Abstract
Study design:
Retrospective study.
Objectives:
The objective of this study was to compare the CO2 response of acute tetraplegic cervical spinal cord injury (SCI) patients undergoing mechanical ventilation with a control group of critically ill patients ready for weaning of mechanical ventilation and successfully extubated.
Setting:
This study was conducted at the intensive care unit of a University Hospital in Mallorca, Spain.
Methods:
CO2 response was studied in 12 acute tetraplegic cervical SCI patients at the C4−C7 level and 22 control patients. The control group patients were consecutively selected from a database of patients with mechanical ventilation and who were successfully extubated after a CO2 response test. To increase the CO2, we used the method of re-inhalation of expired air, and we evaluated the hypercapnic ventilatory response, the change in minute ventilation induced by the increase of partial pressure of arterial carbon dioxide (PaCO2), which measures the whole respiratory system (metabolic control, neuromuscular or ventilatory apparatus), and the hypercapnic drive response, the change in the airway occlusion pressure at 100 ms induced by the increase in PaCO2, which measures the chemosensitivity of the respiratory center.
Results:
Cervical SCI patients were younger than the control group patients (26±7 and 62±12 years, respectively; P<0.001). Mean values of the hypercapnic ventilatory response in cervical SCI and control groups were 0.52±0.31 and 0.64±0.33 l min−1 per mm Hg (P=0.40), respectively, and the hypercapnic drive response was 0.24±0.16 and 0.48±0.23 cm H2O per mm Hg (P=0.001), respectively.
Conclusion:
Acute tetraplegic cervical SCI patients had reduced hypercapnic drive response that may contribute to the difficult weaning, without reduction in hypercapnic ventilatory response.
Similar content being viewed by others
Introduction
Respiratory neuromuscular dysfunction leads to long-term ventilation and tracheostomy in many patients with cervical spinal cord injury (SCI). In spite of this, there is a subset of patients with cervical SCI that can be weaned early and extubated.1 The pathophysiology of respiratory failure in cervical SCI patients is not well known, and, consequently, no recommendations are available to identify which patients with cervical SCI can be successfuly extubated and which patients may benefit from early tracheostomy.
The respiratory neuromuscular function including muscular strength and control of breathing can be evaluated by measuring maximal inspiratory pressure (PImax), maximal expiratory pressure (PEmax)2 and the carbon dioxide (CO2) response test with hypercapnic ventilatory response, defined as the increase in minute volume (VE) to the increase in partial pressure of arterial carbon dioxide (PaCO2) and the hypercapnic drive response, defined as the increase in occlusion pressure (P0.1) to the increase in PaCO2.3, 4 Any alteration of the respiratory system (metabolic control, neuromuscular or ventilatory apparatus) can reduce the hypercapnic ventilatory response, whereas reduced hypercapnic drive response indicates an alteration in the chemosensitivity of the respiratory center.
Studies measuring the CO2 response in patients with chronic tetraplegia after cervical SCI reported discordant results. Some studies showed blunted CO2 response in chronic patients,5, 6 independently of seated or supine position, whereas other studies found normal CO2 response in the supine position.7, 8
To date, there are no studies linking the control of breathing, evaluated through the CO2 response, with weaning failure of mechanical ventilation in acute cervical SCI patients. To our knowledge, the CO2 response has only been studied in two patients with acute tetraplegic cervical SCI,6 in which the hypercapnic ventilatory response was reduced compared with control subjects, whereas the hypercapnic drive response did not show differences.
Our aim was to compare the CO2 response of patients with acute tetraplegic cervical SCI undergoing mechanical ventilation with a control group of critically ill patients ready for weaning of mechanical ventilation who were successfully extubated on the same day of CO2 response study.
Methods
Patients
Patients were retrospectively studied in two medical-surgical ICUs, at the beginning of weaning of mechanical ventilation. The study was conducted from July 2005 to November 2009, and was approved by the review board of our hospital. We certify that all applicable institutional and governmental regulations were followed during the course of this research. Informed consent was obtained in all cases from patients or closest relatives.
