Abstract
Objectives:
Many complex mechanisms responsible for the pathogenesis of pressure ulcers (PUs) currently remain poorly understood. The objective of this study was to discover the major roles for inflammatory cytokines, growth factors and several apoptosis-related signal molecules in chronic PU wound.
Methods:
We investigated expression of inflammatory cytokines, growth factors and their corresponding receptors, and the apoptosis signal of caspase-3 in chronic stage III/IV chronic PU wound, acute wounds as well as normal skin controls. Tissues were stained by hematoxylin and eosin (HE) for histopathology and Masson’s trichrome for collagen. Vascular endothelial growth factor (VEGF), fibroblast growth factors 2 (bFGF) and caspase-3 were detected by immunohistochemical analysis. Expression of mRNAs for interleukin (IL)-1β, tumor necrosis factor-α (TNF-α), VEGF, KDR, bFGF and FGFR1 was determined by real-time reverse transcription PCR.
Results:
Stage III and IV chronic PUs stained had increased inflammatory cell infiltration and decreased collagen compared with controls. Levels of mRNAs for inflammatory cytokines IL-1β and TNF-α were elevated in PUs compared with acute wounds and normal skin. VEGF and bFGF, together with their receptors KDR and FGFR1, respectively, were significantly decreased compared with controls. However, the expression levels of caspase-3 were elevated in the PUs.
Conclusion:
Our series of studies have shown that chronic PUs displayed high levels of inflammation and disruption of the collagen matrix, along with increased indications of apoptosis and decreased levels of growth factors and their receptors. These characteristics can be used to comprehensively evaluate the etiology and treatment of chronic PUs.
Similar content being viewed by others
Introduction
Pressure ulcers (PUs) remain one of the most common wound healing problems in elderly, spinal cord injured and immobilized patients. Chronic wounds consisting of stage III and/or IV PUs are a common, but under-recognized problem. They significantly impact individual health and social aspects of quality of life, and can even lead to the patients death. Thus, it is imperative to take appropriate care to promote wound healing.
Normal physiological wound healing is a complex process involving several overlapping phases including inflammation, proliferation and remodeling. This process is delayed and complicated in diseased conditions like diabetes1 and venous ulcers.2 The wound healing process is controlled by the action of cytokines, chemokines and growth factors that direct the progression of events leading to the re-establishment of the barrier function of the skin. In chronic wounds, however, the expression of inflammatory cytokines is upregulated and/or prolonged. Further, the wound microenvironment sequesters various growth factors and cytokines, inhibiting their functions resulting in delaying wound healing.3
Cytokines and growth factors play major roles in wound healing by regulating cell proliferation, differentiation, migration and metabolism. In the process of wound healing, activated macrophages, fibroblasts, endothelial cells and other components release cytokines and growth factors, such as interleukin-1 (IL-1) and tumor necrosis factor-α (TNF-α), vascular endothelial growth factor (VEGF), fibroblast growth factors 2 (bFGF) and so on. A key proinflammatory cytokine, IL-1β, is generally associated with the regulation of immune and inflammatory responses. In vitro, it also stimulates collagenase production,4 TNF-α is synthesized and secreted by circulating monocytes and tissue macrophages, and is an important mediator of the host response to systemic infection and various other inflammatory disorders. VEGFs and their receptors, especially VEGFR-2 (KDR), may promote early events in angiogenesis, particularly endothelial cell migration and proliferation. Fibroblast growth factors, especially FGF2 (bFGF) and its receptor bFGFR, are preferentially involved in the process of angiogenesis, and also modulate cell growth and differentiation. In chronic non-PU wounds, decreases of growth factors and receptors such as bFGFR result in delayed wound healing.5 Apoptosis is an active and genetically controlled cell suicide program that occurs naturally to maintain the appropriate cellular composition of each organ.6 In chronic wounds, excessive apoptosis delays wound healing. Caspase is a key effector molecule that initiates the apoptotic process that results in the morphological and biochemical changes. Therefore, we investigated the role of apoptosis in PU wound healing.
