Abstract
ACLF is characterized by a systemic inflammatory response, but the cytokines involved in this process have not been well studied. The aim of this study was to characterize the systemic inflammatory response in patients with cirrhosis and ACLF and its relationship with prognosis. Fifty-five patients with cirrhosis, 26 with ACLF, were studied prospectively. Systemic inflammatory response was analyzed by measuring a large array of plasma cytokines by using a multiplex kit. A principal component analysis show noticeable differences between ACLF and decompensated cirrhosis without ACLF. Patients with ACLF had significant abnormal levels of 12 cytokines compared to those without ACLF, including: VCAM-1, VEGF-A, Fractalkine, MIP-1α, Eotaxin, IP-10, RANTES, GM-CSF, IL-1β, IL-2, ICAM-1 and MCP-1. Cytokines showing the most marked relationship with ACLF were VCAM-1 and VEGF-A (AUCROC 0.77; p = 0.001). There was a significant relationship between some of inflammatory mediators and 3-month mortality, particularly VCAM-1, ICAM-1 and GM-CSF (AUCROC>0.7; p < 0.05). Functional Enrichment Analysis showed that inflammatory markers differentially expressed in ACLF patients were enriched in leukocyte migration, particularly monocytes and macrophages and chemotaxis pathways. In conclusion, ACLF is characterized by a marked inflammatory reaction with activation of mediators of adhesion and migration of leukocytes. The intensity of the inflammatory reaction correlates with prognosis.
Similar content being viewed by others
Introduction
Liver cirrhosis is a chronic disease characterized by relentless deposition of collagen and disruption of the normal liver architecture that causes progressive portal hypertension and liver failure that eventually leads to complications and death unless liver transplantation is performed1. There is increasing evidence supporting the existence of a systemic inflammatory reaction in cirrhosis that contributes to complications and disease progression2,3. This systemic inflammatory reaction is likely initiated by translocation of bacteria or bacterial products from the intestinal lumen to the mesenteric lymph nodes and then reaching the systemic circulation. This leads to increased levels of pathogen-associated molecular patterns (PAMPs) that stimulate pattern recognition receptors (PRRs), expressed on innate immune cells. Moreover, the generation of damage-associated molecular patterns (DAMPs) from the diseased liver may also stimulate immune cells. Once stimulated, PRRs induce a transcriptional response leading to synthesis of a number of pro and anti-inflammatory cytokines, chemokines, cell adhesion molecules responsible for an adaptive immune response4,5. It has been shown that treatments that reduce bacterial translocation reduce the intensity of the immune response, while a number of complications, particularly bacterial infections are associated with an increased intensity of the immune reaction6,7. It is currently believed that such “chronic” inflammatory response may lead to a paralysis of the immune system, which in turn may be pathogenically related to the high frequency of severe infections that occur in patients with cirrhosis8,9.
There is growing interest among clinicians and researchers about acute-on-chronic liver failure (ACLF), a syndrome that occurs in patients with chronic liver diseases, particularly cirrhosis, which is characterized by development of failure of different organs and systems and high mortality rate10,11. The hypothesis has been raised that ACLF is associated with a remarkable inflammatory state that contributes to the pathogenesis and progression of this syndrome10,12. This hypothesis is based on the findings of increased leukocyte count and C-reactive protein (CRP) levels in patients with ACLF compared to those of patients with cirrhosis without ACLF and their correlation with prognosis13. Yet bacterial infections are very common as precipitating events of ACLF, it has been suggested that the inflammatory reaction in ACLF may occur in the absence of bacterial infections, at least undetectable by current standard diagnostic methods10,13. Nonetheless, despite these suggestive findings, there is very little information on the type of inflammatory mediators that are increased in ACLF and its relationship with outcomes. Moreover, the few studies published have investigated only either single or limited number of cytokines9,14; therefore neither a complete picture about the characteristics of the inflammatory reaction nor the types of pathways involved are known. Therefore, the current study was aimed at addressing the issue of the inflammatory response and its relationship with ACLF and survival in patients with cirrhosis. A large number of cytokines was measured in patients with and without ACLF using a multiplex approach. Moreover, the results were analyzed with a principal component analysis and functional enrichment analysis to gain further insight on activated inflammatory pathways. Our findings demonstrate that the syndrome of ACLF is characterized by marked inflammatory reaction with activation of mediators of adhesion and migration of leukocytes, particularly monocytes and macrophages. Moreover, the levels of some of these cytokines are associated with prognosis, a finding that links the inflammatory reaction with outcome in ACLF.
