Abstract
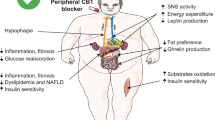
Therapeutics aimed at blocking the cannabinoid 1 (CB1) receptor for treatment of obesity resulted in significant improvements in liver function, glucose uptake and pancreatic β-cell function independent of weight loss or CB1 receptor blockade in the brain, suggesting that peripherally-acting only CB1 receptor blockers may be useful therapeutic agents. Neuropsychiatric side effects and lack of tissue specificity precluded clinical use of first-generation, centrally acting CB1 receptor blockers. In this study we specifically analyzed the potential relevance to diabetes of human CB1 receptor isoforms in extraneural tissues involved in glucose metabolism. We identified an isoform of the human CB1 receptor (CB1b) that is highly expressed in β-cells and hepatocytes but not in the brain. Importantly, CB1b shows stronger affinity for the inverse agonist JD-5037 than for rimonabant compared to CB1 full length. Most relevant to the field, CB1b is a potent regulator of adenylyl cyclase activity in peripheral metabolic tissues. CB1b blockade by JD-5037 results in stronger adenylyl cyclase activation compared to rimonabant and it is a better enhancer of insulin secretion in β-cells. We propose this isoform as a principal pharmacological target for the treatment of metabolic disorders involving glucose metabolism.
Similar content being viewed by others
Introduction
The endocannabinoid system (ECS) is a key regulator of numerous physiological processes including food intake, energy balance and glucose metabolism1, and becomes over-activated in obesity and type 2 diabetes mellitus (T2DM)2,3. T2DM is characterized by hyperglycemia due to insulin resistance and pancreatic beta (β)-cell dysfunction. The cannabinoid 1 (CB1) receptor emerged as an attractive therapeutic target for obesity-related diseases since pharmacologic inhibition of CB1 receptor by inverse agonists such as rimonabant produced potent anorectic effects in both rodents and humans4,5. However, therapeutic use in whole populations revealed that rimonabant caused adverse psychiatric and neurological side effects such as irritability, anxiety and suicidal ideation6 and was therefore suspended from human use. Nevertheless, CB1 receptors are found in both central and peripheral tissues and several studies demonstrate beneficial effects on glucose metabolism and insulin sensitivity devoid of central CB1 receptor blockade and food intake7,8,9. Consequently, there is an interest in developing compounds that target peripheral CB1 receptors.
In rodent and human pancreatic islets of Langerhans an autonomous ECS exists, which includes the cannabinoid receptors and endocannabinoids (ECs) that are synthesized in a Ca2+- and glucose-dependent manner2,10,11,12. While the orphan cannabinoid receptor GPR55 has been reported in β-cells13,14, there is no consensus on which cell types within the islet express the CB1 or CB2 receptors10,11,13,14,15,16,17,18,19,20,21. The exact role(s) of the ECS in islets is also a point of contention. While some studies have reported that CB1 receptor stimulates insulin secretion2,18,22,23, others have reported the contrary15,20,24,25. Our previous work has demonstrated that first-generation CB1 receptor blockers, such as AM251 and rimonabant, stimulated β-cell proliferation both in vitro and in vivo11,26. Recently, a novel CB1 receptor inverse agonist with low brain penetrance named JD-5037 has been characterized27,28,29. This compound was shown to protect β-cell function by reducing islet inflammation and to restore glycemic plasma levels to normal in ZDF rats30. Moreover, JD-5037 treatment led to reduced body weight and hepatic steatosis, and reversed hyperleptinemia and insulin resistance in diet-induced obese mice28,31.
Despite the renewed interest in peripheral CB1 receptors, knowledge of their fundamental regulation and molecular signaling in humans is limited. Along with full length CB1 receptor, two additional N-terminal shorter isoforms are present in humans and not in rodents. These isoforms (CB1a and CB1b) result from intra-exonal splicing of the CNR1 coding exon32,33,34. However, the pharmacological importance of these three different CB1 receptor isoforms has been subjected to debate32,34,35 and therefore their further characterization and respective actions may be of considerable interest. In the current study, we characterize the expression of the human CB1 isoforms in the brain and several peripheral tissues and determine their functional differences upon activation. CB1b is preferentially expressed in β-cells and hepatocytes, where it is a more powerful modulator of adenylyl cyclase activity than the other isoforms. We also demonstrate the therapeutic potential of the peripherally-restricted CB1 receptor blocker JD-5037 in human islets. These findings give rationale for the development of second generation selective CB1b receptor blockers aimed at regulating β-cell function and improving insulin sensitivity.
Results
Human CB1 receptor gene encodes unique isoforms which differ in potency of action
Human CNR1 gene has four exons: within exon 1 there are two intra-exonal splicing sites (1A and 1B), and in coding exon 4 there are four intra-exonal splicing sites (4A-D), all of which are unique to humans (Fig. 1A). Alternative splicing of both exons 1 and 4 results in six transcript variants (Fig. 1B,C). Translation of intact exon 4 leads to the full length CB1 receptor protein, while intra-exonal alternative splicing events produce two N-terminal altered and deleted isoforms. CB1a lacks the first 89 amino acids of the full-length sequence in the N-terminus, and the sequence is substituted with 28 amino acids due to a frame-shift. CB1b has an internal deletion of 33 amino acids between Leu-21 and Gly-55 (Fig. 1D). Under high GLP-1R expression conditions, exendin 4 (Ex4) is a powerful activator of adenylyl cyclase and intracellular cAMP accumulation36. We therefore generated stable CB1-transfected CHO-GLP-1R cell lines expressing each isoform at a comparable level (Supplementary Fig. S1). Non-transfected CHO-GLP-1R cells lack CB1 receptors and the inhibition was not observed (Fig. 1E). Treatment of CHO-GLP-1R cells expressing full length CB1 receptor with the synthetic CB1 receptor agonist ACEA (≥1 nM) resulted in a 20% reduction of cAMP accumulation (Fig. 1F). This effect was further reduced by approximately 30% and 45% in the CB1a- and CB1b-expressing cells, respectively (Fig. 1F).
