Abstract
Autonomic dysreflexia is a medical emergency in spinal cord injury. Majority of cases of autonomic dysreflexia are known to be induced by either bladder or bowel distension. Very few cases of recurrent postural autonomic dysreflexia, due to secondary spinal pathology, have been reported. Discovertebral or Andersson lesion, a recognized complication in Ankylosing Spondylitis, can give rise to similar kind of recurrent postural dysreflexic symptoms. Here, we report a case of Ankylosing Spondylitis with high level, complete spinal cord injury, where the patient was developing recurrent postural autonomic dysreflexia and its successful management. Andersson lesion in the lumbar spine below the level of injury was demonstrated in this case report.
Similar content being viewed by others
Introduction
Autonomic dysreflexia (AD) is an acute and potentially life threatening syndrome in persons with spinal cord injury (SCI) with lesions at or above sixth thoracic level.1,2
It is characterized by bilateral pounding headache, facial flushing, nasal congestion, piloerection, malaise, nausea and sweating above the level of lesion, whereas cool, pale skin below the level of lesion.1–3 Paroxysmal hypertension is commonly associated with reflex bradycardia, although tachycardia is not rare.4
Ankylosing spondylitis (AS), an idiopathic chronic inflammatory disease, primarily affects the spine and sacroiliac joints, causing pain, stiffness and a progressive thoracolumbar kyphotic deformity.5 Discovertebral or Andersson Lesion (AL) is a recognized complication in AS. It is a destructive discovertebral lesion, which occurs transversely through the disc space and or the vertebral body of a spinal segment. The presence of a posterior element defect from either a fracture or unfused facet joint is an essential component in the development of AL. The AL is revealed by osteolytic destruction with a surrounding zone of reactive sclerosis and vertebral osteophytes.6
AD is frequently associated with bladder or bowel distension, urinary tract infection, pressure sore, hemorrhoid, anal fissure, paronychia or it can be triggered by any activation of pain receptors below the level of injury.7–9 Here we present a case report of a patient with AS with complete high SCI, developed AD, triggered by AL in ankylosed lumbar spine and her rehabilitation perspectives. This is the only case report of a person with AS with tetraplegia, who developed AD, induced by AL.
Case report
A 36-year-old lady, known case of AS for 8 years, was suffering from traumatic tetraplegia for 3 years. She had a history of a fall from steps during stair climbing, and after that she was diagnosed to have C6 Complete American Spinal Injury Association A (ASIA A) tetraplegia. She presented to the Department of Physical Medicine & Rehabilitation with complaints of recurrent episodes of increased sweating, severe headache and very high blood pressure during position change for last 5 months besides of having stiffness of neck, weakness of lower limbs, spasticity, impaired sensations in all four limbs and impaired bladder-bowel control following spine surgery 3 years ago. She had been diagnosed with AS at the age of 28 years based on clinical, pathological and radiological findings.
Historically, she had inflammatory back pain and stiffness of neck since 28 years of age. She was very active and completely independent until she sustained a neck injury at 33 years of age. She underwent decompression and cervico-thoracic stabilization surgery with C3-D1 contoured rods 1 day after trauma. After 4 weeks of surgery, she received comprehensive rehabilitation training including wheel chair, activities of daily living training and bowel-bladder training. She was apparently well for the initial two and half years, but after that she started developing recurrent episodes of hot flush, headache and dizziness during position change and sitting position. Blood pressure at that moment was going more than 210/120 mm Hg with heart rate 90 per minute. The symptoms were getting relieved within 15–20 min after she was made to lie down in supine position. Blood pressure measurement in supine position was 80/56 mm Hg, with heart rate 80 per minute. During last 6 months, she had visited several hospitals. she stopped sitting and mobilizing in wheel chair. Although she was diagnosed of having AD, cause of AD remained uncertain and could not be managed successfully. Her symptoms continued and frequencies of high blood pressure were increasing day by day.
