Key Points
-
Dental amalgam continues to be used widely for the restoration of posterior teeth.
-
Rubber dam, despite it considerable advantages, is not used routinely.
-
Tooth whitening and bleaching procedures are frequently prescribed.
Abstract
Objective To investigate, by postal questionnaire, aspects of the selection and use of direct restorative materials, endodontic techniques and approaches to bleaching by general dental practitioners in the UK, and to compare and contrast the findings with those of a related study reported in 2004.
Methods A questionnaire comprising 18 questions, each of a number of elements, was sent to 1,000 general dental practitioners in the UK, selected at random from the Dentists Register. Non-responders were sent a second copy of the questionnaire after a period of four weeks had elapsed.
Results A total of 662 useable responses were returned, giving a response rate of 66%. Key findings included: dental amalgam was found to be the most commonly used material in the restoration of occlusoproximal cavities in premolar (59% of respondents) and molar teeth (75% of respondents); glass-ionomer cements and related materials were applied extensively in the restoration of deciduous molars (81% of respondents) and for the luting of indirect restorations (67% of respondents); the use of rubber dam was limited, in particular as an adjunct to procedures in operative dentistry (18% of respondents); relatively few respondents used preformed stainless steel crowns, and among the users only occasionally in the restoration of deciduous molars (23%); and bleaching, predominantly home-based (nightguard) vital bleaching (81% of respondents) was widely practised.
Conclusion It is concluded that, for the practitioners surveyed, factors other than best available evidence influenced various aspects of the use of direct restorative materials and the clinical practice of endodontics. As a consequence, many of the features of general dental practice revealed in the process of the investigation were at variance with teaching in dental schools. Bleaching, in particular home-based (nightguard), vital bleaching, was provided by >80% of respondents, indicating widespread interest among patients in enhanced dental attractiveness.
Similar content being viewed by others
Introduction
This is one of three papers reporting the findings of an investigation designed to provide a profile of everyday aspects of contemporary general dental practice in the UK. This investigation was undertaken five years after a survey with similar aims to the present study.1,2,3 The first of the current series of papers reported on demographic data and practising arrangements.4 The third paper will report the findings of the survey pertaining to indirect restorations and fixed prosthodontics. The present paper deals primarily with aspects of direct restorations of different materials, endodontics and bleaching in general dental practice.
Regarding the previous study reported in 2004,1,2,3 it was concluded for the practitioners surveyed that dental amalgam was the most frequently selected direct restorative material; few practitioners used amalgam bonding, let alone direct resin composites for posterior restorations. Home-based rather than practice-based bleaching procedures were preferred, and traditional endodontic techniques tended to be applied in preference to new, emerging endodontic techniques at that time. In addition, it was noted that there was an apparent gulf between what was considered at that time to be evidence-based (best) practice, as taught in dental schools, and approaches adopted in general dental practice. This led to a series of questions: is it any wonder that new graduates continue to find it challenging to make the transition from undergraduate dental student to vocational dental practitioner, let alone independent practice? Are third party rules and regulations for remuneration a barrier to evidence-based practice? Do evidence-based methodologies rely too heavily on the outcome of research conducted in environments other than general dental practice where most patients are treated? And, how could the apparent gulf be closed? Part of the purpose of the present investigation was to ascertain whether these questions are as pertinent today as they were in 2004.
Methods
A questionnaire, comprising 18 questions, each of a number of elements, was sent to 1,000 general dental practitioners in the UK, selected at random from the Dentists Register. Non-responders were sent a second copy of the questionnaire after a period of four weeks had elapsed.
The data obtained from the completed questionnaires (66%; n = 662) was analysed using Minitab (version 15, Minitab Inc.) and StatXact (version 8, Cytel Inc.). Summary statistics including cross tabulations were obtained and, where appropriate, nonparametric tests, including Mann Whitney and Kruskal Wallis were performed. The level of significance was set at p <0.01.
Results
A total of 662 usable, completed questionnaires were returned. Demographic details of the respondents have been reported in the first of the three papers in the present series.4
Restorative materials – posterior teeth
When questioned as to the most commonly used material in the restoration of occlusoproximal cavities in premolar and permanent molar teeth, the respondents indicated that amalgam continues to predominate – premolars 59% (n = 381), permanent molars 75% (n = 484). Regarding the use of composites as the most common direct restorative material for the restoration of occlusoproximal cavities, this was the preference of 199 (40%) of the respondents in respect of premolars, and 97 (15%) of the respondents for permanent molar teeth.
When commenting on their attitude towards the use of dental amalgam, 75% (n = 484) of respondents indicated that amalgam should continue to be used, with 19% (n = 121) of the respondents being undecided on this issue.