Human CNR1 Gene Splice Variants.
Human CNR1 (6q15) gene structure (A) and its alternatively spliced transcript variants (B): the open bar represents the exons with exon numbers inside and horizontal lines represent the introns. Human CNR1 has splicing sites in two of its exons (A). Within exon 1 there are two splicing sites (1A and 1B) and within coding exon 4 there are four splicing sites (4A-D) indicated by arrows above the exons. Alternatively-spliced transcript variants are shown (B) and GenBank accession numbers are included in parenthesis; the corresponding protein isoforms are indicated with an arrow. CB1 receptor full length protein and N-terminal isoforms are represented by CB1, CB1a and CB1b, respectively. CB1 full length amplicons align the common deleted region in between exon 4C-4D, recognizing all full length splice variants. Each TaqMan probe recognizes the adjacent and inter-exonal spliced exons and is represented by short horizontal bars in black, grey and white for CB1, CB1a and CB1b receptors, respectively. The specific full length CB1 receptor amplicon (black bar) aligns the intra-exonal sequence between splicing sites 4B and 4C, and does not recognize the spliced variants CB1a and CB1b (C). Alignment of the protein N-terminal amino acid sequences of CB1a and CB1b with full length CB1 receptor (D). Gaps are represented by dashed lines, identical amino acids by the asterisks. The beginning of the first transmembrane domain is underlined. Increasing concentrations of ACEA did not influence on Ex4-mediated cAMP accumulation in CHO cells when the cells were not transduced with any CB1 receptor (E). Cells were pre-treated with ACEA for 20 min before addition of Ex4 for a further 15 min. **p < 0.01, n.s. = not significant compared to vehicle. Treatment with the synthetic CB1 receptor agonist ACEA attenuated Ex4-mediated cAMP accumulation in CHO-GLP-1R cells when transduced with CB1 and CB1a, and to a greater extent with CB1b (C). All values were normalized to protein concentration. Data represent mean percentage over maximum response ± SEM from at least three independent experiments. ***p ≤ 0.005 compared to CB1 full length. For cell line validation, see Supplementary Fig. S1.
N-terminal CB1 receptor isoforms are differentially expressed in human tissues
Since CB1 receptor isoforms differ in their ligand binding and downstream signaling response34,35 (Fig. 1F), we sought to characterize the expression of these isoforms in human tissues. We first designed a combination of TaqMan primers and probes; the CB1a and CB1b amplicons align the intra-exonal junctions of exons 4B-4D and exons 4A-4C, respectively (Fig. 1B). Full length CB1 amplicons align the common deleted region between 4B-4C without interfering with CB1a or CB1b (Fig. 1C). As shown in Fig. 2A, the predominant isoform in the brain is full length CB1 with low relative expression of CB1a and virtual absence of CB1b. This pattern was consistent throughout the various brain regions tested (nucleus accumbens, hippocampus and cortex; Fig. 2B). Likewise, skeletal muscle displayed the same pattern of expression (Fig. 2A). Conversely, CB1b was clearly the predominant isoform in the liver, with a 10-fold greater expression compared to full length CB1 (Fig. 2A). To confirm that expression of the CB1 isoforms in liver was due to expression in hepatocytes specifically we analyzed primary human hepatocytes and found a predominance of CB1b (Fig. 2C). Within islets, full length CB1 was present along with high expression of the CB1b isoform, where levels were similar to those found in liver (Fig. 2A). To further confirm the expression in human islets, freshly isolated islets from 15 cadaveric donors were analyzed. The pattern of expression was the same as in whole islets: CB1b and CB1a expression levels were approximately 60% and 25% that of the full length, respectively (Fig. 2D). We confirmed the presence of CB1 protein in human islets from a T2DM donor using a targeted proteomic approach (Fig. 2E). Although we could not confirm CB1b protein in human islets, due to a paucity of tissue and its lower expression compared to CB1 within islets, CB1b protein was detectable in human hepatocytes (Fig. 2F). The overall expression of CB1 receptors was significantly higher in obese donors (BMI ≥ 30) compared to leaner donors in both hepatocytes (Fig. 2G) and islets (Fig. 2H).
Relative abundance of CB1 receptor isoforms mRNA in human tissues.
Real time PCR quantification of relative expression of CB1 receptor isoforms in brain and peripheral tissues (A). CB1 receptor isoforms expression in human brain regions (B): nucleus accumbens (NAc), hippocampus and cortex. Expression is represented as fold change over CB1 expression in muscle. Data show mean ± SD (n = 3); p ≤ 0.001. Real time PCR quantification of CB1 receptor isoforms in purified human hepatocytes (C) (n = 5 separate livers) and isolated islets of Langerhans (D) (n = 15 donors). Chromatographic separations of the digested protein samples for immunoprecipitated CB1 protein isoforms from human islets (43.1 BMI; confirmed T2DM donor) (E) and primary human hepatocytes (F). Isotopically labeled synthetic versions of the corresponding proteotypic peptides were used to determine retention times (Supplementary Fig. S3). Relative expression of CB1 isoforms in hepatocytes (G) or in isolated islets (H) from donors with a BMI lower than 30 (n = 17 for hepatocytes; n = 3 for islets) or ≥ 30 (n = 5 for hepatocytes; n = 5 for islets). Data represented as fold change over CB1, with horizontal bars representing the median; **p ≤ 0.01, ***p ≤ 0.001. β-actin was used as housekeeping gene.