We studied patients presenting with tetraplegia due to acute cervical SCI who underwent mechanical ventilation. All patients had complete traumatic SCI at the C4–C7 level according to the American Spinal Injury Association scale (ASIA grade A). Patients with concomitant head, thoracic or abdominal injuries were excluded.
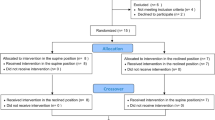
Control group patients were consecutively selected from a database of patients on whom a CO2 response test was performed on the first day of meeting the criteria for a spontaneous breathing trial (Figure 1). Patients were selected if they had been successfully extubated on the same day of the study. Their CO2 response test values were considered as a surrogate of preserved response to hypercapnia. We excluded patients with acute respiratory failure due to neuromuscular disease, chronic respiratory diseases or obesity. Obesity was defined as a body mass index higher than 30 Kg m−2. We did not include female patients in the control group, as all cervical SCI patients were male.
Protocol
Patients were eligible to be included in the trial when the physician in charge determined that they were clinically stable and fulfilled the clinical criteria for a spontaneous breathing trial. The routine clinical criteria for considering a spontaneous breathing trial included that patients be free of sedatives, awake, able to obey oral commands, hemodynamically stable, with core temperature <38.3 °C and with improvement or resolution of the condition that required mechanical ventilation, with partial pressure of arterial oxygen/FIO2>150 mm Hg and PEEP⩽8 cm H2O. A spontaneous breathing trial was performed every day if the patient fulfilled the clinical criteria until he was weaned from mechanical ventilation. The respiratory muscular strength and control of breathing were evaluated by measuring PImax, PEmax and CO2 response test. All these measurements were carried out in the semirecumbent position at 20 degrees. We first performed the CO2 response test and then, after a resting period, we measured the PImax and PEmax.
Measurements and procedures
Maximal inspiratory and expiratory pressure
PImax and PEmax were measured, after 1–2 min of spontaneous breathing, with an external pressure transducer via a unidirectional valve (Hans Rudolph, Kansas City, MO, USA) connected to the endotracheal tube. Patients were asked to breathe normally during the procedure. PImax was obtained at residual volume, by occluding the inspiratory port of the unidirectional valve, whereas PEmax was measured at total lung volume, by occluding the expiratory port.2 Two measurements were performed and the highest value was used for analysis.
CO2 response test
CO2 response test was conducted in both groups of patients. To increase the CO2, we used the method of re-inhalation of expired air3, 4 by inserting a 22-mm corrugated tube (CORR-A-FLEX II, Hudson RCI/Teleflex Medical, Research Triangle Park, NC, USA) between the Y-piece and the endotracheal tube, which increased the dead space with a volume similar to the tidal volume and obtained with a pressure support of 7 cm H2O in each patient.
Baseline values for CO2 response test were obtained after applying 5 min of pressure support ventilation with a pressure of 7 cm H2O without positive end-expiratory pressure, and FiO2 was set at 1.0 to prevent hypoxemia for patients’ security and to avoid hypoxic stimuli. Then, breathing frequency, P0.1 and VE were recorded from the ventilator, and an arterial blood sample was withdrawn. Thereafter, we initiated the CO2 response test by increasing the dead space maintaining the same ventilatory support, and when the exhaled CO2 (measured through capnography) had increased by above 10 mm Hg we measured again the breathing frequency, P0.1 and VE, and withdrew another arterial blood sample. Once the CO2 response test was complete, the added dead space was removed and the patient was returned to his original assisted ventilation mode.
We studied the following derived indexes of CO2 response test: the hypercapnic ventilatory response, defined as the ratio of the change in VE to the change in PaCO2 (ΔVE/ΔPaCO2), and the hypercapnic drive response, defined as the ratio of the change in P0.1 to ΔPaCO2 (ΔP0.1/ΔPaCO2). P0.1 was measured by means of the built-in system of the Dräger ventilator (Evita 2 Dura or Evita 4, Dräger, Lübeck, Germany),9 and P0.1 was calculated as the mean of five measurements at each point of the study. Arterial blood gases were measured with a blood gas analyzer (IL-1650, Instrument Laboratory, Izasa, Spain).
