Key Points
-
Discusses articaine which is a local anaesthetic differing in chemical structure from the other amide anaesthetics and generally used in higher concentrations.
-
Notes that several retrospective studies suggest a higher risk of paraesthesia after administration of articaine at a concentration of 4 % when compared to other anaesthetics used at lower concentrations.
-
Highlights that in animal studies and in cell culture experiments articaine did not have a higher toxicity compared to other amide-anaesthetics.
Abstract
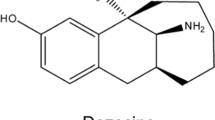
The biochemical composition of articaine differs from other amide anaesthetics. The lipophilic part of articaine consists of a thiophene ring, whereas other amide anaesthetics contain a benzene ring. When used correctly, local anaesthetics are remarkably safe. However, all local anaesthetics are potentially neurotoxic. In rare cases a prolonged abnormal perception/sensation may be present after the expected duration of action (paraesthesia). In several countries retrospective studies have been conducted that examined the incidence of persistent paraesthesia after the use of local anaesthetics. In most studies the number of paraesthesia cases after the use of articaine was higher than the market share of this anaesthetic. In animal studies and in cell culture experiments, however, articaine did not have a higher toxicity compared to other amide anaesthetics. Further studies of the cause of paraesthesia after administration of local anaesthetics seem to be warranted.
Similar content being viewed by others
Introduction
Local anaesthetics are frequently used in dental practice. Suppression of pain increases the patient's comfort and enables the dentist to work calmly and concentrate. After some time, the normal sensation should return.
Pain stimuli are primarily generated by sensory free nerve endings. Mechanical, thermal or chemical stimuli can open ion canals, thereby changing the electrical balance of the nerve membrane. If the depolarisation exceeds the threshold, an action potential is generated. This action potential is conducted through successive depolarisation over the nerve membrane. Anaesthetics block the ion canals, causing a temporary local insensitivity for pain stimuli.1
Amide anaesthetics used in dentistry are composed of a lipophilic part, connected to a hydrophilic part through an amide chain. The molecular structure of articaine differs from other amide anaesthetics in that the lipophilic part consists of a thiophene ring, whereas other anaesthetics have a benzene ring. This thiophene ring is thought to increase the lipid solubility. The thiophene ring also contains an additional ester group.2
The duration of the actual anaesthetic effect depends on diffusion and subsequent redistribution within the tissues around the injection site. Therefore, administered dose, lipid solubility and the presence of a vasoconstrictor will affect the duration time.3
In 2011, a meta-analysis compared the effectiveness of articaine 4% with the effectiveness of lidocaine 2%. Articaine gave a significant increase in achieving successful anaesthesia for infiltration anaesthesia. For conductive block anaesthesia, there was no significant difference between either anaesthetics.4
In general, local anaesthetics are very safe agents. However, in some cases an abnormally long alteration/sensation is still present after the expected duration. This is called paraesthesia, and may be temporary or permanent.
A test group of 1,325 people, who had had articaine or lidocaine injected during dental treatment, were contacted at a later date by phone. One in every 53 participants reported a prolonged duration of anaesthesia or an abnormal sensation. There was a higher frequency observed among those patients who had received articaine (1 in 49) compared to those injected with lidocaine (1 in 63). The duration of paraesthesia ranged from less than a day to 18 days after dental treatment.5
Estimations of persistent paraesthesia caused by local anaesthetics range from 1:160,5716 to 1:4,156,8487 in the available literature. This could be caused by the use of a higher concentration of an anaesthetic, which is intrinsically neurotoxic.2 Every anaesthetic is potentially neurotoxic. Direct injection of a high concentration anaesthetic (5% lidocaine) causes irreversible nerve damage.8 Intrafascicular injection of amide anaesthetics also results in nerve damage.9 This could be caused by the use of high pressure during injection, or the formation of oxygen radicals.10
Paraesthesia can also be caused by penetration of the nerve by the needle or dental procedure. Surgical removal of a mandibular third molar or the placing of an implant in the mandibular premolar/molar area could provoke a persistent sensitivity disturbance. Furthermore, paraesthesia can be caused by non dental causes, for example infections or degenerative diseases.11,12
In Canada, 1995, a retrospective study of complaints after administration of anaesthetics was published. The complaints were submitted to a liability programme. According to this study, there was an increased frequency of paraesthesia after injection with articaine, compared to the market share for this anaesthetic.13 In the last few years, warnings have been posted on the internet and published through other media against the use of articaine. Besides paraesthesia, several other physical complaints have also been attributed to the use of articaine. Dentists are frequently confronted with patients refusing anaesthetics containing articaine. In the Netherlands, 2011, a Dutch dentist was convicted for the repeated use of articaine during dental treatment (Box 1).