CB1 receptor isoforms are expressed in β-cells but not in α- or δ-cells in human islets
Islets are heterogeneous clusters consisting of five different endocrine cell types and other non-endocrine cells resulting from the natural innervation of the islet and its blood supply (Fig. 3A). To determine if the CB1 receptor isoforms were specific for β-cells, we separated β-cells from the other four endocrine cell types present within islets (namely glucagon-producing α-cells, somatostatin-producing δ-cells, pancreatic polypeptide-producing PP-cells, and ghrelin-producing ε-cells) using specific staining of disaggregated islets following cells sorting by FACS. Neither Newport Green™ DCF diacetate (NG) staining, which is based on the analysis of intracellular zinc content known to be enriched in insulin granules, nor targeting GLP-1R with FAM-Ex4, described as being specific for β-cells37,38 resulted in a pure β-cell population (Supplementary Fig. S4A–F). As an alternative approach, we utilized antibodies developed specifically for surface markers on human β-cells39. Human islets from a single cadaveric donor were dissociated and stained with HIC3-2D12 IgM and HIC1-2B4 IgG. The sorting resulted in four populations, P1, P2, P3, and non-endocrine cell population (NE) (Fig. 3B). While P1 was positive for glucagon expression and was highly enriched for α-cells (Fig. 3C), we were unable to obtain an equally enriched β-cell population by this method (Fig. 3D,E). We then further sorted these populations to obtain single cells. RNA from a single cell was equally divided into three aliquots and pre-amplified independently for each of CB1 receptor isoform-specific primers and probe set so as to avoid interference between the isoforms. The three major cell types were identified as α-, δ- and β-cells through expression of their specific hormones (Fig. 3C–E). We could not sort single PP- or ε-cells by FACS, presumably because of their low abundance in human islets. Only insulin-positive β-cells expressed the CB1 receptor, with predominant expression of CB1b, while CB1 receptor was not expressed in any other islet endocrine cell type examined (Fig. 3F).
mRNA expression of CB1 receptor isoforms in single pancreatic β-cells.
Islets of Langerhans are a complex cluster of different cell types: endocrine cells (α-, β-, δ-, ε- and PP-cells), nerve fibers and blood cells (A). Disaggregated human islets were stained with two antibodies for cell surface markers and sorted into three endocrine fractions (P1, P2 and P3) and a non-endocrine fraction (NE) (B). RNA from P1, P2 and P3 was extracted and retro-transcribed into cDNA. RT-PCR of the five endocrine hormones was performed to confirm the enrichment in each endocrine cell type (C–E). Expression was normalized to insulin in P3. Data represent mean ± SD, p < 0.001. The endocrine fractions (P1-P3) were then sorted into individual single cells. From those, RNA was extracted and reverse transcribed into cDNA, pre-amplified for the hormone transcripts of interest and diluted prior to real time PCR amplification. Expression was normalized to glucagon (F), somatostatin (G) and insulin (H). p ≤ 0.001. CB1 isoforms were quantified and represented as fold difference relative to corresponding hormone levels (I). ***p ≤ 0.005. Data are represented in box and whisker plot (n = 10). Relative amount of copies of each CB1 receptor isoform was quantified using specific Taqman primers and probes.
Activity of CB1 receptor inverse agonists is dependent upon human isoform expression
We next sought to determine if the two major isoforms present in pancreatic β-cells and hepatocytes, namely full length CB1 and CB1b, differed in their response to a global (rimonabant) versus peripherally-restricted (JD-5037) CB1 receptor inverse agonist. As a result, the binding affinity of rimonabant and JD-5037 was determined for both CB1 and CB1b receptors (Table 1). Rimonabant had a slightly stronger affinity (~3 fold) for the CB1 receptor, while JD-5037 affinity was significantly stronger (~30 fold) for the CB1b receptor (Table 1). Similar trends were observed with the functional assay, where JD-5037 inhibited CB1b receptor to a greater extent than CB1 (Supplementary Fig. S5). These data point at JD-5037 as a stronger inhibitor of the peripheral isoform CB1b than rimonabant.
We have recently published that CB1 receptors influence adenylyl cyclase activity in β-cells in response to GLP-140. In order to confirm that CB1b also regulates adenylyl cyclase activity that would lead to intracellular cAMP accumulation we utilized primary human hepatocytes, which endogenously express CB1b (Fig. 2C). Hepatocytes also express abundant glucagon receptors, which are Gs G-protein coupled receptors. Isolated primary human hepatocytes were treated with rimonabant or JD-5037 following glucagon stimulation. Blockade of the CB1b with JD-5037 significantly increased glucagon-mediated cAMP accumulation (Fig. 4A). In the presence of physiological concentrations of glucagon (1 nM), JD-5037 increased cAMP accumulation to a greater extent than rimonabant, while at low glucagon concentrations (0.1 nM) there was no significant effect. At supra-physiological concentrations of glucagon (10 nM), the cAMP amount reached a plateau and the effect of the inverse agonists was no longer evident. Similar data were obtained using primary hepatocytes from separate donors. In human islet of Langerhans, 1nM of JD-5037 significantly stimulated adenylyl cyclase activity (Fig. 4B). A concentration of up to 100 nM rimonabant was needed to obtain a significant increase on adenylyl cyclase activity (Fig. 4B).
CB1 receptor human isoforms differ in activity for cannabinoid receptor inverse agonists in metabolic systems.
Quantification of glucagon-stimulated cAMP accumulation in primary human hepatocytes (A). Hepatocytes from a human donor were pretreated with rimonabant (100 nM) or JD-5037 (100 nM) prior to glucagon stimulation. Data are the mean ± SEM from two independent experiments; *p ≤ 0.05 compared to vehicle. Quantification of cAMP accumulation in isolated human islets of Langerhans (B). Islets from one donor (20.4 BMI) were pre-cultured in 2 mM glucose for 2 hours followed by stimulation with 7.5 mM glucose in the presence or absence of increasing concentrations of rimonabant or JD-5037. Data are the mean ± SEM of 3 separated incubations; *p ≤ 0.05 compared to 7.5 mM glucose alone.
