Abstract
We examined the predictive value of neutrophil–lymphocyte ratio (NLR) by examining their association with the baseline presence and subsequent development of brain metastases in patients with stage IV non-small cell lung cancer (NSCLC). We examined the predictive value of NLR for brain metastasis in 260 stage IV NSCLC. Logistic regression models and competing risk analysis were used to determine the association of NLR with baseline and subsequent presence of brain metastases. Multivariate analysis reveals that patients with high NLR (≥4.95) had significantly more brain metastases at diagnosis than those with low NLR (Odds Ratio = 2.59, P = 0.01). In patients who had no baseline brain metastasis, competing risks analysis revealed that patients with high NLR showed higher cumulative incidence of subsequent brain metastases, compared to those with low NLR (P = 0.017). A high NLR was associated with the baseline presence or the subsequent development of brain metastases, particularly in the group with adenocarcinoma (P = 0.013 and P = 0.044, respectively). Furthermore, an increase in NLR during treatment was associated with subsequent brain metastases (P = 0.004). The NLR is an independent predictive factor for the baseline presence of brain metastases and subsequent brain metastases in stage IV NSCLC.
Similar content being viewed by others
Introduction
Non-small-cell lung cancer (NSCLC) with brain metastasis is the most common central nervous system malignancy, accounting for as much as 20% of all brain metastasis cases1. Because of advances in cancer therapy, some cancer patients can prolong their lives, resulting in a higher probability of brain metastasis. NSCLC with brain metastasis often has a dismal prognosis with median survival ranging between 4 and 6 months2. There are currently no validated biomarkers for patients with NSCLC to predict the development of brain metastases.
Previous studies demonstrated associations between epidermal growth factor receptor (EGFR) mutation status and the development of brain metastases3,4,5, however other investigator reported negative result6. EGFR mutated adenocarcinoma comprises up to 20–50% of adenocarcinomas7. Furthermore, most patients with squamous cell carcinoma have no EGFR mutation8,9. Therefore, new biomarkers for detecting brain metastasis are needed for many EGFR wild type patients. Prophylactic cranial irradiation or chemotherapy was considered in patients with advanced NSCLC10,11,12. If we can find new biomarkers for early identification of patients at the greatest risk of brain metastasis, we can decrease mortality among NSCLC patients by more intensive brain imaging surveillance and prophylactic treatment strategies.
Neutrophil-to-lymphocyte ratio (NLR) is a useful biomarker for systemic inflammatory disease13,14. Large-scale meta-analysis revealed that NLR was associated with an adverse clinical outcome in many solid tumors15. Recent studies have found that the NLR at diagnosis is a prognostic indicator in malignant tumors including NSCLC16,17,18,19,20,21. It has been proposed that the imbalance between neutrophils and lymphocytes is secondary to tumor hypoxia or necrosis and is associated with tumor growth and metastasis22,23,24. Systemic elimination of neutrophils reduced pulmonary and lymph node metastases in a mouse model of breast cancer25.
Although the biologic behavior of NLR in NSCLC has been heavily researched18,19,26,27,28, there are no studies exploring the association of NLR and the development of brain metastases. This retrospective study evaluated the predictive value of NLR by examining its association with the baseline presence and subsequent development of brain metastases in patients with stage IV NSCLC.
Materials and Methods
Patient selection
This research was approved by the Institutional Review Board of Ajou University Hospital. Inform consent was granted a waiver due to the retrospective nature of this study. All treatments were performed in accordance with relevant guidelines and regulations. We carried out a retrospective study of 260 consecutive patients who received chemotherapy for NSCLC at the Ajou University Hospital (Suwon, Korea) between 2002 and 2011. All patients in this analysis had pathologically or radiologically confirmed stage IV NSCLC. Patients using corticosteroids at baseline was excluded. Brain computed tomography (CT) or magnetic resonance imaging (MRI) scans were used to detect brain metastases. Clinical information, including age, gender, clinical TNM stage, histologic subtype, chemotherapic regimen, smoking history and the Eastern Cooperative Oncology Group (ECOG) status were evaluated for association with the baseline presence and subsequent development of brain metastases. Anemia was defined as hemoglobin <130 g/l in men and <120 g/l in women based on the World Health Organization classification.
