Abstract
To discuss the status of epidemiology of stroke in the Mongolian and Han population aged over 45 years and to understand the treatment and prevention of stroke. Data collected on stroke populations aged over 45 years in the six areas in Inner Mongolia were analyzed by using stratified multi-stage cluster sampling. The prevalence rate of stroke in patients aged over 45 years in Inner Mongolia was 4.62%. The stroke prevalence rate increased with age in both males and females, the Han and Mongolian populations, and was higher in males than in females in Inner Mongolia. The prevalence rate of stroke in the Mongolian population was higher than in the Han population. The incidence rate of stroke in patients aged over 45 years in Inner Mongolia was 0.28%, of which the rate of relapsed ischemic stroke was 23.29%. The proportion of ischemic stroke in the stroke patients was higher than hemorrhagic stroke. The prevalence and incidence rates of stroke in patients aged over 45 years in Inner Mongolia were high. The prevalence rate of stroke in both the Han population and the Mongolian population increased with age. Ischemic stroke was the major form of stroke.
Similar content being viewed by others
Introduction
Stroke is a cerebral blood circulation disorder that can cause acute cerebral blood circulation obstacles for various reasons, such as atherostenosis, arterial occlusion, and arteriorrhexis in the brain. Stroke causes temporary or permanent nerve dysfunction, and has high prevalence, death, and disability rates1. From 1990 to 2010, the number of strokes worldwide doubled to 33 million. Currently, there are 16.9 million stroke patients each year worldwide, and the prevalence rate of stroke is 0.26%. The burden of stroke has increased worldwide because of the increasing sizes and aging of populations2,3, especially in low- and middle-income countries4,5. Economic development improved quality of life, and Western influence has affected disease patterns and aging. The occurrence of stroke in young patients greatly affects the economic situation and labor productivity in our country. The prevention and control of stroke is comprehensive in big cities and the developed eastern area of China because of good economic and medical condition. However, the epidemiological investigation of stroke in the western areas of China is less comprehensive because of bad economic and medical conditions. The prevention of stroke in minority areas apparently lags behind the developed provinces and cities, which does not benefit the health work in minority areas6,7.
Inner Mongolia is located along the northern border of China, which is an alpine region without convenient transportation. The diet is simple there, but the high intake of salt and fat may cause hypertension and cardiovascular disease. Hence, it is meaningful to raise the levels of the prevention of chronic diseases in these areas, as well as to improve the quality of life and health care and to construct a harmonious society by enhancing the study of the comprehensive prevention of stroke.
In this study, we investigated the status of the epidemiology of stroke in patients aged over 45 years among the Mongolian and Han populations in Inner Mongolia. The objective was to understand the treatment and prevention of stroke, which could provide a basis for making reasonable and effective prevention policies. Standardized management was used in the stroke populations. Establishing individual health records could lay a solid foundation for a prospective cohort study on stroke patients.
Materials and Methods
Sample population
We used stratified multi-stage cluster sampling to select six areas in Inner Mongolia-Hohhot, Baotou, Hulunbuir, Bayannaoer, Xilinguole League, and Xingan League-because of their unique geographical location. The six areas were chosen by using the primary cluster sampling, and then relevant county seats were randomly selected using the secondary cluster sampling. The county seats were divided into two levels (urban and rural) according to the economic conditions. A corresponding number of communities were selected according to the sample size, and 20% communities were selected as a reference. The number of samples was determined by the proportion of the population in the six areas. We selected 10,779 residents aged over 45 years, including the Mongolian population, the Han population, and other nationalities. The human related study was approved by the ethics committee of First Affiliated Hospital of Inner Mongolia Medical University and each patient provided informed consent.
Diagnostic criteria
We used the standard formulated at the Fourth National Cerebrovascular Disease Conference8 to diagnose stroke, and confirmed it by imaging examination. To improve the accuracy of the investigation, three attending doctors reached a consensus of diagnosis when it was difficult to make a decision. If the attending doctors could not reach a consensus, then another senior doctor would participate in the discussion and make the decision. The leaked individuals in the first stage were checked. Each case was discussed and analyzed repeatedly according to the detailed medical history and physical examination. The head of the project made the final diagnosis combined with the examination results. Ischemic stroke was diagnosed by the criteria used in Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification9.
