Key Points
-
Stresses the need for a multidisciplinary approach to the management of patients presenting with hypodontia.
-
Presents the process and benefits of measuring aspects of a clinical service to allow improvements in clinical efficiency to be successfully introduced.
-
Recognises the benefits of using patient feedback on the design and development of a clinical service.
Abstract
Objective To assess the efficiency of the Manchester Hypodontia Clinic (MHC) in improving patient experience and satisfaction.
Setting In January 2010, the University Dental Hospital of Manchester applied a more modern approach to the design of a treatment planning clinic for patients with hypodontia. This brought together all the necessary dental specialties in one multidisciplinary clinic.
Design A questionnaire study of patients attending the MHC between January 2010 and March 2012 was used to monitor each patient's journey through the clinic.
Subjects 400 patients attended the MHC between January 2010 and March 2012.
Method Patient satisfaction was assessed before and after attending the clinic via questionnaires in an attempt to understand more about patient expectations and satisfaction with the structure and management of the clinic.
Results Ninety-nine percent of patients received a clear explanation of why they had been invited to attend the clinic and 98% felt that they had been directly involved in their treatment planning and were fully informed of the decisions made regarding their future treatment. Almost all patients (99%) felt that attending the MHC had been worthwhile. Nearly a third of patients rated their experience as good and over two-thirds of patients (69%) rated their experience as excellent.
Conclusions The results prove that by designing the service around the patients' needs it is possible to run an efficient clinic and achieve high levels of patient satisfaction.
Similar content being viewed by others
Introduction
Hypodontia affects up to 7% of the British population1 and is a common presentation in general dental practice. By definition it is the congenital absence of one or more teeth. The management of hypodontia patients often involves a multidisciplinary approach with involvement from restorative dentistry, orthodontics, oral surgery and paediatric dentistry. This has long been recognised and in 1977 the Eastman Dental Institute, London, founded the multidisciplinary hypodontia clinic, which included specialists and consultants in orthodontics, restorative and paediatric dentistry. Clinics such as these have led to streamlined and comprehensive treatment planning for patients affected by hypodontia. In addition, the hypodontia team from Newcastle Dental Hospital have previously published an excellent series of articles in the British Dental Journal explaining the clinical management of hypodontia patients.2,3,4,5,6
Until recently, such patients attending the University Dental Hospital of Manchester have attended up to five separate consultation appointments in order to determine a comprehensive treatment plan. It is not surprising that this has led to patient confusion and a disjointed patient journey, from initial referral to commencement of and eventual completion of treatment. This in turn has resulted in patient dissatisfaction and a number of complaints.
While training opportunities for colleagues, such as specialist registrars, in the delivery of hypodontia treatment have always existed, there was previously no formal structured training in the equally important diagnostic and treatment planning processes.
It is clear that in the wake of the NHS improvements and publications such as the Darzi report,7 the service being provided was predominantly hospital focused. The hypodontia service was not designed around the patient. There was a distinct need for change and to put the patient back at the heart of the service. In 2010, the Manchester Hypodontia Clinic was formed.
Previous hypodontia service arrangements
Before 2010, patients with hypodontia could be referred to any one of the restorative, orthodontic, oral surgery or paediatric dentistry departments. As orthodontic treatment is frequently required for these patients, an internal referral would be made to an orthodontic colleague. This consultation visit would usually lead to a further appointment, at which photographs, study casts and radiographs would be obtained.
A small number of orthodontic/restorative dentistry joint clinics existed and a hypodontia patient was therefore offered a consultation at one of these joint clinics. When appropriate, treatment proceeded until such point as a final plan regarding restoration of the hypodontic spaces was required. As dental implants are frequently considered for this, a consultation appointment was made at a restorative dentistry/oral surgery joint dental implant clinic.
In total, a patient often attended five consultation appointments before a definitive treatment plan was agreed. The considerable delays in this process and the inevitable confusion created for the patient, the hospital consultants and the referring dentist detracted from the high standards of specialist dental treatment provided.