Data collection and definitions
We recorded clinical and demographic variables as appropriate. Duration of mechanical ventilation before the study day was defined as the number of days between the beginning of mechanical ventilation and the day that the CO2 response test was performed. Duration of weaning was defined as the time between the first day of meeting the weaning criteria (this was the day at which CO2 response test was performed) and the day that the patient was disconnected from mechanical ventilation. Spontaneous breathing trial failure was considered by the occurrence of tachypnea, tachycardia, hypertension, hypotension, hypoxemia, hypoventilation, depressed mental status, agitation, diaphoresis or evidence of increasing respiratory effort.
Statistical analysis
Categorical data are expressed as number and percentages. Continuous variables are expressed as mean±standard deviation or as median and interquartile ranges, as appropriate. The differences between the SCI group and the control group in clinical characteristics, respiratory parameters, arterial blood gases, respiratory muscular strength and control of breathing were analyzed with the Mann–Whitney U test. We used linear regression to establish the association between hypercapnic drive and hypercapnic ventilatory response. Statistical analysis was performed with specific statistics software (SPSS 18.0, SPSS, Chicago, IL, USA).
Results
During the study period, 43 patients were admitted with cervical SCI. We excluded 22 patients with associated head, abdominal or thoracic trauma, 8 patients who did not require and 1 patient who refused to consent. We therefore included 12 male patients with complete acute cervical SCI. The levels of fracture or fracture dislocation of SCI were as follows: C4 and C5 in one patient, C5 in seven patients, C6 in two patients, C6 and C7 in one patient and C7 in one patient. None of them had diabetes or chronic obstructive pulmonary disease. Surgical fixation of cervical fractures was performed at a median (interquartile ranges) of 4 (0–6) days. Tracheostomy was performed in nine patients at 18 (12–20) days after acute SCI. Five patients were successfully weaned from mechanical ventilation during admission, and seven patients (three without tracheostomy) were transferred with mechanical ventilation to a referral hospital and were lost to follow-up for weaning of mechanical ventilation.
The control group included 22 male patients (Figure 1). Their main diagnoses were pneumonia in 11 patients, other sepsis in 5, postoperative state in 5 and heart failure in 1. The control group of patients was older than the SCI group, more severely ill but had the same length of mechanical ventilation before the CO2 response test (Table 1).
There were no differences between groups in baseline respiratory parameters (breathing frequency, VE, P0.1) and in baseline arterial pH, plasma bicarbonate concentration and partial pressure of arterial oxygen (Table 2). Baseline PaCO2 was higher in the cervical SCI group than in the control group (Table 2).
The cervical SCI group had values of muscular strength (PImax and PEmax) lower than the control group (Table 3). The CO2 response test in the SCI group showed a lower increase in P0.1 and a lower hypercapnic drive response compared with the control group, whereas no significant differences between groups were observed in the increase of VE, the increase of PaCO2 or the hypercapnic ventilatory response (Table 3). Individual changes in VE, P0.1 and PaCO2 induced by the CO2 response test are represented for both groups in Figure 2.
Discussion
Our study showed that patients with an acute cervical SCI had a reduced PImax, PEmax and hypercapnic drive response compared with the control group, but had a similar hypercapnic ventilatory response.
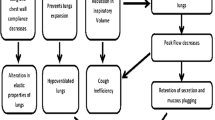
Acute respiratory failure in cervical SCI patients is attributed to the paralysis of the diaphragm, the intercostals and abdominal muscles and to an increased pulmonary elastance (elastics load), as well as resistance (resistive load). Thereby, the endurance of respiratory muscles is compromised owing to a reduction in its efficiency contributing to the risk of respiratory muscle fatigue and respiratory failure. Unexpectedly, our cervical SCI patients and control patients had similar values of hypercapnic ventilatory response, and, in spite of that, control patients were successfully weaned from mechanical ventilation, whereas cervical SCI patients remained mechanically ventilated by repeated failure of spontaneous breathing trial. This finding may suggest that the decreased respiratory muscle capacity was not the only reason to remain on mechanical ventilation in acute cervical SCI patients and other factors, such as the reduced hypercapnic drive response or a decreased muscle endurance, may also have played a role. Unfortunately, respiratory muscle endurance was not assessed in our patients.