In this contribution, a literature review of possible neurotoxicity after use of articaine is described. Both clinical and in-vitro studies are investigated.
Material and methods
PubMed and Web of Science were searched with the search query described below. References of articles were searched for additional articles:
(paresthesia OR paraesthesia OR neurotoxic OR neurotoxicity OR toxicity OR nerve damage OR nerve injury OR prolonged anaesthesia OR prolonged anaesthesia OR hypoaesthesia OR hypoesthesia OR dysaesthesia OR dysesthesia OR neuropraxia OR neurotmesis OR axonotmesis OR numbness) AND (carticain OR articain OR articaine OR septanest OR ultracain OR ultracaine OR septocain OR septocaine OR bucanest OR deltazine OR ubistesin OR loncarti OR citocartin OR zorcain OR zorcaine OR astracain OR astracaine OR articadent OR citocain OR citocaine OR alphacain OR alphacaine OR dentocain OR dentocaine)
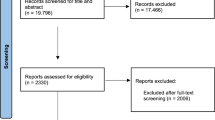
This search resulted in 128 records (see Figure 1). One investigator (A. J. G. H.) screened potential articles based on the titles. Eighty records were excluded as non-relevant. One publication could not be retrieved. The abstracts and the complete text of the remaining 47 articles were read by two investigators (A.J. G. H. and H. S. B.). Retrospective studies and clinical trials were included if they reported an incidence rate of paraesthesia or they evaluated the frequency of paraesthesia in relation to the market share of anaesthetics. If the available data could be converted to one of these parameters, the study was also included. Animal and in vitro studies were also included if articaine had been compared to other anaesthetics. The term paraesthesia is used for any type of changed sensation. 'Persistent' paraesthesia was defined as duration of paraesthesia for at least three months after administration of the anaesthetic. Ultimately, 16 clinical studies and four in vitro studies were included in this review.
Clinical studies
In Canada, the United States and Europe several retrospective studies on the incidence of paraesthesia after the use of local anaesthetics have been performed. An overview of study design and reported incidences of paraesthesia are presented in Table 1.
Canada
The first retrospective study of paraesthesia after administration of local anaesthetics appeared in 1995.13 The Professional Liability Program of the Royal College of Dental Surgeons of Ontario provided spontaneous complaints about anaesthetics, filed between 1973 and 1993. Every reported case of prolonged anaesthesia after the administration of a local anaesthetic was investigated. In 29% of the cases the lower lip was affected, in 65% the tongue, and in 6% both lower lip and tongue. Paraesthesia was not related to the age or gender of the patient. The market share of the local anaesthetics during the last year of the studied period was examined by the use of a questionnaire. Fourteen cases of paraesthesia were reported in 1993. Articaine was used in 71% of these cases, while its market share was 38%. The reported incidence of paraesthesia after administration of articaine was 1:439.897 injections. Prilocaine 4% was also associated with a slightly increased incidence of paraesthesia: 28% of the cases were related to prilocaine 4%, with a market share of 20% for this anaesthetic. In 1994, a subsequent study was conducted by the same researchers, again using complaints filed at the liability programme.14 In this study, the incidence of paraesthesia after administration of articaine was 1: 487,805.
