Abstract
We report a case of a giant intra and extradural cervical schwannoma in a patient affected by a severe myelo-radiculopathy. Clinical features, diagnosis and the issues concerning the surgical management of this benign tumor are discussed. We also review similar cases previously reported in the literature. A 50-year old caucasian woman was complaining of a 1 year of neck pain and worsening motor impairment in all four limbs causing the inability to walk. Neuroradiological assessment revealed a suspected schwannoma involving the nerve roots from C3 to C5, compressing and deviating the spinal cord. The vertebral artery was also encased within the lesion, but still patent. A posterior cervical laminectomy with a microsurgical extradural resection of the lesion was performed. Moreover, an accurate dissection of the lesion from the vertebral artery and the resection of the intraspinal component was achieved. Vertebral fixation with screws on the lateral masses of C3, C5 and C6 and a hook on C1 was performed. The procedure was secured using electroneurophysiological monitoring. A progressive improvement of the motor functions was achieved. A cervical post-contrast MRI revealed optimal medullary decompression and a gross-total resection of the lesion. Schwannomas are benign, slowly growing lesions which may cause serious neurological deficit. Early diagnosis is necessary and it maybe aided by imaging studies such as MRI or CT. The accepted treatment for these tumors is surgical resection and, when indicated, vertebral fixation.
Similar content being viewed by others
Spinal schwannomas are benign slow-growing tumors, representing ~30% of all primary spinal cord tumors. Schwannomas more frequently (70%) arise from sensory root, rather than motor roots (20%). Rarely, 10% of their origin is undefined or from both motor and sensory roots.1,2 The vast majority of spinal schwannomas are intradural. The extradural localization is less common.3 Dumbbell schwannomas have been reported as a separate group of spinal tumors, which characteristically involve both the intra and the extradural compartments, occupying the intervertebral foramen. Such tumors are most frequently located in the cervical segment of the spine, but the existing literature reports only a few cases of giant lesions extending to different vertebral levels.4–6 Moreover, the cervical localization of an extradural schwannoma may raise several issues related to the extended involvement of the extradural neural vascular structure, such as the high spinal nerve roots and the vertebral artery.
The aim of this report is to describe the successful surgical management of these kind of lesions, focusing on the pre-operative planning and surgical management. The role of new technologies in supporting these surgical procedures, as well as, the importance of knowledge of the anatomic and pathological features of these lesions will be emphasized.
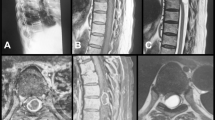
A 50-year-old lady was admitted to our institution complaining of neck pain, moderate weakness of the left arm, severe weakness in the right arm and severe paresis of the lower limbs with the inability to erect stand. She provided a 1-year history of worsening motor impairment, initially involving the lower limbs and then extending to the upper limbs during 2 months before admission. Moreover, a progressive extension of the motor defect to the arms and the hands, especially on the left side, was noted by the patient. Furthermore, she suffered a condition of psychiatric impairment and her social environment did not provide early recognition of the neurological compromise. Neurological examination revealed severe spastic tetraparesis, positive Babinsky and Hoffman signs and ankle clonus on the left side. A cervical spine magnetic resonance imaging (MRI) scan with and without gadolinium revealed a large mass in the cervical spine with a double extension into the intra and extradural region. The intraspinal component demonstrated a severe compression of the spinal cord, which was displaced anteriorly at C4–C5 level (Figure 1).
The pre-operative MRI scan did not reveal the position of the tumor with respect to the dural layer. The tumor was also responsible for a distortion of the bone structure of the C3, C4 and C5 vertebrae, with a involvement of the neuroforamina and the posterior facet joints on the left side. This was confirmed by the computed tomography (CT) scan with multiplanar and CT reconstruction (Figure 2).
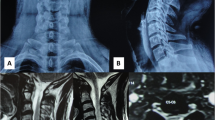
The extradural component of the tumor encased and displaced the vertebral artery on the left side as demonstrated by a CT-Angio scan (Figure 3).
After an informed consent was obtained from the patient and relatives, the patient underwent surgery.
