Abstract
Study design:
Self-catheterising males aged ⩾18 years with spinal cord lesion and normal/impaired urethral sensation were enrolled in this comparative, randomised, crossover and open-labelled multicentre trial.
Objectives:
When possible, intermittent catheterisation is the preferred method of bladder emptying for neurogenic bladder dysfunction. Hydrophilic-coated catheters have improved safety and ease of use, and a new compact catheter for men has been developed to improve discretion.
Methods:
Participants self-catheterised at least four times daily for 14 days with a standard or compact catheter. The primary outcome measure was discomfort, using a visual analogue scale. Non-inferiority was defined as a difference in mean discomfort score of <0.9 cm. Other assessments included ease of use, discretion and the degree of pain, stinging or resistance.
Results:
A total of 36 individuals participated and 30 were included in the intention-to-treat analysis. The mean difference between catheters for participant discomfort was −0.347 cm (95% confidence intervals: −1.493, 0.800). There were significant differences (P⩽0.0001) in favour of the compact catheter for disposal and discretion, and inserting, storing, carrying and controlling the catheter. Fewer participants experienced resistance with the compact catheter. Participants were less likely to touch the coated part of the compact catheter. One adverse event was reported for each catheter.
Conclusions:
The coated compact catheter is at least as acceptable to the user as the standard catheter, with no inferiority observed in the level of discomfort. Secondary endpoints suggest that there are advantages of using the compact catheter, particularly with regard to discretion and ease of use.
Setting:
France/Denmark.
Similar content being viewed by others
Introduction
Individuals with spinal cord injuries and disorders, which affect the peripheral or central nervous system, are at high risk of developing functional disturbances in the urinary tract.1 The recommended method of bladder emptying for these individuals with neurogenic bladder dysfunction is intermittent catheterisation (IC), if they are willing and able to perform the procedure.1, 2 Good adherence to catheterisation can decrease the risk of upper urinary tract infections and maintain renal function, as well as improving continence.1, 3 These advantages over continuous catheterisation can have a considerable positive impact on an individual's day-to-day activities.4, 5
Acceptance of intermittent self-catheterisation largely relies on the efficacy of catheterisation and on the user's confidence that use of the catheter will not lead to increased sickness or injury.5, 6 Ease and quickness of use is another key consideration.6 To address this issue, coated catheters that provide improved lubrication and may reduce the frequency of urinary tract infections have been developed.7 Such improvements are important because the method of catheterisation can significantly affect an individual's quality of life.8 Several different types of coating have been developed, including gel-coated polyvinyl chloride (pre-lubricated with gel by the manufacturer) and hydrophilic-coated catheters.9
Another important and often overlooked factor influencing long-term compliance with self-catheterisation is a requirement for privacy and discretion.5, 10 Standard intermittent catheters for men can be unwieldy and difficult to use and carry discreetly; their standard length is ∼40 cm, despite the fact that the male urethra is usually less than 30 cm.11 A new compact male hydrophilic-coated catheter has therefore been developed, using a telescopic design that extends from 19 to 30 cm in length. Preliminary investigations in healthy male volunteers have suggested that the short-term safety profile of this compact catheter is at least as good as a standard-sized catheter, but that the compact catheter has better handling qualities.12 However, as catheterisation can be a long-term technique, often required for the lifetime of an individual, the longer-term safety profile and ease of use of the compact catheter needed to be confirmed in individuals with neurogenic bladder dysfunction using the catheter on a daily basis.
The objective of this study was to evaluate whether the compact catheter was no less accepted than a standard catheter when used at least four times a day for 14 days by individuals with neurogenic bladder dysfunction and normal or impaired sensation in the urethra. The discretion and ease of use of the compact catheter were also investigated.
Participants and methods
Study design
This was a comparative, randomised, cross-over and open-labelled multicentre trial, which included males aged ⩾18 years with spinal cord lesion (SCL) and neurogenic bladder dysfunction. All participants reported having some sensation in the urethra and self-catheterised at least four times a day. Other inclusion criteria were: use of clean, intermittent self-catheterisation for at least 14 days at enrolment and the ability to open and prepare the catheters for catheterisation. Individuals were excluded from the trial if they had a symptomatic urinary tract infection, as assessed by the investigator, or if they were mentally unstable and unable to comply with study procedures. Participants could be reassessed for enrolment 5 days after termination of treatment for a symptomatic urinary tract infection.
Local ethics committee approval or written opinion was obtained before the study was initiated and signed informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki II, 1964, as amended in Seoul, October 2008.
Intervention
Participants were randomised to one of two treatment groups by computer and instructed on the use of a single-use standard coated catheter (SpeediCath Male, Coloplast A/S, Humlebaek, Denmark) or a single-use compact coated catheter (SpeediCath Compact Male) when appropriate (Figure 1). Sealed randomisation envelopes were provided and participants were randomised in blocks of four within each investigational site. Group A assessed the standard catheter first, followed by the compact catheter; Group B tested the compact catheter first, followed by the standard catheter. During each test period, participants self-catheterised using a minimum of four catheters each day for 14 days (±2 days) (Figure 2).
Design of the compact catheter and its packaging. The compact catheter uses a telescopic design. The connector (or handle) of the catheter is exposed after removal of the lid from the packaging. Pulling this handle telescopically extends the catheter to its full length and removes it from the packaging. A ‘click’ indicates that the catheter has been released and is ready to use; a lock mechanism ensures that the catheter remains extended during catheterisation.
Each participant made three hospital visits: one at baseline, one at crossover and one at study end. A week after the first visit and a week after the crossover visit, the investigator contacted the participant via telephone to confirm that they were following the correct procedure.