Thirty-four percent of respondents (n = 217) reported that they bonded amalgams in certain situations. Of the respondents who did not use amalgam bonding (66%; n = 427), 64% (n = 262) were not convinced as to the need for this procedure, with a small minority of respondents indicating that amalgam bonding was too time-consuming (6%; n = 26) or too expensive (5%; n = 19). Eight percent (n = 32) of the respondents appeared to have found the question on amalgam bonding irrelevant to their clinical practice, as they simply ticked the option 'not covered by third party payment'.
The factors influencing the respondents' decisions as to which material to use in the restoration of an occlusoproximal cavity were as follows: durability 21% (n = 136); patient preference 12% (n = 79); need to withstand occlusal loading 11% (n = 71); aesthetics 4% (n = 26); and concern about mercury toxicity 1% (n = 6). A further 50% (n = 322) selected the 'other' option, with a number specifying 'cost of material'.
Glass-ionomer cements
Glass-ionomer cements (GICs) were found to be used most commonly in the treatment of adult patients for the luting of indirect restorations (67%; n = 455). Only 64% (n = 421) of the respondents found applications for GICs and related materials in the restoration of permanent teeth. Regarding the use of GICs for linings and bases, this was limited to 54% (n = 359) and 51% (n = 334) of the respondents respectively.
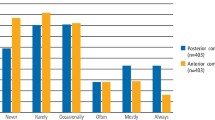
Bleaching
Eighty-one percent (n = 533) of the respondents indicated that they provided home-based (nightguard) vital bleaching, and 32% (n = 208) indicated that they provided practice-based bleaching. More of the practitioners reporting the use of home-based vital bleaching indicated being satisfied with the clinical outcomes (99%; n = 523) than those reporting the use of practice-based bleaching (82%; n = 172). The findings pertaining to experience of side effects with bleaching are set out in Table 1.
Endodontics
Regarding endodontics, it was found that only 78% (n = 512) of the respondents considered root canal therapy to be 'safe', ie not liable to cause harm, with 14% (n = 94) of the respondents indicating that they were beginning to question the sufficiency of traditional root canal procedures. Cold lateral condensation obturation techniques predominated (65%; n = 427); warm lateral condensation techniques were preferred by 16% of respondents (n = 106). Thirty-two percent of respondents (n = 208) reported using reamers, rather than files or rotary instruments, for root canal shaping.
Rubber dam
Twenty-nine percent (n = 191) of respondents indicated that they did not use rubber dam. Sixty-five percent (n = 432) used rubber dam for endodontic treatments, 18% (n = 121) in the provision of operative dentistry and 14% (n = 94) for practice-based bleaching.
Paediatric dentistry
Two questions in relation to the restorative aspects of paediatric dentistry were asked. These revealed that 70% (n = 462) of the respondents never used preformed metal crowns (PMCs) in the restoration of deciduous molars, with a further 23% (n = 150) indicating that they used such crowns but only occasionally. Regarding the most commonly used materials for the restoration of occlusoproximal cavities in deciduous molars, GICs were preferred by 56% (n = 358) of the respondents, with compomers and resin-modified GICs being used by a further 11% (n = 69) and 14% (n = 87) of the respondents respectively. Amalgam was selected by only 15% (n = 96) of the respondents. Regarding the use of rubber dam for fissure sealants, only 5% (n = 34) of the 284 (43%) respondents who applied fissure sealants indicated using rubber dam for moisture isolation.
Discussion
Given the scope of the present investigation, spanning preferences and arrangements across the spectrum of the clinical practice of dentistry, it was considered counterproductive in terms of the response rate and in turn, the value of the findings, to ask multiple supplemental questions to ascertain reasons for preferences and attitudes. It is suggested, however, that further understanding and insight into preferred attitudes and arrangements would be of considerable value, if for no other reason than the targeting of continuing professional development programmes to address approaches to aspects of clinical practice which are either outdated or worse, recognised to be contrary to the best interests of patients. Such further understanding and insight could be obtained through further surveying or alternative means, including methodologies involving focus groups.