Neutrophil-to-lymphocyte ratio
Complete blood counts (CBC), which included total white blood cells, neutrophils and lymphocytes were obtained at the time of admission.
To evaluate the predictive value of change in NLR during treatment, we analyze a correlation of post-treatment NLR and subsequent development of brain metastases in patients with low NLR and no baseline brain metastasis. Patients with stage IV NSCLC have a terrible prognosis2. Potential patients for subsequent development of brain metastases should have sufficient observation period because quick deaths without brain metastasis precluded the observation of brain metastasis. Therefore, we excluded patients died before 12 months after treatment to reduce competing effect. Post-treatment NLR was obtained at subsequent development of brain metastases in patients with subsequent development of brain metastases. In patients without subsequent development of brain metastases, post-treatment NLR was obtained at 15 months after treatment because median month was 15 months for subsequent development of brain metastases. If patients died between 12 and 15 months after treatment, the NLR at last follow up was obtained. The NLR was calculated using the standard formula: NLR = ANC/ALC.
Statistical Analysis
Receiver operating characteristic (ROC) curve analysis was used to determine the optimal cut-off value of NLR, corresponding to maximum joint sensitivity and specificity.
Our statistical analyses consisted of three steps. In the first step, to evaluate whether NLR and clinical variables have prognostic significance for brain metastasis, we first examined their association with the presence of brain metastasis at diagnosis. Associations between factors and the presence of brain metastasis were determined using logistic regression. If the test has a p-value of 0.05 or less in univariate analysis, or if it was a clinically important variable, a multivariable logistic regression analysis was performed to adjust for potential covariate imbalances.
In the second step of analyses, competing risks analyses were conducted, where death and subsequent development of brain metastases in patients who did not have baseline brain metastasis were modeled as competing events. The numerous deaths without brain metastasis in stage IV NSCLC precluded the observation of brain metastasis. The time interval to subsequent development of brain metastases in patients who did not have baseline brain metastasis was calculated from the day of diagnosis until the day of subsequent development of brain metastases.
In the third step of analyses, we analyze a correlation of post-treatment NLR and subsequent development of brain metastases in patients with low NLR and no baseline brain metastasis.
Statistical significance of differences in survival rates was assessed using the Gray test29. The data were analyzed using the IBM SPSS/PC version 18.0 for Windows and R version 3.1.1 (http://www.R-project.org). All P values are two-sided associations and P < 0.05 was considered statistically significant.
Results
Patient characteristics
The clinical characteristics of the 260 patients included in the study are summarized in Table 1. Among 260 NSCLC patients, 94 (36%) developed brain metastases, detected either at diagnosis (n = 60, 23%) or subsequently during the course of treatment (n = 34, 13%). Patient ages ranged from 30 to 84 years (median: 59.5 years), 166 were men and 94 were women. By histologic subtyping, 194 had adenocarcinoma and 66 had non-adenocarcinoma. Two hundred and five patients received platinum-based chemotherapy as first-line treatment and 55 patients received non-platinum-based chemotherapy The median follow-up time was 11.5 months (range: 1–95 months). Median NLR was 3.29 (range: 0.67–95).
Association of NLR with brain metastasis at diagnosis
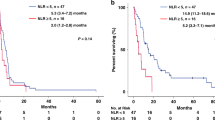
ROC curves for NLR according to brain metastasis at diagnosis were generated to determine the appropriate cut-off values. The area under the curve was recorded as 0.623 (95% confidence interval [CI]: 0.545–0.700) for NLR, with an NLR value of 4.95, corresponding to the maximum joint sensitivity and specificity on the ROC curve (50% sensitivity and 68% specificity, Fig. 1).