Peripherally-specific CB1 receptor blocker improves insulin secretion in human islets
In order to assess if CB1b receptor blockade would directly influence insulin secretion, we used a perifusion system. Human islets from donors with BMI higher than 30 (when possible) were used since they have higher expression levels of CB1b receptor (Fig. 2F). Islets were first subjected to non-stimulatory levels of glucose (2 mM, equivalent to 36 mg/dl) in perfusion medium for 60 min (Fig. 5). We then increased the glucose level to 7.5 mM (135 mg/dl to mimic circulating blood level of glucose in non-diabetic subjects after an oral glucose tolerance test) in order to stimulate insulin secretion and EC synthesis (Fig. 5A). Islets that were perfused with 0.1 nM of JD-5037 in addition to stimulatory levels of glucose had a far greater increase in insulin secretion than islets subjected to glucose alone, Ex4 or to the same concentration of rimonabant (Fig. 5B). Stimulation of insulin secretion by JD-5037 was dose-dependent (Fig. 5C) and it had no effect on glucagon secretion (Fig. 5D).
CB1 receptor blockade stimulates insulin secretion in isolated islets of Langerhans.
Experimental timeline for perfusion of human islets (A). Insulin secretion from human islets perfused with glucose alone (7.5 mM) (blue line) and in combination with 0.33 nM Ex4 (red line) (half maximum insulin secretion), 0.1 nM JD-5037 (green line) or 0.1 nM rimonabant (purple line) (B). Treatment time point is indicated with a black arrow. Islets were obtained from a single obese donor (34.7 BMI). Area under the curve (AUC) of insulin secretion in perfused islets from 3 independent donors (BMIs of 53.2, 32.8 and 34.7) with glucose alone or in combination with increasing concentrations of JD-5037 (C). Ex4 and rimonabant AUC are indicated with red and purple dotted lines respectively. Glucagon secretion from human islets perfused with glucose alone, glucose and Ex4 or glucose and JD-5037 (D). Data are the mean ± SEM of 3; *p ≤ 0.05 compared to vehicle.
Discussion
The present study provides evidence that the human CB1 receptor isoform, CB1b, is expressed at significant levels in pancreatic β-cells. Furthermore, it is unequivocally the main isoform in hepatocytes: this has not been previously reported. We also report that JD-5037, a CB1 receptor inverse agonist with low brain penetrance27,28 shown to improve numerous metabolic parameters in rodent models of obesity28,30,31, has preferential inverse agonistic activity for CB1b when compared to full length CB1. Moreover, CB1b influences adenylyl cyclase activity in metabolically-active tissues and its blockade enhances insulin secretion in a glucose-dependent manner.
While it is accepted that CB1 receptors are present in human islets, controversy remains as to which cells within the islet express them10,11,15,16,17,18,20,21. The use of specific primers instead of CB1 receptor antibodies, which are fraught with non-specific binding41, combined with rigorous sorting of single islet cells allowed us to obtain a definitive answer. Here we confirm at the single cell level that in human islets the expression of this receptor is specific to β-cells, corroborating previous studies that the CB1 receptor is present in β-cells11,18,21,22, and is not found in the other major endocrine cell types. Human islets express both full length CB1 receptor and the CB1b receptor isoform at comparable levels, with little expression, if any, of CB1a. Upon islet disaggregation, isolated human β-cells actually mainly express the CB1b isoform. The difference in the pattern of expression between whole islets and isolated β-cells may be explained by the presence of nerves fibers and immune cells normally found in islet structures (Fig. 3A). Indeed, macrophages in islets have been shown to express their own ECS30. Furthermore, there is a positive relationship between CB1 isoforms expression and BMI in both isolated human hepatocytes and islets, in accordance to the previous literature that shows an overactivation of the ECS in obesity2,3, making this receptor an accessible target in obesity. The long N-terminal tail of the CB1 receptor can affect receptor trafficking to the membrane and therefore its availability and consequent activity42. In fact both shorter isoforms, CB1a and CB1b, have been shown to more potently regulate synaptic transmission in isolated hippocampal neurons35. In accordance, we demonstrate that the peripheral CB1b receptor isoform exhibits stronger inhibition of adenylyl cyclase than CB1 and CB1a. Therefore, its presence in human β-cells likely modulates the intensity of cAMP/PKA down-stream signaling. We found that JD-5037 has greater affinity for CB1b than CB1, which is not the case for other inverse agonists previously tested32,34, while rimonabant has greater affinity for full length CB1.
After proving the presence of CB1b in human hepatocytes by a proteomic approach and in order to study the potency of CB1b in modulating Gs G-protein activity, we treated primary human hepatocytes with CB1 receptor inverse agonists prior to stimulation of AC. Blockade by JD-5037 significantly enhanced glucagon-stimulated cAMP accumulation, confirming that CB1b executes a strong influence on adenylyl cyclase activity. In human islets of Langerhans stimulated with glucose, JD-5037 increased intracellular cAMP beyond that achieved by glucose and comparable to Ex4. Conversely rimonabant, less potent for CB1b inhibition, was needed at higher concentration to result in the same levels of cAMP as JD-5037. These results demonstrate that blockade of CB1b receptor strongly influences Gs activity in both hepatocytes and β-cells. While the activation of AC and resultant cAMP production in β-cells is well known to enhance insulin release, the influence of the CB1 receptor activation on insulin secretion is still hotly contested2,15,18,20,22,23,24,25. The existing discrepancies may be due in part to differences in the type of agonist/inverse agonists used, their concentrations, off-target effects and islet quality. Results are also affected by the design of the experiment (i.e. perifusion vs. static insulin release: static experiments result in accumulation of end products such as hormones and ECs) as well as differences caused by the use of cell lines that lack the islet’s multicellular and potentially neural and immune environment. In this study we have used human islets from healthy donors in a dynamic system stimulated with usual postprandial levels of glucose to stimulate both insulin secretion and EC synthesis, and perfused them with nanomolar concentrations of inverse agonists in order to avoid off target effects. We show that JD-5037 potently enhances insulin secretion from isolated human islets in a concentration-dependent manner. This degree of stimulation was donor-dependent, which may be a factor in reported discrepant findings. Furthermore, rimonabant stimulated insulin secretion to a lesser extent than JD-5037 when compared across various concentrations. The inverse agonist AM251 has been shown to stimulate insulin secretion in BRIN-BD11 cells, which is only partially reversed by the GPR55 antagonist cannabidiol14, possibly owing to a combination of GPR55 and CB1 targeting29. We conclude that in isolated islets, ECs play a role in dampening insulin secretion that is circumvented by a CB1b receptor inverse agonist. CB1b is therefore a possibility for therapeutic targeting of peripheral CB1 receptors. Future studies examining the mechanisms by which tissue-specific alternative splicing occurs as well as the relationship between isoform expression and pathological states such as T2DM and fatty liver states would enable greater understanding of peripheral CB1 receptor signaling.