Results
Baseline characteristics of patients
The current study includes 55 patients with decompensated cirrhosis, 26 with ACLF and 29 without ACLF, admitted to the Liver Unit of the Hospital Clínic in Barcelona for the management of complications of the disease. Demographic, clinical and analytical data were collected prospectively at admission and during hospitalization. Blood samples for the measurement of cytokines were collected at the time of inclusion in the study. The characteristics of patients at time of inclusion in the study are shown in Table 1. As expected, patients with ACLF had greater frequency of ascites, hepatic encephalopathy and shock compared to that of patients with acute decompensation of cirrhosis without ACLF. Moreover, liver function tests, Child-Pugh score and model of end-stage liver disease (MELD) score, serum creatinine, serum sodium and mean arterial pressure were more markedly impaired in patients with ACLF than in those without ACLF. Of interest, neither the frequency of bacterial infections nor that of systemic inflammatory response syndrome (SIRS) was significantly different among groups. Leukocyte count and CRP levels were higher in patients with ACLF but the difference did not reach statistical significance.
Cytokine levels and relationship with ACLF
An initial exploration of the concentrations of cytokines was performed using principal component analysis (PCA) including all cytokines with and without standard laboratory variables in all cirrhotic patients as well as in healthy subjects. Figure 1A shows a three dimensional scatter plot corresponding to the first three principal components including only cytokines. A relatively good distinction between healthy subjects, patients with acute decompensation of cirrhosis without ACLF and patients with ACLF was observed. The group of healthy subjects was clearly separated from the other two groups. The group of patients with ACLF was scattered at the opposing end of healthy subjects, whereas patients with acute decompensation of cirrhosis without ACLF had a more heterogeneous distribution and some of them overlapped with patients with ACLF. A slightly better distinction between the 3 groups was observed when laboratory variables were added to cytokines in the principal component analysis (Fig. 1B).
Principal Component Analysis (PCA) of all subjects included in the study with only cytokine data (Panel A) or cytokine and biochemical data (Panel B). Confidence region (95%) was indicated by an ellipsoid for each group. Each circle corresponds to one patient. Blue circles: healthy subjects; green circles: patients with acute decompensation without ACLF; Red circles: patients with ACLF.
Table 2 shows the levels of different cytokines in patients with and without ACLF with their respective AUCROC curves. Patients with ACLF had significantly increased levels of vascular cell adhesion molecule 1 (VCAM-1), vascular endothelial growth factor A (VEGF-A), fractalkine, macrophage inflammatory protein 1-aplha (MIP-1α), eotaxin and interferon-inducible protein-10 (IP-10) compared to those of patients without ACLF. Levels of intercellular adhesion molecule 1 (ICAM-1) and monocyte chemoattractant protein-1 (MCP-1) were also higher in patients with ACLF but did not reach statistical significance. By contrast, levels of RANTES (Regulated on activation, normal T cell expressed and secreted), Granulocyte-macrophage colony-stimulating factor (GM-CSF), interleukin-1 beta (IL-1β) and interleukin 2 (IL-2) were significantly lower in patients with ACLF compared to those of patients without ACLF. There were no significant differences in the levels of the remaining cytokines.
Figure 2 shows the individual values of cytokines showing statistical significance (including the two cytokines with p values between 0.05 and 0.10) in patients with and without ACLF. A group of healthy subjects was also included for comparison. Two main messages can be derived from a close observation of this figure. First, there was overlap in the levels of most cytokines between patients with and without ACLF. Second, despite this overlap there was a clearly progressive increase (or decrease) of median cytokine levels from healthy subjects to patients without ACLF and patients with ACLF, suggesting that disease progression from decompensated cirrhosis without ACLF to ACLF is associated with significant changes in cytokine pattern. Pathway enrichment analysis using cytokines that were statistically different among groups showed that the most significant functional terms were related to migration and chemotaxis of leukocytes. Interestingly, most of the pathways were related to monocytes and macrophages (Table 3).