Based on the above observations, we hypothesized that inflammation, growth factors and corresponding receptors, as well as apoptosis play important roles in PU wounds healing. Thus, in this study, we characterized the expression of IL-1β, TNF-α, VEGF, KDR, bFGF, bFGFR and collagen in PU wounds to provide a theoretical basis for the development of new treatments that promote more rapid healing of chronic PU wounds.
Patients and methods
Patients
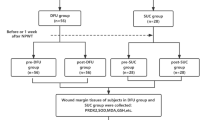
The procedures for this study were approved by the Human Ethics Committee of Wenzhou Medical College Research Center, Wenzhou, China. All subjects provided informed consent and were treated in accordance with the tenets of the Declaration of Helsinki. PU patients (16 men and 5 women; mean age, 62 years; range: 25–93 years) were recruited from hospitals in China. Inclusion criteria for this study were patients with either stage III or IV PUs according to the American National Pressure Ulcer Advisory Panel’s revised definitions.7 Tissue samples were taken from the center and margin of each PU.
Patients (eight men and six women; mean age, 48 years: range, 38–75 years) with acute non-PU wounds 3–7 days old were recruited as a control group. For a second control group, skin with no evidence of disease was retrieved after unrelated surgery of otherwise healthy subjects (three men and three women; mean age, 52 years; range: 50–56 years). Exclusion criteria for control groups included diabetes mellitus or peripheral vascular disease. Our investigations comply with the ethical rules for human experimentation that are stated in the 1975 Declaration of Helsinki, including approval by the institutional review board of Wenzhou Medical College.
Hematoxylin and eosin and Masson’s trichrome staining
Specimens taken from PU wounds, acute wounds and normal skin were embedded in paraffin and sectioned at 4 μm for histopathological examination by hematoxylin and eosin (HE) staining and for collagen by Masson’s trichrome staining. The sections were observed and photographed with a Nikon microscope (Eclipse 80i, Tokyo, Japan).
Immunohistochemistry
For the immunodetection of VEGF, bFGF and caspase-3, endogenous peroxidase in the deparaffinized and rehydrated tissue sections were inactivated by incubation with 3% H2O2 for 10 min. After antigen recovery, the sections were then blocked with 3% bovine serum albumin in phosphate-buffered saline for 1 h at 37 °C. After the excess liquid was discarded, the sections were incubated with anti-VEGF polyclonal rabbit antibody or anti-bFGF polyclonal rabbit antibody or anti-Caspase-3 polyclonal rabbit antibody (1:200 in 3% bovine serum albumin, Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA) at 4 °C overnight. The slides were then incubated with biotinylated secondary antibody (1: 400 in bovine serum albumin, Santa Cruz Biotechnology Inc.) for 2 h. The antibody binding sites were visualized by incubation with 5% diaminobenzidine in phosphate-buffered saline. The sections were then observed for the distribution and staining of positive cells of VEGF, bFGF and caspase-3 with Image-Pro Plus 6.0 software (Media Cybernetics Inc., Rockville, MD, USA) to analyze the integrated optical density in quantity. The higher the value of the integrated optical density, the higher the content of VEGF, bFGF and caspase-3.
Quantitative real-time reverse transcription PCR
Expression levels of mRNAs for IL-1β, TNF-α, VEGF, KDR, bFGF, bFGFR1 and glyceraldehyde phosphate dehydrogenase were determined by quantitative real-time reverse transcription PCR (Q–RT–PCR). Frozen samples (1.0 g) were crushed in a mortar under liquid nitrogen and then homogenized in TRIZOL (Invitrogen, Carlsbad, CA, USA) for extraction of total RNA (0.956 μg) according to each manufacturer’s protocol. Both reverse transcription and quantitative PCR were carried out using a two-step M-MLV Platinum SYBR Green qPCR SuperMix-UDG kit (Invitrogen). An Eppendorf Mastercycler (Eppendorf, Hamburg, Germany) was used for Q–RT–PCR analysis. Gene primer sequences (Table 1) for human IL-1β, TNF-α, VEGF, KDR, bFGF, FGFR1 and glyceraldehyde phosphate dehydrogenase were purchased from Invitrogen. The amount of each cytokine, growth factors and their receptors as well as mRNA was determined and normalized by the amount of glyceraldehyde phosphate dehydrogenase mRNA.