When the period between 1999 and 2008 was studied, 64 cases of paraesthesia were identified.15 The market share of different local anaesthetics was investigated with a questionnaire for 2006, 2007 and 2008. During these three years, 70% of the cases of paraesthesia were observed after the administration of articaine. Since the market share for this anaesthetic was 44% during the same period, this meant again an overrepresentation of paraesthesia if articaine was used. The incidence of paraesthesia after administration of articaine was 1:410,000, with no difference between men and women. In 94.5% of the cases, paraesthesia was observed after a mandibular block, in 4.4% after a combination of a mandibular block and another injection technique, and in one case after infiltration anaesthesia near the 35. The tongue was most frequently affected (79%), followed by the lower lip and chin (28%) and the cheek (4.5%). In 10 % of the cases the tongue and lower lip were both affected.
United States
Between 2003 and 2005, the University of California investigated 57 patients, who were referred to the department of Oral and Maxillofacial Surgery for injuries of the inferior alveolar nerve or the lingual nerve.16 Patients were included when the symptoms lasted for at least nine months, being considered permanent. Symptoms ranged from mild to severe paraesthesia. There was no report of full anaesthesia in the affected area. Articaine was used in 30% of the cases of paraesthesia, while its market share was estimated at 25%. During a subsequent study of the period between 2006 and 2011 by the same researcher, 41 patients were included.17 No overrepresentation of paraesthesia after use of articaine was observed: articaine was used in 33% of the patients, and its estimated market share in this period was 38%. However, an increased risk of paraesthesia was observed after administration of prilocaine 4%:34% of the cases with only a market share of 8%.17
A retrospective study retrieved data from the Adverse Event Reporting System of the Food and Drug Administration (FDA) for the period 1997–2008.7 This database records adverse reactions to medication, reported by health professionals and consumers on a voluntary basis. The database was searched for neuropathy (including paraesthesia, hyperesthesia, hypo-esthesia, dysesthesia, dysgeusia, ageusia and a burning sensation). Inclusion criteria were oral paraesthesia and dental treatment without surgical procedures. This resulted in 248 cases. The researchers bought information about the market share from a company called Strategic Data Marketing. During the whole study period, articaine was used in 51% of the paraesthesia cases, while its market share was 14%. However, articaine was not introduced on the American market until 2000. When the data are limited to the period 2000–2008, the results change. Namely, articaine was used in 84% of the paraesthesia cases, with a market share of 19%.
The incidence of paraesthesia after articaine administration was 1: 4,159,848. The duration of paraesthesia was documented in approximately half of the cases, and ranged from one day to 736 days. In 94.5% of the cases paraesthesia was reported after a mandibular block, in 1% after a mental nerve block and in 4.5% after infiltration anaesthesia in the maxilla. The most frequently affected area was the tongue (89%), in 7% the lower lip and both in 4 %. In 34 cases resolution of the paraesthesia was reported.
Another study used data from the Adverse Event Reporting System of the FDA for the period 2004 to 2011.18 Searching for 'paraesthesias and dysaesthesias', 528 cases were found in the database. Searching for 'oral paraesthesia' resulted in an additional 82 reports. Adverse reactions were not related to market share, but a reporting odds ratio was calculated for each anaesthetic. This is the ratio between the cases of paraesthesia, and the number of other adverse reactions reported for the same anaesthetic. Articaine showed the highest reporting odds ratio, suggesting an increased chance of paraesthesia after use. However, the authors did not seem to realise articaine's lower risk of systemic toxicity.19 This may also be (partly) responsible for the increased reporting odds ratio.
Europe
In Denmark, patients with lingual nerve damage were investigated between 2002 and 2004 using a database from an insurance company.20 Articaine was used in 87% of the reported cases of paraesthesia, with a market share of 42%. However, it is not clear how the market share of the different anaesthetics was determined. Inclusion criteria and the duration of paraesthesia were also not reported. The estimated incidence of paraesthesia after use of articaine was 1: 140,000.