The positioning of the patient was the first challenging step of the procedure, because of her obesity (body mass index: 34.7) together with a short neck. Neurophysiological monitoring electromyography and motor evoked potentials were utilized. A posterior approach to the cervical spine was performed which involved muscle dissection extending on both sides from C1 to C7. Before approaching the tumor, three screws on the right lateral masses of C3, C5 and C6 were inserted, under fluoroscopic guidance. Therefore, a left-sided hemilaminectomy extending from C2 to C5 was performed. The intraspinal component of the tumor was exposed; the lesion was unexpectedly extradural, without infiltration of the dural sheath. This facilitated a blunt dissection of the intracanalar component, which was completely removed with the aid of the ultrasonic aspiration. During and after the decompression of the spinal cord, no changes in spinal cord monitoring were recorded. The extradural component of the tumor was reached after performing the resection of the C4 left lateral mass, and a partial artrectomy of C3–C4 and C4–C5 joints. The lesion was initially debulked with the aid of an ultrasonic aspirator, in order to increase the handling of the capsule and facilitate the dissection. The tumor was highly vascular and encased the left vertebral artery. The dissection of the tumor was achieved through a cautious use of the CO2-laser. This device allowed an adequate control of the bleeding from the small venous tributaries of the perivertebral plexus. The optimal hemostasis achieved with CO2-laser ensured optimal visualization of the operative field, avoiding inadvertent injuries to the vertebral artery and the nerve roots. The left C3, C4 and C5 roots were gently separated from the capsule, whereas the C2 sensory nerve root was resected, being impossible to dissect from the tumor. This suggested a likely origin of the tumor from the C2 sensory nerve root. The vertebral artery was exposed and properly freed after completing tumor resection.
Subsequently, the instrumented construct was completed by the insertion of a further screw into the left C6 lateral mass and the positioning of two sublaminar hooks on C1 posterior arch under fluoroscopic control. Two rods were fixed from C1 to C6 on both sides, taking care to restore a good sagittal alignment of the spine. The intraoperative neuromonitoring did not show any anomaly during the entire procedure. During the phase of hemostasis, the application of autologous fibrin glue (Vivostat, Alleroed, Denmark) reduced the use of bipolar coagulation, maintaining the integrity of the tissues and reducing the risks of lesions on adjacent vascular and neural structures.7,8
The post-operative period was uneventful. The patient experienced a good recovery of the upper limb weakness and an improvement in the movements of the legs. Post-operative MRI scan documented adequate resection of the tumor decompression of the spinal cord (Figure 4). Furthermore, a control CT scan examination was performed, documenting the correct positioning of the implanted devices and a good alignment of the cervical spine (Figure 5).
The patient was discharged 5 days after the surgical procedures, and started a rehabilitation program in a dedicated center.
Despite a high incidence rate of dumbbell cervical tumors among spinal tumors has been recently reported,4 surgical management of these lesions remains challenging. Relatively few cases of giant dumbbell schwannomas have been reported. Furthermore, the definition of ‘dumbbell’ tumor and the related classification systems may not always apply to giant lesions. Giant schwannomas are able to deform and destruct the bone tissue, even while the dura is intact. This feature make often difficult to determine the relationship of the tumor with the foramina and the neural structures. Moreover, in those cases with an extended location involving more vertebral segments, the identification of the nerve root from which the tumor arose is impossible.
The first classification of dumbbell spinal tumor has been proposed by Eden in 1941.6 During the subsequent years, other classifications have been published, but the debate about the features and the growing modalities of these lesions still remains controversial.9 Ang et al.,10 in 2009 focused the anatomical and radiological features of cervical dumbbell tumors, reporting a new classification system based on the pre-operative radiological evaluation and related to the surgical approach. This classification appears more complete covering all type of tumors, but the correct pre-operative assessment and the subsequent decision of the surgical approach are strictly dependent on the quality of the neuroradiological imaging. Interestingly, Kim et al.,11 highlighted the features of the intraspinal component of dumbbell tumors, finding that the relationship of the tumor mass to dural sac in pre-operative MRIs was unclear in 5 of 7 cases reported. The surgical treatment of the dumbbell tumors in the cervical spine have also been debated. The most relevant issues related to the surgical approach of dumbbell tumors have been widely discussed. George et al.,12 proposed in 1985 the initial control of the vertebral artery during antero-lateral approach in order to minimize bleeding. Unfortunately, in our case, this maneuver was not feasible, because the resection of a giant tumor requested a prolonged surgical time. A good control of the bleeding was achieved in our case through the application of the laser technology for hemostasis. The selectivity of the CO2-laser for the small-caliber arterial channels coming from the vertebral artery appeared more effective than the use of the bipolar coagulation. This device facilitated the dissection maneuver avoiding injury to the neural structures.
The only paper on dumbbell cervical tumor, focusing on giant schwannomas, was published by Zhao and Xu13 in 2009. They proposed an extended postero-lateral approach for giant dumbbell schwannomas, in order to ensure an adequate exposure of the paravertebral component of the tumor. This is essential to achieve an optimal control of neural and vascular structures involved by the tumor. The authors performed laminectomy and lateral mass resection in a series of 16 patients and they did not report the occurrence of secondary instability during a 28-month period of follow-up. This data should be critically interpreted, because the limited number of patients and the lack of long-term follow up. Indeed, in another recent series,14 involving the surgical treatment of dumbbell cervical schwannomas in 75 patients, the incidence of post-operative deformities was significant. In our case, we chose to perform a spinal stabilization because the tumor, as well as the surgical approach caused compromise of the facet joints. Moreover, the patient presented also with neck pain, which was interpreted as a symptom owing to the neck instability.