Statistical analysis
Statistical Procedures for the Social Sciences (v. 17.0) was used for statistical analyses. Data were expressed as means±s.d. Comparisons between two groups were made by least significant difference, and analysis of variance was used for comparison among different groups. Significant differences were accepted when P<0.05.
Results
HE and Masson’s trichrome staining
HE staining of skin associated with PU wounds (Figure 1) revealed large aggregations of inflammatory cells (blue arrow), fibroblasts and vascular endothelial cells. In skin from the acute wounds, there were numerous inflammatory cells and fibroblasts compared with the normal skin, but much less compared with the PU skin. As revealed by Masson’s trichrome staining, very little collagen was present in skin from the PU wounds (Figure 2). Skin from the acute wounds contained relatively more collagen protein, but much less than that in normal skin.
Expression of VEGF
Strong immunoreactivity for VEGF was present in the PU margins (Figure 3A and c) and in the acute wounds (Figure 3A and b), but little was present in the PU centers (Figure 3A and d), and almost none was present in the normal skins (Figure 3A and a). VEGF was present in various cell types, such as fibroblasts, endothelial cells and others. By quantitative immunohistochemistry (Figure 3B), expression of VEGF by normal skin was significantly less than the expression by other groups. The amount of VEGF expressed in the PU centers was significantly less than in the PU margins and in the acute wound.
(A) Immunohistochemical staining for VEGF expression (arrows) in normal skin (a), acute wounds (b), PU margin (c) and PU center (d); scale bar=50 μm. (B) Immunohistochemical analysis of image gray integral optical density (IOD) of VEGF protein in different groups. *P<0.01 other three groups versus normal skin; ⋆P<0.01 PU center versus PU margin; ▴P<0.01 PU groups versus acute wound.
Expression of bFGF
Strong immunoreactivity for bFGF was present in the PU margins (Figure 4A and c) and in the acute wounds (Figure 4A and b), but there was little present in the PU centers (Figure 4A and d) and almost none in normal skins (Figure 4A and a). bFGF was visualized in various cell types, such as fibroblasts, endothelial cells and others. By quantitative immunohistochemistry (Figure 4B), expression of bFGF by normal skin was significantly less than expression by the PU centers, PU margins and acute wounds. The highest amount of bFGF is expressed in the acute wounds.
(A) Immunohistochemical staining for bFGF expression in normal skin (a), acute wounds (b), PU margin (c) and PU center (d); scale bar=50 μm. (B) Immunohistochemical analysis of image gray integral optical density (IOD) of bFGF protein in different groups. *P<0.01 other three groups versus normal skin; ⋆P<0.01 PU center versus PU margin; ▴P<0.01 PU groups versus acute wound.
Expression of caspase-3
Strong immunoreactivity for caspase-3 was present in the PU centers (Figure 5A and d) and margins (Figure 5A and c), but little was present in acute wounds (Figure 5A and b), and almost none in normal skins (Figure 5A and a). Caspase-3 was evident in fibroblasts, endothelial cell and others. By quantitative immunohistochemistry (Figure 5B), expression of caspase-3 by normal skin was significantly less than expression by the PU centers, PU margins and acute wounds (Figure 4B). The amount of caspase-3 expressed in the PU centers was significantly more than that in the PU margins and in acute wounds.
(A) Immunohistochemical staining for caspase-3 expression (short arrows) in normal skin (a), acute wounds (b), PU margins (c) and PU centers (d); scale bar=50 μm. (B) Immunohistochemical analysis of image gray integral optical density (IOD) of caspase-3 protein in different groups. *P<0.01 other three groups versus normal skin; ⋆P<0.01 PU center versus PU margin; ▴P<0.01 PU groups versus acute wound.