Restorative materials – posterior teeth
Contrary to teaching in dental schools as reported before the survey,5 the findings indicated that amalgam continued to be the direct restorative material of choice for the restoration of most occlusoproximal cavities. Yet it would appear that there had been a shift in preference in favour of composite materials, with the percentages of respondents in the previous study preferring to use amalgams in the restoration of occlusoproximal cavities in premolars and molars being 86% and 90% respectively, compared to 59% and 75% in the present investigation. This shift, while not insubstantial, could be considered to be disappointing given the increasing evidence base to justify the use of composites in the restoration of posterior teeth in clinical practice, including posterior teeth with large cavities,6,7 let alone the widely recognised advantages of minimally interventive techniques which negate the need for mechanical resistance and retention forms, with the resultant substantial weakening of remaining tooth structures.8
Given the above, it came as no surprise that 75% (n = 484) of the respondents indicated that amalgam should continue to be used. Interestingly, however, the corresponding figure in the previous investigation was 60%, despite the higher percentage preference findings for the use of amalgam recorded at that time. These findings are considered to indicate that practitioners were using composites more than five years ago for the restoration of posterior teeth, and that amalgam has a continuing role to play in operative dentistry as provided in general practice.
Thirty-four percent of respondents (n = 217) indicated that they bonded amalgams in certain situations. Of those who did not use amalgam bonding (66%; n = 427), 64% (n = 262) could not see the need for this procedure, with a small minority of respondents indicating that amalgam bonding was too time-consuming (6%; n = 26) or too expensive (5%; n = 19). Eight percent (n = 32) of the respondents would appear to have found the question on amalgam bonding irrelevant as they simply ticked the option 'not covered by third party payment'. Given the lack of evidence in respect of the benefits of bonding restorations of amalgam,9 it was somewhat unexpected that 217 (34%) of the respondents found any application for this procedure in particular, given that it is time consuming and therefore relatively costly to apply. That said, it is acknowledged that there is relatively little good quality evidence in respect of the efficacy of amalgam bonding,9 particularly pertaining to perceived benefits such as reduction in postoperative sensitivity.
Factors influencing the decision as to which material to use for restoring an occlusoproximal cavity were as follows: durability 21% (n = 136), patient preference 12% (n = 79), ability to withstand occlusal loading 11% (n = 71), aesthetics 4% (n = 26) and concern about mercury toxicity 1% (n = 6). In all cases, the influence of these factors was substantially reduced relative to the findings from the previous investigation: durability 56%, patient preference 50%, ability to withstand occlusal loading 45%, aesthetics 34% and concerns in respect of mercury toxicity 9%; however, a greater increased proportion of respondents selected 'other' factors. These 'other' factors were typically a combination of the influencing factors, for example aesthetic preferences and ability to withstand loading, indicating a greater appreciation of the multifactorial nature of the performance of restorative materials in clinical service than had been the case previously. Cost of material was identified as a factor by some, while others cited size and, in some cases, depth of preparation was an important factor. Given the cost of the material used is typically a very small proportion of the overall cost of a procedure, it could be considered disappointing that this factor may be influencing key clinical decisions in terms of the subsequent cost of maintaining a tooth over the lifetime of the patient.
Glass-ionomer cements
The finding that GICs were found to have a principal application in the luting of indirect restorations mirrored the corresponding finding in the previous study (67% of respondents vs 68% of respondents). Similarly, only 64% (n = 421) of respondents found applications for GICs in the restoration of permanent teeth. This compared with 60% of respondents in the previous study. The use of GICs for liners and bases showed some change since the time of the previous study (52% compared to 47%), indicating that traditional approaches to the protection of operatively exposed dentine continue to be widely practised.
Irrespective of one's views on the attributes and clinical performance of GICs and related materials, in the absence of high quality objective data, the findings could be viewed as surprising. Surprisingly positive in certain respects and surprisingly negative in others, showing little, if any change in the time between the two investigations, despite important developments to the materials. Notwithstanding such considerations, GICs and related materials are clearly considered to have a place in general dental practice. However, their importance would not appear to be increasing and may even have plateaued. In this respect, it is of interest to note the findings of a previous study of glass-ionomer use in England and Wales.10 When the data were analysed to ascertain what material was used when a glass-ionomer restoration failed, it was apparent that glass-ionomer was re-used in only 30% of cases, whereas the corresponding figures for resin composites and amalgam were in the order of 60%. The authors took this to indicate a certain lack of 'faith' by practitioners in glass-ionomer materials. This may go some way to explain the lack of growth in the use of glass-ionomer restorative materials identified in the present work.
Bleaching
Despite the continuing regulatory uncertainties over the use of bleaching systems for so-called 'tooth whitening', it would appear that the application of bleaching techniques, both home- and practice-based, has greatly increased in the UK in recent years, given that in the present study 81% of respondents indicated that they used home-based bleaching compared with 35% in the previous study. The corresponding figures for practice-based bleaching techniques were 35% and 18%.