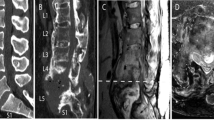
At the time of admission in our center, she was completely bed bound and she was on indwelling catheter. There was no catheter block. During sitting position or any posture change blood pressure went up to 300/150 mm Hg. Her detailed evaluation was done and was found to have following parameters. White blood cells: 7100 per μl, C-reactive protein: positive, erythrocyte sedimentation rate 50 mm h−1. Urine culture showed catheter-related asymptomatic urinary tract infection. Ultrasound abdomen was normal. Her bowel habit was regular, she was practicing attendant digital stimulation and regularly receiving Dulcolax suppository. She did not have any pressure sore, paronychia, anal fissure or hemorrhoids. Her cardiac evaluation (electrocardiogram and echocardiogram) was normal. Her episodes of AD were persisting even after treating asymptomatic bacteruria. Radiographs of thoracolumbar spinal region revealed ankylosed spine with obvious transverse fracture through L3 vertebral body, pedicle and spinous process. Magnetic resonance imaging was not done in view of spinal instrumentation. Computed tomography of lumbar spine (Figure 1) revealed transverse fracture of L3 vertebra including posterior element and marked spinal cord compression along with major ligamentous ossification around the lumbar region. Dual-energy x-ray absorptiometry (DEXA) scan was done, which showed severe osteoporotic lumbar spine. X-ray pelvis showed bilateral sacroilitis. There was no fracture in pelvis or hip joints.
Neurosurgery opinion was taken regarding any surgical intervention for the new onset L3 fracture (AL), but they decided not to operate in view of severe osteoporotic and ankylosed spine. Hence, she was planned for conservative management. She was given bed rest for 4 weeks in view of unstable spine, although she was continued breathing exercises, stretching, range of motion exercises, strengthening exercises for upper limbs and hand function training. She was started on non-steroidal anti-inflammatory drugs (NSAIDs; Indomethacin 75 mg per day). She was already on anti-spastic medications (Baclofen 60 mg per day and Tizanidine 6 mg per day). After starting NSAIDs, and giving her bed rest, her frequency of AD was gradually coming down. She was also given oral vitamin D and calcium and single-injection Zolendronic Acid in view of severe osteoporosis. After 4 weeks of starting conservative management, frequency of AD had significantly come down, maximum one episode per day during position change, and her blood pressure was not going beyond 150/100 mm Hg. She was started on tilt table as part of gradual ambulation training. She was asymptomatic even after tilting in 70°. Bladder management by indwelling catheter was continued as she was still having occasional AD and L3 vertebral fracture. Bowel management was continued with high-fiber diet and attendant digital rectal stimulation. Neuropsychological evaluation and psychological counseling was done on regular basis to monitor her psychological health. She was planned for another 4 weeks rehabilitation training, but she decided to go home and come back later for further training. At the time of discharge, she was very happy and she got back her confidence.
Discussion
Andersson, in 1937, first described the development of a localized vertebral or discovertebral lesions of the well developed complete ankylosed spine.6 These localized discovertebral lesions of the spine, ‘ALs’ are also known as ‘destructive vertebral lesions’, pseudoarthrosis’ or ‘(stress-) fracture’.6 The reported prevalence of AL or discovertebral lesions complicating AS, ranges from 1.5% to over 28%. AL is most commonly found in middle-aged patient population (63–86%) with long-standing AS. Bron et al.6 pointed out that AL can be either transdiscal or transvertebral, and is usually accompanied by fractures or non-fusion of the posterior elements of the spine. Extensive AL/ pseudoarthrosis develop due to both active inflammation and mechanical factors (trauma/ stress).6
Studies have found that ~50% the patient population with AS are osteoporotic. It is evident from literature that the osteoporotic, ankylosed spine in AS patients is prone to develop spinal fractures owing to the altered biomechanics of the ankylosed spine. It has been reported that AL may occur during every course of the disease.6
AD is more commonly found with complete and higher level SCI. The incidence of AD ranges from 48 to 83% in persons with SCI, with injuries above the major splanchnic outflow in response to noxious stimuli below the level of the lesion.1,2,10 Although the precise mechanisms have not been fully understood, the loss of the descending central sympathetic inhibitory activity has been implicated as a possible contributing factor.10 It is well documented that any afferent painful stimuli below the lesion may induce an AD reaction.11 In our case, we searched extensively for common triggering factors, including hollow organ distension and infection foci in areas such as the urinary tract, lung and skin but we did not find any abnormalities. In most situations, the episode of AD often resolves very quickly, once the patients’ head rise from the bed and remove the noxious stimuli. But in our case, our patient was suffering from hypertension and profuse sweating, whenever she was in an upright position. Several case reports2,4,10 have already illustrated that instability of spine or pelvis may trigger postural AD. Charcot spine, second spinal fracture below the neurological level of injury (NLI) or unstable pelvis may manifest this kind of dysreflexic symptoms.2,4,9,10 Then we suspected spine /or pelvis might be the culprit for AD. The computed tomography scan of the spine did reveal the characteristic pattern AL of the Ankylosed spine. As AD induced by postural change was its feature and blood pressure was increasing with manual compression of the L2 /L3 vertebra, we confirmed that unstable spine due to AL to be the most likely cause of our patient’s AD.
