Abstract
Study design:
Single case-report.
Objectives:
To describe subarachnoid haemorrhage; an unusual complication following implantation of an intrathecal baclofen pump in an adult with spinal cord injury.
Setting:
Princess Royal Spinal Injuries Unit, Sheffield, UK.
Methods:
Review of the medical notes and literature.
Results:
A 77-year-old man with an incomplete ASIA-C spinal cord injury at C5 level sustained 2 years previously, developed subarachnoid haemorrhage following implantation of an intrathecal baclofen pump for the management of spasticity that was unresponsive to treatment with oral antispasticity agents.
Conclusion:
Subarachnoid haemorrhage can occur as a rare complication of insertion of Intrathecal baclofen pump. This need to be considered while evaluating patients who present with headache, confusion and seizures in the post operative period.
Sponsorship:
Not applicable.
Similar content being viewed by others
Introduction
Spasticity is a common problem affecting individuals with spinal cord injuries and can contribute to the development of contractures and pressure ulcers.1,2 Some patients may be unable to tolerate oral antispasticity drugs due to side-effects such as confusion, dizziness, drowsiness, muscle weakness and nausea.2 The Intrathecal baclofen (ITB) pump stores and delivers a selected dose of baclofen through a catheter into the spinal subarachnoid space; resulting in a high concentration of the drug within the spinal cord. The ITB helps in getting a good muscle relaxation with less side-effects. It is effective in the treatment of spasticity secondary to spinal cord disorders, stroke, cerebral palsy, traumatic brain injury and multiple sclerosis.2,3 Procedure-related complications of ITB pump include infection, skin erosions, and cerebrospinal fluid (CSF) leak and seroma formation around the pump.4 We report a patient who developed subarchnoid haemorrhage, a hitherto unreported procedure-related complication of insertion of an intrathecal catheter for the implantation of an ITB drug delivery system.
Case report
A 77-year-old man with an incomplete ASIA-C spinal cord injury at C5 level sustained 2 years previously, underwent implantation of an ITB pump for the management of spasticity that was unresponsive to treatment with oral antispasticity agents. He had an ileostomy for inflammatory bowel disease.
The baclofen pump (SynchroMed II, Medtronic, Minneapolis, MN, USA) and catheter insertion was carried out as an elective procedure under general anaesthesia. A 15G Touhy needle was used for the procedure. The lumbar puncture was done between the third and fourth lumbar vertebrae. The catheter used was the Medtronic 8731. The insertion of catheter was difficult. At the first attempt the catheter could not be passed. The catheter was completely withdrawn leaving the Tuohy needle in place. On second attempt, the X-ray revealed that the catheter has coiled and had to be reinserted with guide wire. The catheter went in between the third and fourth lumbar vertebrae posteriorly, traversed to the right anterior aspect, and then curved to the left lateral aspect of the spinal canal before coming back to the posterior aspect of the spinal cord at the T7 level. The catheter was within the intrathecal space. There was no obvious excessive bleeding during insertion of the catheter. The overall CSF loss was <5 ml. The anaesthetic induction and the immediate post operative period were uneventful. Around 12 h after the surgery; the patient developed headache and confusion. The pump site was healthy with no signs of a collection or infection around the pump. There was no sign leakage in the wound bandage. His right pupil was not reacting to light. He was unable to follow simple commands. He also had neck stiffness. Spasticity was well controlled.
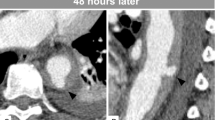
A computed tomography scan of the head demonstrated areas of high density over both parietal lobes suggestive of subarachnoid haemorrhage (Figure 1). Lumbar puncture showed 2000 red blood cells and 80 white blood cells (90% lymphocytes) in the CSF. He was treated with intravenous acyclovir, cefotaxime and amoxicillin to cover for bacterial meningitis and viral encephalitis. No organisms were visualised on gram stain and Polymerase Chain reaction of CSF for herpes simplex virus was negative magnetic resonance imaging of the head with magnetic resonance angiogram showed lesions with low signal intensity in the subarachnoid spaces and ventricles consistent with blood (Figure 2). No aneurysms were identified on the angiogram.
Subsequently he had partial seizures with secondary generalisation that were treated with Sodium Valoprate. He was treated conservatively and over the course of the next week his confusion improved. He was subsequently discharged.
Discussion
Potentially life-threatening complications of ITB include overdose and withdrawal syndrome.5,6 Infections, wound dehiscence, seroma and CSF leak have also been reported as have mechanical problems such as tear in the metal connector to the pump.5,6 A review on complications of ITB pump showed that procedure-related complications were present in more than one third of implants and pump related complications occurred infrequently.7 The data are mainly related to old catheter types. The design of the catheter has since improved and the incidence of the complications should hopefully reduce in future.