Regarding the side effects experienced with bleaching, as set out in Table 1, these findings, in comparison to those obtained in the previous study (Table 2) indicate an increase in the percentage of practitioners experiencing soft tissue inflammation with practice-based bleaching (40% vs 21%), and tooth sensitivity with both techniques, especially with practice-based bleaching (77% vs 33%). It is speculated that this increase, which could reflect different levels of awareness and reporting, may be related to developments in practice-based bleaching to reduce chairside time and increase the immediate lightening ('whitening') effect. The provision of bleaching by >80% of the respondents is considered to be an indication of widespread interest in enhanced dental attractiveness. As such, practitioners and students must understand the mechanisms, applications and pitfalls of the relevant techniques.11
Endodontics
As in the previous study, around three quarters of the respondents only considered root canal therapy to be safe (78%) with a sizeable minority of respondents (14%) having certain issues in respect of the sufficiency of standard root canal procedures. As discussed in the report of the previous study, having approximately 25% of practitioners questioning the safety of root canal therapy and approximately 15% concerned about the sufficiency of widely used techniques should be considered cause for concern. The lack of moisture control is a well known cause of failure of endodontic treatments.12 Practitioners undertaking endodontic procedures without the use of the rubber dam (45% of the respondents) therefore are likely to experience suboptimal success rates and this might result in the lack of confidence in the safety of endodontic procedures shown by a surprisingly high number of dentists. Such findings are considered to demonstrate the ways in which studies of the present type may reveal aspects of dental practice worthy of more detailed research and more emphasis in continuing professional development programmes.
A further aspect of the findings in respect of endodontics, which was considered to be cause for concern, was the finding that 32% (n = 208) of respondents still used reamers for root canal shaping.
Rubber dam
The relatively limited use of rubber dam, in particular for endodontic treatments – only 65% of respondents, with 30% of respondents having indicated that they did not use rubber dam for any procedures, could be viewed as a real risk to patients, let alone a factor which could limit the success of endodontics in clinical practice in the UK. This, however, is almost an identical finding to one reported from a recent USA dental practice-based research network investigation in which 63% of dental practitioners did not use a rubber dam for any operative dentistry procedures.13 In this investigation the most common reasons for not using a rubber dam were 'inconvenience' and the perception that it was not necessary. Time and costs were not major reasons for the lack of use of rubber dam – the time saved by securing a clear, dry field with good visibility was considered to compensate for the time spent applying a rubber dam.14 In relation to the lack of use of rubber dam in endodontics, considering the risk for the patient of inhalation and ingestion of root canal instruments,15 strict guidelines should be issued by all relevant standard setting and where appropriate, regulatory bodies, with full compliance across the spectrum of clinical practice.
Paediatric dentistry
Regarding the findings pertaining to paediatric dentistry, relatively little would appear to have changed since the time of the previous study, with the majority of respondents indicating, contrary to best available evidence,16 that they never used preformed metal (stainless steel)- PMC crowns- in the restoration of deciduous molar teeth (70% compared with 84% in the previous study). Also, the most commonly used materials for the restoration of occlusoproximal cavities in deciduous molars were GICs (56% compared with 55% in the previous study), with compomers and resin-modified GICs being selected by a further 11% (n = 69) and 14% (n = 87) of the respondents respectively. Dental amalgam was selected by only 15% (n = 96) of the respondents, the corresponding figure in the previous study having been 14% (n = 96). The limited use of amalgam together with the relatively widespread use of GICs and related materials when practising paediatric dentistry is in sharp contrast to the popularity of amalgam and relatively limited use of GICs in the restoration of permanent molar teeth. These findings could be interpreted to indicate that some of the most important factors in the selection of direct restorative materials are ease and speed of use, rather than best available evidence – expedience over efficacy. A limitation of the present study, in terms of understanding the selection of restorative materials, was that dentists were not asked whether they were comfortable to routinely administer local anaesthesia to children. The present study demonstrates, however, that UK dentists are willing to attempt to stabilise caries in children and perhaps acknowledge the fluoride releasing effect of glass-ionomer materials. This is considered important given that dentinal caries in children, although possibly plateaued at 40% for under 5-year-olds, remains a challenge in the clinical practice of dentistry. The possible benefits of alternative techniques (that do not require local anaesthesia but which combine the effect of GICs with the longevity of preformed metal crowns) such as the 'Hall' technique17 did not appear to have been realised by the respondents at the time of the survey.
Conclusions
It is concluded that, for the practitioners surveyed, factors other than best available evidence influenced various aspects of the use of direct restorative materials and the clinical practice of endodontics. These factors could be found to include ease of use and cost. As a consequence of factors other than best evidence influencing various aspects of dental practice, there are differences between teaching in dental schools and what occurs in clinical practice. Such differences, apart from being educationally unhelpful, are not considered to be in the best interests of patients, particularly when preferred materials, instruments and techniques have been shown to be associated with suboptimal clinical outcomes.
