Key Points
-
Reviews the UK literature on factors associated with dental general anaesthesia.
-
Highlights that factors beyond child age, dental anxiety and dental status were associated with receiving dental treatment under general anaesthesia.
-
Understanding the distal determinants of use of dental general anaesthesia among children may help to identify high risk groups for targeted oral health promotion.
Abstract
Objectives To assess the demographic, socioeconomic, behavioural and clinical factors associated with use of dental general anaesthesia (DGA) among British children.
Methods This study used data from 3053 children who participated in the 2013 Children's Dental Health Survey in England, Wales and Northern Ireland. Data were collected through parental questionnaires and clinical examinations. The crude and adjusted association of demographic (sex, age, ethnicity and country of residence), socioeconomic (socioeconomic classification and area deprivation), behavioural (age toothbrushing started, age when first went to the dentist, usual reason for dental visit and dental anxiety) and clinical factors (numbers of decayed and filled teeth) with DGA was assessed in logistic regression models.
Results The lifetime prevalence of DGA use was 9.1%. Older children and those living in Wales, with higher levels of dental anxiety and more dental fillings, who visited the dentist only when in trouble, and who had parents in routine/manual occupations and parents who never worked have greater odds of reporting having ever used DGA.
Conclusion This study shows that family socioeconomic background, usual reason for dental visit and country of residence were associated with DGA use among British children, over and above the effect of child age, dental anxiety and dental status.
Similar content being viewed by others
Introduction
Dental general anaesthesia (DGA) is a pharmacological technique to provide extensive or urgent dental treatment – usually extractions – to children with caries within a hospital setting.1,2 DGA should not be used routinely for healthy patients but only as a last resort for dental treatment.3 The number of children being admitted for elective extractions of teeth due to caries under DGA is increasing annually,4,5 as is the average number of teeth removed.6 Approximately 45,000 children between 1 and 15 years of age were admitted to hospital for GA with a diagnosis of dental caries in England in 2014–2015.7 The 2013 UK National Health Service Anaesthesia Activity Survey shows that dental caries was the second most common reason for general anaesthesia (GA) in preschool age children and the third most common reason in school age children.8,9 There has been a significant increase in spending by the NHS for the extraction of teeth under GA,5 from £21 million in 2010/11 to £35 million in 2014/15.10,11
Given the interest in improving standards of paediatric DGA, the impact of the service on children and their parents/careers, and the financial burden to the NHS, it is important to understand the factors contributing to children who need tooth extraction due to caries under DGA. Such knowledge may help developing strategies to minimise its use in the future. It may also help characterise population groups at higher risk of receiving dental treatment under DGA with a view to target them for oral health promotion and caries prevention programmes.
Managing these DGA children and their families is a local and a national challenge.12 Few studies have explored factors associated with DGA use among children. Multiple extractions, dental anxiety and young age are the main reasons for referral of children to DGA.13,14,15,16,17 More distal determinants – those beyond behavioural factors and dental status – have rarely been explored. There is some evidence that children from ethnic minority groups18,19 and living in deprived areas4,16 are overrepresented among DGA patients compared to national statistics. However, most studies to date were based on patient samples, which limits the ability to generalise the findings to the wider population. Using hospital records also limits the amount of information available and restricts data analysis to a few specific variables. Population-based studies may overcome these limitations.
The aim of this study was to assess the demographic, socioeconomic, behavioural and clinical factors associated with the use of DGA among British children.
Materials and methods
Study population
This study used data from the 2013 Children's Dental Health Survey (CDHS), a cross-sectional survey based on a national representative sample of children aged 5, 8, 12 and 15 years attending state and independent schools in England, Wales and Northern Ireland. The total sample of 13,628 children was recruited using multi-stage stratified sampling. Children in Wales and Northern Ireland and those in most deprived schools (>30% of children eligible for free school meals) were oversampled. In England and Wales stratification was done by region. Eighty-one local authorities (LA) in England and 27 unitary authorities (UA) in Wales were selected with probability proportional to size. Primary and secondary school clusters were created within LAs and UAs. Using simple random sampling, 81 primary school clusters and 81 secondary school clusters were selected from the sampled LAs in England and 27 primary and 27 secondary school clusters were selected from the sampled UAs in Wales. A simple random sampling of schools in Northern Ireland was performed. A total of 9,866 children were clinically examined (72% participation rate), and 4214 productive parental questionnaires were returned (43% response rate).20 The sample for this study included 3053 (72%) children with complete data on all relevant variables.