To assess whether the abnormal cytokine pattern found in patients with ACLF could be related to presence of bacterial infections, we next compared cytokine levels in patients with ACLF with those of the subset of patients without ACLF but with bacterial infections. The cytokines that showed statistically significant difference between the two groups of patients were the same cytokines which were significantly altered in ACLF vs no ACLF, with the only exception of VEGF-A, which showed a trend towards statistical significance (p = 0.079) (Table 4). These findings suggest that the abnormal cytokine pattern of ACLF does not appear to be related, at least for the most part, to the presence of bacterial infections.
Cytokine levels and relationship with survival
At the end of the 3-month follow-up period, 15 patients (27%) had died, 3 (5%) had been transplanted and the remaining 37 patients (67%) were still alive. Twelve of the 26 patients from the ACLF group died compared to only 3 of the 29 patients without ACLF (46% vs 10%, p < 0.001). The probability of survival of patients according to the presence or absence of ACLF is shown in Supplementary Figure 1. ACLF was the cause of death in all patients from the ACLF group, whereas the 3 patients from the no ACLF group died due to septic shock (two patients) and ACLF. The 3 patients transplanted belonged to the ACLF group.
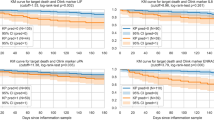
Several cytokines showed an association with 3-month mortality. The cytokines with strongest association with mortality (AUCROC >0.7) were VCAM-1, ICAM-1 and GM-CSF (Table 5 and Fig. 3). Increased levels of VCAM-1 and ICAM-1 were associated with increased mortality rate. By contrast, reduced levels of GM-CSF were associated with high mortality. In multivariate analysis including these 3 cytokines, only VCAM-1 was associated with independent prognostic value (Supplementary Table 1). The independent prognostic value of VCAM-1 was maintained even when individual variables known to have a powerful prognostic value, such as leukocyte count or bilirubin levels, were included in the multivariate analysis.
Discussion
The findings of the current study indicate that ACLF syndrome is associated with an abnormal plasma cytokine profile, characterized by alterations of cytokines mainly related to chemotaxis and migration of leukocytes, particularly monocytes and macrophages. These findings confirm the existence of a marked inflammatory reaction in the setting of ACLF. The abnormal plasma cytokine profile is already present in patients with decompensated cirrhosis but is markedly enhanced in patients with ACLF. Moreover, some of the cytokines correlated with prognosis, a finding that links the inflammatory activity with disease outcome.
The landmark CANONIC study shed light on the existence and clinical relevance of systemic inflammation in decompensated cirrhosis and ACLF syndrome. Main findings of this study were: 1/ systemic inflammation, as assessed by leukocyte count and CRP levels, seems to be an important pathogenic component of the ACLF syndrome; 2/ systemic inflammation in ACLF is independent of the existence of bacterial infections; and 3/ systemic inflammation is associated with poor short-term mortality13. There is very little information about inflammatory cytokines in ACLF. Earlier studies showed increased serum levels of interleukin 6 (IL-6) and interleukin 10 (IL-10) in patients with ACLF compared to those of patients with stable cirrhosis, in a manner similar to that reported in patients with severe sepsis8. However, this study used a definition of ACLF different from the currently accepted definition. A recently published study, which investigated the expression of MERTK in immune cells showed greater serum levels of tumor necrosis factor-alpha (TNF-α), IL-6, IL-10 and interleukin 8 (IL-8) in patients with ACLF than in those without ACLF, but normal levels of Interferon gamma (IFN-ϒ), transforming growth factor beta 1 (TGF-β1), IL-1β and interleukin 12 (IL-12)9, suggesting the existence of an altered cytokine profile in ACLF. The current study extends these observations by assessing a larger number of cytokines, using a multiplex approach, in a series of patients without ACLF and with well-defined ACLF. Our findings indicate that in decompensated cirrhosis without ACLF there is already an abnormal plasma cytokine profile compared to healthy subjects, which is further stressed in the setting of ACLF. The presence of abnormal plasma cytokine profile was suggested by using PCA approach and demonstrated by standard comparison of cytokine levels among groups (see Figs 1 and 2). An interesting observation of our study is that this abnormal plasma cytokine profile is not exclusively related to bacterial infections, because significant differences in cytokine levels persisted among groups when patients with ACLF were compared to the subset of patients with associated bacterial infections without ACLF.