Another study in Denmark used data from the Danish Medicines Agency.21 This agency maintains a database for adverse reactions to prescribed medication, and also registers the number of medication sales. During 2001–2007, 181 complaints of paraesthesia after the use of anaesthesia were filed. Articaine was used in 78% of the cases, with a reported market share of 41%. For prilocaine used in a concentration of 3% the opposite was found: 8.8% of the cases of paraesthesia were related to prilocaine, with a market share of 19.4%.21
A subgroup of patients was examined by an oral maxillofacial surgeon. Seventy percent of these patients were female, and articaine was used in 71% of the patients. Articaine had been administered in ten of the 11 patients with permanent paraesthesia of two branches of the trigeminal nerve.
In Germany, a retrospective study was conducted for the period from 1975 to 1999, using the registration of adverse reactions by the manufacturer of local anaesthetics containing articaine.22 The sales numbers were also provided by the manufacturer. In the period investigated, 242 cases of 'neurological symptoms' were reported to the manufacturer, but without details of the duration of the symptoms. In the same period, 775 million cartridges of articaine were sold, resulting in an incidence of 1:3,202,480.
In 2003 the Dutch Dental Association distributed a questionnaire to dentists about sensibility disorders related to local anaesthetics.23 In 89 % of the cases of paraesthesia after a mandibular block, articaine had been administered. During the same period, 70 % of the Dutch dentists used articaine as a local anaesthetic.24
In the United Kingdom, adverse reactions to local anaesthetics were investigated for the period 1998–2008.25 The Yellow Card Scheme is helping the Medicines and Healthcare products Regulatory Agency (MHRA) to monitor the safety of all healthcare products. Adverse reactions to medication can be filed by both health professionals and patients on a voluntary basis. In most of the cases registered in this database, information is missing about the duration of the complaints. Information about other potential causes of paraesthesia, for example, surgical procedures, is also absent. In 77% of the identified complaints about paraesthesia, articaine had been administered. According to the Strategic Data Marketing company, the market share of articaine was 13%. The incidence of paraesthesia after use of articaine was estimated 1: 1,684,132. In 85 % of the cases the mandibula was affected, in 15 % the maxilla. The affected area was the tongue in 53% of the cases, the lower lip in 20%, and in the other cases the upper lip, chin, cheek, and/or oral mucosa. Almost two thirds of the patients were female.
Animal and in vitro studies
Toxicity of anaesthetics has also been investigated in animal and in vitro investigations. Paper cones packed inside polyethylene tubes were soaked in different anaesthetics and subcutaneously implanted in rats. Several anaesthetics, 0.5%-bupivacaine with 1:200,000 adrenaline, 4%-articaine with 1:100,000 adrenaline, 2%-lidocaine without vasoconstrictor, 2%-mepivacaine with 1:100,000 adrenaline were compared with each other and with a physiological salt solution. Articaine induced a higher inflammatory reaction than lidocaine but was comparable with the other anaesthetics investigated. The investigators assumed that their results are related to the pH of the anaesthetic solution: the local anaesthetics containing adrenaline having a much lower pH than lidocaine without adrenaline.26
Neuroblastoma cells have been incubated with different anaesthetics for 24 hours, and subsequent cell death was determined.27 The cell death was dependent on the concentration of the anaesthetic. When the concentration leading to 50% cell death was determined for each anaesthetic, articaine proved to be less toxic than the other evaluated anaesthetics: tetracaine, bupivacaine, prilocaine, mepivacaine, ropivacaine and lidocaine. In a similar study by the same researchers, T-lymphoma cells were also incubated with anaesthetic.28 Also for this cell type, a concentration dependent toxicity was observed with articaine being more toxic than mepivacaine but less toxic than the other anaesthetics, among which was lidocaine.
In these two laboratory studies, cells were exposed to anaesthetics for 24 hours. As this differs considerably from the much shorter exposure in patients, an in vitro study has been performed in which neuroblastoma cells were exposed to anaesthetics for only 20 minutes.29 Articaine and ropivacaine proved to be the least toxic, mepivacaine, prilocaine and lidocaine average, and bupivacaine the most toxic. However, the authors of this study warn that one should be careful with the clinical interpretation of these results: articaine might be 2.7 times less toxic than lidocaine, but at equal concentrations articaine is clinically 1.5 times less effective.