Variables selection
The outcome measure for this study was the lifetime prevalence of DGA use. Parents were asked whether their child has ever had a general anaesthetic before dental treatment (child is unconscious). The survey question did not ascertain the reason for the use of DGA.
A number of variables were selected as potential determinants of DGA use. They were broadly classified as demographic, socioeconomic, behavioural and clinical factors. Demographic factors were sex, age, ethnicity and country of residence. Ethnicity was extracted from school records (White, South Asian, Black, Mixed and Other) and recoded as White or ethnic minority group due to the small numbers in some ethnic categories. Family socioeconomic position (SEP) was measured by the National Statistics Socio-Economic Classification (NS-SEC) and area deprivation. NS-SEC groups were derived using the self-coded method based on current or last main job or occupation, employment status, size of organisation and supervisory status of the parent or guardian. Eight operational categories were derived: (1) higher managerial and professional; (2) lower managerial and professional; (3) intermediate; (4) small employers and own account workers; (5) lower supervisory and technical; (6) semi-routine; (7) routine; and (8) never worked and long‐term unemployed.21 The eight categories were collapsed into managerial and professional, intermediate, and routine and manual occupations.22,23 For complete coverage of the population, individuals who had never worked or were in long-term unemployment and those not classified for other reasons were added as not classified.22,23 Area deprivation was determined based on the postcode of children's home address using the Index of Multiple Deprivation (IMD) at the Lower Super Output Area level. The 2010 IMD was used for England and Northern Ireland and the 2011 IMD for Wales. Area deprivation was divided into quintiles (least deprived to most deprived) in order to enhance comparability across countries.
Behavioural factors were the age when child started toothbrushing, age when child first visited the dentist, usual reason for dental visit and dental anxiety. Parents were asked how old the child was when they started brushing their teeth or having them brushed for them (under 6 months of age, between 6 months and 1 year, 1 and 2 years, 2 and 4 years, 4 and 6 years, and 6 years or older), how old the child was when they first went to the dentist (response in years), and the usual reason for the child going to the dentist (either for a check-up or when having trouble with teeth). Parents also indicated how anxious their child gets when they visit the dentist, using a 10-point scale, ranging from 1 for 'not at all anxious' to 10 for 'extremely anxious'.
Clinical factors were the numbers of decayed and filled teeth for both dentitions combined. Examinations were conducted by 75 trained dentists with children sitting on a fully reclining chair and using plain mouth mirrors, a periodontal probe and artificial light. Cotton wool/gauze was used to clear teeth of debris and moisture. Dental caries was visually diagnosed at the caries into dentine threshold (including visual dentine caries) without radiography or fibre-optic trans-illumination. Examiners were trained in eight groups, with good inter-examiner reliability (Kappa values ranged from 0.814 to 0.928).20
Data analysis
All analyses were performed in STATA 13 (StataCorp., College Station, TX). Analyses were weighted to adjust for the unequal probability of selection, non-response at school and pupil levels. They also took into account the complex survey design (stratification and clustering) to produce correct standard errors.
We first describe the study sample in terms of demographic (sex, age groups, ethnicity and country of residence), socioeconomic (NS-SEC classification and area deprivation), behavioural (age when started brushing, age when first went to the dentist, usual reason for dental visit and dental anxiety) and clinical dental factors (number of decayed teeth and number of filled teeth) and compare it against those excluded because of missing values to evaluate the impact of missing data. Chi-square and ttest were used when comparing categorical and continuous factors, respectively.
The association of demographic, socioeconomic, behavioural and clinical factors with lifetime prevalence of DGA use was evaluated in crude and adjusted models using logistic regression because the binary outcome was an uncommon (<10%).24 Odds ratio (OR) with 95% confidence intervals (CI) were therefore reported as the measure of association.25
Results
The characteristics of the study sample are presented in Table 1. No major differences were observed between the study sample and the full sample of participating children with complete parental questionnaires. The lifetime prevalence of DGA use was 9.1% (95% CI: 6.811.3%).