Investigation method
Questionnaires were used for this cross-sectional study. The preparations and the field survey were conducted from Jan 2013 to Dec 2014. Follow-ups, second reviews, second interviews, analyses, and data analyses were conducted from Jan 2015 to Dec 2015. The investigation was divided into two stages. In the first stage, agreement was obtained from the family members of households for interviewers from the Center for Disease Prevention and Control to collect basic information about screening and individual symptoms. In the second stage, trained neurologists re-checked the confirmed and suspected stroke cases mainly using data collected from the concentrated survey and the telephone survey. They carefully examined the medical history of physical and neurological examinations with reference to the hospitalization records and laboratory data. They checked the results according to the diagnostic criteria of stroke.
Analysis of risks
The NIH Stroke Scale (NIHSS) is used for stroke severity measure in this study. Fifteen categories of brain function that are commonly affected by stroke are measured, and each item is scored between 0 and 4 points, including: best gaze level (0–2 points), consciousness level (0–3 points), consciousness questions level (0–2 points), consciousness commands level (0–2 points), left motor arm (0–4 points), right motor arm (0–4 points), left motor leg (0–4 points), right motor leg (0–4 points), limb ataxia (0–2 points), sensory (0–2 points), visual level (0–3 points), facial palsy level (0–3 points), best language (0–3 points), dysarthria (0–2 points), extinction and inattention (0–2 points). Chi-square test was used to assess the difference of scores in each risk factor.
Statistical analysis
EpiData 3.1 was used to input the data and SPSS 13.0 was used for the data analysis. The enumeration data were analyzed by the χ2 test, and the results were according to mean number ± standard deviation. The statistical significance of differences between males and females, Han population and the Mongolian population were evaluated using the four-fold table chi-square test; the differences in the of the education levels, careers, family structures were analyzed by rows × columns chi-square test; and the differences in different age periods were analyzed using linear trend chi-square test11,11. P < 0.05 was considered statistically significance.
Ethic Statement
The human related study was approved by the ethics committee of First Affiliated Hospital of Inner Mongolia Medical University and each patient provided informed consent.
Results
Characteristics of the sample population
This survey obtained complete data for 10,779 people aged over 45 years from six areas of Inner Mongolia. Five hundred and fifty-eight patients suspected of stroke were primary-screened, and the response rate was 99.28%. Four patients suspected of stroke did not reply, because they were not available, could not be contacted, or refused to be investigated. Four hundred and ninety-eight patients were diagnosed with stroke. In the Han population, there were higher proportions of stroke in female patients, patients with a minimum education level of junior middle school, and patients living with a spouse. There were significant differences between the education levels in the Han and Mongolian populations, as well as careers and family structures (Tables 1 and 2).
Statistical results
The prevalence rate of stroke in patients aged over 45 years in Inner Mongolia was 4.62%, and the standardized prevalence rate was 4.64%. The standardized prevalence rates of stroke in males and females were 2.56% and 2.07%, respectively (Table 3). The standardized prevalence rates in the Han and Mongolian populations were 3.95% and 0.02%, respectively. The prevalence rate of stroke was higher in males than in females aged over 45 years (x2 = 4.854a, P = 0.028), and there was a significant difference between them. The prevalence rate of stroke in the Mongolian population was higher than in the Han population (x2 = 12.808b, P = 0.002), and there was significant difference between them (Table 4).
The prevalence rates of stroke in patients aged over 45 years increased with age, and there were significant differences between age groups (x2 = 253.301, P = 0.000) (Table 5). The prevalence rates of stroke in patients aged over 45 years were higher in males than in females, in which the prevalence rates of stroke in patients aged between 45 and 55 years were higher in females than in males; while the prevalence rates of stroke in patients aged between 55 to 65 years, 65 to 75 years and over 75 years were higher in males than in females. The prevalence rate of stroke patients increased with age, and there were significant differences between them (male: χ2 = 132.086, p = 0.000; female: χ2 = 121.725, p = 0.000) (Table 5).