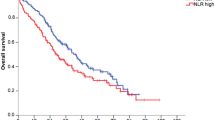
We performed univariate and multivariate analyses in order to assess the associations between NLR and brain metastasis at diagnosis. In univariate analyses, compared to patients with low NLR, patients with high NLR (≥4.95) had significantly more brain metastases at diagnosis (31.7% vs 19.1%; Odds Ratio [OR 1.96], 95% CI: 1.08–3.57, P = 0.026) (Table 2). Although other risk factors were not associated with brain metastases at diagnosis in univariate analyses, we performed multivariate analyses because most risk factors were clinically important. A multivariate analysis revealed that NLR (OR: 2.59, 95% CI: 1.25–5.38, P = 0.01) was significant independent predictor of brain metastasis at diagnosis (Table 3). When we performed univariate and multivariate analysis, using NLR as continuous variable, NLR as continuous value was also significant predictor of brain metastasis at diagnosis in univariate and multivariate analysis (P = 0.021 and P = 0.014, respectively).
To further assess the additional prognostic information regarding NLR, we performed subgroup analyses according to histologic subtype. In adenocarcinoma, patients with high NLR had significantly more brain metastases at diagnosis (OR: 3.03, 95% CI: 1.25–7.25, P = 0.013). However, in non-adenocarcinoma, NLR was not associated with brain metastases at diagnosis (P = 0.537).
Association of NLR with subsequent development of brain metastases in patients who did not have baseline brain metastasis
We then performed competing risks analyses to evaluate the association between NLR and subsequent development of brain metastases in patients. Therefore, cases with brain metastases at diagnosis were excluded in this analysis. In 200 patients without brain metastasis at diagnosis, subsequent brain metastasis was identified in 34 (17%) patients.
Patients with high NLR showed higher cumulative incidence of subsequent brain metastases, compared to those with low NLR (P = 0.017, Fig. 2A). In the group with adenocarcinoma, patients with high NLR also showed higher cumulative incidence of subsequent brain metastases, compared to those with low NLR (P = 0.044, Fig. 2B).
Next, we examined a correlation of post-treatment NLR and subsequent development of brain metastases in patients with low NLR and no baseline brain metastasis. The incidence of subsequent brain metastases was significantly higher for patients with high post-treatment NLR (≥4.95) than patients with low post-treatment NLR (<4.95)(40.6% vs 12.5%, P = 0.004) (Table 4).
Discussion
In the current study, we evaluated risk factors for predicting the baseline presence or the subsequent development of brain metastases in patients with stage IV NSCLC. A high NLR (≥4.95) was an independent predictor for the baseline presence of brain metastases. Competing risks analyses revealed that high NLR was associated with higher cumulative incidence of subsequent brain metastases, compared to those with patients with low NLR. Furthermore, a high NLR was associated with the baseline presence or the subsequent development of brain metastases, particularly in the group with adenocarcinoma. An increase in NLR during treatment was associated with subsequent brain metastases in patients who did not have baseline brain metastasis.
To our knowledge, we are the first to identify and validate the predictive value of NLR in NSCLC brain metastases using a competing risk model. The NLR is a readily available biomarker, which is easy to obtain from a CBC at diagnosis and will probably be one of the most inexpensive tests that can be used as a predictive model in cancer.
Although it remains unclear why a high NLR is associated with poor prognosis, it may be associated with increased neutrophil-dependent inflammation and reduced lymphocyte mediated tumor response30. A high NLR is detected when the absolute neutrophil count is high and the absolute lymphocyte count is low. Neutrophils can favor cancer progression or metastasis and impede the activity of lymphocytes and other immune cells, whereas the presence of tumour infiltrating lymphocytes was associated with a survival benefit31. Coffelt et al. recently reported that the depletion of neutrophils in a mouse model of breast cancer leads to a dramatic reduction in spontaneous lung metastases25. IL-17-producing γδ T cells induce neutrophil activation, which has the ability to suppress CD8+ cytotoxic T cells and directly promote metastatic spread.