In summary, our findings support that peripheral blockade of the CB1 receptor may result in beneficial effects on glucose homeostasis observed previously with globally-acting inverse agonists. We establish a novel target, CB1b, which is present in both liver and β-cells of humans, for possible therapeutic development.
Methods
Reagents
Arachidonyl-2-chloroethylamide (ACEA) was purchased from Cayman Chemical (Ann Arbor, MI). Ex4 was obtained from Bachem (Torrance, CA). JD-5037 and rimonabant were kindly donated by Drs. John F. McElroy and Robert Chorvat (Jenrin Discovery, Inc., West Chester, PA).
Cell and islet culture
CHO cells and CHO-GLP-1R cells (CHO cells stably transfected with GLP-1R36) were maintained in DMEM/F-12 medium (Invitrogen, Grand Island, NY), 10% FBS, G418. CHO-GLP-1R cells were transduced with lentiviral particles for each of the CB1 isoforms35. Cells were plated on 24-well plates with regular media 24 h before transduction. Transductions were performed with 1 μl of Lentifect™ Lentivirus (Genecopoeia, Rockville, MD) and 8 μg/ml of Polybrene® (Santa Cruz, Dallas, TX) for 24 h. Selection with 10 μg/ml of Puromycin (Invitrogen) was done 72 h after. Freshly isolated islets of Langerhans from human cadaveric donors were obtained from the NIH/NIDDK-supported Integrated Islet Distribution Program (http://www.iidp.coh.org). Islet were maintained in CMRL 1066 medium (Mediatech Cellgro, Herndon, VA), 5.6 mM glucose, 10% FBS, 100 μg/ml streptomycin and 100 U/ml penicillin in non-adherent flasks overnight prior to being processed. Primary human hepatocytes were obtained from GIBCO (Grand Island, NY) and plated at a density of 0.9 × 106 cells/ml onto 24-well collagen-I coated plates in plating medium (Williams E Medium supplemented with 5% FBS, 1 μM dexamethasone, 1% penicillin/streptomycin, 4 μg/ml bovine insulin, 2 mM GlutaMAXTM and 15 mM HEPES). Following a 5 h attachment period at 37 °C with 5% CO2, cells were washed briefly and incubated in serum-free medium (Williams E Medium supplemented with 0.1 μM dexamethasone, 0.5% penicillin/streptomycin, 6.25 μg/ml human insulin, 6.25 μg/ml human transferrin, 6.25 μg/ml selenous acid, 1.25 mg/ml BSA, 5.35 μg/ml linoleic acid, 2 mM GlutaMAXTM, and 15 mM HEPES) overnight.
Assays for cAMP detection
CHO-GLP1R transduced cells were plated in complete media for 48 h. Cells were washed in PBS and pre-incubated for 2 h in serum-free media at 37 °C following pretreatment with DMSO or ACEA for 20 min before addition of 5 nM of Ex4 for a further 15 min. Primary human hepatocyte were plated and pretreated with DMSO, rimonabant or JD-5037 for 1.5 h at 37 °C before stimulation with various concentrations of glucagon (Eli Lilly and Company, Indianapolis, IN) for 5 min. Human islets of Langerhans were pre-cultured for 2 hours in 2 mM glucose insulin secretion assay buffer (130 mM NaCl, 5 mM KCl, 1 mM Na2HPO4-H2O, 1 mM MgSO4-7H2O, 2 mM CaCl2-2H2O, 20 mM HEPES, 25.5 mM NaHCO3, 0.1% BSA), following stimulation in 7.5 mM glucose insulin secretion assay buffer with DMSO (Vehicle), rimonabant or JD-5037 for 15 min in the presence of 25 μM 3-isobutyl-1 methylxanthine (Sigma-Aldrich, St Louis, USA) (non-specific phosphodiesterase inhibitor). Cells or islets were lysed in 0.1 M HCl for determination of cAMP by ELISA. cAMP was measured using the cAMP ELISA kit from Enzo Life Sciences (Farmingdale, NY) according to the manufacturer’s instructions. The data were normalized to protein concentration using a BCA protein assay (Pierce Biotechnology, Rockford, IL) or islet number, and estimated from a minimum of three independent experiments, each performed in triplicate.
Isolation of β-cells population by FACS
Islets (10,000) were picked manually, washed in DPBS (PBS 1X, 0.1% HAS, 2 mM MgCl2) and dissociated with TrypLE (Invitrogen) at 37 °C for 15 min. The reaction was stopped with cold FBS and cells were filtered through a 40 μm filter and washed in DPBS. A β-cell enriched population was sorted using cell surface markers developed by Markus Grompe39. HIC3-2D12 IgM and HIC1-2B4 IgG were added at 1:20 for 30 min on ice, washed with DPBS, and incubated for 30 min on ice with secondary antibodies 1:200 (R-Phycoerythrin conjugated Anti-Mouse IgM, Alexa Fluor® 488 conjugated Anti-Mouse IgG; Jackson ImmunoResearch). Prior to sorting, cells were washed, filtered and resuspended in fresh media. For dead cell discrimination, cells were stained with Violet LIVE/DEAD® Fixable Dead Cell Stain Kit, following the manufacturer’s instructions (Molecular Probes, Grand Island, NY). Dissociated and stained islet cells were analyzed and sorted using a FACSAria I flow cytometer/cell sorter (BD Biosciences, San Jose, CA). All sorted cells were subjected to doublet discrimination gating strategy and dead cell discrimination.