Recently, an animal study was performed on the toxicity of articaine and lidocaine.30 Rats were divided into three groups. One group of rats received articaine 4% with adrenaline near the first molar on one side of the jaw. The other two experimental groups received lidocaine 2% with adrenaline or only adrenaline. Twenty-four hours after injection, the rats were killed and prepared for histological investigation. The inflammatory response in the rats injected with articaine did not differ from the group that received a lidocaine injection.
Discussion
In most retrospective investigations of paraesthesia cases, an overrepresentation of articaine has been reported relative to its market share. A possible explanation is that articaine is used at a 4%-concentration, a higher concentration than most other anaesthetics. This suggestion is supported by the observation that prilocaine used in a concentration of 4%, is also associated with an increased incidence of paraesthesia,13,17 while used in a concentration of 3% the opposite was found.21
Articaine could, because of its different chemical structure with a thiophene ring, have a higher intrinsic neurotoxicity than other anaesthetics at equal concentrations. However, animal and in vitro investigations do not support this suggestion. In most of these studies, articaine was less cytotoxic than, or comparable to, other anaesthetics.26,27,28,29,30 It has been suggested that enzymes could hydrolyse the amide structure of anaesthetics at the injection site. For articaine, used in a concentraton of 4%, this could result in the formation of higher concentrations of alcohol molecules in and around neurons. Neuronal damage by this alcohol could be the cause of paraesthesia.31
A potential confounding factor in the clinical studies of the incidence of paraesthesia after administration of a local anaesthetic might be the age of the dentist. In Australia and the Netherlands, mainly young dentists used articaine as an anaesthetic.23,32 Specifically in the Netherlands, dentists reporting patients with a sensibility disorder were on average younger.24 Overdoses of local anaesthetics are also more frequently administered by less experienced dentists.33 Less experienced dentists could have a higher risk of causing nerve damage by injecting too fast9 or damaging nerves mechanically with the injection needle. Therefore, the overrepresentation of sensibility disorders for articaine might be related by the use of articaine by younger, less experienced dentists. This suggestion is rejected by Hillerup and colleagues.21 In their investigation, 11 patients had damage to two branches of the trigeminal nerve. This is considered highly improbable as the result of mechanical damage done by an injection needle.
In the retrospective clinical studies, the number of patients with paraesthesia is often compared to the relative market share of the anaesthetics used. This market share is sometimes estimated. It is also worth noticing that the studies reporting a highly increased risk for paraesthesia after use of articaine, were both based on sales data from the same company, reporting a very small market share for this anaesthetic.7,25
The differences in the number of cases with paraesthesia between the studies of Garisto et al. (2010)7 and Piccinni et al. (2014)18 is also remarkable. Both studies obtained their information from the same database, but used different search queries. Over a periode of 11 years, Garisto and colleagues identified 116 cases of paraesthesia related to articaine, 97 to prilocaine, 11 to lidocaine, one to bupivacaine and one to mepivacaine. However, Piccinni et al. found over a period of seven years, 266 cases of paraesthesia after administration of lidocaine, 122 after articaine, 106 after bupivacaine, 58 after a combination of anaesthetics and 44 after prilocaine. This difference suggests that the search query used during the analysis of a database may have a considerable effect on the outcome.
Retrospective studies show that the lingual nerve is more frequently damaged after administration of articaine than the inferior alveolar nerve. The lingual nerve might be more vulnerable, as it consists of less fasciculi.34 Moreover, damage of the lingual nerve is considered more unpleasant by patients,20 increasing the likelihood that is it reported more often.
Retrospective studies are useful to identify rare complications of medication, but are also liable to bias. The retrospective studies discussed above are based mainly on voluntary information, sometimes from patients. The information provided is often incomplete. Furthermore, articaine is a relatively new anaesthetic, increasing the chance that complications will be reported. Media and internet attention for articaine could also lead to an increased awareness and reportage of complaints related to this anaesthetic.