A striking finding of our investigation was that most of the cytokines altered in patients with ACLF were related functionally with chemotaxis and migration of leukocytes, particularly monocytes and macrophages. This finding points towards an important role of monocytes/macrophages in the pathogenesis of ACLF. This observation is in keeping with previous studies showing impaired “sepsis-like” monocyte function in patients with ACLF. Wasmuth et al. showed that patients with ACLF have abnormal monocyte function as indicated by impaired ex-vivo production of TNF-α after stimulation with lipopolysaccharide (LPS) and reduced HLA-DR expression, suggesting the existence of a functional impairment of the innate immune response8. More recently, it has been shown that ACLF is characterized by an increased number of monocytes and macrophages that express MERTK in circulation, liver and lymph nodes, compared to patients without ACLF and healthy controls, which correlated with inflammatory response. These MERTK-positive immune cells have an impaired response to LPS stimulation and may likely contribute to ACLF progression and infectious complications9. Along the same lines, our study showed that ACLF was associated with reduced levels of GM-CSF. Moreover, reduced levels of GM-CSF correlated with mortality, further suggesting the important role of the monocyte/macrophage system in determining poor outcome in cirrhosis. GM-CSF is member of a family of hematopoietic growth factors that mobilize immune cells from bone marrow and also enhances the activity of different types of leukocytes, including neutrophils and monocytes15,16. To our knowledge, there are no data on GM-CSF levels in cirrhosis and its relationship with ACLF and outcome. Interestingly, a recent study in patients and animals with experimental acute liver failure (ALF) showed that ALF is associated with reduced levels of CSF1 (also known as macrophage colony-stimulating factor, M-CSF), a growth factor that stimulates monocytes exclusively, which predicted poor outcome17. In the same study, it was shown that administration of CSF1 to animals with ALF improved liver regeneration. These findings are in keeping with recent studies showing that the administration of granulocyte colony-stimulating factor (G-CSF) reduces bacterial infections and improves survival in patients with decompensated cirrhosis without ACLF as well as in ACLF18,19. Although these latter studies include a small number of patients and require confirmation in larger series, overall, these data point towards an important role of impaired monocytes/macrophages function in the pathogenesis of ACLF. Further studies are needed to investigate the cause of impaired monocytes/macrophages, as well as neutrophils, function and whether colony-stimulating factors could be an effective approach to therapy of ACLF.
Another interesting observation of the current study was the markedly increased levels of VCAM-1 and ICAM-1 in patients with ACLF and their relationship with survival, so that higher levels were associated with reduced survival. VCAM-1 and ICAM-1 are molecules that are expressed in the endothelial cells, particularly in post-capillary venules, but also liver sinusoidal cells, that participate in the slow rolling, arrest and adhesion, crawling, transmigration and diapedesis of leukocytes20,21. Because all these processes are essential initial steps in inflammation, these findings underscore the relevance of leukocyte chemotaxis and migration in ACLF and its relationship with prognosis. Similar findings of increased VCAM-1 and ICAM-1 levels have been observed in sepsis and correlate with prognosis in this condition22. Moreover, increased levels of ICAM-1 and VCAM-1 have been reported in patients with decompensated cirrhosis, particularly those with advanced liver failure, that correlated with prognosis23,24.
Because VCAM and ICAM are produced in endothelial cells, increased levels of these proteins have also been used as surrogate markers of endothelial dysfunction in sepsis as well as in cardiovascular diseases25,26,27. Therefore, our findings support the existence of endothelial dysfunction in ACLF.
It should be noted that despite that our study investigated a wide range of inflammatory mediators, there are still other potential interesting molecules (i.e., cytokines, chemokines) that could not be investigated as the number and type of measured molecules was limited to the multiplex kit selected. In this context, two recent studies have investigated the role of CXCL9 and CXCL11 in patients with cirrhosis receiving TIPS. Interestingly, results of these studies showed that increased levels of CXCL9 (monokine induced by human gamma interferon) and CXCL11 (Interferon-inducible T-cell alpha chemoattractant) were independent predictors of mortality in patients with cirrhosis receiving TIPS28,29. Therefore, it would be interesting to further investigate the role of these chemokines in the setting of ACLF in future studies.
