Abstract
Cholesterol has been shown to regulate numerous ion channels. HCN channels represent the molecular correlate of If or Ih in sinoatrial node (SAN) and neuronal cells. Previous studies have implicated a role for cholesterol in the regulation of rabbit HCN4 channels with effects on pacing in the rabbit SAN. Using electrophysiological and biochemical approaches, we examined the effect of cholesterol modulation on human HCN1, HCN2 and HCN4 isoforms. Patch-clamp experiments uncovered isoform specific differences in the effect of cholesterol on gating kinetics upon depletion by MβCD or mevastatin or enrichment using MβCD/cholesterol. Most dramatically cholesterol had isoform specific effects on mode-shifting, which has been suggested to play a key role in stabilizing firing rate and preventing arrhythmic firing in SAN cells and neurons. Mode-shifting in HCN1 channels was insensitive to cholesterol manipulation, while HCN2 and HCN4 were strongly affected. Trafficking of each isoform to the plasma membrane was also affected by cholesterol modulation differentially between isoforms, however, each isoform remained localized in lipid raft domains after cholesterol depletion. These effects may contribute to the side effects of cholesterol reducing therapies including disrupted heart rhythm and neuropathic pain, as well as the susceptibility of sinus dysfunction in patients with elevated cholesterol.
Similar content being viewed by others
Introduction
The action potential of a sinoatrial node (SAN) cell is characterized by the presence of a progressive diastolic depolarization between −65 mV and −45 mV. Although the diastolic depolarization results from the concerted action of several currents, Ih, which was identified in the late 1970s, serves as a primary initiator. Hyperpolarization activated cyclic-nucleotide gated (HCN) channels represent the molecular correlate of the currents Ih or If in SAN and neuronal cells. The sensitivity of these channels to cyclic-nucleotides enables Ih to adjust to stimulation of the autonomic nervous system.
Four mammalian isoforms (HCN1-HCN4) exist, sharing approximately 60% sequence identity. In all mammals examined to date, HCN4 is the principle component of Ih in the SAN1,2,3,4,5. The expression of other isoforms is significantly weaker and species dependent3,4. SAN cells of HCN4 deficient mice have a 70–80% reduction in Ih6, while HCN2 channels contribute the remaining 20–30%7. Moreover, HCN4–/– deletion resulted in embryonic death in mice due to a failure to generate mature pacemaking SAN cells7,8, while HCN2 deficient mice display only mild sinus dysrhythmia at rest7. Non-pacemaking cardiomyocytes of the atria and ventricles also express HCN channels, with their function in these cells yet to be conclusively determined. However, increased Ih in ventricular myocytes has been reported in cardiac diseases such as hypertrophy, ischemic cardiomyopathy and heart failure9,10,11,12,13. Also, the addition of the HCN channel specific inhibitor ivabradine to standard therapy reduced the rates of hospital admissions and cardiovascular death in heart failure patients examined during a large clinical trial (Systolic Heart Failure Treatment with the If Inhibitor Ivabradine Trial, SHIFT)14,15. Thus, understanding the regulation of HCN channels is an important factor for understanding cardiac and neuronal function and the consequences of various therapeutic approaches.
Topologically, HCN channels are members of the pore-loop cation channel superfamily, with each subunit containing 6 transmembrane α-helices (S1–S6), a re-entrant loop between the S5 and S6 helices that forms the selectivity filter and a C-terminal cyclic-nucleotide binding domain (CNBD) attached to the S6 via an 80 amino acid C-linker. Channels are formed by homo- or hetero-tetrameric assembly of the subunits16. Electrophysiological recordings of HCN channels have characteristic properties, including activation with sigmoidal kinetics upon membrane hyperpolarization, a lack of voltage-dependent inactivation, conduction of Na+ and K+, a shift in the activation curve as a result of direct interaction with cAMP and cGMP and inhibition by millimolar concentrations of external Cs+17. The activation kinetics of the four mammalian isoforms vary by several fold and differ from one another in their response to cyclic nucleotides. cAMP shifts the voltage-dependence of activation in HCN2 and HCN4 by +15 mV, while HCN1 and HCN3 are only weakly modulated by cAMP2,18,19,20.
The activity of HCN channels have been recently shown to be regulated by membrane lipids. Voltage-dependent gating of HCN channels is allosterically regulated by phosphoinositides (particularly PIP2 but not PI), phosphatidic acid (PA) and the fatty acid arachidonic acid (AA)21,22,23,24. This regulation appears independent of the action of cAMP, since their effects are still observed in channels lacking the CNBD23,24. Cholesterol, the major sterol in all mammalian plasma membranes, has been implicated in the modulation of the function of various ion channels25. Cholesterol content in the sarcolemma of cardiac myocytes has been shown to increase when serum cholesterol levels are elevated26, increasing nearly 20% in diabetes27. A recent study has indicated that cholesterol depletion by MβCD in HEK cells and ventricular myocytes impaired rabbit HCN4 channel localization into lipid rafts and shifted V1/2 of activation to more positive potentials and increased diastolic depolarization in rabbit SAN cells28. In this study, we systematically explore the regulation of the three human cardiac HCN isoforms (HCN1, HCN2 and HCN4) by membrane cholesterol.