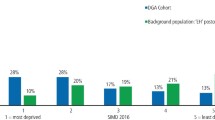
The lifetime prevalence of DGA use varied according to demographic, socioeconomic, behavioural and clinical factors (Table 2). DGA use was more common among Welsh and Irish children and those who go to the dentist only when in trouble. DGA use increased with age, age when brushing started and decreased with family SEP (both socioeconomic classification and area deprivation). In addition, children who had undergone a DGA had greater dental anxiety scores and more decayed and filled teeth than those who never used those services.
The results from regression analysis show that lifetime prevalence of DGA use was associated with some, but not all of the factors that were investigated (Table 3). Age and country of residence were the only demographic factors significantly associated with DGA use. Eight, 12- and 15-year-olds had 2.70 (95%CI: 1.29–5.69), 2.78 (95%CI: 1.50–5.14) and 3.32 (95%CI: 1.60–6.87) greater odds of DGA use than 5-year-olds, whereas Welsh children had 2.35 (95%CI: 1.47–3.75) greater odds of using DGA than English children. Socioeconomic classification, but not area deprivation, was significantly associated with DGA use. Children of parents in routine and manual occupations and those of parents who never worked had 2.08 (95%CI: 1.20–3.60) and 3.52 (95% CI: 1.10–11.26) greater odds of using DGA than those of parents in managerial and professional occupations. In terms of behavioural factors, children who visit the dentist only when in trouble had 2.47 (95% CI: 1.07–5.68) greater odds of using DGA than those who visit the dentist for regular check-ups, whereas the odds of using DGA increased by 1.20 (95%CI: 1.11–1.29) times per unit increase in dental anxiety score. As for clinical factors, the number of filled teeth, but not the number of decayed teeth, was significantly associated with DGA use. The odds of using DGA increased by 1.51 (95%CI: 1.25–1.83) times per additional tooth filled.
Discussion
This population-based study shows that nine children in every hundred in the 2013 Children's Dental Health Survey used DGA in their lifetime. In addition, the lifetime prevalence of DGA use was associated with some but not all factors investigated. Over and above the effect of child age, dental anxiety and dental status, the family SEP, usual reason for dental visit and country of residence were other factors associated with DGA in the adjusted model.
Some limitations of this study need to be addressed. First, this was a cross-sectional study, and thus, unable to establish a temporal ordering between child characteristics and DGA use. We minimised this issue by using lifetime prevalence of DGA use as the outcome measure and selecting risk factors in early life (such as age when started brushing or when first went to the dentist) or those reflecting cumulative experience (such as usual reason for dental visit and caries experience). Second, our study sample included 72% of the participants with productive parental questionnaires, which may raise some concerns about the impact of missing data and the representativeness of the sample. However, we found no differences between our study sample and the full sample of participants, suggesting that the present findings could be generalised to the study population. Third, lifetime prevalence of DGA use was based on parental reports, without information on the reasons for DGA. It is therefore possible that some children used DGA for reasons other than caries treatment, such as surgical procedures (for example, removal of unerupted supernumeraries). However, extractions due to dental caries remain the most common reason for using DGA in children.8,9 More importantly, our prevalence of DGA was comparable to previous estimates based on hospital episode statistics,4,7 supporting the validity of our data. Fourth, our analysis did not include any data on sugars, an important determinant of dental caries and subsequent services utilisation.26,27 Data on sugars intake was gathered in the pupil questionnaire, which was only administered to 12- and 15-year-olds. Furthermore, questions on sugars intake referred to current consumption, which was more likely to have happened after the actual use of DGA.
Our findings corroborate those from earlier hospital-based studies suggesting that age, dental anxiety and clinical status are the main reasons for referral of children for DGA.13,14,15,16,17 The fact that in our study older children were more likely to have had DGA is a reflection of the cumulative nature of the outcome measure used (lifetime prevalence), as opposed to the young age at presentation reported among patient samples.13,14,15,16,17 Although children who used DGA had higher caries experience than their counterparts, it was the number of filled (not decayed) teeth which remained significantly associated with DGA use in the adjusted model. This was expected as the number of fillings indicates past caries experience, although it is not possible to know from the available data whether those teeth were restored under DGA.