The reduced hypercapnic drive response found in our cervical SCI group compared with the control group is difficult to explain, particularly if we consider the Holle et al.10 study in which the hypercapnic drive response was not affected by progressive muscular paralysis induced by curare. Consequently, we expected to find no alteration in the hypercapnic drive response in patients with cervical SCI.
Despite the fact that patients with acute cervical SCI may have early reduction in lung and chest-wall compliances11 or may experience air trapping because of the increase of VE during hypercapnic stimulation that may contribute to reduce the hypercapnic ventilatory response, these disorders should not affect the measurement of the hypercapnic drive response given that the P0.1 measurement is independent of respiratory-system resistance, compliance and Hering−Breuer inflation reflex.12 Moreover, Conti et al.13 found a reliable measurement of P0.1 during pressure-support ventilation in patients with variable levels of air trapping. Anyway, the possible air trapping by the increase in VE during the CO2 response test in our patients should be similar for the two compared groups, as it is also similar to the increase in VE.
Reduced hypercapnic drive response is a consequence of reduced sensitivity of chemoreceptors to chemical CO2 stimuli. The sensitivity can be reduced by genetic condition, observed in about 10% of the population,14 or, in some patients, it can be acquired by chronic diseases such as chronic obstructive pulmonary disease15 or diabetes16—conditions that were not present in our patients with SCI. In critically ill patients, sensitivity to CO2 may also be reduced because of sedatives and opioids17 used during mechanical ventilation, and because of the metabolic alkalosis18 frequently observed with the use of diuretics and corticosteroids. However, in our patients, the CO2 response test was performed free of sedatives and opioids, with the patient awake and able to obey oral commands, and plasma bicarbonate concentration did not show differences between SCI and control groups. We hypothesize that the reduction in CO2 sensitivity of chemoreceptors in cervical SCI patients could be explained by autonomic dysfunction by a loss of supraespinal control,19 similar to that described in diabetic patients with autonomic neuropathy.16 However, we assumed a linear association between P0.1 and PaCO2, and we cannot completely rule out that the paralysis of the respiratory muscles in patients with SCI or the method used to measure P0.1 through the ventilator may modify this relationship. Indeed, we measured P0.1 through the EVITA ventilators instead of the conventional method. This method of measuring P0.1 shows a trend to overestimate high P0.1 values and to underestimate low P0.1 values.9
Half of our patients with cervical SCI had values of hypercapnic drive response equal or lower than 0.19 cm H2O per mm Hg, a value associated with prolonged weaning of mechanical ventilation in critically ill patients.4 We believe that, along with the respiratory muscle paralysis, the reduced hypercapnic drive response to CO2 may contribute to the difficult weaning of mechanical ventilation observed in cervical SCI patients.
The potential clinical interest in evaluating the CO2 response test in acute cervical SCI patients could be the ability to identify those patients who will require long-term mechanical ventilation, similarly to what occurred in non-traumatic critically-ill patients ready for weaning of mechanical ventilation in whom a reduced CO2 response was associated with spontaneous breathing failure20 and prolonged weaning.4 Thus, these patients may benefit from early tracheostomy. Unfortunately, most of our cervical SCI patients were transferred to referral long-term rehabilitation hospitals in their country of origin connected to the ventilator, making follow-up impossible. Further studies will test this hypothesis.
Our study has several limitations. First, we studied a small number of patients with cervical SCI. Second, we could not match both groups for age because of the lower age of patients with SCI compared with non-traumatic critically ill patients. However, age diminishes the response to hypercapnia, and thus this bias would favor a higher CO2 response in the group of patients with SCI. Third, although the P0.1 measurement is independent of respiratory-system resistance and compliance, its interpretation can be challenging when the connecting nerves from the neural respiratory control to the respiratory muscles are disrupted or the P0.1 measurements are not obtained at functional residual capacity.12 Fourth, our PImax and PEmax values may not be accurate enough, as we measured them twofold instead of the recommended threefold.
In conclusion, acute tetraplegic cervical SCI patients had reduced hypercapnic drive response that may contribute to explain the difficult weaning of these patients, without significant reduction in hypercapnic ventilatory response.
Data archiving
There were no data to deposit.
