Abstract
Aims The aims were to determine the profile of patients referred for treatment with dental general anaesthetic (DGA) and identify patient-related factors that contributed to a child requiring a DGA.
Design setting In total, 42 patients were recruited from new patient assessment clinics at the Edinburgh Dental Institute, Scotland. Prospective questionnaires were given to the patients' caregivers with questions regarding their child's dental anxiety level, ethnicity, level of English spoken and languages spoken at home. Height and weight (BMI) measurements were taken and other information (age, sex, medical history status and postcode for level of social deprivation) were collected from their medical records.
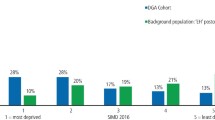
Results Compared to the local population, children referred for treatment with DGA had a significantly decreased level of English (p = 0.0001) with an increase in non-English languages at home (p = 0.0004). Patients from minority ethnic groups (p = 0.008) and children from socially deprived areas (p = 0.0001) were significantly overrepresented. Self-reported dental anxiety was high and more common in primary than secondary school-aged children (p = 0.039).
Conclusions This study highlighted several patient-related variables that may increase the likelihood of DGA treatment. Further work is required to confirm these associations and develop interventions to reduce the number of children requiring DGAs.
Key points
-
Children from minority ethnic groups and areas of increased socioeconomic deprivation were significantly overrepresented in requiring treatment under general anaesthetic.
-
Children requiring treatment under general anaesthetic had significantly lower levels of self-reported English and significantly higher levels of non-English languages at home compared to the background population.
-
Highlights several patient-related factors that may increase the likelihood of dental treatment under general anaesthetic.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Welbury R, Duggal M S, Hosey M T. Paediatric Dentistry. Oxford: Oxford University Press, 2018.
Association of Paediatric Anaesthetists of Great Britain and Ireland. Your child's general anaesthetic for dental treatment: Information for parents and guardians of children. 2009. Available at https://www.apagbi.org.uk/sites/default/files/inline-files/Your%20childs%20general%20anaesthetic%20for%20dental.pdf (accessed July 2020).
Knapp R, Marshman Z, Rodd H. Treatment of dental caries under general anaesthetic in children. BDJ Team 2017; DOI: 10.1038/bdjteam.2017.116.
Goodwin M, Sanders C, Pretty I A. A study of the provision of hospital based dental general anaesthetic services for children in the northwest of England: part 1 - a comparison of service delivery between six hospitals. BMC Oral Health 2015; 15: 50.
Landes D P. The provision of general anaesthesia in dental practice, an end which had to come? Br Dent J 2002; 192: 129-131.
British Dental Journal. Potential surge in post-COVID child tooth extractions. Br Dent J 2020; 229: 278.
Hosey M T, Macpherson L M D, Adair P, Tochel C, Burnside G, Pine C. Dental anxiety, distress at induction and postoperative morbidity in children undergoing tooth extraction using general anaesthesia. Br Dent J 2006; 200: 39-43.
Cantekin K, Yildirim M D, Cantekin I. Assessing change in quality of life and dental anxiety in young children following dental rehabilitation under general anaesthesia. Paediatr Dent 2014; 36: 12-17.
Scottish Dental Clinical Effectiveness Programme. Prevention and Management of Dental Caries in Children. 2018. Available at https://www.sdcep.org.uk/media/2zbkrdkg/sdcep-prevention-and-management-of-dental-caries-in-children-2nd-edition.pdf (accessed July 2020).
Scottish Intercollegiate Guidelines Network. Dental Interventions to prevent caries in children. 2014. Available at https://www.sign.ac.uk/media/1533/sign138.pdf (accessed July 2020).
Mejàre I, Axelsson S, Dahlën G A, Espelid I, Norlund A, Tranæus S, Twetman S. Caries risk assessment. A systematic review. Acta Odontol Scand 2014; 72: 81-91.
Ramdaw A, Hosey M T, Bernabé E. Factors associated with use of general anaesthesia for dental procedures among British children. Br Dent J 2017; 223: 339-345.
Scotland's Census. Census Data. 2011. Available at https://www.scotlandscensus.gov.uk/search-the-census#/search-by (accessed July 2020.
Scottish Government. Scottish Index of Multiple Deprivation 2020v2 local and national share calculator. 2020. Available at https://www.gov.scot/publications/scottish-index-of-multiple-deprivation-2020v2-local-and-national-share-calculator-2/ (accessed July 2020).
Information Services Division Scotland. Body Mass Index of Primary 1 Children in Scotland: School Year 2018/19. 2019. Available at https://www.isdscotland.org/Health-Topics/Child-Health/Publications/2019-12-10/2019-12-10-P1-BMI-Statistics-Publication-Report.pdf?#:~:text=Based%20on%20the%20epidemiological%20thresholds,of%20overweight%20or%20obesity%20combined) (accessed July 2020).