Bleaching, in particular bleaching of the home-based (nightguard), vital variety is widely applied, indicating that so-called 'tooth whitening' is a firmly established feature of everyday clinical practice, and that there is widespread interest in enhanced dental attractiveness.
It is suggested that studies of the type reported highlight topics for both further research and targeted continuing professional development.
References
Burke F J, Wilson N H, Christensen G J, Cheung S W, Brunton P A. Contemporary dental practice in the UK: demographic data and practising arrangements. Br Dent J 2005; 198: 39–43.
Wilson N H, Christensen G J, Cheung S W, Burke F J, Brunton P A. Contemporary dental practice in the UK: aspects of direct restorations, endodontics and bleaching. Br Dent J 2004; 197: 753–756.
Brunton P A, Christensen G J, Cheung S W, Burke F J, Wilson N H. Contemporary dental practice in the UK: indirect restorations and fixed prosthodontics. Br Dent J 2005; 198: 99–130.
Brunton P A, Burke T, Shariff M O, Muirhead E K, Creanor S, Wilson N H F. Contemporary dental practice in the UK: demographic details and practising arrangements in 2008. Br Dent J 2012; 212: 11–15.
Lynch C D, McConnell R J, Wilson N H. Challenges to teaching posterior composites in the United Kingdom and Ireland. Br Dent J 2006; 201: 747–750.
Lynch C D. Successful posterior composites. London: Quintessence, 2008
Opdam N J, Bronkhorst E M, Loomans B A, Huysmons M C. DNJM 12-year survival of composite vs amalgam restorations. J Dent Res 2010; 89: 1063–1067.
Van Amerongen J P, Davidson C L, Opdam J J M, Roeters F J M, Kidd E A M. Restoring the tooth: 'the seal is the deal'. In Fejerskov O, Kidd E A M (eds) Dental caries. The disease and its clinical management. pp 385–425. Oxford: Blackwell Munksgaard, 2008.
Fedorowicz Z, Nasser M, Wilson N H. Adhesively bonded versus non-bonded amalgam restorations for dental caries. Cochrane Database Syst Rev. 2009; 4. Online article available at http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD007517/frame.html.
Burke F J, Lucarotti P S. Re-intervention in glass ionomer restorations: what comes next? J Dent 2009; 37: 39–43.
Kelleher M. Dental bleaching. London: Quintessence, 2007.
Chandra A. Discuss the factors that affect the outcome of endodontic treatment. Aust Endod J 2009; 35: 98–107.
Gilbert G H, Litaker M S, Pihlstrom D J, Amundson C W, Gordan W, DPBRN Collaborative Group. Rubber dam use during routine operative dentistry procedures: findings from the Dental PBRN. Oper Dent 2010; 35: 491–499.
Knight G T, Berry T G, Borghi N, Burns T R. Effects of two methods of moisture control on marginal microleakage between resin composite and etched enamel: a clinical study. Int J Prosthodont 1993; 6: 475–479.
Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J 2007; 40: 585–589.
Randall R C, Vrijhoef M M, Wilson N H. Efficacy of preformed metal crowns in amalgam restorations in primary molars: a systematic review. J Am Dent Assoc 2000; 131: 337–343.
Innes N P, Stirrups D R, Evans D J, Hall N, Leggate M. A novel technique using preformed metal crowns for managing carious primary molars in general practice-a retrospective analysis. Br Dent J 2006; 200: 451–454.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Brunton, P., Burke, F., Sharif, M. et al. Contemporary dental practice in the UK in 2008: aspects of direct restorations, endodontics and bleaching. Br Dent J 212, 63–67 (2012). https://doi.org/10.1038/sj.bdj.2012.46
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.46
This article is cited by
-
Dental amalgam teaching phase-out - a step too soon? Foundation trainees' experience of amalgam use in dental school compared to practice: a mixed-methods survey
British Dental Journal (2023)
-
Dental practice in the UK in 2015/2016. Part 2: aspects of direct restorations, bleaching, endodontics and paediatric dentistry
British Dental Journal (2019)
-
Dental practice in the UK in 2015/2016. Part 4: changes since 2002?
British Dental Journal (2019)
-
The ultimate guide to restoration longevity in England and Wales. Part 2: Amalgam restorations – time to next intervention and to extraction of the restored tooth
British Dental Journal (2018)
-
No more amalgams: Use of amalgam and amalgam alternative materials in primary dental care
British Dental Journal (2018)