References
Call MS, Kutcher ME, Izenberg RA, Singh T, Cohen MJ . Spinal cord injury: outcomes of ventilatory weaning and extubation. J Trauma 2011; 71: 1673–1679.
Marini JJ, Smith TC, Lamb V . Estimation of inspiratory muscle strength in mechanically ventilated patients: the measurement of maximal inspiratory pressure. J Crit Care 1986; 1: 32–38.
Sidney DA, Poon CS . Ventilatory responses to dead space and CO2 breathing under inspiratory resistive load. J Appl Physiol 1995; 78: 555–561.
Raurich JM, Rialp G, Ibanez J, Llompart-Pou JA, Ayestaran I . CO2 response and duration of weaning from mechanical ventilation. Respir Care 2011; 56: 1130–1136.
McCool FD, Brown R, Mayewski RJ, Hyde RW . Effects of posture on stimulated ventilation in quadriplegia. Am Rev Respir Dis 1988; 138: 101–105.
Manning HL, Brown R, Scharf SM, Leith DE, Weiss JW, Weinberger SE et al. Ventilatory and P0.1 response to hypercapnia in quadriplegia. Respir Physiol 1992; 89: 97–112.
Pokorski M, Morikawa T, Takaishi S, Masuda A, Ahn B, Honda Y . Ventilatory responses to chemosensory stimuli in quadriplegic subjects. Eur Respir J 1990; 3: 891–900.
Ben-Dov I, Zlobinski R, Segel MJ, Gaides M, Shulimzon T, Zeilig G . Ventilatory response to hypercapnia in C(5-8) chronic tetraplegia: the effect of posture. Arch Phys Med Rehabil 2009; 90: 1414–1417.
Subirana M, Irrazabal C, Bak E, Jara F, Mancebo J . Evaluación de la medida de la presión de oclusión incorporada en los ventiladores Evita. Med Intensiva 1997; 21: 305–310.
Holle RHO, Schoene RB, Pavlin EJ . Effect of respiratory muscle weakness on P0.1 induced by partial curarization. J Appl Physiol 1984; 57: 1150–1157.
Scanlon PD, Loring SH, Pichurko BM, McCool FD, Slutsky AS, Sarkarati M et al. Respiratory mechanics in acute quadriplegia. Lung and chest wall compliance and dimensional changes during respiratory maneuvers. Am Rev Respir Dis 1989; 139: 615–620.
Whitelaw WA, Derenne J-P . Airway occlusion pressure. J Appl Physiol 1993; 74: 1475–1483.
Conti G, Montini L, Pennisi MA, Cavaliere F, Arcangeli A, Bocci MG et al. A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med 2004; 30: 830–836.
Irsigler GB . Carbon dioxide response lines in young adults: the limits of the normal response. Am Rev Respir Dis 1976; 114: 529–536.
Altose MD, McCauley WC, Kelsen SG, Cherniack NS . Effects of hypercapnia and inspiratory flow-resistive loading on respiratory activity in chronic airways obstruction. J Clin Invest 1977; 59: 500–507.
Tantucci C, Scionti L, Bottini P, Dottorini ML, Puxeddu E, Casucci G et al. Influence of autonomic neuropathy of different severities on the hypercapnic drive to breathing in diabetic patients. Chest 1997; 112: 145–153.
Gross JB, Blouin RT, Zandsberg S, Conard PF, Haussler J . Effect of flumazenil on ventilatory drive during sedation with midazolam and alfentanil. Anesthesiology 1996; 85: 713–720.
Irsigler GB, Stafford MJ, Severinghaus JW . Relationship of CSF pH, O2, and CO2 responses in metabolic acidosis and alkalosis in humans. J Appl Physiol 1980; 48: 355–361.
Krassioukov A . Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol 2009; 169: 157–164.
Montgomery A, Holle R, Neagley S, Pierson D, Schoene R . Prediction of successful ventilator weaning using airway occlusion pressure and hypercapnic challenge. Chest 1987; 91: 496–499.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Raurich, J., Rialp, G., Llompart-Pou, J. et al. Respiratory CO2 response in acute cervical spinal cord injury (CO2 response in spinal cord injury). Spinal Cord 52, 39–43 (2014). https://doi.org/10.1038/sc.2013.115
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.115