Materials and Methods
Cell culture
CHO-K1 cells (ATCC, Manassas, VA) were cultured at 37°C, 5% CO2 in F12K Eagle’s medium supplemented with 10% (v/v) fetal bovine serum (FBS) and 1% Penicillin/Streptomycin. Cells were transfected with 4 μg of human HCN1, HCN2 or HCN4 as well as 750 ng of eGFP using Lipofectamine 2000 (Life Technologies, Carlsbad, CA) in serum-free OptiMEM (Sigma-Aldrich, St. Louis, MO) and returned to supplemented F12K after 3-4 hrs. Transfected cells were incubated in supplemented culture media for 24–48 hours prior to the electrophysiological recordings or biochemical experiments. Cholesterol depletion was accomplished by exposing cells to 5 mM Methyl-β-cyclodextrin (MβCD) for 60 min as previously performed29,30 or by inhibition of the cholesterol synthesis pathway by culturing cells in F12K media supplemented with 10% LPDS and 30 μM mevastatin. Cholesterol enrichment was achieved by incubating cells for 30 min with 5 mM MβCD pre-saturated with cholesterol (Sigma-Aldrich). Efficacy of the treatments were quantified, using the Amplex Red cholesterol assay kit (Life Technologies) to quantify the cholesterol content in the cell membrane. After 30–60 min fluorescence from the reaction was read using an Infinite® 200 Pro plate reader (Tecan Group Ltd., Männedorf, Switzerland).
Preparation of Lipoprotein-deficient serum (LPDS)
Lipoprotein-deficient serum (LPDS) was prepared following the protocol of Renaud et al.31 with slight variation. Briefly, FBS was adjusted to a density of 1.215 g/mL by adding KBr. After overlaying the FBS with a KBr solution at the same density, the mixture was centrifuged for 65 h at 235,500 g at 4 °C. The floating lipoproteins were removed and the remaining serum was dialysed against 6 changes of 4L Phosphate-buffer saline (PBS) pH 7.4 at 4 °C.
Membrane fractioning by discontinuous sucrose gradient
24–30 h post-transfection, cells were washed thrice with PBS and scraped into Na2CO3 pH 11 and left on ice for 20 min. The solution was sonicated thrice for 20 sec bursts. By adding an equal volume of 90% sucrose/MES/NaCl-Buffer, the solution was adjusted to 45% sucrose density. Layers of 35% and 5% sucrose were then cautiously added on top of the lysate. All samples were centrifuged at 273,000 g for 16 hours at 4 °C (SW60 rotor, Beckman Instruments, Palo Alto, CA). 12 fractions of equal volumes (1 mL) were collected and their protein content quantified by Nanodrop. The content of cholesterol for each fraction was assayed by the Amplex Red Assay (Life Technologies, Carlsbad, CA) according to the manufacturer’s instructions. Notably, low-density fractions 1–3 usually contain little to no protein and therefore these samples were excluded from use during further experiments.
Cell surface biotinylation
Cells were washed thrice with ice-cold PBS and then incubated for 30 min at 4 °C with 1 mM EZ-link sulfo-N-hydroxysuccinimide (sulfo-NHS)-SS-biotin (Pierce, Rockford, IL). After rinsing the cells twice with PBS-glycine, the cells were scraped into a lysis buffer (0.1% IGEPAL, 1% SDS, 250 mM NaCl, 50 mM Tris-HCl pH 7.5 and protease inhibitor) and incubated for 30 min at 4 °C. Three 20 secs bursts of sonication ensured complete cell rupturing. After a 30 min centrifugation at 20,800 g the protein in the supernatant was determined and 800 mg of protein was incubated overnight at 4 °C with immobilized Streptavidin (Pierce). After washing the resin at least seven times with binding buffer (PBS, 0.1% IGEPAL, 0.1% SDS), the biotinylated proteins were eluted by Laemmli buffer containing 0.5 M DTT. Samples were then probed by western blot using isoform specific anti-HCN antibodies.
Western blotting and densitometric analysis
Since the expression several of candidates for internal controls, such as Na/K ATPase, have also been shown to be modulated by MβCD32, protein content in each faction was quantified in each fraction by assessing absorption at λ = 280 nm and normalizing before loading on an SDS/PAGE. Protein samples were separated by SDS-PAGE on 8% polyacrylamide gels and transferred onto a PVDF membrane (BioRad). The blots were blocked with 5% milk and probed with rabbit anti-HCN antibody (1:500, Alomone labs, Jerusalem, Isreal) followed by a horseradish-peroxidase-conjugated secondary antibody (1:10,000, Santa Cruz Biotechnology, Santa Cruz, CA). HCN and Caveolin-1 bands were visualized using a peroxidase-based chemiluminescent detection kit (Pierce, Rockford, IL) and quantitated using ImageJ software (NIH).
Electrophysiology
Whole-cell currents were recorded from CHO-K1 cells transfected with HCN1, HCN2, or HCN4 channels 24–48 hours post-transfection. Glass pipettes were pulled to a final resistance of 2–4 MΩ. The external and internal solution were symmetrical and contained (in mM): 150 KCl, 10 HEPES pH 7.3, 2 MgCl2 and 1 EGTA. All recordings were performed after 2 mins of dialyzing the internal solution following membrane rupture in order to avoid issues of current rundown. Data were collected at 22–25 °C at 10 kHz with a 1 kHz low-pass Bessel filter using a conventional Axopatch 200B Amplifier and Digidata 1440A digitizer. Capacitance and series resistance were electronically compensated. Activation was assessed by stepping to voltages between −160 mV and −40 mV (Δ + 10 mV) from a holding potential (VH) of 0 mV, followed by a step to +30 mV. Steady-state activation curves were assessed from the peak of the tail currents. Non-equilibrium experiments involved a pre-pulse to −70 mV prior to the activation steps for a duration of 100 ms, 500 ms, or 1000 ms for HCN1, HCN2 and HCN4 respectively. Deactivation was assessed by a pre-pulse to −130 mV followed by test pulses from +50 mV to −60 mV (Δ-10 mV). Hysteresis was also assessed by ramps from 0 mV to −150 mV and back at varying speeds. For every protocol, each test pulse was followed by a 17–24 s interpulse interval at VH to ensure complete channel deactivation. Data were analyzed using pClamp 10 and Origin8.0 software packages.