The present findings also emphasise the role of determinants beyond child dental status and behaviours, particularly the parental influences.28 Parents in routine/manual occupations and those unemployed were more likely to have children using DGA than parents in professional and managerial occupations. The significant crude association between area deprivation and DGA use was fully attenuated when adjusting for other factors and suggests that family socioeconomic classification may be a more sensitive indicator to identify children at higher risk of receiving DGA. Indeed, any association with area deprivation could be due to the referral pattern of dental practices in the child's area of residence rather than the relative deprivation of the neighbourhood. The fact that there was a clear social gradient in DGA use independent of child dental anxiety and clinical status implies that there must be other reasons for these groups to end up receiving dental care under GA. The influence of the family could also be seen in terms of usual reason for dental visit, with problem oriented attenders more likely to have had DGA than those who were regular attenders. Moreover, recent evidence has suggested that there are high repeat rates and GA usage within the same family and that GA for tooth extraction is culturally acceptable in some communities.15,18 We also found that Welsh children were more likely to have ever used DGA than their English counterparts, which may reflect the contrasting prevalence and severity of childhood dental caries between the two countries.29,30 This is in addition to regional differences in the availability of fluoride in public water supply as well as in access and utilisation of NHS dental care services.
This study has helped characterise children more likely to receive dental care under GA. More attention should be directed at preventing caries early in life and at addressing the main cause of caries, namely sugars consumption, and the social determinants of early childhood caries. This should be coupled with oral health promotion programmes tailored to children at greater risk (proportionate universalism). This study also provides a platform for further research into the family environment and parental influences as broader determinants of DGA use.
Conclusion
This study shows that nine children in every hundred who participated in the 2013 Children's Dental Health Survey have had DGA in their lifetime. Beyond child age, dental anxiety and dental status, other factors associated with lifetime prevalence of DGA use were family socioeconomic conditions, emergency-only dental visits and country of residence.
References
Adewale L, Morton N, Blayney M . Guidelines for the management of children referred for dental extractions under general anaesthesia. London: Association of Paediatric Anaesthetists of Great Britain and Ireland, 2011.
RCS. Guideline for the Use of General Anaesthesia (GA) in Paediatric Dentistry. London: Royal College of Surgeons of England, 2008.
Knapp R, Gilchrist F, Rodd H D, Marshman Z . Change in children's oral health-related quality of life following dental treatment under general anaesthesia for the management of dental caries: a systematic review. Int J Paediatr Dent 2016; 27: 302–312.
Moles D R, Ashley P . Hospital admissions for dental care in children: England 1997–2006. Br Dent J 2009; 206: E14.
RCS. The State of Children's Oral Health in England. London, UK: Faculty of Dental Surgery, Royal College of Surgeons of England, 2015.
Deery C, Owen J, Welbury R, Chadwick B . Dental caries in children and the level of repeat general anaesthetics for dental extractions. A national disgrace. Dent Update 2015; 42: 305–306.
HSCIC. Health Episode Statistics: Admitted Patient Care England 2014–2015. London: Health and Social Care Information Centre, 2015.
Sury M R, Arumainathan R, Belhaj A M, Mac G P J H, Cook T M, Pandit J J . The state of UK pediatric anesthesia: a survey of National Health Service activity. Paediatr Anaesth 2015; 25: 1085–1092.
Sury M R, Palmer J H, Cook T M, Pandit J J . The State of UK Dental Anaesthesia: Results From The NAP5 Activity Survey. A national survey by the 5th National Audit Project of the Royal College of Anaesthetists and the Association of Anaesthetists of Great Britain and Ireland. SAAD Dig 2016; 32: 34–36.
DOH. National Schedule of Reference Costs 2010–11. London: Department of Health, 2011.
DOH. National Schedule of Reference Costs 2014–15. London: Department of Health, 2015.
Aljafari A K, Gallagher J E, Hosey M T . Failure on all fronts: general dental practitioners' views on promoting oral health in high caries risk childrena qualitative study. BMC Oral Health 2015; 15: 45.