The current study has some limitations that should be mentioned. First, the sample size is relatively low. However, patients included belong to two clearly differentiated clinical phenotypes of patients with and without ACLF, which makes the comparison between the two groups very accurate by avoiding clinical overlap. No patient without ACLF was in the process of rapid development of ACLF, which could have been a confounding factor. In fact, none of the patients without ACLF developed ACLF within one month after inclusion in the study. With respect to patients with ACLF, their characteristics were very similar to those of patients in the CANONIC study, with similar ACLF grades (50%, 31% and 19% of patients with grades I, II and III in the current study vs 49%, 36% and 16%, respectively, in the CANONIC study) and mortality (28-day and 90-day mortality of 27% and 46% in the current study vs 34% and 51%, respectively, in the CANONIC study). Second, plasma cytokine levels were measured exclusively at inclusion in the study; a second measurement at a later time point was not available. Therefore, assessment of changes in plasma cytokine levels according to certain outcomes, such as improvement/worsening of ACLF could not be made. However, plasma cytokines levels correlated with mortality which is the most important clinical outcome in ACLF. Finally, the use of a multiplex system allows the measurement of a large number of cytokines but is associated with some intrinsic limitations. The main limitation is that some of the cytokines included in the system could not be measured. This is probably related to cross-reading that may affect negatively the sensitivity of detection. This may explain why some cytokines that have been reported as increased in cirrhosis (i.e., TNF-α, IL-6) were not detected by the method used in the current study6,30.
In conclusion, the results of the current study show that the syndrome of ACLF is characterized by marked inflammatory reaction with activation of mediators of adhesion and migration of leukocytes, particularly monocytes and macrophages. The intensity of the inflammatory reaction correlates with prognosis.
Methods
Patient population and study design
The current study includes 55 patients with decompensated cirrhosis, 26 with ACLF and 29 without ACLF, admitted to the Liver Unit to the Hospital Clínic in Barcelona for the management of complications of the disease. These patients were selected from a prospective database with biobank collection that includes consecutive patients with decompensated cirrhosis admitted to hospital for treatment of an acute decompensation of the disease. Patients were randomly selected from the database from the groups with or without ACLF. Exclusion criteria were: previous kidney/liver transplantation, chronic haemodialysis before admission, hepatocellular carcinoma outside the Milan criteria or any other advanced malignancy and lack of inform consent. Causes of admission in patients without ACLF were: infection, ascites, gastrointestinal bleeding and hepatic encephalopathy (13, 10, 4 and 2 patients, respectively). Importantly, none of the patients without ACLF developed ACLF during at least one month after sample collection. All patients with ACLF met the criteria of ACLF at admission to hospital. Causes of admission in patients with ACLF were: acute kidney injury, infection, ascites, gastrointestinal bleeding and hepatic encephalopathy (9, 6, 4, 3 and 4 patients, respectively). A group of healthy subjects was included for comparison of plasma cytokine levels.
Demographic, clinical and analytical data were collected prospectively at admission and during hospitalization. All complications developing during hospitalization were recorded and managed according to protocols of the Liver Unit which are based on international treatment guidelines31,32. ACLF was defined according to the CANONIC study13. Patients discharged from hospital were followed-up for at least 3 months.
Blood samples were collected at the time of inclusion in the study. The median time between admission to hospital and collection of samples was 1 day (0 to 3 days). Blood was centrifuged at 2,000G, at 4 °C, for 10 minutes. Plasma was stored at −80 °C until analysis. All samples were stored at the biobank as required by spanish law. All patients signed a written informed consent document and gave permission for samples to be used in the study following current national and institutional guidelines for sample storage and usage for research purposes. All the analysis and the sample collection were performed in accordance with relevant guidelines and regulations. This study was presented and approved by the Ethics Committee of Hospital Clinic registration number 2014/0577. The creation of the biobank collection was presented and approved by the Ethics Committee registration number (2011/6689).