The Manchester Hypodontia Clinic
The Manchester Hypodontia Clinic (MHC) has at least one consultant representative from each dental speciality present to provide a specialist opinion in order to propose an appropriate and comprehensive treatment plan.
The multidisciplinary clinic design meets the needs of the patient and their families by reducing the number of appointments required and by providing an opportunity for patients to meet with all relevant specialties, so they develop a good understanding of their clinical condition, the treatment required and can share in the decision making process.
Each patient receives a clear and concise treatment plan, avoiding confusion and further time delays. Agreement is reached on what treatment will be provided, when the treatment will be provided, who will provide the treatment at each stage and how the treatment is to be funded. This process is known as 'the Ws'.
The MHC also provides an enviable educational opportunity for colleagues in senior training positions, such as specialty registrars. These colleagues take on clinical leadership roles within the multidisciplinary meetings and are closely involved with each patient's case at the diagnosis and treatment planning stage. Before the development of the MHC, such a specialist trainee would see very few patients at each consultation appointment attended. Since 2010, a specialist registrar will be involved with well over 200 patient cases. With a focus on the management of hypodontia patients, training colleagues now also provide treatment for a large number of patients as part of a comprehensive treatment plan delivered by a well-defined clinical team.
The hypodontia care pathway
Initial referral
Almost all patient journeys commence with referral from their general dental practitioner. This may be directed to any one of the dental specialties. At this initial consultation the patient's needs are assessed and in a small number of cases of mild hypodontia, the treatment outcomes may be fulfilled with single specialty involvement (for example, by a simple restorative dentistry intervention). In these situations it is not usually appropriate for the patient to attend the MHC.
However, those patients more affected by hypodontia will be offered an appointment on the MHC. All have appropriate radiographs, study casts and photographs taken at their initial consultation appointment. The appointment for the MHC is booked and the patient is given written information outlining what to expect at their next visit. This allows patients to familiarise themselves with the process and prepare any questions or concerns they may want to discuss with members of staff.
Pre-clinic multidisciplinary meeting
The pre-clinic Multi-Disciplinary Team (MDT) meeting is held for one hour, immediately before each hypodontia clinic. All staff attending and taking part on the clinic attend this meeting.
The pre-clinic meeting is lead by the speciality registrars, who present each patient attending the clinic, using a case history, photographs, study casts and radiographs. The treatment options are then discussed in depth. The pre-clinic meeting allows all colleagues to familiarise themselves with the patients before their visit and provides focus for the expected joint clinic discussions with the patient and family.
The hypodontia clinic
The MHC is usually held once every calendar month for three hours and is attended by on average sixteen patients. Approximately equal numbers of male and female patients attend. Most patients are between 14 and 24 years of age. The clinic is held in an open plan area with six dental chairs. Each unit has a computer screen for viewing radiographs and photographs to assist in the discussion process.
The clinic is managed by one or more senior nurses, allowing the dental staff to spend more time with patients. Typically the MHC is attended by two orthodontic consultants, two restorative dentistry consultants, one oral surgery consultant, the dental implant service coordinator and a number of dental specialty trainees. The clinical team divides itself between patients and ensures that a small number of clinicians can meet each patient in an efficient and supportive way, without fear of intimidation.
Measuring clinical efficiency
The senior nurse managing the clinic records a data set for each patient both during the MDT and while in the clinic. This provides details of the information available for the MDT: who was involved in meeting the patient and the efficiency of the patient's attendance at the clinic.
Two efficiency objectives of the MHC are to see all patients within 15 minutes of their appointment time and to complete their appointment within 30 minutes of entering the clinic. Two further efficiency objectives are that during each appointment a treatment plan will be agreed with the involvement of all parties and that all letters will be dictated.
After the visit, the patient is either booked for a treatment appointment or have their name added to an appropriate treatment waiting list, if necessary.
Measuring patient satisfaction
Patient satisfaction data is collected using patient questionnaires immediately before and following the appointment.
The purpose of the pre-clinic questionnaire is to ascertain patient expectations of their visit to the MHC. The questionnaire also serves as a method of raising the patients' awareness that a quality improvement process is taking place.