Like all other anaesthetics used in dentistry, articaine is very safe. However, dentists might be confronted with patients who object against the administration of this anaesthetic. The decision of the Dutch judges (Box 1) indicates that it seems wise to take these objections seriously and, if the patient persists in this opinion, to divert to another anaesthetic. Considering that dentists must be able to demonstrate informed consent, obtaining written informed consent before the administration of an anaesthetic seems recommendable.1
The occurrence of a persistent sensitivity disorder after administration of local anaesthesia is very rare, and usually the result of the subsequent dental procedure. Only very rarely is it a complication of the administered anaesthetic. Most sensitivity disorders will recover spontaneously. However, when it persists unaltered from more than three months, the patient should be referred to an oral maxillofacial surgeon.1
Conclusion
Persistent sensibility disorders after administration of local anaesthetics are rare. Several retrospective studies suggest a higher risk of paraesthesia after administration of articaine in a concentration of 4 % compared to other anaesthetics used at lower concentrations. However, this observation is not supported by in vitro studies and animal experiments. Further investigation of possible causes of paraesthesia after use of local anaesthetics seems to be warranted. Improved registration of the use of local anaesthetics and eventual complications would facilitate and contribute to this.
References
Baart J A, Brand H S . Local anaesthesia in dentistry. Second edition. Springer: Switzerland, 2017.
Becker D E, Reed K L . Local anaesthetics: review of pharmacological considerations. Anesth Prog 2012; 59: 90–101.
Becker D E, Reed K L . Essentials of local anaesthetic pharmacology. Anesth Prog 2006; 53: 98–108.
Brandt R G, Anderson P F, McDonald N J, Sohn W, Peters M C . The pulpal anaesthetic efficacy of articaine versus lidocaine in dentistry: a meta-analysis. J Am Dent Assoc 2011; 142: 493–504.
Malamed S F, Gagnon S, Leblanc D . Articaine hydrochloride: a study of the safety of a new amide local anaesthetic. J Am Dent Assoc 2001; 132: 177–185.
Pogrel M A, Thamby S . Permanent nerve involvement resulting from inferior alveolar nerve blocks. J Am Dent Assoc 2000; 131: 901–907.
Garisto G A, Gaffen A S, Lawrence H P, Tenenbaum H C, Haas D A . Occurrence of paresthesia after dental local anaesthetic administration in the United States. J Am Dent Assoc 2010; 141: 836–844.
Lambert L A, Lambert D H, Strichartz G R . Irreversible conduction block in isolated nerve by high concentrations of local anaesthetics. Anaesthesiology 1994; 80: 1082–1093.
Jeng C L, Rosenblatt M A . Intraneural injections and regional anaesthesia: the known and the unknown. Minerva Anestesiol 2011; 77: 54–58.
Saray A, Apan A, Kisa U . Free radical-induced damage in experimental peripheral nerve injection injury. J Reconstr Microsurg 2003; 19: 401–406.
Smith J H, Cutrer F M . Numbness matters: a clinical review of trigeminal neuropathy. Cephalalgia An Int J Headache 2011; 31: 1131–1144.
Sharif-Alhoseini M, Rahimi-Movaghar V, Vaccaro A R . Underlying Causes of Paresthesia. In Imbelloni L E, Gouveia MA (editors) Paresthesia. pp 71–100. InTech: Croatia, 2012.
Haas D A, Lennon D . A 21 year retrospective study of reports of paresthesia following local anaesthetic administration. J Can Dent Assoc 1995; 61: 319–330.
Haas D A, Lennon D . A review of local anaesthetic-induced paresthesia in Ontario in 1994. J Dent Res 1996; 75: 247.
Gaffen A S, Haas D A . Retrospective review of voluntary reports of nonsurgical paresthesia in dentistry. J Can Dent Assoc 2009; 75: 579.
Pogrel M A . Permanent nerve damage from inferior alveolar nerve blocks an update to include articaine. J Calif Dent Assoc 2007; 35: 271–273.
Pogrel M A . Permanent nerve damage from inferior alveolar nerve blocks: a current update. J Calif Dent Assoc 2012; 40: 795–797.