Our results found that subsequent brain metastases happen more frequently in high post-treatment NLR (≥4.95) than in patients with low post-treatment NLR (<4.95). These results suggest that increase NLR was correlated with subsequent brain metastasis. Some previous studies reported the prognostic role of NLR changes. Early decline of NLR is associated with favorable outcomes in patients with metastatic renal cell carcinoma32. The posttreatment NLR change was a significant prognostic indicator for recurrence in patients with clear cell renal cell carcinoma33. The postoperative NLR change was an independent prognostic factor for hepatocellular carcinoma patient undergoing radiofrequency ablation34. Therefore, changes in NLR may help to predict a brain metastasis more accurately.
The brain is a common site of metastases for NSCLC, with 40–50% of patients developing brain metastases over the course of the disease35,36,37. Brain metastases are related with a generally poor prognosis, low quality of life and high economic burden, which varies depending on the treatment option38. Although whole-brain radiation therapy is the standard treatment for brain metastases, stereotactic radiosurgery is widely used in limited brain disease38. Prophylactic cranial irradiation showed a survival benefit and decreased incidence of brain metastasis in small cell lung cancer cases39, however there was no survival benefit in NSCLC12. Temozolomide has better blood-brain barrier permeability than other systemic chemotherapic agent and has modest activity in intracranial NSCLC40. Surprisingly, Temozolomide may have the potential to prevent the development of brain metastasis in NSCLC10,11. The NLR may help select NSCLC patients with high risk of developing brain metastases. More intensive brain imaging surveillance and prophylactic treatment strategies in this group can improve their survival and quality of life.
Our study has several limitations. First, this study had no data on EGFR mutation. Our dataset was collected between 2002 and 2011. The EGFR tyrosine kinase inhibitor was not widely used as first-line therapy during this period in Korea, therefore there were no EGFR mutational data. Some investigators found associations between EGFR mutation status and the development of brain metastases3,4,5,41. Further studies are needed to investigate the predictive role of NLR for brain metastases in NSCLC with or without EGFR mutation and the association between NLR and EGFR mutation. Second, there have been many previous studies evaluating the prognostic role of NLR in patients with NSCLC18,19,42,43. However, a well-established cutoff for NLR was not identified due to diverse study populations and various selection methods. Our identified cutoff for NLR needs to be validated in external populations. Third, our study was susceptible to bias in data selection and analysis due to retrospective design.
Using corticosteroids before measuring NLR at baseline may be a confounding factor. Small doses of corticosteroids, administered over a prolonged period of time, can induce extreme and persistent leukocytosis44. Corticosteroids also cause a granulocytosis primarily by a shift of neutrophils from the marginated pool to the circulating pool45. Previous studies described that NLR prognostic value can be used independently of prior use of corticosteroids in advanced prostate cancer and melanoma46,47. Cedrés et al. excluded patients taking chronic corticosteroids in prognostic analysis of NLR of NSCLC48. Our study also excluded patients taking corticosteroids to reduce the confounding effect.
In summary, our results suggest that a high NLR is an independent predictive factor for the baseline presence of brain metastases and subsequent brain metastases in patients who did not have baseline brain metastasis in NSCLC, particularly in the group with adenocarcinoma. The NLR can be used to identify a subgroup of adenocarcinoma patients who are at a high risk for brain metastasis, and who may benefit from aggressive chemotherapy or radiotherapy. More multicenter studies and larger sample sizes are needed to validate predictive value of NLR for subsequent brain metastases in NSCLC.
Additional Information
How to cite this article: Koh, Y. W. et al. Baseline neutrophil–lymphocyte ratio is associated with baseline and subsequent presence of brain metastases in advanced non-small-cell lung cancer. Sci. Rep. 6, 38585; doi: 10.1038/srep38585 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Barnholtz-Sloan, J. S. et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22, 2865–2872 (2004).