Isolation of single β-cells by FACS
Single cell sorting was performed using the automated cell deposition unit (ACDU). Analysis of flow cytometry data was performed using FCS Express software (De Novo software). Sorted cells were collected directly from FACS into 50 μl of extraction buffer from PicoPure RNA Isolation Kit (Invitrogen) and mRNA extraction was performed following manufacturer’s protocol. Whole mRNA extracts were converted to cDNA with SuperScript III (Invitrogen). Single cells cDNA samples were divided equally in three. Pre-amplification of cDNA was carried out with TaqMan PreAmp Master Mix (Applied Biosystems, Carlsbad, CA) in a 14 cycle PCR43,44. For semi-qPCR, 2 μl of a 1:3 dilution was used with TaqMan Fast Advanced Master Mix (Applied Biosystems). Samples with unequal distribution of cDNA (assessed by β-actin expression) were discarded.
Real Time PCR analysis
Human brain and peripheral tissue cDNAs were synthesized using pooled total RNA purchased from Clontech (Palo Alto, CA). Total RNAs were purified from whole islets or sorted islet cells (500–2000 cells) using Trizol Reagent (Invitrogen) and RNeasy Plus Mini Kit (Qiagen, Valencia, CA). Reverse transcription was performed with SuperScript III First-Strand Synthesis System (Invitrogen). Gene expression was assayed by qPCR with TaqMan Fast Advanced Master Mix (Applied Biosystems). Primers and FAM-labeled TaqMan probes were ordered from Applied Biosystems (the sequences of custom primers and probes are provided in Supplementary Table S1). Human VIC-labeled β-actin (ABI Cat#43263115E) was used for endogenous control of the duplex assay. Custom primers and probes were designed with Primer Express v3.0 (Applied Biosystems) and validated by CHO transduction with the CB1 isoforms. Efficiency testing was performed and was equal for all CB1 isoform primers and probes in comparison with β-actin endogenous control (Supplementary Fig. S2).
Detection of CB1 protein by Chromatographic Analysis
CB1 isoforms immunoprecipitation from CHO-CB1 cells, CHO-CB1b cells, human primary hepatocytes and human islets using Anti-CB1 Monoclonal Antibody (ImmunoGenes, Switzerland) and proteomic analysis of CB1 isoforms were carried out as described previously (Ghosh et al, unpublished material).
CB1/CB1b receptor binding and functional assay
The receptor binding assay in the column was carried out as previously described45 utilizing CHO cells stably expressing CB1 receptor isoforms. Briefly, 0.5 nM [3H]-CP55,490 (Perkin Elmer, Waltham, MA) was used as the marker ligand. A series of concentrations of the displacer ligands were added with the marker ligand: CB1: JD-5037: 0.25nM-100 nM and rimonabant 0.25 nM-10 nM; CB1b: JD-5037: 0.2–10 nM and rimonabant: 0.5–100 nM. The CB1/CB1b receptor plate-based functional assay was performed following a previously described protocol29 utilizing CHO-GLP-1R cells stably expressing CB1 receptor isoforms.
Plate based functional assay was performed in CHO cells stably expressing CB1 or CB1b were cultured in a 96-well plate in DMEM/F12, 10% FBS. After 48 h, when cells reached 100% confluence, media was changed for fresh one containing serial dilutions of the inverse agonist. Each experiment was run using a 1:4 serial dilution starting from 4 μM. Six replicates were performed on every plate for each concentration. After 1 h at 37 °C, the radioactive CB1 receptor agonist [3H]CP55,490 (Perkin Elmer, Waltham, MA) was added at a final concentration of 2 nM and incubated for 45 min at 37 °C. Supernatants were discarded and cells washed twice with PBS. Cells were lysed with NaOH (1 M). Lysates were transferred to scintillation vials containing scintillation liquid (National Diagnostics, Charlotte, GA). Data were analyzed with nonlinear regression and the log(inhibitor) vs. response (three parameters) curve using GraphPad Prism software.
Human islet perifusion
Human cadaveric islets perifusion experiments were performed using a mini-perifusion system previously described46. Islets were cultured overnight prior to use in the assay. Approximately one hundred islets were placed into insulin secretion assay buffer in polyacrylaminde P4 BioGel fine (Biorad, Hercules, CA). The islet-gel mixture was placed into the perifusion column (Biorep Technologies, Miami, FL) and connected to the perifusion system. Islets were perifused for 1 h in low glucose (2 mM) at a rate of 100 μl/min, followed by perifusion with either stimulatory glucose (7.5 mM) alone or in combination with Ex4, rimonabant or varying concentrations of JD-5037 for 25 min. During this stimulatory period, samples were collected every min. The dead volume of the perifusion system is 11 min. Insulin concentrations were determined by ELISA (Mercodia, Uppsala, Sweden) according to the manufacturer’s instructions.
Additional Information
Accession codes: GenBank Accession: KC292264.
How to cite this article: González-Mariscal, I. et al. Human CB1 Receptor Isoforms, present in Hepatocytes and β-cells, are Involved in Regulating Metabolism. Sci. Rep. 6, 33302; doi: 10.1038/srep33302 (2016).
References
Silvestri, C. & Di Marzo, V. The endocannabinoid system in energy homeostasis and the etiopathology of metabolic disorders. Cell Metab 17, 475–490 (2013).