The prevalence rates of stroke in the Mongolian and Han populations increased with age, and there were significant differences between age groups (χ2 = 245.474, P = 0.000) (Table 6). The prevalence rates in the Mongolian population from 45 to 55, 55 to 65, 65 to 75 years and over 75 years were significantly higher than in the Han population, especially in the 55 to 65 age group, in which the prevalence rate was twice as high as in the Han population. Overall, the prevalence rate of stroke patients aged over 45 years was higher in the Mongolian population than in the Han population. There were significant differences between the age groups (Han population: χ2 = 209.609, P = 0.000; Mongolian population: χ2 = 48.459, P = 0.000) (Table 6).
The incidence and recurrence of stroke
Thirty cases of stroke were diagnosed from 01 January 2014 to 31 December 2014, including two death cases. The incidence rate of stroke was 0.28%. Four hundred and ninety-eight stroke patients were surveyed, among which stroke did not reoccur in 382 patients; the number of stroke patients who relapsed once, twice, three times, and four times were 73 (14.66%), 33 (6.63%), 6 (1.2%) and 4 (0.8%), respectively (Table 7). The relapsed patients accounted for 23.29% of all stroke patients. Cerebral infarction recurred in 30 cases, and lacunar infarction recurred in two cases. Cerebral hemorrhage recurred in one case, and subarachnoid hemorrhage recurred in one case.
Classification of stroke
Among the stroke patients, there were 435 cases of cerebral ischemic stroke (87.35%) and 63 cases of hemorrhagic stroke (12.65%). There were eight cases of cerebral embolism among the cerebral ischemic stroke patients (1.84%) and three cases of subarachnoid hemorrhage among the hemorrhagic stroke patients (4.76%) (Table 8). In the Han population, the proportion of cerebral infarction in stroke patients was higher than cerebral hemorrhage in stroke patients. There were significant differences between the Mongolian and Han populations in the classification of stroke (χ2 = 6.511a, P = 0.011). The proportions of large-artery athero-sclerosis (LAA) and small-artery occlusion lacunar (SAO) were higher in the TOAST classification of cerebral ischemic stroke. There were no significant differences between the Mongolian population and the Han population in the TOAST classification of cerebral ischemic stroke (χ2 = 3.497a, P = 0.478).
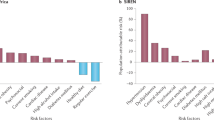
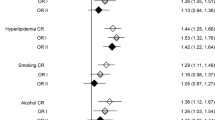
Analysis of risk factors in stroke
A case-control study on the risk factors of stroke was conducted in 1: 4 matched stroke patients of Mongolian and Han population by age, sex and origin. We found there were significant differences of scores in risk factors between Mongolian and Han populations. In Mongolian population, there were significant differences in the scores of hypertension, diabetes and drinking; while in Han population, there were significant differences in the scores of hypertension, diabetes and hyperlipidemia. Hence, hypertension and diabetes were the common risk factors in Mongolian and Han populations (Tables 9 and 10).
Discussion
The results showed significant differences between nationalities in the prevalence of stroke. In 1985, a national epidemiology investigation of stroke12 showed that the standardized prevalence rate of cerebrovascular disease was 0.31%. In 2003, Feigin et al.13 reviewed the existing studies of the prevalence rate of stroke in 10 countries. The standardized prevalence rate of stroke in people aged over 65 years ranged between 4.6% and 7.3%. According to the reports from different countries worldwide, the prevalence rate of stroke ranged from 0.4% to 1%. The prevalence rate of the white (except Hispanic) in the United States, the black (except Hispanic), Hispanics, and people in Pacific region were 2.3%, 4%, 2.6%, and 1.6%, respectively.