Howard K E, Freeman R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int J Paediatr Dent 2007; 17: 281-288.
Javadinejad S, Farajzadegan Z, Madahain M. Iranian version of a face version of the modified child dental anxiety scale: transcultural adaptation and reliability analysis. J Res Med Sci 2011; 16: 872-877.
Porritt J, Buchanan H, Hall M, Gilchrist F, Marshman Z. Assessing children's dental anxiety: a systematic review of current measures. Community Dent Oral Epidemiol 2013; 41: 130-134.
Humphris G M, Dyer T A, Robinson P G. The modified dental anxiety scale: UK general population norms in 2008 with further psychometric and effects of age. BMC Oral Health 2009; 9: 20.
Scottish Dental Clinical Effectiveness Programme. Oral Health Assessment and Review. 2011. Available at https://www.sdcep.org.uk/media/b1vlxume/sdcep-ohar-guidance-in-brief.pdf (accessed July 2020).
Haworth S, Dudding T, Waylen A, Thomas S J, Timpson N J. Ten years on: Is dental general anaesthesia in childhood a risk factor for caries and anxiety? Br Dent J 2017; 222: 299-304.
Large J.F, Keightley, A J, Busuttil-Naudi A. Participation of paediatric patients in primary dental care before and after a dental general anaesthetic. Eur Arch Paediatr Dent 2021; 22: 887-897.
Harper R, Nevill A, Senghore N, Khan I. Socioeconomic and ethnic status of two-and three-year-olds undergoing dental extractions under general anaesthesia in Wolverhampton, 2011-2016. Br Dent J 2019; 226: 349-353.
Raja A, Daly A, Harper R, Senghore N, White D, Ravaghi V. Characteristics of children undergoing dental extractions under general anaesthesia in Wolverhampton: 2007-2012. Br Dent J 2016; 220: 407-411.
Public Health Scotland. National Dental Inspection Programme (NDIP) 2020. 2020. Available at https://www.scottishdental.org/wp-content/uploads/2020/10/2020-10-20-ndip-report.pdf (accessed August 2022).
Hosey M T, Bryce J, Harris P, McHugh S, Campbell C. The behaviour, social status and number of teeth extracted in children under general anaesthesia: A referral centre revisited. Br Dent J 2006; 200: 331-334.
Patel H, Reid C, Wilson K, Girdler N M. Inter-rater agreement between children's self-reported and parents' proxy-reported dental anxiety. Br Dent J 2015; DOI: 10.1038/sj.bdj.2015.98.
Davidson K, Schroth R J, Levi J A, Yaffe A B, Mittermuller B-A, Sellers E A C. Higher body mass index associated with severe early childhood caries. BMC Paediatr 2016; 16: 137.
Camilleri A, Roberts G, Ashley P, Scheer B. Analysis of paediatric dental care provided under general anaesthesia and levels of dental disease in two hospitals. Br Dent J 2004; 196: 219-223.
Kantovitz K R, Pascon F M, Rontani R M P, Gavião M B D. Obesity and dental caries - A systematic review. Oral Health Prev Dent 2006; 4: 137-144.
Tsai C-L, Tsai Y-L, Lin Y-T, Lin Y-T. A retrospective study of dental treatment under general anaesthesia of children with or without a chronic illness and/or a disability. Chang Gung Med J 2006; 29: 412-418.
Sari M E, Ozmen B, Koyuturk A E, Tokay U. A retrospective comparison of dental treatment under general anaesthesia on children with and without mental disabilities. Niger J Clin Pract 2014; 17: 361-365.
Childsmile. Policies and guidelines which form the evidence base for Childsmile. 2022. Available at http://www.child-smile.org.uk/professionals/about-childsmile/evidence.aspx (accessed August 2022).
Acknowledgements
The authors would like to express their sincere gratitude to Steve Turner for his efforts with data statistical analyses.
Author information
Authors and Affiliations
Contributions
Lewis Hua: lead author; data collection; drafting the manuscript; reviewing and editing the manuscript to create the final version; referencing. Antoniella-Busuttil-Naudi: second author; supervisor; conceptualisation; reviewing and editing the manuscript to create the final version. Alex Keightley: third author; supervisor; conceptualisation; reviewing and editing of the manuscript to create the final version.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Ethical approval was gained from the Berkshire Research Ethics Committee (19/SC/0494). For all study participants aged 16 and under, consent was given by their parent or legal guardian. Additionally, the study participants aged eight and above consented to participate in the study and to have their data used as part of the research by completing an assent form.
Rights and permissions
About this article
Cite this article
Hua, L., Busuttil-Naudi, A. & Keightley, A. Do paediatric patient-related factors affect the need for a dental general anaesthetic?. Br Dent J 233, 407–412 (2022). https://doi.org/10.1038/s41415-022-4922-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-4922-2