Results
Biophysical properties of HCN1, 2 and 4 after manipulating cellular cholesterol content
To study the effect of cholesterol content on human HCN channel activity, we first verified the effect of treatment on cholesterol content in CHO-K1 cells. Treatment with either 5 mM methyl-beta-cyclodextrin (MβCD) or 30 μM mevastatin (an HMG-CoA reductase inhibitor) had nearly equivalent effects on decreasing cholesterol content by 40–60% compared to untreated (control) cells, while treatment with MβCD pre-complexed with cholesterol (MβCD/cholesterol) increased membrane cholesterol by nearly 50% (Supp. Fig. 1).
Treatment of CHO-K1 cells expressing human HCN1 channels by MβCD resulted in reduced current density compared to untreated control cells (Fig. 1A,B). To verify that this effect was specific to the effects of membrane cholesterol and not due to unspecific effects of MβCD, we also examined the effect of 30 μM mevastatin, which blocks cholesterol synthesis. Similar to the effect of MβCD, current densities were also reduced in cells treated with mevastatin. While there was a trend towards an increase in the current density with the enrichment of cellular cholesterol by MβCD/cholesterol (P = 0.12), statistical significance could not be resolved. Both depletion and enrichment had no effect on the steady-state activation properties of HCN1 channels (Fig. 1C; Table 1). HCN1 activation currents can be described by a dual-exponential function, whose fast time component (τfast) was unchanged by modulation of membrane cholesterol (Fig. 1D), however, cholesterol depletion reduced the slow component of activation (τslow) by 2-fold (Fig. 1E). No observable effect on HCN1 deactivation kinetics could be discerned.
Regulation of HCN1 by cholesterol.
(A) Representative HCN1 current traces from cells that underwent cholesterol depletion by MβCD (red) or enrichment by MβCD/cholesterol (blue) were compared to control (black). (B) Current densities of HCN1 are reduced upon cholesterol depletion and unchanged with enrichment. (C) Steady-state activation was not affected by modification of membrane cholesterol content. (D) HCN1 channel activation can be fit by a dual-exponential function. The fast component of HCN1 channel activation was unaffected by cholesterol modification, however, (E) the slow component was slower by nearly 2-fold upon cholesterol depletion. (F) The kinetics of HCN1 deactivation were unaffected by cholesterol manipulation. (n > 6; P < 0.05).
To determine if the effect of cholesterol modulation on HCN1 channels could be generalized to other human HCN channel isoforms, we further examined the effects on the other cardiac isoforms, HCN2 and HCN4 (Figs 2 and 3). Intriguingly, we observed differential effects of cholesterol modulation on these isoforms. Similar to HCN1, both HCN2 and HCN4 channels showed a decrease in current density upon cholesterol depletion by either MβCD (Fig. 2A,B; Fig. 3A,B) or mevastatin (Supp. Fig. 1B,C). Moreover, current densities in cells expressing these isoforms enriched with cholesterol remained similar to control (Fig. 2A,B; Fig. 3A,B). HCN2 channels showed no differences in steady-state activation properties with changes in cholesterol content, however, steady-state properties of HCN4 channels were shifted approximately +10 mV by either cholesterol depletion or enrichment (Fig. 3C; Table 1). Tail currents were too small in HCN4 expressing cells treated with mevastatin to reliably enable us to determine steady-state activation properties. Intriguingly, the effects of cholesterol modulation on human HCN2 and HCN4 kinetics differed from our observations in human HCN1 channels. The activation kinetics of HCN2 and HCN4 channels were unaffected by cholesterol modulation (Figs 2D and 3D,E). However, unlike HCN1 channels, the deactivation kinetics of HCN2 and HCN4 channels were slowed by cholesterol enrichment (Figs 2E and 3F). These data suggest the effect of cholesterol on HCN channels is isoform specific.
Regulation of HCN2 by cholesterol.
(A) Representative HCN2 current traces from cells that underwent cholesterol depletion by MβCD (red) or enrichment by MβCD/cholesterol (blue) were compared to control (black). (B) Current densities of HCN2 are reduced upon cholesterol depletion and unchanged with enrichment. (C) Steady-state activation was not affected by modification of membrane cholesterol content. (D) HCN2 channel activation can be fit by a single-exponential function which was unaffected by cholesterol modification. (E) HCN2 deactivation can also be described by a single-exponential function whose rate decreased upon cholesterol enrichment and was unchanged upon depletion. (n > 10; P < 0.05).
Regulation of HCN4 by cholesterol.
(A) Representative HCN4 current traces from cells that underwent cholesterol depletion by MβCD (red) or enrichment by MβCD/cholesterol (blue) were compared to control (black). (B) Current densities of HCN4 are reduced upon cholesterol depletion and unchanged with enrichment. (C) Steady-state activation was not affected by modification of membrane cholesterol content. (D,E) HCN4 channel activation can be fit by a dual-exponential function whose 2 components were unchanged compared to control. (F) The kinetics of HCN4 deactivation can be described by mono-exponential functions which were slowed with cholesterol depletion and enrichment. (n > 8; P < 0.05).
Effect of cholesterol modulation on HCN channel distribution and trafficking.
Cholesterol is capable of self-aggregating into low density domains in which numerous channels have been shown to associate33. In some cases, disruption of these raft-like domains leads to a redistribution of channels into higher density lipid fractions and altered protein function29. Rabbit HCN4 channels have been suggested to reside in cholesterol rich domains28, while this has not been examined in human HCN channels. We determined that human HCN1, HCN2 and HCN4 channels are all expressed in low-density cholesterol rich membrane fractions, isolated by discontinuous sucrose gradient (Fig. 4A). These fractions have typically been associated with lipid rafts, which can be identified by probing for caveolin proteins34. Depletion of cholesterol by 5 mM MβCD had no effect on the distribution of channels, which all remained in raft-like fractions following treatment. Thus, the functional effects of cholesterol modulation we observed in human HCN channels cannot be attributed to a redistribution of channels in the cell membrane.