Literatures6,12,13 have found that repeated stress itself may lead to a fracture thoracolumbar junction, the levels proximal to the lumbosacral junction of the ankylosed spine. The thoracolumbar and lumbar spines have disc spaces most susceptible to shearing or distraction under the effect of gravity in the kyphotic spine.6 In our case, she developed AL due to both active inflammation and repeated stress on lumbar spine due to continuous sitting in wheel chair even with severe abdominal and lower limb spasticity. However, it is very important to differentiate spinal fracture complicating AS from infectious spondylilitis, especially in tuberculosis-prevalent areas like India. Radiologically L3 vertebral fracture involving posterior column and the different morphology of anterior longitudinal ligament are characteristic of AL. Besides that, the repetitive negative results of smear test as well as Mycobacterium and bacteria culture might exclude the diagnosis of infectious etiology.4 Spinal instability may exert pressure on the presacral plexus of nerves and retroperitoneal viscera and may induce the dysreflexic reaction.1,14 In our case, we explain that probable displacement of L3 spine during posture change might have exerted a traction effect on the preganglionic fibers of sympathetic nervous system, producing the noxious stimulus. Besides that, recent onset local inflammatory reaction in front of lumbar spine might have irritated the sympathetic trunk through afferent or efferent fibers. As soon as she was lying down, this instability or traction effect was lessened and the dysreflexia was alleviated.4 In our case, exercise training in the upright position was postponed due to AD reactions.
AD is a medical emergency, should be managed quickly and successfully, otherwise it can arise complications like stroke, seizure, cardiac arrhythmias and death.3,15–17 Therefore, the immediate diagnosis and quick treatment of AD are paramount for all medical professionals involved in the care of SCI patients. Most of the reported cases2,4,14 had benefited from surgical intervention for underlying pathologies, such as decompression and stabilization of the unstable vertebra. However, Selmi et al.,9 reported two patients with AD, caused by Charcot spine, successfully managed with conservative management (6–8 weeks of bed rest). In our case, as she was not willing for surgery, we decided for conservative management. As AL occurs due to inflammatory mechanism and stress, we decided to control local inflammation by NSAIDs and give her bed rest. It is already evident from the literature that during the active phases of the disease forms, NSAIDs are the mainstay of the pharmacological management of AS. Although rigorous spinal exercise program is advocated in the treatment of AS, is contraindicated in patients with AL complicating AS. In our case, we managed our patient successfully with high doses of NSAIDs and with bed rest. Our patient progressed steadily throughout her rehabilitative course despite few episodes of AD. Although she had lumbar fracture, she was not suggested any lumbar brace, as it may further aggravate episode of AD due to tight abdominal bracing and sweating under the brace may precipitate pressure sore in sacral region.
Conclusion
Discovertebral lesion (AL) of the ankylosed spine is a recognized entity in AS, but may be overlooked as a precipitating cause for dysreflexic symptoms in SCI patient, especially as they commonly occur below the neurological level of injury. Therefore, physicians should check radiographs not only at the site of injury, but also at the thoracolumbar and lumbar spine, when AS patients with SCI with a lesion above the level of the sixth thoracic segment complain of symptoms of AD reaction.