Mehta, M. P. et al. Survival and neurologic outcomes in a randomized trial of motexafin gadolinium and whole-brain radiation therapy in brain metastases. J Clin Oncol 21, 2529–2536, doi: 10.1200/jco.2003.12.122 (2003).
Eichler, A. F. et al. EGFR mutation status and survival after diagnosis of brain metastasis in nonsmall cell lung cancer. Neuro-oncology 12, 1193–1199, doi: 10.1093/neuonc/noq076 (2010).
Daniele, L. et al. Epidermal growth factor receptor gene in primary tumor and metastatic sites from non-small cell lung cancer. J Thorac Oncol 4, 684–688 (2009).
Sun, M. et al. HER family receptor abnormalities in lung cancer brain metastases and corresponding primary tumors. Clin Cancer Res 15, 4829–4837 (2009).
Li, B. T. et al. Serum Biomarkers Associated with Clinical Outcomes Fail to Predict Brain Metastases in Patients with Stage IV Non-Small Cell Lung Cancers. PLoS One 11 (2016).
Siegelin, M. D. & Borczuk, A. C. Epidermal growth factor receptor mutations in lung adenocarcinoma. Laboratory investigation; a journal of technical methods and pathology 94, 129–137, doi: 10.1038/labinvest.2013.147 (2014).
Chou, T. Y. et al. Mutation in the tyrosine kinase domain of epidermal growth factor receptor is a predictive and prognostic factor for gefitinib treatment in patients with non-small cell lung cancer. Clin Cancer Res 11, 3750–3757, doi: 10.1158/1078–0432.ccr-04–1981 (2005).
Shukuya, T. et al. Efficacy of gefitinib for non-adenocarcinoma non-small-cell lung cancer patients harboring epidermal growth factor receptor mutations: a pooled analysis of published reports. Cancer science 102, 1032–1037, doi: 10.1111/j.1349–7006.2011.01887.x (2011).
Adonizio, C. S. et al. Temozolomide in non-small-cell lung cancer: preliminary results of a phase II trial in previously treated patients. Clinical lung cancer 3, 254–258 (2002).
Choong, N. W. et al. Phase II trial of temozolomide and irinotecan as second-line treatment for advanced non-small cell lung cancer. J Thorac Oncol 1, 245–251 (2006).
Gore, E. M. et al. Phase III comparison of prophylactic cranial irradiation versus observation in patients with locally advanced non-small-cell lung cancer: primary analysis of radiation therapy oncology group study RTOG 0214. J Clin Oncol 29, 272–278, doi: 10.1200/jco.2010.29.1609 (2011).
Lee, S. J. et al. Usefulness of neutrophil to lymphocyte ratio in patients with chronic obstructive pulmonary disease: a prospective observational study. The Korean journal of internal medicine 31, 891–898, doi: 10.3904/kjim.2015.084 (2016).
Kucuk, A. et al. The role of neutrophil lymphocyte ratio to leverage the differential diagnosis of familial Mediterranean fever attack and acute appendicitis. The Korean journal of internal medicine 31, 386–391, doi: 10.3904/kjim.2015.039 (2016).
Templeton, A. J. et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Journal of the National Cancer Institute 106, dju124, doi: 10.1093/jnci/dju124 (2014).
Chua, W., Charles, K. A., Baracos, V. E. & Clarke, S. J. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer 104, 1288–1295 (2011).
Ohno, Y., Nakashima, J., Ohori, M., Hatano, T. & Tachibana, M. Pretreatment neutrophil-to-lymphocyte ratio as an independent predictor of recurrence in patients with nonmetastatic renal cell carcinoma. J Urol 184, 873–878 (2010).
Sarraf, K. M. et al. Neutrophil/lymphocyte ratio and its association with survival after complete resection in non-small cell lung cancer. J Thorac Cardiovasc Surg 137, 425–428 (2009).
Shimizu, K. et al. Preoperative neutrophil/lymphocyte ratio and prognostic nutritional index predict survival in patients with non-small cell lung cancer. World J Surg Oncol 13, 015–0710 (2015).