Multiplex cytokine assay
The following 34 cytokines and growth factors were determined with the Procarta® Immunoassay Kit (Panomics, Affymetrix Inc., Santa Clara, USA): IFN-γ, fibroblast growth factor (FGF-2), interleukin-1 receptor antagonist (IL-1RA), GM-CSF, Interleukin 4 (IL-4), IL-6, IL-8, IP-10, MIP-1α, macrophage inflammatory protein 1-beta (MIP-1β), platelet-derived growth factor subunit B (PDGF-BB), TNF-α, eotaxin, IL-1β, IL-2, interleukin 5 (IL-5), interleukin 7 (IL-7), interleukin 9 (IL-9), interleukin 12 (IL-12p70), interleukin 27 (IL-27), interleukin 21 (IL-21), interleukin 15 (IL-15), MCP-1, placental growth factor-1 (PIGF-1), VEGF-A, interleukin 23 (IL-23), interleukin 17 (IL-17A), interleukin 13 (IL-13), IL-10, fractalkine, G-CSF, RANTES, VCAM-1 and ICAM-1. Briefly, 50 μL of microparticles precoated with specific antibodies were added to each well with standards or 25 μL of plasma samples and incubated for 60 minutes at room temperature in the dark. After washing the plate, 25 μL of detection antibody solution was added and the plate was incubated for 30 minutes at room temperature in the dark. A mix with streptavidin-PE solution was added to the plate for 30 minutes and then the median relative fluorescence units from the antibody reactions was measured in 120 μL of reading buffer using a Luminex 200 analyzer (Luminex, Austin, TX, USA) and the xPONENT software (v. 3.1; Luminex, Austin, TX, USA). The concentration of each analyte was calculated using five-parameter regression models. We only considered standard points with recoveries ranging from 70 to 130%. The intra-assay coefficient of variation was less than 8%. In individual samples with values below the detection limits, the lower level of detection was used in the calculation of the results. Cytokines in which the levels were below the detection limit in more than 30% of the samples (n = 14) were excluded from the analysis (the median number of samples below detection limits in this subset was 69%). These cytokines were: FGF-2, IL-1RA, IL-4, IL-8, TNF-α, IL-5, IL-9, IL-12p70, IL-27, IL-21, IL-15, PIGF-1, IL-23 and IL-17A.
Principal component analysis
This is a technique developed for simplifying a dataset, based on orthogonal linear transformations, that converts the data to a new coordinate system such that the greatest variance by any projection of the data comes to lie on the first coordinate (first principal component), the second greatest variance on the second coordinate and so on33. By this way, it may be determined whether the variation of protein abundance represents defined patterns that correlate with the already defined sample groups. We performed PCA of the integration of multiplex cytokines abundance and other biochemical data in R platform (www.r-project.org) using “stats” and “rgl” packages. An ellipsoid from the covariance matrix was drawn to show the confidence region (95%) for each of the three plotted groups.
Statistical analysis
Categorical variables were compared with the Chi-Square test. Comparisons of parametric continuous variables between groups were made with Student’s T-test or ANOVA. Comparisons of non-parametric continuous variables between groups were made with Mann-Whitney U or Kruskal-Wallis tests. Alpha error was adjusted according to Bonferroni correction method in multiple comparisons. The area under the receiver-operating characteristic curves (AUCROC) was used to assess the relationship between each cytokine and outcomes, specifically: ACLF and 90-day transplant-free survival. Survival probability curves were calculated with the Kaplan-Meier method and compared with log-rank test. Multivariate Cox regression was performed to identify the independent factors associated with mortality. All statistical analyses were performed using SPSS 20.0 software. Results for continuous variables are expressed as median and interquartile range (IQR). Categorical variables are expressed as number and percentage. The significance level for all tests was set at 0.05 two-tailed.
Functional enrichment analysis
Functional analysis was analyzed through the use of QIAGEN’s Ingenuity Pathway Analysis (IPA®, QIAGEN Redwood City, www.qiagen.com/ingenuity). The significance value associated with the functional enrichment analysis for a given dataset is a measure of the likelihood that the association between a set of focus molecules in the experiment and a given process or pathway is not due to random chance. The p-value is calculated using the right-tailed Fisher Exact Test. We selected 1.0e−07 as the significance threshold.
Additional Information
How to cite this article: Solé, C. et al. Characterization of Inflammatory Response in Acute-on-Chronic Liver Failure and Relationship with Prognosis. Sci. Rep. 6, 32341; doi: 10.1038/srep32341 (2016).
References
Tsochatzis, E. A., Bosch, J. & Burroughs, A. K. Liver cirrhosis. Lancet 383, 1749–1761, doi:10.1016/S0140-6736(14)60121-5 (2014).