Distribution of HCN channels in CHO-K1 cell membranes.
(A) HCN1, HCN2 and HCN4 channels were all found to be distributed into low-density fractions typically associated with lipid-raft domains isolated by discontinuous sucrose gradient methods. The distribution of these channels was unchanged upon treatment with MβCD to deplete membranes of cholesterol. (n = 3). Biotinylation assays were used to assess the effect of cholesterol modulation HCN channel trafficking to the membrane (B–D). We observed isoform dependent effects of on trafficking upon cholesterol depletion by MβCD or enrichment by MβCD/cholesterol. (n = 3; P < 0.05).
Next we examined the effect of altered cholesterol content on trafficking of human HCN channels to the plasma membrane. Intriguingly, biotinylation experiments indicated that the effect of cholesterol on HCN channel trafficking is specific to the isoform examined. Expression of HCN1 channels at the plasma membrane increased when cholesterol was enriched or depleted, while HCN2 trafficking was reduced with cholesterol enrichment and unchanged by cholesterol depletion. Fewer HCN4 channels were observed at the plasma membrane upon cholesterol depletion, but increased expression compared to control was observed with cholesterol enrichment. Thus, cholesterol has isoform specific effects on HCN channel trafficking.
Cholesterol regulation of non-equilibrium behaviour in HCN channels
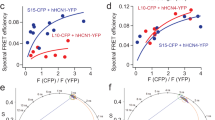
HCN channels have been shown to undergo a hysteresis in their voltage-dependence or mode-shift in which the voltage sensitivity of gating charge movement depends on the previous state35,36,37. Moreover, since voltage-hysteresis is thought to play an important role in preventing arrhythmias35,36,37, we examined the effect of cholesterol modulation on this non-equilibrium property of the cardiac HCN isoforms. Two protocols were chosen to assess hysteresis. The addition of a short −70 mV pre-pulse prior to the activation pulses and bidirectional ramps from 0 mV to −150 mV and back. As previously reported, HCN1 channels show a large depolarizing shift in their steady-state activation in response to a −70 mV pre-pulse (Fig. 5A). Pre-pulses induced an identical shift in the V1/2 of activation in cells that underwent cholesterol depletion by MβCD or mevastatin, as well as cholesterol enrichment by MβCD/cholesterol (Fig. 5A). Subtle effects on the slope were observed, suggesting co-operativity may be slightly affected. On the other hand HCN2 channels did not show a shift in steady-state activation following a −70 mV pre-pulse (Fig. 5B). However, depletion of membrane cholesterol strongly shifted V1/2 by +10 mV with mevastatin treatment and +17 mV with MβCD, while the slope constants remained unchanged. Enrichment of membrane cholesterol also shifted the voltage-dependence of activation by +10 mV. The −70 mV pre-pulse induced a +10 mV shift in steady-state activation in HCN4 channels. HCN4 channels that underwent treatments of cholesterol enrichment and depletion had V1/2’s more depolarized than control, however, −70 mV pre-pulses further shifted the V1/2 of HCN4 channels in membranes enriched with cholesterol (Fig. 5C).
Cholesterol effects on HCN channel mode-shift (hysteresis) behaviour.
(A) Steady-state activation of HCN1 channels with and without a 100 ms pre-pulse to −70 mV. The pre-pulse induced a +14 mV shift in the V1/2 of activation in HCN1 channels which was unchanged by the depletion or enrichment of membrane cholesterol. (B) Steady-state activation of HCN2 channels with and without a 250 ms pre-pulse to −70 mV. The pre-pulse induced did not shift the V1/2 of activation in HCN2 channels under control conditions, however, depletion of cholesterol induced a +10–17 mV shift in V1/2 of activation , while enrichment induced a +11 mV shift in V1/2. (C) Steady-state activation of HCN4 channels with and without a 1s pre-pulse to −70 mV. The pre-pulse induced a +10mV shift in the V1/2 of activation in HCN4 channels under control conditions, while cholesterol enrichment induced an additional +5 mV shift in V1/2. Cholesterol depletion did not have a large effect on HCN4 activation.
We further examined voltage hysteresis in HCN channels using ramp protocols of various rates between 600 mV/s and 37.5 mV/s. We quantified the degree of hysteresis by the difference in area under the curves in the forward and reverse direction. We observed that for HCN1 channels, hysteresis increased with more rapid ramp speeds and that manipulation of cholesterol levels in the membrane had no effect on the amount of hysteresis (Fig. 6A). On the other hand, HCN2 channels showed increased hysteresis as ramp speeds slowed. Cholesterol enrichment had no statistically significant consequences on the amount of hysteresis we observed for HCN2 channels, however, cholesterol depletion by MβCD and particularly mevastatin resulted in a drastic increase in the amount of hysteresis HCN2 channels underwent (Fig. 6B). This was particularly evident at 600 mV/s ramps in which in control membranes the current from 0 mV to −150 mV overlapped with the trace from −150 mV to 0 mV, while a large separation could be observed in all traces of cholesterol depleted cells expressing HCN2. Lastly, hysteresis was observed for HCN4 channels, however, the degree was unaffected by changes in ramp speeds. Moreover, hysteresis in HCN4 channels were unaffected by modulation of cholesterol levels (Fig. 6C). Taken together, these data indicate that cholesterol modifies hysteresis properties in HCN channels in an isoform specific manner.
Cholesterol effects on HCN channel mode-shift (hysteresis) behaviour examined by ramps.