Neuromonitoring is helpful during neurosurgery and in spine surgery.15 The aim of the monitoring in cervical spine surgery is a direct control of the functional status of the spinal cord and the verification of the integrity of the spinal roots. Indeed, the neuromonitoring not only improves the safety of the dissection of the extradural component of the tumor ensuring the integrity of the neural structures, but also it provides information about the possible occurrence of vascular or mechanical damages to the spinal cord.
Giant dumbbell cervical spine schwannomas are uncommon lesions and their surgical treatment is demanding and challenging. The rationale application of the available technological armamentarium improves the safety of the resection, leading to a better functional outcome. The most important critical points to keep in mind during the management of such lesions are: the prevention of instability of the spine; the optimal control of the bleeding and the preservation of the neural function. The application of the current technologies to achieve these points as well an accurate knowledge of the indications and the techniques significantly influence the results.
References
Heros RC . Lateral suboccipital approach for vertebral andvertebrobasilar artery lesions. J Neurosurg 1986; 64: 559–562.
Lot G, George B . The extent of drilling in lateral approaches to the cranio-cervical junction area from a series of 12 cases. Acta Neurochir (Wien) 1999; 141: 111–118.
Levy WJ, Latchaw J, Hahn JF, Sawhny B, Bay J, Dohn DF . Spinalneurofibromas: a report of 66 cases and a comparison with meningiomas. Neurosurgery 1986; 18: 331–334.
Ozawa H, Kokubun S, Aizawa T, Hoshikawa T, Kawahara C . Spinal dumbbell tumors: an analysis of a series of 118 cases. J Neurosurg Spine 2007; 7: 587–593.
Su X, Ni LC, Yan YH, Zhao W, Chen J . Giant dumbbell-shaped lumbar schwannoma. Spine J 2013; 13: 984.
Eden K . The dumb-bell tumors of the spine. Br J Surg 1941; 28: 549–570.
Giugno A, Maugeri R, D’Arpa S, Visocchi M, Iacopino DG . Complex reconstructive surgery following removal of extra-intracranial meningiomas, including the use of autologous fibrin glue and a pedicle muscle flap. Interdisciplinary Neurosurg 2014; 1: 84–87.
Graziano F, Certo F, Basile L, Maugeri R, Grasso G, Meccio F et al. Autologous fibrin sealant (Vivostat(®)) in the neurosurgical practice: Part I: Intracranial surgical procedure. Surg Neurol Int 2015; 6: 77.
Asazuma T, Toyama Y, Maruiwa H, Fujimura Y, Hirabayashi K . Surgical strategy for cervical dumbbell tumors based on a three-dimensional classification. Spine (Phila Pa 1976) 2004; 29: E10–E14.
Ang L, Lv Y, Liu XG, Ma QJ, Wei F, Dang GT . Results of surgical treatment of cervical dumbbell tumors: surgical approach and development of an anatomic classification system. Spine (Phila Pa 1976) 2009; 34: 1307–1314.
Kim JH, Han S, Kim JH, Kwon TH, Chung HS, Park YK . Surgical consideration of the intraspinal component in extradural dumbbell tumors. Surg Neurol 2008; 70: 98–103.
George B, Laurian C, Keravel Y, Cophignon J . Extradural and hourglass cervical neurinomas: the vertebral artery problem. Neurosurgery 1985; 16: 591–594.
Zhao B, Xu J . Extensive posterolateral exposure and total removal of the giant extraforaminal dumbbell tumors of cervical spine: surgical technique in a series of 16 patients. Spine J 2009; 9: 822–829.
Nakamura M, Iwanami A, Tsuji O, Hosogane N, Watanabe K, Tsuji T et al. Long-term surgical outcomes of cervical dumbbell neurinomas. J Orthop Sci 2013; 18: 8–13.
Lall RR, Lall RR, Hauptman JS, Munoz C, Cybulski GR, Koski T et al. Intraoperative neurophysiological monitoring in spine surgery: indications, efficacy, and role of the preoperative check list. Neurosurg Focus 2012; 33: E10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Iacopino, D., Giugno, A., Gulì, C. et al. Surgical nuances on the treatment of giant dumbbell cervical spine schwannomas: description of a challenging case and review of the literature. Spinal Cord Ser Cases 2, 15042 (2016). https://doi.org/10.1038/scsandc.2015.42
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2015.42