Úbeda, M. et al. Critical role of the liver in the induction of systemic inflammation in rats with preascitic cirrhosis. Hepatology 52, 2086–2095, doi:10.1002/hep.23961 (2010).
Albillos, A., Lario, M. & Álvarez-Mon, M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol 61, 1385–1396, doi:10.1016/j.jhep.2014.08.010 (2014).
Chen, G. Y. & Nuñez, G. Sterile inflammation: sensing and reacting to damage. Nat Rev Immunol 10, 826–837, doi:10.1038/nri2873 (2010).
Kumar, H., Kawau, T. & Akiras S. Pathogen recognition by the innate immune system. Int Rev Immunol 30, 16–34 (2011).
Albillos, A. et al. Tumour necrosis factor-alpha expression by activated monocytes and altered T-cell homeostasis in ascitic alcoholic cirrhosis: amelioration with norfloxacin. J Hepatol 40, 624–631 (2004).
Navasa, M. et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology 27, 1227–1232 (1998).
Wasmuth, H. E. et al. Patients with acute on chronic liver failure display “sepsis-like” immuneparalysis. J Hepatol 42, 195–201 (2005).
Bernsmeier, C. et al. Patients with acute-on-chronic liver failure have increased numbers of regulatory immune cells expressing the receptor tyrosine kinase MERTK. Gastroenterology 148, 603–615, doi:10.1053/j.gastro.2014.11.045 (2015).
Arroyo, V., Moreau, R., Jalan, R. & Ginès, P. EASL-CLIF Consortium CANONIC Study. Acute-on-chronic liver failure: A new syndrome that will re-classify cirrhosis. J Hepatol 62, S131–S143, doi:10.1016/j.jhep.2014.11.045 (2015).
Jalan, R. et al. Toward an improved definition of acute-on-chronic liver failure. Gastroenterology 147, 4–10, doi:10.1053/j.gastro.2014.05.005 (2014).
Bernal, W. et al. Acute-on-chronic liver failure. Lancet 386, 1576–1587, doi:10.1016/S0140-6736(15)00309-8 (2015).
Moreau, R. et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 144, 1437.e1421–1429, doi:10.1053/j.gastro.2013.02.042 (2013).
Metha, G., Moorkerjee, R. P., Sharma, V. & Jalan, R. Systemic inflammation is associated with increased intrahepatic resistance and mortality in alcohol-related acute-on-chronic liver failure. Liver Int 35, 724–734, doi:10.1111/liv.12559 (2015).
Shi, Y. et al. Granulocyte-macrophage colony-stimulating factor (GM-CSF) and T-cell responses: what we do and don’t know. Cell Res 16, 126–133 (2006).
Hamilton, J. A. & Anderson, G. P. GM-CSF Biology. Growth Factors 22, 225–231 (2004).
Stutchfield, B. M. et al. CSF1 Restores Innate Immunity After Liver Injury in Mice and Serum Levels Indicate Outcomes of Patients With Acute Liver Failure. Gastroenterology 149, 1896–1909, doi:10.1053/j.gastro.2015.08.053 (2015).
Kedarisetty, C. K. et al. Combination of granulocyte colony-stimulating factor and erythropoietin improves outcomes of patients with decompensated cirrhosis. Gastroenterology 148, 1362–1370, doi:10.1053/j.gastro.2015.02.054 (2015).
Garg, V. et al. Granulocyte colony-stimulating factor mobilizes CD34(+) cells and improves survival of patients with acute-on-chronic liver failure. Gastroenterology 142, 505–512, doi:10.1053/j.gastro.2011.11.027 (2012).
Vestweber, D. How leukocytes cross the vascular endothelium. Nat. Rev. Immunol 15, 692–704, doi:10.1038/nri3908 (2015).
Kolaczkowska, E. & Kubes, P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 13, 159–175, doi:10.1038/nri3399 (2013).
Schuetz, P. et al. The association of endothelial cell signaling, severity of illness and organ dysfunction in sepsis. Crit Care 14, R182, doi:10.1186/cc9290 (2010).
Girón-González, J. A. et al. Adhesion molecules as a prognostic marker of liver cirrhosis. Scand J Gastroenterol 40, 217–224 (2005).