Ramps were run from VH = 0 to −150 mV and back to 0 mV at varying rates. The degree of hysteresis was quantified by the area between the forward and backward current traces. (A) HCN1 channels showed increasing hysteresis with faster ramp speeds, but cholesterol modulation had no effect on this behaviour. (B) Hysteresis could only be observed in HCN2 channels as ramp speeds slowed. However, upon membrane depletion, hysteresis could be readily observed at fast ramp speeds (eg. 600 mV/s). Cholesterol enrichment had no significant effect on hysteresis compared to HCN2 control. (C) Hysteresis was uniformly observed in HCN4 channels at all ramp speeds, with no observable effects from cholesterol enrichment or depletion with MβCD. Currents were too small to assess ramps at 300 mV/s for cells depleted of cholesterol by 30 μM Mevastatin. (n > 4 for all conditions; *P < 0.05).
Discussion
In the conduction system of the heart, HCN4 channels are the predominant isoform expressed, accounting for nearly 80% of Ih. The isoform which contributes most to the remaining current is species dependent, with HCN1 dominant in rabbit4 and HCN2 dominant in mouse7. In non-conduction tissue, HCN2 appears to be the dominant isoform with ubiquitous distribution in atrial and ventricular myocytes at low levels compared to the conduction system. Since cholesterol regulates a variety of ion channels important for cardiac function29,38,39,40,41, including rabbit HCN4 in which cholesterol depletion had previously been shown to modulate voltage dependence of activation and the kinetics of deactivation28, we systematically examined the role of cholesterol in regulating the 3 human cardiac isoforms of HCN channels. Intriguingly, we observed isoform specific differences in the regulation of these channels. While cholesterol depletion or enrichment had no effect on the voltage-dependence of human HCN1 and HCN2 activation, we observed a +10 mV shift to more depolarized potentials in human HCN4 channels. In HCN1 channels, cholesterol depletion slowed the slow-component of activation (τslow), but did not alter the deactivation kinetics. Cholesterol modulation did not affect the activation kinetics of HCN2 and HCN4 channels, but cholesterol enrichment slowed the rate of deactivation in these isoforms. The effect of cholesterol modulation on channel trafficking was striking (Fig. 4B). While HCN1 channel expression increased with cholesterol depletion, the slower activation kinetics and unchanged deactivation kinetics explain the unchanged current density compared to control (Fig. 1). In HCN2 channels, cholesterol enrichment caused a reduction in surface expression, however, channels at the surface deactivated more slowly, which likely recovers the current density to control levels (Fig. 2). Cholesterol depletion did not change the expression of channels at the surface, but decreased the current density despite no changes in kinetics. It is possible that cholesterol depletion in HCN2 channels causes a reduction in the unitary conductance, or generates a subpopulation of channels that are “silenced” (ie. Popen = 0), similarly to what is expected to occur in Kir2 channels upon cholesterol enrichment29,42. This could arise from altered sensitivity to tonic levels in cAMP, or sensitivities to changes in the physiochemical properties of membranes with decreased cholesterol43. However, it is not immediately clear why slowed deactivation and increased expression of HCN4 channels upon cholesterol enrichment does not lead to increased current densities at steady-state.
Also striking was the isoform specific effect on hysteretic behaviour in HCN channels. By including a short −70 mV pre-pulse prior to activation, the voltage-dependence of HCN1 channel activation is more depolarized by +14 mV. Cholesterol depletion or enrichment had no effect on HCN1 hysteresis (Fig. 5), which was corroborated by ramp protocols (Fig. 6). On the other hand, HCN2 channels showed no hysteresis in untreated cells, however, cholesterol depletion shifted the voltage-dependence of activation following the pre-pulse by +10–17 mV. Cholesterol enrichment also affected hysteresis in HCN2 channels with a small depolarizing shift observed (Fig. 6). Again these results were corroborated by examining hysteresis using ramp protocols in which we observed increased sensitivity to hysteresis upon cholesterol depeletion (Fig. 6). In HCN4 channels, a pre-pulse induced at +10 mV depolarizing shift in the voltage-dependence of activation, which was furthered an additional +5 mV with cholesterol enrichment (Table 1). Cholesterol regulation appears to differentially regulate the sensitivity or propensity for hysteresis or mode-shifting to occur in each isoform. In HCN1 channels, which readily undergo mode-shifting, the manipulation of cholesterol levels does not affect hysteresis. Cholesterol appears to make it easier for HCN4 channels to undergo mode-shifting, while mode-shifting appears more readily in HCN2 channels upon cholesterol depletion. Thus, it is evident that cholesterol regulates each isoform of human HCN channels uniquely.
Mode-shifting or hysteresis in HCN channels has been suggested to play a key role in stabilizing firing rate and preventing arrhythmic firing in SAN cells and thalamic neurons35,36,37. Conceptually, during the hyperpolarization phase of the action potential, HCN channels do not open until very negative potentials are reached. This would prevent HCN channels from interfering with the recovery from inactivation of Nav and Cav channels. On the other hand, during the interval between action potentials, HCN channels would remain open, depolarizing the membrane potential towards threshold36. Since hysteresis is also rate dependent, it seems as though mode-shifting in HCN channels provides additional protection against bradycardia or tachycardia. As the heart rate slows, hysteresis in HCN2 and HCN4 channels would increase, leading to more HCN current, faster depolarization and thus faster heart rate. With this in consideration, we would anticipate that excessive depletion of membrane cholesterol should increase heart rate and could trigger tachycardia. This is in line with MβCD-treated SAN cells which showed a 58% faster spontaneous rhythm28. Our results may in part explain why up to 1% of patients who take statins to lower cholesterol are susceptible to tachycardia. Additionally, these changes in HCN function upon cholesterol depletion may contribute to the neuropathic pain44 reported in approximately 9% of patients being treated with statins45. Alternatively, elevated amounts of blood cholesterol have also been implicated in increasing heart rate in obese patients46. The enhanced activity we observed for HCN2 and HCN4 channels following cholesterol enrichment could also contribute to the increased heart rate in these patients.