The result of real-time-RT–PCR
As determined by real-time-RT–PCR, the expression IL-1β (Figure 6a) and TNF-α (Figure 6b) mRNAs in normal skin was significantly less than that in acute wounds, PU centers and PU margins. Within the PUs, the amount of mRNA TNF-α and IL-1β expressed in the centers was significantly less than that in the margins. The expression of VEGF mRNA (Figure 6c) in normal skins was significantly less than in the PU centers, PU margins and acute wounds. Further, the VEGF mRNA expression in the PU centers was significantly less than that in the PU margins and acute wounds. KDR mRNA (Figure 6d) levels in the PU centers was significantly less than in the PU margins, normal skin and acute wounds. The expression of bFGF mRNA (Figure 6e) followed the same pattern as that for VEGF mRNA, with lowest levels in normal skins and significantly higher levels in the PU centers, PU margins and in the acute wounds. Similarly, the expression of FGFR1 mRNA (Figure 6f) followed the same pattern as KDR mRNA. Thus, the lowest levels were in the PU centers, whereas significantly higher levels were in normal skins, PU margins and acute wounds.
Discussion
Wound healing has traditionally been divided into three overlapping phases: inflammation, proliferation and remodeling. The complexity of the process makes it susceptible to interruption at many steps, resulting in delayed healing typical of chronic wounds. Based on the known roles of cytokines, growth factors and apoptosis in wound healing, we selected the cytokines IL-1β and TNF-α, the growth factors VEGF and bFGF and associated receptors, and the apoptosis signal molecule caspase-3 for study in chronic PU wound healing.
During the inflammatory phase, the most well-known cytokines involved in the healing process are the proinflammatory molecules IL-1β and TNF-α. These cytokines are essential in the early phases of wound healing because they induce neutrophil recruitment and maturation and increased vascular permeability. However, overproduction or prolonged expression of IL-1β and TNF-α in the inflammatory phase may cause increased tissue destruction due to the overactivation of immune cells and the production of proteases, along with decreased collagen synthesis and reduced formation of granulation tissue.8
In our study, HE staining showed that normal skin contains large bundles of mature collagen with scattered fibroblasts and few inflammatory cells. In sharp contrast, all of the 21 histologic sections obtained from the chronic PUs revealed massive neutrophil infiltration and increased density of small vessels, which is consistent with results reported by Diegelmann.9 In the extracellular matrix surrounding the dense neutrophil clusters in the PU wounds, there were areas of dissociated matrix. In contrast, in the acute wounds there were fewer neutrophils and collagen than that in the PU wounds. At the same time, the Q–RT–PCR results showed that the inflammatory mRNA levels of IL-1β and TNF-α were specifically increased than the that of acute wounds. Thus, we hypothesize that the chronic PUs are locked into a state of prolonged inflammation that is characterized by abundant neutrophil infiltration, with the potential to produce large amounts of reactive oxygen species and destructive enzymes. Healing of these types of wounds proceeds only after the inflammation becomes controlled. Strategies that downregulate the neutrophil infiltration induced by these powerful inflammatory cells need to be explored.
Apoptosis is involved in the regulation of wound healing in the various stages of tissue repair. In the early phases, inflammatory cells undergo apoptosis starting at 12 h after wounding.10 In the later phases, apoptosis in myofibroblasts occurs on day 12 and peaks at day 20.11 Endothelial cells respond to sustained hypoxia by the production of TNF-α, which along with IL-1β promotes the onset of apoptosis in animal models of wound healing.12 This suggests that apoptosis could be an important factor in the onset of delayed wound healing.
In addition to the elevated levels of IL-1β and TNF-α mRNAs, we found that caspase-3 protein was elevated in PU wounds, especially in the centers. In contrast, acute wounds showed lower levels of caspase-3 than did the PU wounds. In normal skin, caspase-3 expression was detected in only a few epidermal cells. These results suggest that excessive apoptosis in PU chronic wounds may impede granulation and delay wound healing. In the present study, we detected apoptosis only in the late stages of PU wound healing, which contrasts with the early presence of apoptosis in the early stage of our rat model of PU healing. One study has indicated the presence of apoptosis in burn-wound healing during the period from the acute inflammatory stage to the proliferative stage and in the period from the proliferative stage to the remodeling stage.13 Thus, we expected to detect apoptosis in the different phases of PU wound healing. The signaling pathway for apoptosis is complex and may be affected by environmental conditions. Understanding the role and regulation of apoptosis in chronic PU wound healing might enable us to modulate apoptosis to achieve early healing.