Matias, I. et al. Regulation, function, and dysregulation of endocannabinoids in models of adipose and beta-pancreatic cells and in obesity and hyperglycemia. J. Clin. Endocrinol. Metab. 91, 3171–3180 (2006).
Sarzani, R. et al. Altered pattern of cannabinoid type 1 receptor expression in adipose tissue of dysmetabolic and overweight patients. Metabolism . 58, 361–367 (2009).
Ravinet Trillou, C. et al. Anti-obesity effect of SR141716, a CB1 receptor antagonist, in diet-induced obese mice. Am J Physiol Regul Integr Comp Physiol 284, R345–R353 (2003).
Despres, J. P., Golay, A. & Sjostrom, L. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med 353, 2121–2134 (2005).
Moreira, F. A., Grieb, M. & Lutz, B. Central side-effects of therapies based on CB1 cannabinoid receptor agonists and antagonists: focus on anxiety and depression. Best Pr. Res Clin Endocrinol Metab 23, 133–144 (2009).
Osei-Hyiaman, D. et al. Hepatic CB1 receptor is required for development of diet-induced steatosis, dyslipidemia, and insulin and leptin resistance in mice. J Clin Invest 118, 3160–3169 (2008).
Tam, J. et al. Peripheral CB1 cannabinoid receptor blockade improves cardiometabolic risk in mouse models of obesity. J Clin Invest 120, 2953–2966 (2010).
Nogueiras, R. et al. Peripheral, but not central, CB1 antagonism provides food intake-independent metabolic benefits in diet-induced obese rats. Diabetes 57, 2977–2991 (2008).
Bermúdez-Silva, F. J. et al. Presence of functional cannabinoid receptors in human endocrine pancreas. Diabetologia 51, 476–487 (2008).
Kim, W. et al. Cannabinoids inhibit insulin receptor signaling in pancreatic β-cells. Diabetes 60, 1198–1209 (2011).
Matias, I. & Di Marzo, V. Endocannabinoids and the control of energy balance. Trends Endocrinol Metab 18, 27–37 (2007).
Romero-Zerbo, S. Y. et al. A role for the putative cannabinoid receptor GPR55 in the islets of Langerhans. J. Endocrinol. 211, 177–185 (2011).
McKillop, A. M., Moran, B. M., Abdel-Wahab, Y. H. A. & Flatt, P. R. Evaluation of the insulin releasing and antihyperglycaemic activities of GPR55 lipid agonists using clonal beta-cells, isolated pancreatic islets and mice. Br. J. Pharmacol. 170, 978–990 (2013).
Nakata, M. & Yada, T. Cannabinoids inhibit insulin secretion and cytosolic Ca2+oscillation in islet beta-cells via CB1 receptors. Regul Pept 145, 49–53 (2008).
Tharp, W. G., Lee, Y.-H., Maple, R. L. & Pratley, R. E. The cannabinoid CB1 receptor is expressed in pancreatic delta-cells. Biochem. Biophys. Res. Commun. 372, 595–600 (2008).
Starowicz, K. M. et al. Endocannabinoid dysregulation in the pancreas and adipose tissue of mice fed with a high-fat diet. Obesity (Silver Spring) . 16, 553–565 (2008).
Malenczyk, K. et al. CB1 cannabinoid receptors couple to focal adhesion kinase to control insulin release. J. Biol. Chem. 288, 32685–32699 (2013).
Kargl, J. et al. The cannabinoid receptor CB1 modulates the signaling properties of the lysophosphatidylinositol receptor GPR55. J. Biol. Chem. 287, 44234–44248 (2012).
Juan-Pico, P. et al. Cannabinoid receptors regulate Ca(2+) signals and insulin secretion in pancreatic beta-cell. Cell Calcium 39, 155–162 (2006).
Bermúdez-Silva, F. J. et al. The role of the pancreatic endocannabinoid system in glucose metabolism. Best Pract. Res. Clin. Endocrinol. Metab . 23, 87–102 (2009).
Li, C., Jones, P. M. & Persaud, S. J. Cannabinoid receptors are coupled to stimulation of insulin secretion from mouse MIN6 beta-cells. Cell. Physiol. Biochem. 26, 187–196 (2010).
Vilches-Flores, A., Hauge-Evans, A. C., Jones, P. M. & Persaud, S. J. Chronic activation of cannabinoid receptors in vitro does not compromise mouse islet function. Clin. Sci. (Lond). 124, 467–478 (2013).
Li, C. et al. Cannabinoid receptor agonists and antagonists stimulate insulin secretion from isolated human islets of Langerhans. Diabetes. Obes. Metab. 13, 903–910 (2011).
Rivera, P. et al. Obesity-dependent cannabinoid modulation of proliferation in adult neurogenic regions. Eur. J. Neurosci. 33, 1577–1586 (2011).
Kim, W. et al. Cannabinoids induce pancreatic β-cell death by directly inhibiting insulin receptor activation. Sci. Signal. 5, ra23 (2012).
Chorvat, R. J., Berbaum, J., Seriacki, K. & McElroy, J. F. JD-5006 and JD-5037: Peripherally restricted (PR) cannabinoid-1 receptor blockers related to SLV-319 (Ibipinabant) as metabolic disorder therapeutics devoid of CNS liabilities. Bioorg. Med. Chem. Lett. 22, 6173–6180 (2012).
Tam, J. et al. Peripheral cannabinoid-1 receptor inverse agonism reduces obesity by reversing leptin resistance. Cell Metab . 16, 167–179 (2012).
Dossou, K. S. S. et al. Development and preliminary validation of a plate-based CB1/CB2 receptor functional assay. Anal Biochem 437, 138–143 (2013).
Jourdan, T. et al. Activation of the Nlrp3 inflammasome in infiltrating macrophages by endocannabinoids mediates beta cell loss in type 2 diabetes. Nat. Med. 19, 1132–1140 (2013).