Cholesterol can regulate ion channels and membrane proteins by numerous mechanisms. Direct protein-sterol interactions have been reported in several ion channels, GPCRs and transport proteins29,40,42,47,48,49,50,51,52,53,54. These classes of proteins can also be affected by the physiochemical properties of the membrane (such as thickness, fluidity, phase, lateral pressure, etc.). Cholesterol has been shown to increase membrane thickness and decreases permeability of the bilayer43,55. Cholesterol also facilitates phase separation of lipids such as sphingolipids that contribute to the formation of lipid rafts. Consequentially, cholesterol can affect the co-localization and recruitment of other proteins or signaling pathways that regulate a specific protein of interest56. It has been suggested that cholesterol depletion can affect rabbit HCN4 channels in HEK293 and rabbit SAN cells by disorganizing caveolae, disrupting their interaction with caveolin-1 and caveolin-3 proteins, redistributing channels into non-raft domains and reducing overall channel expression28,57. Interestingly, ß1-adrenergic receptors also present in the SA node do not redistribute from cholesterol rich low-density fractions into higher density fractions following cyclodextran treatment58. In our hands, cholesterol depletion reduced the expression of HCN4 at the channel membrane (Fig. 4B) and disrupts the expression of endogenous caveolin-1 in CHO-K1 cells, however, this did not lead to a redistribution of channels into non-raft domains (Fig. 4A). While it is tempting to attribute these differences to the cell type, as HEK and SAN cells contain both caveolin-1 and caveolin-3, while CHO-K1 cells only contain caveolin-1 proteins, a more likely explanation lies in the treatments applied. In their studies, cells were treated with 1–2% MβCD for 1–2 hours, which can remove upwards of 80–90% of membrane cholesterol59,60, disrupt caveolae59,60 and may also extract significant amounts of sphingomyelin and glycosphingolipids61,62,63,64. Here we applied a milder 5 mM MβCD treatment to cells for 60 mins, which reduced the cholesterol content in lipid raft fractions by approximately 50% (Supplemental Figure 2), maintained the integrity of caveolae based on the distribution of caveolin-1 (Figure 4) and likely minimizes the removal of lipids other than cholesterol. However, despite the same effect on caveolin-1, the expression of HCN1 channels increased with cholesterol depletion and enrichment, while the expression of HCN2 channels remained the same with cholesterol depletion and declined with enrichment. Moreover, the effects of cholesterol depletion or enrichment on gating kinetics were also isoform specific. Thus, the underlying mechanism for cholesterol regulation of HCN channels does not appear to be directly conserved among isoforms. While experiments in rabbit SAN cells suggest that cholesterol depletion by MβCD did not affect HCN4 channels by increasing basal cyclic nucleotide levels, it is yet to be determined if cholesterol alters the sensitivity to cAMP in some isoforms but not others. Our data were collected in the absence of cAMP in the pipette solution, which should enable significant rundown of cAMP levels. Thus our data is indicative of what happens in these HCN isoforms at low levels of cAMP. It also remains to be seen whether cholesterol regulation of HCN channels results from direct protein-sterol interactions, as it does in Kir channels, β-Adrenergic receptors, from changes to the properties of the bilayer, or through some intermediary protein(s).
Conclusion
We are slowly gaining an appreciation for the regulation of ion channels and membrane proteins by the lipids in which they are embedded. We have demonstrated that cholesterol regulates the expression and function of the 3 main cardiac isoforms of HCN channels, HCN1, HCN2 and HCN4. Intriguingly, this regulation appears to be isoform specific. Further studies will be needed to address the molecular details and physiological consequences of cholesterol regulation in this family of channels.
Additional Information
How to cite this article: Fürst, O. and D’Avanzo, N. Isoform dependent regulation of human HCN channels by cholesterol. Sci. Rep. 5, 14270; doi: 10.1038/srep14270 (2015).
References
Brioschi, C. et al. Distribution of the pacemaker HCN4 channel mRNA and protein in the rabbit sinoatrial node. J Mol Cell Cardiol 47, 221–7 (2009).
Ishii, T. M., Takano, M., Xie, L. H., Noma, A. & Ohmori, H. Molecular characterization of the hyperpolarization-activated cation channel in rabbit heart sinoatrial node. J Biol Chem 274, 12835–9 (1999).
Moosmang, S. et al. Cellular expression and functional characterization of four hyperpolarization-activated pacemaker channels in cardiac and neuronal tissues. Eur J Biochem 268, 1646–52 (2001).
Shi, W. et al. Distribution and prevalence of hyperpolarization-activated cation channel (HCN) mRNA expression in cardiac tissues. Circ Res 85, e1–6 (1999).
Tellez, J. O. et al. Differential expression of ion channel transcripts in atrial muscle and sinoatrial node in rabbit. Circ Res 99, 1384–93 (2006).
Herrmann, S., Stieber, J., Stockl, G., Hofmann, F. & Ludwig, A. HCN4 provides a ‘depolarization reserve’ and is not required for heart rate acceleration in mice. EMBO J 26, 4423–32 (2007).
Ludwig, A. et al. Absence epilepsy and sinus dysrhythmia in mice lacking the pacemaker channel HCN2. EMBO J 22, 216–24 (2003).
Harzheim, D. et al. Cardiac pacemaker function of HCN4 channels in mice is confined to embryonic development and requires cyclic AMP. EMBO J 27, 692–703 (2008).
Cerbai, E. et al. Characterization of the hyperpolarization-activated current, I(f), in ventricular myocytes from human failing heart. Circulation 95, 568–71 (1997).
Fernandez-Velasco, M. et al. Regional distribution of hyperpolarization-activated current (If) and hyperpolarization-activated cyclic nucleotide-gated channel mRNA expression in ventricular cells from control and hypertrophied rat hearts. J Physiol 553, 395–405 (2003).