Piccinni C, Gissi D B, Gabusi A, Montebugnoli L, Poluzzi E . Paraesthesia after Local Anaesthetics: An Analysis of Reports to the FDA Adverse Event Reporting System. Basic Clin Pharmacol Toxicol 2014; 117: 52–56.
Oertel R, Rahn R, Kirch W . Clinical pharmacokinetics of articaine. Clin Pharmacokinet 1997; 33: 417–425.
Legarth J . Skader på nervus lingualis opstået i forbindelse med mandibularanalgesi. Tandlaegebladet 2005; 109: 786–788.
Hillerup S, Jensen R H, Ersbøll B K . Trigeminal nerve injury associated with injection of local anaesthetics: needle lesion or neurotoxicity? J Am Dent Assoc 2011; 142: 531–539.
Rahn R, Jakobs W, Ihl-Beste W. Häufigkeit von Nebenwirkungen bei zahn-ärztlicher lokalanästhesie: auswertung der nebenwirkungsmeldungen von Ultracain von 1975 bis 1999. ZWR 2000; 109: 378–381.
NMT. Omnibus-enquête najaar 2003: Sensibiliteitsstoornissen bij patiënten na lokale anaesthesie. 2004.
NMT. INDENT-onderzoek, najaar 2002: Gebruik van tandheelkundige materialen. 2003.
Zahedi S . Retrospective review of dental local anaesthetic induced paresthesia in the United Kingdom. 2012.
Ribeiro P D, Sanches M G, Okamoto T . Comparative analysis of tissue reactions to anaesthetic solutions: histological analysis in subcutaneous tissue of rats. Anesth Prog 2003; 50: 169–180.
Werdehausen R, Fazeli S, Braun S et al. Apoptosis induction by different local anaesthetics in a neuroblastoma cell line. Br J Anaesth 2009; 103: 711–718.
Werdehausen R, Braun S, Fazeli S et al. Lipophilicity but not stereospecificity is a major determinant of local anaesthetic-induced cytotoxicity in human T-lymphoma cells. Eur J Anaesthesiol 2012; 29: 35–41.
Malet A, Faure MO, Deletage N, Pereira B, Haas J, Lambert G . The comparative cytotoxic effects of different local anaesthetics on a human neuroblastoma cell line. Anesth Analg 2015; 120: 589–596.
Baroni D B, Franz-Montan M, Cogo K et al. Effect of articaine on mental nerve anterior portion: histological analysis in rats. Acta Odontol Scand 2013; 71: 82–87.
Nickel A A . A retrospective study of paresthesia of the dental alveolar nerves. Anesth Prog 1990; 37: 42–45.
Yapp K E, Hopcraft M S, Parashos P . Dentists' perceptions of a new local anaesthetic drug – articaine. Aust Dent J 2012; 57: 18–22.
Malamed S F . Allergy and toxic reactions to local anaesthetics. Dent Today 2003; 22: 114–121.
Pogrel M A, Schmidt B L, Sambajon V, Jordan R C K . Lingual nerve damage due to inferior alveolar nerve blocks: a possible explanation. J Am Dent Assoc 2003; 134: 195–199.
Acknowledgements
The authors are grateful to Ms Brigid Walker for linguistic correction of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Hopman, A., Baart, J. & Brand, H. Articaine and neurotoxicity – a review. Br Dent J 223, 501–506 (2017). https://doi.org/10.1038/sj.bdj.2017.782
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.782
This article is cited by
-
Efficacy of analgesia promoted by lidocaine and articaine in third molar extraction surgery. A split-mouth, randomized, controlled trial
Oral and Maxillofacial Surgery (2024)
-
A 15-year unique observational study of intraligamentary local anaesthesia for posterior mandibular extractions
British Dental Journal (2021)
-
Inferior alveolar nerve block: is articaine better than lidocaine?
British Dental Journal (2021)
-
The success of using 2% lidocaine in pain removal during extraction of mandibular premolars: a prospective clinical study
BMC Oral Health (2020)
-
Neurosensorische Störungen nach Lokalanästhesie
Der MKG-Chirurg (2019)