Lo Iacono, O. et al. Serum levels of soluble vascular cell adhesion molecule are related to hyperdynamic circulation in patients with liver cirrhosis. Liver Int 28, 1129–1135 (2008).
Peters, K., Unger, R. E., Brunner, J. & Kirkpatrick, C. J. Molecular basis of endothelial dysfunction in sepsis. Cardiovasc Res 60, 49–57 (2003).
Reinhart, K., Bayer, O., Brunkhorst, F. & Meisner, M. Markers of endothelial damage in organ dysfunction and sepsis. Crit Care Med 30, S302–S312 (2002).
Blankenberg, S. et al. Circulating Cell Adhesion Molecules and Death in Patients With Coronary Artery Disease. Circulation 104, 1336–1342 (2001).
Berres, M. L. et al. CXCL9 is a prognostic marker in patients with liver cirrhosis receiving transjugular intrahepatic portosystemic shunt. J Hepatol 62, 332–339 (2015).
Berres, M. L. et al. Chemockine Chemokine (C-X-C motif) ligand 11 levels predict survival in cirrhotic patients with transjugular intrahepatic portosystemic shunt. Liver Int 36, 386–394 (2016).
Girón-Gonzalez, J. A. et al. Implication of inflammation-related cytokines in the natural history of liver cirrhosis. Liver Int 24, 437–445 (2004).
Jalan, R. et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference. J Hepatol 60, 1310–1324, doi:10.1016/j.jhep.2014.01.024 (2014).
Ginès, P. et al. European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome in cirrhosis. J Hepatol 53, 397–417, doi:10.1016/j.jhep.2010.05.004 (2010).
Ringnér, M. What is principal component analysis? Nat Biotechnol 26, 303–304, doi:10.1038/nbt0308-303 (2008).
Acknowledgements
This study was funded by a grant awarded to P.G. (PI12/00330), from Fondos de Investigación de Salud Carlos III integrated in the Plan Nacional I + D + I and co-funded by ISCIII-Subdirección General de Evaluación and European Regional Development Fund FEDER. Cristina Solé was supported by a grant from the Instituto de Salud Carlos III (PFIS fellowship: FI14/00227). Isabel Graupera was supported by a grant from the Plan Estatal I + D + I and Instituto Carlos III (Rio-Hortega fellowship: CM14/00122). Patricia Huelin was supported by a grant from the University of Barcelona (APIF2015). P.G. is a recipient of an ICREA Academia Award and AGAUR (Agencia de Gestió d’Ajuts Universitaris I de Recerca) Award (2014/SGR 708). We thank Nicki Van Berckel for the administrative support during all the process of this project. We also thank the medical and nursing staff of the liver unit for their participation and the patients who participated in the study and their families.
Author information
Authors and Affiliations
Contributions
All authors have contributed to this manuscript and approve the version of this submission. C.S. contributed to the conception and design of the study, acquisition of data, the analysis and interpretation of the data and drafting the manuscript; M.M.-R., G.F., P.H., I.G., R.M., G.d.P., X.A., E.P., N.F., S.G.K. and W.J. participated in the generation and collection of data, assembly of data, analyses of the results, interpretation of data, and/or critical revision of the manuscript for important intellectual content. P.G. and E.S. participated in the study concept, interpretation of the data, drafting the manuscript, critical revision of the manuscript for important intellectual content, obtained funding and study supervision.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Solé, C., Solà, E., Morales-Ruiz, M. et al. Characterization of Inflammatory Response in Acute-on-Chronic Liver Failure and Relationship with Prognosis. Sci Rep 6, 32341 (2016). https://doi.org/10.1038/srep32341
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep32341
This article is cited by
-
Biomarkers of hepatocellular synthesis in patients with decompensated cirrhosis
Hepatology International (2023)
-
Utility of prognostic scores in predicting short-term mortality in patients with acute-on-chronic liver failure
Egyptian Liver Journal (2022)
-
Cirrhosis-associated immune dysfunction
Nature Reviews Gastroenterology & Hepatology (2022)
-
Biomarkers of endothelial dysfunction in alcoholic hepatitis
Hepatology International (2021)
-
Prediction of Decompensation in Patients with Compensated Cirrhosis: Does Etiology Matter?
Current Hepatology Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.