Our country had a high incidence rate of stroke. The distribution of stoke was consistent with hypertension. The prevalence rate of stroke in the northern region was higher than in the southern region. The median age of onset in the eastern region was 61 years, 59 years in the central region and 57 years in the western region14, which might be related to economics and medical conditions. Three large-scale surveys on stroke in China were conducted in 1985, 1986, and 19919,15,16. Because the survey year and age–sex structure of the investigation area varied in these previous studies, their results might differ from those in our study.
In Inner Mongolia, the prevalence rate of stroke was lower than in developed countries. However, because of the backward economic and medical conditions in Inner Mongolia, it was still higher than in other regions in China. Because the population aged over 75 years was lower than other age groups, the prevalence rate was significantly lower than other age groups. According to the demographic yearbook17, the population aged over 70 years in the Mongolian population was lower than other age groups; therefore, the prevalence rate of patients aged over 75 years was significantly lower than in the Han population. The prevalence rates of patients aged 45 to 55, 55 to 65, and 65 to 75 years were significantly higher than in the Han population, which might be related to geographical location, culture, education, and alcohol consumption in Inner Mongolia. The prevalence rates of stroke in the age groups studied in the Mongolian population were significantly higher than in the Han population. Similarly, the prevalence rate of hypertension in Mongolian population was significantly higher than in the Han population18. Hypertension and stroke in the Mongolian population might be related to the genes ACEDD, CYPCT, and TT19. The proportions of herdsman and peasants were very high in this survey. The number of patients with a junior middle school education level was higher than the number of patients with other education levels. The proportion of total annual family income less than RMB 30,000 was high. The awareness and understanding of stroke and the incidence of physical examinations in the middle-aged and high-risk population were worse than in developed areas. The risk factors of hypertension, diabetes, and fat combined with low income could increase the incidence of the disease and increase the burden on low-income countries and areas20.
The number of stroke patients worldwide will increase by 90,000 each year in the next few years because of the increased number of people aged over 65 years. In addition, the prevalence rate of stroke and its different subtypes increase with age19,20. Fang XH reported21 that the standardized prevalence rates of stroke in patients aged from 55 to 59, 60 to 64, and over 65 years were 9.5%, 11.7%, and 14%, respectively. The genetic differences between sex and income had an obvious relationship with the occurrence of stroke22,23. The present study found that the prevalence of stroke in males was higher than in females, which might be related to estrogen, which was a protective factor for cerebrovascular disease. Estrogen could regulate lipid metabolism, thus inhibit intimal hyperplasia caused by platelet aggregation, stress, and mechanical damage. The prevalence rate of stroke in males aged 55 to 65 years was twice as high as in females and accelerated significantly, and in males aged over 65 years was higher than in females, which might be related to the unhealthy living habits, such as heavy smoking and alcohol consumption.
Feigin et al.24 reviewed the prevalence rates in the reports of stroke in high-income, middle-income, and low-income countries. From 1970 to 2008, the prevalence rate in high-income countries decreased by 42%. The prevalence rate, especially in people aged 75 years in middle-income and low-income countries, increased by 100%. In addition, from 2000 to 2008, the incidence rate was higher than in high-income countries for the first time. The prevalence rate of stroke in China ranged from 0.12% to 0.22%, while it was 0.28% in Inner Mongolia, which might be related to the following reasons: the investigated population aged over 45 years; the investigated areas were mainly rural and pastoral; economic and medical conditions were relatively backward. The proportion of recurrence of stroke in patients was high, which might be related to the limited knowledge about the incidence and recurrence of stroke. LAA was the most common, followed by SAO. This result was in accordance with previous reports25. The proportions of LAA and SAO were high in China, and cardiogenic cerebral embolism was very common in Western countries. The proportion of symptomatic atherosclerotic intracranial arterial stenosis in Asians was higher than in the white26. The TOAST classification could help in the prognosis, diagnosis, and prevention of ischemic stroke. In China, hypertension is closely related to LAA27. The proportions of LAA and SAO were high in this study, which indicates that key in the prevention and treatment of stroke is preventing and treating the risk factors of hypertension and diabetes. The proportion of ischemic stroke was high in both the Mongolian population and the Han population. The incidence rate of ischemic stroke increases by 8.7% every year in China28. Hu RL reported29 that the knowledge of hypertension and the adherence to a medication regime were higher in the Han population than in the Mongolian population. In this study, we found there were significant differences in risk factors in stroke between Mongolian and Han populations. Hypertension and diabetes were the common risk factors in Mongolian and Han populations. Therefore, it is important to strengthen the education about the risk factors of stroke for patients, high-risk populations, community hospital workers, and primary hospital workers.