Hoppe, U. C., Jansen, E., Sudkamp, M. & Beuckelmann, D. J. Hyperpolarization-activated inward current in ventricular myocytes from normal and failing human hearts. Circulation 97, 55–65 (1998).
Stilli, D. et al. Myocardial remodeling and arrhythmogenesis in moderate cardiac hypertrophy in rats. Am J Physiol Heart Circ Physiol 280, H142–50 (2001).
Stillitano, F. et al. Molecular basis of funny current (If) in normal and failing human heart. J Mol Cell Cardiol 45, 289–99 (2008).
Bohm, M. et al. Heart rate as a risk factor in chronic heart failure (SHIFT): the association between heart rate and outcomes in a randomised placebo-controlled trial. Lancet 376, 886–94 (2010).
Swedberg, K. et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 376, 875–85 (2010).
Ulens, C. & Tytgat, J. Functional heteromerization of HCN1 and HCN2 pacemaker channels. J Biol Chem 276, 6069–72 (2001).
Biel, M., Wahl-Schott, C., Michalakis, S. & Zong, X. Hyperpolarization-activated cation channels: from genes to function. Physiol Rev 89, 847–85 (2009).
Ludwig, A. et al. Two pacemaker channels from human heart with profoundly different activation kinetics. EMBO J 18, 2323–9 (1999).
Mistrik, P. et al. The murine HCN3 gene encodes a hyperpolarization-activated cation channel with slow kinetics and unique response to cyclic nucleotides. J Biol Chem 280, 27056–61 (2005).
Seifert, R. et al. Molecular characterization of a slowly gating human hyperpolarization-activated channel predominantly expressed in thalamus, heart and testis. Proc Natl Acad Sci USA 96, 9391–6 (1999).
Pian, P., Bucchi, A., Decostanzo, A., Robinson, R. B. & Siegelbaum, S. A. Modulation of cyclic nucleotide-regulated HCN channels by PIP(2) and receptors coupled to phospholipase C. Pflugers Arch 455, 125–45 (2007).
Pian, P., Bucchi, A., Robinson, R. B. & Siegelbaum, S. A. Regulation of gating and rundown of HCN hyperpolarization-activated channels by exogenous and endogenous PIP2. J Gen Physiol 128, 593–604 (2006).
Zolles, G. et al. Pacemaking by HCN channels requires interaction with phosphoinositides. Neuron 52, 1027–36 (2006).
Flynn, G. E. & Zagotta, W. N. Molecular mechanism underlying phosphatidylinositol 4,5-bisphosphate-induced inhibition of SpIH channels. J Biol Chem 286, 15535–42 (2011).
Levitan, I. Cholesterol and Kir channels. IUBMB Life 61, 781–90 (2009).
Huang, Y. et al. Cardiac systolic and diastolic dysfunction after a cholesterol-rich diet. Circulation 109, 97–102 (2004).
Pierce, G. N. & Dhalla, N. S. Sarcolemmal Na+-K+-ATPase activity in diabetic rat heart. Am J Physiol 245, C241–7 (1983).
Barbuti, A. et al. Localization of pacemaker channels in lipid rafts regulates channel kinetics. Circ Res 94, 1325–31 (2004).
Romanenko, V. G. et al. Cholesterol sensitivity and lipid raft targeting of Kir2.1 channels. Biophys J 87, 3850–61 (2004).
Romanenko, V. G., Rothblat, G. H. & Levitan, I. Modulation of endothelial inward-rectifier K+ current by optical isomers of cholesterol. Biophys J 83, 3211–22 (2002).
Renaud, J. F. et al. Normal serum and lipoprotein-deficient serum give different expressions of excitability, corresponding to different stages of differentiation, in chicken cardiac cells in culture. Proc Natl Acad Sci USA 79, 7768–72 (1982).
Mitsnefes, M. M. et al. Abnormal carotid artery structure and function in children and adolescents with successful renal transplantation. Circulation 110, 97–101 (2004).
Maguy, A., Hebert, T. E. & Nattel, S. Involvement of lipid rafts and caveolae in cardiac ion channel function. Cardiovasc Res 69, 798–807 (2006).
Macdonald, J. L. & Pike, L. J. A simplified method for the preparation of detergent-free lipid rafts. J Lipid Res 46, 1061–7 (2005).
Elinder, F., Mannikko, R., Pandey, S. & Larsson, H. P. Mode shifts in the voltage gating of the mouse and human HCN2 and HCN4 channels. J Physiol 575, 417–31 (2006).
Mannikko, R., Pandey, S., Larsson, H. P. & Elinder, F. Hysteresis in the voltage dependence of HCN channels: conversion between two modes affects pacemaker properties. J Gen Physiol 125, 305–26 (2005).
Xiao, Y. F. et al. Hysteresis in human HCN4 channels: a crucial feature potentially affecting sinoatrial node pacemaking. Sheng Li Xue Bao 62, 1–13 (2010).
Bolotina, V., Omelyanenko, V., Heyes, B., Ryan, U. & Bregestovski, P. Variations of membrane cholesterol alter the kinetics of Ca2(+)-dependent K+ channels and membrane fluidity in vascular smooth muscle cells. Pflugers Arch 415, 262–8 (1989).
D’Avanzo, N., Cheng, W. W., Doyle, D. A. & Nichols, C. G. Direct and specific activation of human inward rectifier K+ channels by membrane phosphatidylinositol 4,5-bisphosphate. J Biol Chem 285, 37129–32 (2010).
Heaps, C. L., Tharp, D. L. & Bowles, D. K. Hypercholesterolemia abolishes voltage-dependent K+ channel contribution to adenosine-mediated relaxation in porcine coronary arterioles. Am J Physiol Heart Circ Physiol 288, H568–76 (2005).