At the end of the appointment, each patient is given a post-clinic questionnaire, aimed at assessing the level of patient satisfaction with the service provided and the outcomes of the clinic.
Results
Clinical efficiency
Four hundred and forty patients were given appointments and a total of 400 patients attended the MHC from January 2010 until March 2012. This was an overall 91% attendance rate with only 7% of patients failing to attend and 2% cancelling and re-appointing. More recent clinics in 2011 and 2012 have had an even higher attendance rate.
Pre-clinic MDT meetings
The clinical records were available 99% of the time, with radiographs (95%), photographs (80%) and study casts (78%) accessible in the majority of cases. The poorer results for the latter three were skewed by the earlier clinics in 2010. More recent clinics in 2011 and 2012 have usually achieved 100% results.
Clinical efficiency
Over half (58%) of the patients were seen either on time or within 15 minutes of their appointment. The results include those patients who arrived late for their appointments. The longest overall appointment delay was 40 minutes, due to the pre-clinic meeting starting late and running over by 20 minutes, thus having the effect of delaying patient appointment times. On occasions when the pre-clinic MDT meeting ran over, the earliest appointments were frequently delayed. Thirty-five percent of the remaining patients were seen within 30 minutes of their appointment time and only 7% of patients were delayed longer than 30 minutes. On no occasions were patients who attended late for their appointments turned away.
Length of appointment
The average time for a patient consultation was 22 minutes with the shortest appointment being 15 minutes and the longest 55 minutes, for a patient who unexpectedly required additional radiographs.
In all of the hypodontia cases referred to the clinic, both an orthodontic and restorative dentistry consultant opinion was sought. In more than half of the cases (58%) an oral surgery opinion was obtained.
In 99% of cases, treatment plans were agreed and 95% of letters were dictated during the appointment. The patient was always subsequently provided with a copy of the correspondence.
Patient satisfaction
Pre-clinic and post-clinic questionnaires are handed to all patients and families on attendance of the appointment. Ninety-one percent of patients returned the pre-clinic questionnaire and 85% returned the post-clinic questionnaire. A small number of post-clinic questionnaires were posted back to the department or hand delivered at a subsequent appointment.
Pre-clinic results
Pre-clinic results were more focused around patient expectations:
-
Eighty-two percent of patients attending the MHC were accompanied by a family member or friend
-
Eighty-three percent of patients were aware why they were attending the Hypodontia Clinic
-
Forty-seven percent of patients were aware of whom they would be meeting and what would be happening.
When asked what they hoped to get out of their appointment, the majority of the comments were focused around two main points. The first being the treatment outcomes and included comments from patients wanting better, straighter, nicer and even perfect teeth. The second commonly desired outcome from the clinic was around treatment timings, patients wanted an idea of when treatment would start and how long treatment would take.
Post-clinic results
Post clinic results were focused on patient satisfaction and experience:
-
One hundred percent of patients said that every member of staff had introduced themselves to them
-
Ninety-nine percent of patients received a clear explanation of why they had been invited to attend the clinic
-
Ninety-eight percent of patients felt that they had been directly involved in their treatment planning
-
Ninety-eight percent of patients felt that they were fully informed of the decisions made regarding their future treatment
-
Almost all patients (99%) felt that attending the MHC had been worthwhile.
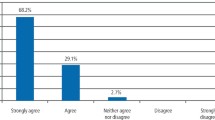
Patients are asked to rate their experience on the clinic, using a scale of:
Very Poor – Poor - Good – Excellent
There were no negative responses recorded. Nearly a third of patients rated their experience as good and over two-thirds of patients (69%) rated their experience as excellent.
When patients were asked after the clinic to comment about their visit, of all the responses recorded only four were negative. These included 'dissatisfaction with the funding restrictions for dental implant treatment' applied to their specific case and to the 'limitations of treatment on the NHS'. The resounding positive comments centred on the 'impressive level of expertise', 'sound explanations of treatment proposals', 'friendliness and helpfulness of staff' and 'the pleasure of being seen on time, with a short appointment'. (See Appendix 1)
Discussion
The structure of the Manchester Hypodontia Clinic has proved highly successful in a number of respects: an efficient clinic; an opportunity for clinicians, patients and families to participate in the treatment planning process; provision of enviable training opportunities for all staff and the opportunity for colleagues from several specialties to regularly work closely together. This is clearly reflected in post-clinic questionnaires in which the patients felt fully engaged with the dental team and felt able to make informed decisions about their treatment. A resounding majority (99%) of the patients attending the clinic found it worthwhile.