Conclusion
The prevalence rates, incidence rates, and recurrence rates of stroke patients aged over 45 years were higher in the Mongolian population than in the Han population. The proportion of ischemic stroke was also high. Hence, we should take effective and reasonable measures according to characteristics of epidemiology in local populations.
Additional Information
How to cite this article: Zhang, C. et al. Epidemiology Investigation of stroke among Mongolian and Han population aged over 45 in Inner Mongolia. Sci. Rep. 7, 45710; doi: 10.1038/srep45710 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Krishnamurthi, R. V. et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. The Lancet. Global health 1, e259–281, doi: 10.1016/S2214-109X(13)70089-5 (2013).
Bejot, Y., Daubail, B. & Giroud, M. Epidemiology of stroke and transient ischemic attacks: Current knowledge and perspectives. Revue neurologique 172, 59–68, doi: 10.1016/j.neurol.2015.07.013 (2016).
Barker-Collo, S. et al. Sex Differences in Stroke Incidence, Prevalence, Mortality and Disability-Adjusted Life Years: Results from the Global Burden of Disease Study 2013. Neuroepidemiology 45, 203–214, doi: 10.1159/000441103 (2015).
Strong, K. & Mathers, C. 19–The Global Burden of Stroke. Neuroepidemiology 45, 143–145 (2015).
Suwanwela, N. C., Poungvarin, N. & Asian Stroke Advisory, P. Stroke burden and stroke care system in Asia. Neurology India 64 Suppl, S46–51, doi: 10.4103/0028-3886.178042 (2016).
Zhao, D. et al. Epidemiological Transition of Stroke in China. Stroke 39, 1653–1654 (2008).
Ning et al. The epidemiological transition of first-ever stroke among low-income population in China: a population-based study from 1992 to 2014. Lancet 386, S66–S66 (2015).
Wang, X. D. et al. Diagnosis of various types of cerebrovascular disease. Chinese Medical Association for NeuroscienceVol. 29, 379–380 (Chinese Journal of Neurology, 1996).
Chen, P. H. et al. Classifying Ischemic Stroke, from TOAST to CISS. CNS neuroscience & therapeutics 18, 452–456, doi: 10.1111/j.1755-5949.2011.00292.x (2012).
Stiff, P. J. et al. Transplanted CD34 + Cell Dose Is Associated with Long-Term Platelet Count Recovery following Autologous Peripheral Blood Stem Cell Transplant in Patients with Non-Hodgkin Lymphoma or Multiple Myeloma. Biology of Blood & Marrow Transplantation Journal of the American Society for Blood & Marrow Transplantation 17, 1146–1153 (2011).
Pradhan, P., Dutta, A. K., Roy, A., Basu, S. K. & Acharya, K. Macrofungal diversity and habitat specificity: a case study. Biodiversity 14, 147–161 (2013).
Li Z. S., Y. Q., Su Q. G., Chen S. M., Shu & Q., Fu YG. Epidemiology investigation of cerebrovascular disease in rural area in China. Chinese Journal of Neurosurgery 5, 7–10 (1989).
Feigin, V. L., Lawes, C. M., Bennett, D. A. & Anderson, C. S. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. The Lancet. Neurology 2, 43–53 (2003).
Qu Y., W. Z., Zhao, W. H., Yang & X. G., Kong LZ. The Prevalence and onset age of stroke in residents aged over 35. Chinese Journal of Preventive Medicine 43, 1069–1072 (2009).