Koh, Y. W., Lee, H. J., Ahn, J. H., Lee, J. W. & Gong, G. Prognostic significance of the ratio of absolute neutrophil to lymphocyte counts for breast cancer patients with ER/PR-positivity and HER2-negativity in neoadjuvant setting. Tumour Biol 35, 9823–9830 (2014).
Gungorduk, K. et al. Prognostic Significance of Retroperitoneal Lymphadenectomy, Preoperative Neutrophil Lymphocyte Ratio and Platelet Lymphocyte Ratio in Primary Fallopian Tube Carcinoma: A Multicenter Study. Cancer research and treatment: official journal of Korean Cancer Association 47, 480–488, doi: 10.4143/crt.2014.058 (2015).
Roxburgh, C. S. & McMillan, D. C. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol 6, 149–163 (2010).
Kuang, D. M. et al. Peritumoral neutrophils link inflammatory response to disease progression by fostering angiogenesis in hepatocellular carcinoma. J Hepatol 54, 948–955 (2011).
Scapini, P. et al. CXCL1/macrophage inflammatory protein-2-induced angiogenesis in vivo is mediated by neutrophil-derived vascular endothelial growth factor-A. J Immunol 172, 5034–5040 (2004).
Coffelt, S. B. et al. IL-17-producing gammadelta T cells and neutrophils conspire to promote breast cancer metastasis. Nature 522, 345–348 (2015).
Lin, G. N. et al. Elevated neutrophil-to-lymphocyte ratio predicts poor outcome in patients with advanced non-small-cell lung cancer receiving first-line gefitinib or erlotinib treatment. Asia Pac J Clin Oncol 31, 12273 (2014).
Kacan, T. et al. Could the neutrophil to lymphocyte ratio be a poor prognostic factor for non small cell lung cancers? Asian Pac J Cancer Prev 15, 2089–2094 (2014).
Go, S. I. et al. Clinical significance of the neutrophil-lymphocyte ratio in venous thromboembolism patients with lung cancer. Lung Cancer 84, 79–85 (2014).
RJ, G. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16, 1141–1154. (1988).
Brandau, S., Dumitru, C. A. & Lang, S. Protumor and antitumor functions of neutrophil granulocytes. Semin Immunopathol 35, 163–176 (2013).
Gooden, M. J., de Bock, G. H., Leffers, N., Daemen, T. & Nijman, H. W. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer 105, 93–103 (2011).
Templeton, A. J. et al. Change in Neutrophil-to-lymphocyte Ratio in Response to Targeted Therapy for Metastatic Renal Cell Carcinoma as a Prognosticator and Biomarker of Efficacy. European urology 70, 358–364, doi: 10.1016/j.eururo.2016.02.033 (2016).
Ohno, Y. et al. Followup of neutrophil-to-lymphocyte ratio and recurrence of clear cell renal cell carcinoma. J Urol 187, 411–417, doi: 10.1016/j.juro.2011.10.026 (2012).
Dan, J. et al. Postoperative neutrophil-to-lymphocyte ratio change predicts survival of patients with small hepatocellular carcinoma undergoing radiofrequency ablation. PLoS One 8, e58184, doi: 10.1371/journal.pone.0058184 (2013).
Sorensen, J. B., Hansen, H. H., Hansen, M. & Dombernowsky, P. Brain metastases in adenocarcinoma of the lung: frequency, risk groups, and prognosis. J Clin Oncol 6, 1474–1480 (1988).
Yawn, B. P., Wollan, P. C., Schroeder, C., Gazzuola, L. & Mehta, M. Temporal and gender-related trends in brain metastases from lung and breast cancer. Minnesota medicine 86, 32–37 (2003).
Patchell, R. A. The management of brain metastases. Cancer treatment reviews 29, 533–540 (2003).