Communication of information and transparency are central to running a patient-centred service. By asking patients before attending the clinic what their expectations are, the team obtains an insight into what kind of service they need to be delivering and what information should be communicated before and during the clinic in order to manage these expectations appropriately. Despite all the efforts of the staff to verbally inform patients regarding the clinic and the written information given at referral to the MHC, rather interestingly nearly a third of patients still stated that they were not aware why they attending the clinic, who they would be seeing and what would be happening. This highlights the importance of not only giving patients written and verbal information but also ensuring that information has been conveyed in a form understandable to the layperson. In spite of this though, the MHC has a 91% attendance record, an indication that the team has effectively emphasised the importance of attendance in their communication with the patient.
The MHC may appear to be a financially expensive method for seeing only sixteen patients, with five consultants and usually seven other clinicians working for the entire session. The average appointment length of 22 minutes is only comparable with attendance at most other outpatient clinics. However, the design of the hypodontia care pathway, with only one initial appointment and one attendance at the MHC for each patient, significantly reduces both the number of appointments required and the total time spent by the patient at the hospital. At worst, the cost implications of having so many senior staff at each MHC are comparable to the total costs of the patient meeting the same senior staff at individual clinic appointments. However, the additional costs that were incurred by each other clinic provide the cost savings delivered by the current MHC care pathway.
Conclusion
Patients rightly expect a good outcome when receiving clinical treatment. A modern, patient-centred service aims to deliver high standards of clinical treatment in a manner that patients appreciate. The Manchester Hypodontia Clinic care pathway focuses on courtesy, punctuality, information sharing, efficiency and teamwork to deliver a service that surpasses both patient expectations and what has been possible in traditional service models.
References
Brook A H . Dental anomalies of number, form and size: their prevalence in British schoolchildren. J Int Assoc Dent Child 1974; 5: 37–53.
Nunn J H, Carter N E, Gillgrass T J et al. The interdisciplinary management of hypodontia: background and role of paediatric dentistry. Br Dent J 2003; 194: 245–251.
Jepson N J, Nohl F S, Carter N E et al. The interdisciplinary management of hypodontia: restorative dentistry. Br Dent Journal 2003; 194: 299–304.
Carter N E, Gillgrass T J, Hobson R S et al. The interdisciplinary management of hypodontia: orthodontics. Br Dent J 2003; 194: 361–366.
Meechan J G, Carter N E, Gillgrass T J et al. The interdisciplinary management of hypodontia: oral surgery. Br Dent J 2003; 194: 423–427.
Hobson R S, Carter N E, Gillgrass T J et al. The interdisciplinary management of hypodontia: the relationship between an interdisciplinary team and the general dental practitioner. Br Dent J 2003; 194: 479–482.
Denham D KBE . High quality care for all: NHS next stage review final report. London: Crown Copyright, 2008. Online report available at http://www.dh.gov.uk/en/Publicationsandstatistics/Publications /PublicationsPolicyAndGuidance/DH_085825 (accessed February 2013).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Tams, C., Ashley, M. Improving patient experience in a multi-disciplinary clinic: clinical efficiency and patient satisfaction of 400 patients attending the Manchester Hypodontia Clinic. Br Dent J 214, E11 (2013). https://doi.org/10.1038/sj.bdj.2013.220
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.220
This article is cited by
-
A service evaluation of the multidisciplinary team approach to hypodontia
British Dental Journal (2023)
-
The interdisciplinary management of hypodontia patients in the UK: a national service evaluation
British Dental Journal (2017)
-
Patient and parent satisfaction following autotransplantation and associated orthodontic treatment delivered by an interdisciplinary team
European Archives of Paediatric Dentistry (2014)