Lu, J. et al. Direct economic burden of cerebrovascular disease, during 1993–2008 in China. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 35, 1263–1266 (2014).
National Collaborative Group of Blood Pressure Sampling Survey. Analysis of the prevalence of stroke and myocardial infarction and related factors. National Blood Sample Survey GroupVol. S1, 43–49 (Chinese Journal of Hypertension, 1995).
China Population Yearbook. (China Social Sciences Press, 2014).
Zhang, C. Y. et al. Prevalence, detection, management, and control of hypertension in the population of Mongolian and Han nationalities with age ≥55 years in a pastoral area of Inner Mongolia Autonomous Region. Zhonghua xin xue guan bing za zhi 40, 786–790 (2012).
Huriletemuer, H., Zhang, C., Niu, G., Zhao, S. & Hurile, H. Gene polymorphisms and related risk factors in Mongolian hypertensive stroke patients. Neurosciences 15, 184–189 (2010).
Wang, J. et al. Trends in Age of First-Ever Stroke Following Increased Incidence and Life Expectancy in a Low-Income Chinese Population. Stroke; a journal of cerebral circulation 47, 929–935, doi: 10.1161/STROKEAHA.115.012466 (2016).
Mills, K. T. et al. Global Burden of Hypertension: Analysis of Population-based Studies from 89 Countries. Journal of Hypertension 33 (2015).
Kolaković, A. et al. Gender-Specific Association between Angiotensin II Type 2 Receptor −1332 A/G Gene Polymorphism and Advanced Carotid Atherosclerosis. Journal of Stroke & Cerebrovascular Diseases the Official Journal of National Stroke Association 25, 1622–1630 (2016).
Arnao, V., Acciarresi, M., Cittadini, E. & Caso, V. Stroke incidence, prevalence and mortality in women worldwide. International journal of stroke: official journal of the International Stroke Society 11, 287–301, doi: 10.1177/1747493016632245 (2016).
Feigin, V. L. et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 383, 245–254 (2014).
Go, A. S. et al. Executive summary: heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation 131, 29–322 (2014).
Saver, J. L., Carroll, J. D., Smalling, R. & Thaler, D. Letter by Saver et al regarding article, “Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association”. Stroke; a journal of cerebral circulation 46, e85–86, doi: 10.1161/STROKEAHA.115.007311 (2015).
Lv, P. et al. Comparison of Risk Factor between Lacunar Stroke and Large Artery Atherosclerosis Stroke: A Cross-Sectional Study in China. Plos One 11 (2016).
Fan, F. F. et al. Effect of enalapril on plasma homocysteine levels in patients with essential hypertension. J Zhejiang Univ Sci B 11, 583–591 (2010).
Hu, R. L. Z. C., Zhao, S. G., Niu, G. M. & Li, H. F. Conjoint analysis of polymorphism environment and genetic interaction of ACE I/D, AGT M235T and CYP11B2 T-344C among Mongolian population. Chinese Journal of Gerontology 27, 1166–1168 (2007).
Acknowledgements
This project was supported by research grants awarded by the National Natural Science Foundation of China (No. 81260185) and the Inner Mongolia Autonomous Region Natural Science Foundation (No. 2015MS(LH)0813 & No2014MS0848).
Author information
Authors and Affiliations
Contributions
T.L. and Y.Z. performed the experiments and G.Z. analyzed the data. B.H. and J.H. contributed reagents/materials/analysis tools. Z.W. drafted the manuscript. MJ prepared the tables. C.Z. wrote the manuscript. R.H. conceived and designed the experiments and analyzed the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, C., Lan, T., Zhe, Y. et al. Epidemiology Investigation of stroke among Mongolian and Han population aged over 45 in Inner Mongolia. Sci Rep 7, 45710 (2017). https://doi.org/10.1038/srep45710
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45710
This article is cited by
-
Protocol of the Inner Mongolian Healthy Aging Study (IMAGINS): a longitudinal cohort study
BMC Public Health (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.