
Vischioni B, van der Valk P, Span SW, Kruyt FAE, Rodriguez JA, Giaccone G . Expression and localization of inhibitor of apoptosis proteins in normal human tissues. Hum Pathol 2006; 37: 78–86.
Lin Y, Ryan J, Lewis J, Wani MA, Lingrel JB, Liu Z-G . TRAF2 exerts its antiapoptotic effect by regulating the expression of Krüppel-like factor LKLF. Mol Cell Biol 2003; 23: 5849–5856.
Moussa O, Riker JM, Klein J, Fraig M, Halushka PV, Watson DK . Inhibition of thromboxane synthase activity modulates bladder cancer cell responses to chemotherapeutic agents. Oncogene 2008; 27: 55–62.
Huang R-Y, Li M-Y, Hsin MKY, Underwood MJ, Ma LT, Mok TSK et al. 4-Methylnitrosamino-1-3-pyridyl-1-butanone (NNK) promotes lung cancer cell survival by stimulating thromboxane A2 and its receptor. Oncogene 2011; 30: 106–116.
Yoshizato K, Zapf S, Westphal M, Berens ME, Giese A . Thromboxane synthase inhibitors induce apoptosis in migration-arrested glioma cells. Neurosurgery 2002; 50: 343–354.
Datar S, McCauley FA, Wilson TW . Testing the ‘redirection hypothesis’ of prostaglandin metabolism in the kidney. Prostaglandins 1987; 33: 275–285.
Hatae T, Wada M, Yokoyama C, Shimonishi M, Tanabe T . Prostacyclin-dependent apoptosis mediated by PPAR delta. J Biol Chem 2001; 276: 46260–46267.
Plati J, Bucur O, Khosravi-Far R . Dysregulation of apoptotic signaling in cancer: molecular mechanisms and therapeutic opportunities. J Cell Biochem 2008; 104: 1124–1149.
Blöchl-Daum B, Pehamberger H, Kurz C, Kyrle PA, Wagner O, Müller M et al. Effects of cisplatin on urinary thromboxane B2 excretion. Clin Pharmacol Ther 1995; 58: 418–424.
Papanikolaou N, Peros G, Morphake P, Gkikas G, Maraghianne D, Tsipas G et al. Does gentamicin induce acute renal failure by increasing renal TXA2 synthesis in rats? Prostaglandins Leukot. Essent Fatty Acids 1992; 45: 131–136.
Rossini M, Belloni A, Remuzzi G, Perico N . Thromboxane receptor blockade attenuates the toxic effect of cyclosporine in experimental renal transplantation. Circulation 1990; 81 (1 Suppl): I61–I67 discussion I68.
Lin F-T, Lai Y-J, Makarova N, Tigyi G, Lin W-C . The lysophosphatidic acid 2 receptor mediates down-regulation of Siva-1 to promote cell survival. J Biol Chem 2007; 282: 37759–37769.
Czembirek C, Eder-Czembirek C, Erovic BM, Turhani D, Selzer E, Thurnher D . Inhibition of cytotoxicity of cisplatin by cyclooxygenase-2 inhibitor nimesulide in head and neck cancer cell lines. Oncol Rep 2005; 14: 1523–1526.
Togna GI, Togna AR, Franconi M, Caprino L . Cisplatin triggers platelet activation. Thromb Res 2000; 99: 503–509.
Suzuki K, Bose P, Leong-Quong RY, Fujita DJ, Riabowol K . REAP: a two minute cell fractionation method. BMC Res Notes 2010; 3: 294.
Gassmann M, Grenacher B, Rohde B, Vogel J . Quantifying Western blots: pitfalls of densitometry. Electrophoresis 2009; 30: 1845–1855.
Acknowledgements
CI-M thanks Dr Audrey Parent for her helpful advice and training in the early phases of this project. We are also grateful to Dr Leonid Volkov for his expertise in confocal microscopy and flow cytometry, and to Dr Jean-Bernard Denault for his guidance with regard to apoptosis detection techniques. CIM has a MD-PhD scholarship from the Fonds de la recherche en santé du Québec. This work was supported by a grant from the Natural Sciences and Engineering Council of Canada (to J-LP). J-LP receives a ‘Chercheur boursier-Sénior’ salary award from the Fonds de la recherche en santé du Québec and is the holder of the ‘André-Lussier Research Chair’.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by H Ichijo
Supplementary Information accompanies the paper on Cell Death and Differentiation website
Rights and permissions
About this article
Cite this article
Iorio-Morin, C., Germain, P., Roy, S. et al. Thromboxane A2 modulates cisplatin-induced apoptosis through a Siva1-dependent mechanism. Cell Death Differ 19, 1347–1357 (2012). https://doi.org/10.1038/cdd.2012.11
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cdd.2012.11
Keywords
This article is cited by
-
Molecular characterization, expression, and apoptosis regulation of siva1 in protogynous hermaphrodite fish ricefield eel (Monopterus albus)
Fish Physiology and Biochemistry (2021)
-
Lentivirus-Mediated Overexpression of SIVA-1 Reverses Cisplatin Resistance in Gastric Cancer in vitro
Cell Biochemistry and Biophysics (2020)