References
Erickson RP . Autonomic hyperreflexia: pathophysiology and medical management. Arch Phys Med Rehabil 1980; 61: 431–440.
Wu KP, Lai PL, Lee LF, Hsu CC . Autonomic dysreflexia triggered by an unstable lumbar spine in a quadriplegic patient. Chang Gung Med J 2005; 28: 508–511.
Pasquina PF, Houston RM, Belandres PV . Beta blockade in the treatment of autonomic dysreflexia: a case report and review. Arch Phys Med Rehabil 1998; 79: 582–584.
Huang SC, Tsai WJ, Chou SW, Wang CM, Wong AMK . Autonomic dysreflexia in ankylosing spondylitis with double spinal cord injuries: a case report. Tw J Phys Med Rehabil 2007; 35: 171–177.
Von Bechterew W . Steifigkeit der wirbelsäule und ihre Verkrümmung als besondere Erkrankungsform. Neurol Zentralblatt 1893; 12: 426–434.
Bron JL, de Vries MK, Snieders MN, van der Horst-Bruinsma IE, van Royen BJ . Discovertebral (Andersson) lesions of the spine in ankylosing spondylitis revisited. Clin Rheumatol 2009; 28: 883–892.
Karlsson AK . Autonomic dysreflexia. Spinal cord 1999; 37: 383–391.
Mathias CJ, Bannister R . Autonomic disturbances in spinal cord lesions. Autonomic failure: A textbook of clinical disorders of the autonimc nervous system. 4th edn Oxford University Press: Oxford, UK, 1999; 494–513.
Selmi F, Frankel HL, Kumaraguru AP, Apostopoulos V . Charcot joint of the spine, a cause of autonomic dysreflexia in spinal cord injured patients. Spinal Cord 2002; 40: 481–483.
Beard JP, Wade WH, Barber DB . Sacral insufficiency stress fracture as etiology of positional autonomic dysreflexia: case report. Paraplegia 1996; 34: 173–175.
Morita M, Iwasaki M, Okuda S, Oda T, Miyauchi A . Autonomic dysreflexia associated with Charcot spine following spinal cord injury: a case report and literature review. Eur Spine J 2010; 19 (Suppl 2): S179–S182.
Chan FL, Ho EK, Fang D, Hsu LC, Leong JC, Ngan H . Spinal pseudarthrosis in ankylosing spondylitis. Acta Radiol 28: 383–388.
Fang D, Leong JC, Ho EK, Chan FL, Chow SP . Spinal pseudarthrosis in ankylosing spondylitis. Clinicopathological correlation and the results of anterior spinal fusion. J Bone Joint Surg Br 70: 443–447.
Thumbikat P, Ravichandran G, McClelland MR . Neuropathic lumbar spondylolisthesis--a rare trigger for posture induced autonomic dysreflexia. Spinal Cord 2001; 39: 564–567.
Yarkony GM, Katz RT, Yeong-Chi W . Seizures secondary to autonomic dysreflexia. Arch Phys Med Rehabil 1986; 67: 834–835.
Pine ZM, Miller SD, Alonso JA . Atrial fibrillation associated with autonomic dysreflexia. Am J Phys Med Rehabil 1991; 70: 271–273.
Eltorai I, Kim R, Vulpe M, Kasravi H, Ho W . Fatal cerebral hemorrhage due to autonomic dysreflexia in a tetraplegic patient: case report and review. Paraplegia 1992; 30: 355–360.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Barman, A., Sinha, M. & Rao, P. Discovertebral (Andersson) lesion of the Ankylosing Spondylitis, a cause of autonomic dysreflexia in spinal cord injury. Spinal Cord Ser Cases 2, 16008 (2016). https://doi.org/10.1038/scsandc.2016.8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.8
This article is cited by
-
Low pelvic incidence is associated with Andersson lesions in ankylosing spondylitis patients with kyphosis
Clinical Rheumatology (2020)