Peters, S., Bexelius, C., Munk, V. & Leighl, N. The impact of brain metastasis on quality of life, resource utilization and survival in patients with non-small-cell lung cancer. Cancer treatment reviews 45, 139–162, doi: 10.1016/j.ctrv.2016.03.009 (2016).
Slotman, B. et al. Prophylactic cranial irradiation in extensive small-cell lung cancer. The New England journal of medicine 357, 664–672, doi: 10.1056/NEJMoa071780 (2007).
Boggs, D. H. et al. Strategies to prevent brain metastasis in high-risk non-small-cell lung cancer: lessons learned from a randomized study of maintenance temozolomide versus observation. Clinical lung cancer 15, 433–440, doi: 10.1016/j.cllc.2014.06.008 (2014).
Guan, J. et al. EGFR mutations are associated with higher incidence of distant metastases and smaller tumor size in patients with non-small-cell lung cancer based on PET/CT scan. Medical oncology (Northwood, London, England) 33, 1, doi: 10.1007/s12032-015-0714-8 (2016).
Cata, J. P. et al. Preoperative anemia, blood transfusion, and neutrophil-to-lymphocyte ratio in patients with stage i non-small cell lung cancer. Cancer Cell Microenviron 3 (2016).
Dirican, N., Karakaya, Y. A., Gunes, S., Daloglu, F. T. & Dirican, A. Association of Intratumoral Tumor Infiltrating Lymphocytes and Neutrophil-to- Lymphocyte Ratio Are an Independent Prognostic Factor in Non-Small Cell Lung Cancer. Clin Respir J 30, 12417 (2015).
Shoenfeld, Y., Gurewich, Y., Gallant, L. A. & Pinkhas, J. Prednisone-induced leukocytosis. Influence of dosage, method and duration of administration on the degree of leukocytosis. The American journal of medicine 71, 773–778 (1981).
Nakagawa, M. et al. Glucocorticoid-induced granulocytosis: contribution of marrow release and demargination of intravascular granulocytes. Circulation 98, 2307–2313 (1998).
Lorente, D. et al. Baseline neutrophil-lymphocyte ratio (NLR) is associated with survival and response to treatment with second-line chemotherapy for advanced prostate cancer independent of baseline steroid use. Annals of oncology: official journal of the European Society for Medical Oncology 26, 750–755, doi: 10.1093/annonc/mdu587 (2015).
Zaragoza, J. et al. High neutrophil to lymphocyte ratio measured before starting ipilimumab treatment is associated with reduced overall survival in patients with melanoma. 174, 146–151, doi: 10.1111/bjd.14155 (2016).
Cedres, S. et al. Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clinical & translational oncology: official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico 14, 864–869, doi: 10.1007/s12094-012-0872-5 (2012).
Author information
Authors and Affiliations
Contributions
Y.W.K., J.H.C., M.S.A., Y.W.C. and H.W.L. collected the data, Y.W.K. and H.W.L. processed the data, Y.W.K. and H.W.L. designed the study and wrote the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Koh, Y., Choi, JH., Ahn, M. et al. Baseline neutrophil–lymphocyte ratio is associated with baseline and subsequent presence of brain metastases in advanced non-small-cell lung cancer. Sci Rep 6, 38585 (2016). https://doi.org/10.1038/srep38585
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep38585
This article is cited by
-
CD39 and LDHA affects the prognostic role of NLR in metastatic melanoma patients treated with immunotherapy
Journal of Translational Medicine (2023)
-
An elevated preoperative cholesterol-to-lymphocyte ratio predicts unfavourable outcomes in colorectal cancer liver metastasis patients receiving simultaneous resections: a retrospective study
BMC Surgery (2023)
-
Validation of the initial brain metastasis velocity in non-small cell lung cancer at a single cancer center
Journal of Neuro-Oncology (2023)
-
Mechanistic insights into the interplays between neutrophils and other immune cells in cancer development and progression
Cancer and Metastasis Reviews (2022)
-
Identification of a high-risk group for brain metastases in non-small cell lung cancer patients
Journal of Neuro-Oncology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.