MacCormac C, Kinirons M . Reasons for referral of children to a general anaesthetic service in Northern Ireland. Int J Paediatr Dent 1998; 8: 191–196.
Carson P, Freeman R . Dental caries, age and anxiety: factors influencing sedation choice for children attending for emergency dental care. Community Dent Oral Epidemiol 2001; 29: 30–36.
Macpherson L M, Pine C M, Tochel C, Burnside G, Hosey M T, Adair P . Factors influencing referral of children for dental extractions under general and local anaesthesia. Community Dent Health 2005; 22: 282–288.
Hosey M T, Bryce J, Harris P, McHugh S, Campbell C . The behaviour, social status and number of teeth extracted in children under general anaesthesia: a referral centre revisited. Br Dent J 2006; 200: 331–334.
Alkilzy M, Qadri G, Horn J, Takriti M, Splieth C . Referral patterns and general anesthesia in a specialized paediatric dental service. Int J Paediatr Dent 2015; 25: 204–212.
Olley R C, Hosey M T, Renton T, Gallagher J . Why are children still having preventable extractions under general anaesthetic? A service evaluation of the views of parents of a high caries risk group of children. Br Dent J 2011; 210: E13.
Raja A, Daly A, Harper R, Senghore N, White D, Ravaghi V . Characteristics of children undergoing dental extractions under general anaesthesia in Wolverhampton: 2007–2012. Br Dent J 2016; 220: 407–411.
Anderson T, Thomas C, Ryan R, Dennes M, Fuller E . Children's Dental Health Survey 2013. Technical Report. London: Health and Social Care Information Centre, 2015.
Office for National Statistics. The National Statistics Socio-Economic Classification: user manual. Basingstoke: Palgrave Macmillan, 2005.
Delgado-Angulo E K, Bernabe E, Marcenes W . Ethnic Inequalities in Periodontal Disease among British Adults. J Clin Periodontol 2016; 43: 926–933
Delgado-Angulo E K, Bernabe E, Marcenes W . Ethnic inequalities in dental caries among adults in East London. J Public Health (Oxf) 2016; 38: e55–62.
Barros A J, Hirakata V N . Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003; 3: 21.
Hosmer D W, Lemeshow S, Sturdivant R X . Applied Logistic Regression. New York: John Wiley & Sons, Inc., 2013.
Kim Seow W . Environmental, maternal, and child factors which contribute to early childhood caries: a unifying conceptual model. Int J Paediatr Dent 2012; 22: 157–168.
Leong P M, Gussy M G, Barrow SY, de Silva-Sanigorski A, Waters E . A systematic review of risk factors during first year of life for early childhood caries. Int J Paediatr Dent 2013; 23: 235–250.
Collett B R, Huebner C E, Seminario A L, Wallace E, Gray K E, Speltz M L . Observed child and parent toothbrushing behaviors and child oral health. Int J Paediatr Dent 2016; 26: 184–192.
Pitts N B, Chadwick B, Anderson T . Children's Dental Health Survey 2013. Report 2: Dental Disease and Damage in Children. London: Health and Social Care Information Centre, 2015.
Pitts N B, Chestnutt I G, Evans D, White D, Chadwick B, Steele J G . The dentinal caries experience of children in the United Kingdom, 2003. Br Dent J 2006; 200: 313–320.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Ramdaw, A., Hosey, M. & Bernabé, E. Factors associated with use of general anaesthesia for dental procedures among British children. Br Dent J 223, 339–345 (2017). https://doi.org/10.1038/sj.bdj.2017.763
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.763
This article is cited by
-
The CALM trial protocol: a randomised controlled trial of a guided self-help cognitive behavioural therapy intervention to reduce dental anxiety in children
Trials (2023)
-
Do paediatric patient-related factors affect the need for a dental general anaesthetic?
British Dental Journal (2022)
-
Childhood caries and hospital admissions in England: a reflection on preventive strategies
British Dental Journal (2021)
-
Participation of paediatric patients in primary dental care before and after a dental general anaesthetic
European Archives of Paediatric Dentistry (2021)
-
A rapid review of variation in the use of dental general anaesthetics in children
British Dental Journal (2020)