Growth factors play major roles in the complex biological and molecular events underlying cutaneous wound healing. During cutaneous wound healing, the development of granulation tissue requires the formation of new capillaries, which is a feature of chronic wounds. Angiogenesis is stimulated by a number of different growth factors, including VEGF and bFGF, which appear to be of primary importance. The effects of these growth factors are mediated through transmembrane receptor tyrosine kinases, such as KDR and bFGFR1.14 Activation of these receptors initiates chemotaxis and proliferation of endothelial cells in vitro, and it accelerates wound healing by increasing neovascularization.15
By immunohistochemistry and real-time RT–PCR, we measured the protein and mRNA levels of VEGF and bFGF. Expression of both growth factor proteins and mRNAs were upregulated in chronic PU wounds compared to the normal skin, which is consistent with the observation by Pufe et al.16 The upregulation may enhance the healing of PUs. However, protein and mRNA levels of VEGF and bFGF in the PUs were significantly lower than that in acute wounds. The stimulus for the upregulation of these growth factors in the PUs is not known with certainty, but it may be derived from autocrine and/or paracrine stimulation of various tissue-repair cells.17 In addition, hypoxia may stimulate the enhanced secretion of VEGF and bFGF.
We also showed that the mRNA for VEGF and bFGF growth factor receptors, KDR and FGFR1, respectively, decreased compared with control skin of healthy individuals and acute wounds. The decrease in mRNAs for these receptors may indicate a decrease in the number of active receptors present. If that is the case, then this could contribute to the delayed wound healing typical of chronic PUs. bFGF promotes angiogenesis by controlling the migration and proliferation of endothelial cells, fibroblasts and others, and it induces VEGF expression. In vitro, bFGF regulates the synthesis and deposition of various extracellular matrix components, increases keratinocyte motility during re-epithelialization, and promotes the migration of fibroblasts and stimulates them to produce collagen.18 VEGF also acts as a survival factor for endothelial cells by inducing the expression of Bcl-2, an anti-apoptotic protein.19
Based on that study, we hypothesized that application of bFGF would improve healing of chronic wounds. However, clinical trials of this hypothesis were not satisfactory,10 probably due to the complexity of the wound healing cascade, and the physical inhibition and biological degradation of bFGF. To overcome these issues, it may be necessary to genetically engineer proteins functionally similar to VEGF and bFGF that will be effective when delivered to chronic PU wound sites. A model for such delivery has already been established by Park et al.20 who used chitosan scaffolds with bFGF to accelerate wound closure of PUs in aged mice.
Data archiving
There were no data to deposit.
References
Brem H, Tomic-Canic M . Cellular and molecular basis of wound healing in diabetes. J Clin Invest 2007; 117: 1219–1222.
Bishop JB, Phillips LG, Mustoe TA, VanderZee AJ, Wiersema L, Roach DE et al. A prospective randomized evaluator-blinded trial of two potential wound healing agents for the treatment of venous stasis ulcers. J Vasc Surg 1992; 16: 251–257.
Schultz GS, Wysocki A . Interactions between extracellular matrix and growth factors in wound healing. Wound Repair Regen 2009; 17: 153–162.
Xiaobing FU . Pay great attention to the study the pathogenesis and preventive treatment of chronic impaired healing wound on body surface. Chin J Traumatol 2004; 20: 449–451.
Banerjee M, Saxena M . Interleukin-1 (IL-1) family of cytokines: role in Type 2 Diabetes. Clin Chim Acta 2012; 413: 1163–1170.
Ziv I, Zilkha-Falb R, Offen D, Shirvan A, Barzilai A, Melamed E . Levodopa induces apoptosis in cultured neuronal cells-a possible accelerator of nigrostriatal degeneration in Parkinson's disease? Mov Disord 1997; 12: 17–23.