Our patient developed subarachnoid haemorrhage after implantation of ITB pump. An MR angiogram excluded aneurysm, the most common cause of Subarachnoid haemorrhage. In subarachnoid haemorrhage following rupture of aneurysm the blood is seen within the basal cisterns.8 In contrast, the computed tomography scan and magnetic resonance imaging of our patient showed blood in the sulci of the both parietal lobes near the vertex without any blood in the cisterns. The trauma during the intrathecal insertion of the catheter could have resulted in haemorrhage into the subarachnoid space in the lumbar spinal canal with subsequent with migration of blood intracranially causing headache and confusion. Alternatively intracranial hypotension following the lumbar puncture could rarely cause subarchnoid haemorrhage.9 Although lumbar puncture is usually a safe routine procedure, rarely serious complications such as subarchnoid haemorrhage, spinal epidural haematoma and intraventricular haemorrhage can occur.10,11
There is only one previous case-report on subarachnoid haemorrhage in a patient with ITB pump.12 In this case, a broken fragment of the intrathecal catheter migrated into the prepontine cistern and caused venous bleeding. The imaging in our patient did not show any evidence of broken catheter fragments in the subarachnoid space and his ITB pump was working satisfactorily. Margo et al.13 reported a patient who developed bilateral subdural haematomas following implantation of ITB pump. This case-report highlights a hitherto unreported procedure related complication that can occur in the immediate post operative period following implantation of ITB pump in patients with SCI. Subarachnoid haemorrhage; though as a rare complication of implantation of ITB pump, needs to be considered while evaluating patients who present with headache, confusion and seizures in the post operative period.
References
Adams M, Hicks A . Spasticity after spinal cord injury. Spinal Cord 2005; 43: 577–586.
Kheder A, Nair KPS . Spasticity: pathophysiology, evaluation and management. Pract Neurol 2012; 12: 289–298.
Penn RD, Kroin JS . Intrathecal baclofen alleviates spinal cord spasticity. Lancet 1984; 1: 1078.
Macdonnell RAL, Talalla A, Swash M, Grundy D . Intrathecal baclofen and the H-reflex. J Neurol Neurosurg Psychiatry 1989; 52: 1110–1112.
Awaad Y, Rizk T, Siddiqui I, Roosen N, Mcintosh K, Waines GM . Complicactions of intrathecal baclofen pump: prevention and cure. ISRN Neurol 2012; 2012: 575168.
Tunali Y, Hanimoglu H, Tanriverdi T, Hanci L, Hanci M . Intrathecal baclofen toxicity and deep coma in minutes. J Spinal Cord Med 2006; 29: 237–239.
Stetkarova I, Yablon SA, Kofler M, Stokic DS . Procedure- and device-related complications of intrathecal baclofen administration for management of adult muscle hypertonia: a review. Neurorehabil Neural Repair 2010; 24: 609–619.
Van Gijn J, Rinkel GJE . Subarachnoid haemorrhage: diagnosis, causes and management. Brain 2001; 124: 249–278.
Wang Y-F, Fuh1 J-L, Lirng J-F, Chang F-C, Wang S-J . Spontaneous intracranial hypotension with isolated cortical vein thrombosis and subarachnoid haemorrhage. Cephalalgia 2007; 27: 1413–1417.
Lee SJ, Lin YY, Hsu CW, Chu SJ, Tsai SH . Intraventricular haematoma, subarachnoid haemorrhage and spinal epidural haematoma caused by lumbar puncture: an unsual complication. Am J Med Sci 2009; 337: 143–145.
Liu WH, Lin JH, Lin JC, Ma HI . Severe intracranial and intraspinal subarachnoid haemorrhage after lumbar puncture: a rare case report. Am J Emerg Med 2008; 26: 633.
Nakaji P, Consiglieri GH, Garrett MP, Bambakidis NC, Shetter AG . Cranial migration of a baclofen pump catheter associated with a subarachnoid hemorrhage: case report. Neurosurgery 2009; 65: 1212–1213.
Magro E, Remy-Neris O, Seizeur R, Allano V, Quinio B, Dam-Hieu P . Bilateral subdural hematoma following implantation of intrathecal drug delivery device. Neuromodulation 2011; 14: 179–182.
Acknowledgements
Authors acknowledge contribution of Heather Allen, Department of Medical Imaging, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK for providing support with graphics used in the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Broadhurst, H., Thumbikat, P., Romanowski, C. et al. Subarachnoid haemorrhage: an unusual complication of implantation of an intrathecal baclofen pump. Spinal Cord Ser Cases 1, 15019 (2015). https://doi.org/10.1038/scsandc.2015.19
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2015.19