Levitan, I., Christian, A. E., Tulenko, T. N. & Rothblat, G. H. Membrane cholesterol content modulates activation of volume-regulated anion current in bovine endothelial cells. J Gen Physiol 115, 405–16 (2000).
D’Avanzo, N., Hyrc, K., Enkvetchakul, D., Covey, D. F. & Nichols, C. G. Enantioselective protein-sterol interactions mediate regulation of both prokaryotic and eukaryotic inward rectifier K+ channels by cholesterol. PLoS One 6, e19393 (2011).
Demel, R. A. & De Kruyff, B. The function of sterols in membranes. Biochim Biophys Acta 457, 109–32 (1976).
Jiang, Y. Q., Sun, Q., Tu, H. Y. & Wan, Y. Characteristics of HCN channels and their participation in neuropathic pain. Neurochem Res 33, 1979–89 (2008).
Gaist, D. et al. Statins and risk of polyneuropathy: a case-control study. Neurology 14, 1333–13337 (2002).
Paschoal, M. A., Trevizan, P. F. & Scodeler, N. F. Heart rate variability, blood lipids and physical capacity of obese and non-obese children. Arq Bras Cardiol 93, 239–46 (2009).
Ambudkar, I. S. Cellular domains that contribute to Ca2+ entry events. Sci STKE 2004, pe32 (2004).
Bavro, V. N. et al. Structure of a KirBac potassium channel with an open bundle crossing indicates a mechanism of channel gating. Nat Struct Mol Biol 19, 158–63 (2012).
Bowles, D. K., Heaps, C. L., Turk, J. R., Maddali, K. K. & Price, E. M. Hypercholesterolemia inhibits L-type calcium current in coronary macro-, not microcirculation. J Appl Physiol 96, 2240–8 (2004).
Lockwich, T. P. et al. Assembly of Trp1 in a signaling complex associated with caveolin-scaffolding lipid raft domains. J Biol Chem 275, 11934–42 (2000).
Lundbaek, J. A. et al. Regulation of sodium channel function by bilayer elasticity: the importance of hydrophobic coupling. Effects of Micelle-forming amphiphiles and cholesterol. J Gen Physiol 123, 599–621 (2004).
Martens, J. R. et al. Differential targeting of Shaker-like potassium channels to lipid rafts. J Biol Chem 275, 7443–6 (2000).
Toselli, M., Biella, G., Taglietti, V., Cazzaniga, E. & Parenti, M. Caveolin-1 expression and membrane cholesterol content modulate N-type calcium channel activity in NG108-15 cells. Biophys J 89, 2443–57 (2005).
Wu, C. C. et al. The effect of hypercholesterolemia on the sodium inward currents in cardiac myocyte. J Mol Cell Cardiol 27, 1263–9 (1995).
Yeagle, P. L. The biophysics and cell biology of cholesterol: An hypothesis for the essential role of cholesterol in mammalian cells. in Cholesterol in Membrane Models (ed. Finegold, L. ) 1–10 (CRC Press, Boca Raton, 1993).
Simons, K. & Toomre, D. Lipid rafts and signal transduction. Nat Rev Mol Cell Biol 1, 31–9 (2000).
Barbuti, A. et al. A caveolin-binding domain in the HCN4 channels mediates functional interaction with caveolin proteins. J Mol Cell Cardiol 53, 187–95 (2012).
Rybin, V. O., Xu, X., Lisanti, M. P. & Steinberg, S. F. Differential targeting of beta -adrenergic receptor subtypes and adenylyl cyclase to cardiomyocyte caveolae. A mechanism to functionally regulate the cAMP signaling pathway. J Biol Chem 275, 41447–57 (2000).
Dreja, K. et al. Cholesterol depletion disrupts caveolae and differentially impairs agonist-induced arterial contraction. Arterioscler Thromb Vasc Biol 22, 1267–72 (2002).
Ushio-Fukai, M. et al. Cholesterol depletion inhibits epidermal growth factor receptor transactivation by angiotensin II in vascular smooth muscle cells: role of cholesterol-rich microdomains and focal adhesions in angiotensin II signaling. J Biol Chem 276, 48269–75 (2001).
Ohtani, Y., Irie, T., Uekama, K., Fukunaga, K. & Pitha, J. Differential effects of alpha-, beta- and gamma-cyclodextrins on human erythrocytes. Eur J Biochem 186, 17–22 (1989).
Ottico, E. et al. Dynamics of membrane lipid domains in neuronal cells differentiated in culture. J Lipid Res 44, 2142–51 (2003).
Shiraishi, T., Hiraiwa, M. & Uda, Y. Effects of cyclodextrins on the hydrolysis of ganglioside GM1 by acid beta-galactosidases. Glycoconj J 10, 170–4 (1993).
Singh, I. & Kishimoto, Y. Effect of cyclodextrins on the solubilization of lignoceric acid, ceramide and cerebroside and on the enzymatic reactions involving these compounds. J Lipid Res 24, 662–5 (1983).
Acknowledgements
We would like to thank Dr. Juliane Stieber for her generous gift of the human HCN clones and Dr. Rikard Blunck for access to necessary equipment. Sources of Funding: This work was supported by a Grant-in-Aid from the Heart & Stroke Foundation of Canada (Award No. G-13-0001882). OF is supported by a bourses de prestige from GÉPROM, an FRQS funded research group.
Author information
Authors and Affiliations
Contributions
O.F. performed experiments. O.F and N.D. designed experiments, analyzed the data, wrote the manuscript and prepared figures.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Fürst, O., D’Avanzo, N. Isoform dependent regulation of human HCN channels by cholesterol. Sci Rep 5, 14270 (2015). https://doi.org/10.1038/srep14270
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep14270
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.