Black J, Baharestani MM, Cuddigan J, Dorner B, Edsberg L, Langemo D et al. National Pressure Ulcer Advisory Panel. National Pressure Ulcer Advisory Panel's updated pressure ulcer staging system. Adv Skin Wound Care 2007; 20: 269–274.
Rapala K, Laato M, Niinikoski J, Kujari H, Söder O, Mauviel A et al. Tumor necrosis factor alpha inhibits wound healing in the rat. Eur Surg Res 1991; 23: 261–268.
Diegelmann RF . Excessive neutrophils characterize chronic pressure ulcers. Wound Repair Regen. 2003; 11: 490–495.
Brown DL, Kao WW, Greenhalgh DG . Apoptosis down-regulates inflammation under the advancing epithelial wound edge: delayed patterns in diabetes and improvement with topical growth factors. Surgery 1997; 121: 372–380.
Desmoulière A, Redard M, Darby I, Gabbiani G . Apoptosis mediates the decrease in cellularity during the transition between granulation tissue and scar. Am J Pathol 1995; 146: 56–66.
Seth AK, Geringer MR, Hong SJ, Leung KP, Galiano RD, Mustoe TA . Comparative analysis of single-species and polybacterial wound biofilms using a quantitative, in vivo, rabbit ear model. PloS ONE 2012; 7: e42897.
Nagata M, Takenaka H, Shibagaki R, Kishimoto S . Apoptosis and p53 protein expression increase in the process of burn wound healing in guinea-pig skin. Br J Dermatol 1999; 140: 829–838.
Carmeliet P, Jain RK . Molecular mechanisms and clinical applications of angiogenesis. Nature 2011; 473: 298–307.
Chiu LL, Radisic M . Scaffolds with covalently immobilized VEGF and Angiopoietin-1 for vascularization of engineered tissues. Biomaterials 2010; 31: 226–241.
Pufe T, Paulsen F, Petersen W, Mentlein R, Tsokos M . The angiogenic peptide vascular endothelial growth factor (VEGF) is expressed in chronic sacral pressure ulcers. J Pathol 2003; 200: 130–136.
Menke J, Iwata Y, Rabacal WA, Basu R, Yeung YG, Humphreys BD et al. CSF-1 signals directly to renal tubular epithelial cells to mediate repair in mice. J Clin Invest 2009; 119: 2330–2342.
Sasaki T . The effects of basic fibroblast growth factor and doxorubicin on cultured human skin fibroblasts: relevance to wound healing. J Dermatol 1992; 19: 664–666.
Rao X, Zhong J, Zhang S, Zhang Y, Yu Q, Yang P et al. Loss of methyl-cpg-binding domain protein 2 enhances endothelial angiogenesis and protects mice against hind-limb ischemic injuryclinical perspective. Circulation 2011; 123: 2964–2974.
Park CJ, Clark SG, Lichtensteiger CA, Jamison RD, Johnson AJ . Accelerated wound closure of pressure ulcers in aged mice by chitosan scaffolds with and without bFGF. Acta Biomater 2009; 5: 1926–1936.
Acknowledgements
This work was supported by the National Natural Science Funding of China (81372064), Science and Technical Department of Zhejiang Province, China (2008C33044) and supported in part by the National Major Basic Research Project (973 program, 2012CB518105).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jiang, L., Dai, Y., Cui, F. et al. Expression of cytokines, growth factors and apoptosis-related signal molecules in chronic pressure ulcer wounds healing. Spinal Cord 52, 145–151 (2014). https://doi.org/10.1038/sc.2013.132
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.132
Keywords
This article is cited by
-
Uncovering the molecular identity of cardiosphere-derived cells (CDCs) by single-cell RNA sequencing
Basic Research in Cardiology (2022)
-
Photobiomodulation by dual-wavelength low-power laser effects on infected pressure ulcers
Lasers in Medical Science (2020)
-
Elevated Risk of Infections after Spinal Cord Surgery in Relation to Preoperative Pressure Ulcers: a Follow-up Study
Scientific Reports (2018)
-
Regulation of Langerhans cell functions in a hypoxic environment
Journal of Molecular Medicine (2016)
-
Immune dysfunction and chronic inflammation following spinal cord injury
Spinal Cord (2015)