Cinar, R. et al. Hepatic cannabinoid-1 receptors mediate diet-induced insulin resistance by increasing de novo synthesis of long-chain ceramides. Hepatology 59, 143–153 (2014).
Xiao, J. C. et al. Similar in vitro pharmacology of human cannabinoid CB1 receptor variants expressed in CHO cells. Brain Res . 1238, 36–43 (2008).
Shire, D. et al. An amino-terminal variant of the central cannabinoid receptor resulting from alternative splicing. J. Biol. Chem. 270, 3726–3731 (1995).
Ryberg, E. et al. Identification and characterisation of a novel splice variant of the human CB1 receptor. FEBS Lett. 579, 259–264 (2005).
Straiker, A., Wager-Miller, J., Hutchens, J. & Mackie, K. Differential signalling in human cannabinoid CB1 receptors and their splice variants in autaptic hippocampal neurones. Br. J. Pharmacol. 165, 2660–2671 (2012).
Montrose-Rafizadeh, C. High Potency Antagonists of the Pancreatic Glucagon-like Peptide-1 Receptor. J. Biol. Chem. 272, 21201–21206 (1997).
Doyle, M. E. & Egan, J. M. Mechanisms of action of glucagon-like peptide 1 in the pancreas. Pharmacol. Ther. 113, 546–593 (2007).
Körner, M., Christ, E., Wild, D. & Reubi, J. C. Glucagon-like peptide-1 receptor overexpression in cancer and its impact on clinical applications. Front. Endocrinol. (Lausanne). 3, 158 (2012).
Dorrell, C. et al. Isolation of major pancreatic cell types and long-term culture-initiating cells using novel human surface markers. Stem Cell Res . 1, 183–194 (2008).
González-Mariscal, I., Krzysik-Walker, S. M., Kim, W., Rouse, M. & Egan, J. M. Blockade of cannabinoid 1 receptor improves GLP-1R mediated insulin secretion in mice. Mol. Cell. Endocrinol. 423, 1–10 (2016).
Grimsey, N. L. et al. Specific detection of CB1 receptors; cannabinoid CB1 receptor antibodies are not all created equal! J. Neurosci. Methods 171, 78–86 (2008).
Andersson, H., D’Antona, A. M., Kendall, D. A., Von Heijne, G. & Chin, C.-N. Membrane assembly of the cannabinoid receptor 1: impact of a long N-terminal tail. Mol. Pharmacol. 64, 570–577 (2003).
Muller, D., Jones, P. M. & Persaud, S. J. Single-cell RT-PCR identification of genes expressed by human islet endocrine cells. Methods Mol. Biol. 560, 73–86 (2009).
Liu, Q.-R. et al. Detection of molecular alterations in methamphetamine-activated Fos-expressing neurons from a single rat dorsal striatum using fluorescence-activated cell sorting (FACS). J. Neurochem. 128, 173–185 (2014).
Moaddel, R. et al. Development and characterization of immobilized cannabinoid receptor (CB1/CB2) open tubular column for on-line screening. Anal. Biochem. 412, 85–91 (2011).
Bentsi-Barnes, K., Doyle, M. E., Abad, D., Kandeel, F. & Al-Abdullah, I. Detailed protocol for evaluation of dynamic perifusion of human islets to assess beta-cell function. Islets 3, 284–290 (2011).
Acknowledgements
Islet cell sorting was performed by Francis J. Chrest and RC (Johns Hopkins Bayview Medical Center). Human islets of Langerhans from cadaveric donors were obtained from the NIH/NIDDK-supported Integrated Islet Distribution Program (http://www.iidp.coh.org). Human hepatocytes were obtained from RW and Jessica Bonzo (Thermo Fisher Scientific). Vectors for CB1 receptor isoforms were kindly donated by Alex Straiker. We thank Drs. John McElroy and Robert Chorvat for compounds JD-5037 and rimonabant. This work was supported by the Intramural Research Program of NIA in the National Institutes of Health. MED was funded by the Juvenile Diabetes Research Foundation Grant and Sanford Project Funding (6-2013-2, 2-2010-727).
Author information
Authors and Affiliations
Contributions
I.G.-M. designed/performed experiments, analyzed data and wrote the manuscript. M.E.D. performed experiments and contributed to design/interpretation and performance of experiments. S.M.K.-W. designed experiments, interpreted data and wrote/reviewed the manuscript. Q.-R.L. contributed to design/interpretation and performance of experiments. J.F.O. analyzed data and reviewed the manuscript. R.C., R.M., S.S.-C.C., S.G., Ł.C. and O.D.C. performed experiments and analyzed data. R.P.W. provided the primary hepatocytes. J.F.O. contributed to interpretation of data and in the writing of the manuscript. J.M.E. contributed to design of experiments, interpretation of data and writing of manuscript. J.M.E. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
González-Mariscal, I., Krzysik-Walker, S., Doyle, M. et al. Human CB1 Receptor Isoforms, present in Hepatocytes and β-cells, are Involved in Regulating Metabolism. Sci Rep 6, 33302 (2016). https://doi.org/10.1038/srep33302
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep33302
This article is cited by
-
GPCRs involved in metabolic diseases: pharmacotherapeutic development updates
Acta Pharmacologica Sinica (2024)
-
Exploring the therapeutic potential of natural compounds modulating the endocannabinoid system in various diseases and disorders: review
Pharmacological Reports (2023)
-
Hepatocyte cannabinoid 1 receptor nullification alleviates toxin-induced liver damage via NF-κB signaling
Cell Death & Disease (2020)
-
Anti-obesity therapy with peripheral CB1 blockers: from promise to safe(?) practice
International Journal of Obesity (2020)
-
The cannabinoid ligands SR141716A and AM251 enhance human and mouse islet function via GPR55-independent signalling
Cellular and Molecular Life Sciences (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.