Evaluations
Data collected at baseline included: age, previous experience of intermittent catheters, number of catheters used per day, mobility, cause of bladder dysfunction and level and severity (American Spinal Injury Association (ASIA) impairment scale) of the SCL assessed by the International Standards for Neurological Classification of Spinal Cord Injury.13
The primary outcome measure was participant discomfort during catheterisation, measured by subjective evaluation on a 10-cm visual analogue scale (VAS), where 0 was ‘no discomfort’ and 10 was ‘worst discomfort imaginable’.
Each participant completed a questionnaire, answering questions using a five-point scale (for example, 1=very easy; 5=very difficult), as follows:
-
How do you experience the overall discretion of the catheters?
-
How do you experience the disposal of the catheters?
-
How do you experience the carrying of the catheters?
-
How do you experience the storing of the catheters?
-
How is the opening of the catheters’ packaging?
-
How do you experience the insertion of the catheters?
-
How do you experience the control of the catheters during insertion?
Participants were also asked whether they experienced pain, stinging or resistance, measured on a four-point scale (for example for pain: 1=no pain; 4=severe pain), and whether there was need for them to touch the coated part of the catheter during insertion. At the end of the study, participants were asked which catheter they preferred. Quality of life was assessed using questions on influence on daily activities, general satisfaction and overall quality of life using a 10-cm VAS.
Safety was assessed by recording adverse events (AEs) and serious AEs, reported by the investigator at the end of each test period. The presence of visible bleeding was reported by the participants.
Statistical analysis
For the primary outcome measure, non-inferiority of the compact catheter was considered established if the discomfort score of the compact catheter during insertion did not exceed the average discomfort score of the standard-length catheter by more than 0.90 cm on the VAS. A minimum of 33 enrolled patients were estimated as being necessary to demonstrate non-inferiority, as defined above, with a power of 90%, a significance level of 0.05, and an estimated drop-out rate of ∼20%. All randomised participants who performed at least one catheterisation and who were evaluable with respect to at least one endpoint constituted the intention-to-treat (ITT) analysis set. The per protocol (PP) analysis set included the subset of ITT who fulfilled all inclusion and exclusion criteria and completed both test periods according to the study protocol.
The primary outcome was analysed using a paired t-test, derived from a linear analysis of covariance. Separate analysis was performed in the ITT and PP analysis sets. The test was performed as a non-inferiority test, that is, as a test of the (composite) null hypothesis that the mean VAS score, using the compact male catheter, exceeded the mean VAS score, using the regular male catheter, by at least 0.9 cm. The test was carried out at the 2.5% significance level. Secondary endpoints were analysed using Fisher's exact test and proportional odds regression models based on the ITT analysis set. All statistical analyses were performed with SAS software version 9.1.3 (SAS Institute Inc., Cary, NC, USA).
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Demographics and baseline characteristics
In total, 36 participants were enrolled over the period of November 2009–March 2010 in three centres in France and two in Denmark. The majority of participants (66.7%) required bladder control measures because of traumatic SCL, including transport-related accidents (25.0%) or injury as a result of a fall (19.4%). Non-traumatic SCL was the cause of neurogenic bladder dysfunction in 33.3% of participants, including two with spina bifida. Most participants (72.2%) were using the standard-length catheter used in this study before randomisation; these 26 participants had been self-catheterising for a median duration of 24.5 months, using a median of six catheters a day. Participants who were using a different type of catheter before the study had been self-catheterising for a median duration of 114.0 months, using a median of five catheters a day. An overview of the participant demographics at baseline is shown in Table 1.
Participant disposition
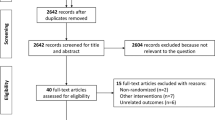
Figure 2 shows the participant disposition during the study. Nine participants discontinued the study: two because of AEs (one for each catheter), two chose to discontinue (both from the standard catheter), three discontinued because of perceived lack of efficacy (all from the compact catheter) and two for other reasons (standard catheter). The ITT analysis included 30 participants (6 participants who discontinued in the first period of the study were excluded because of lack of data); 23 participants were included in the PP analysis.
Primary endpoint
The compact catheter was not inferior to the standard-length catheter with regards to discomfort for both ITT and PP populations (Table 2). In both the ITT and the PP analysis, the upper limit of the 95% confidence interval (0.800 cm for the ITT analysis, −0.145 in for the PP analysis) was below the pre-specified non-inferiority margin of 0.9 cm, showing that the compact catheter was at least as comfortable as the standard catheter. There was a statistically significant difference between participants in Denmark and those in France with regards to the level of discomfort reported; participants in Denmark scored discomfort lower (mean difference of −1.351 cm) than the participants in France (P=0.0315).
Secondary endpoints
A significant difference (P⩽0.0001) in favour of the compact catheter was observed for mean ratings of discretion (odds ratio (OR), 20.40; 95% confidence intervals (CI), 4.91–84.67), storing (OR, 28.91; 95% CI, 7.66–109.06), carrying (OR, 47.32; 95% CI, 12.15–184.34) and disposal (OR, 17.66; 95% CI, 5.61–55.55) (Figure 3). The compact catheter was also rated higher for inserting (OR, 4.09; 95% CI, 1.35–12.36; P=0.0127) and controlling (OR, 13.30; 95% CI, 2.51–70.60; P=0.0024) the catheter (Figure 4). Fewer participants reported the need to touch the coated part of the catheter for the compact catheter than for the standard catheter (OR, 0.09; 95% CI, 0.02–0.35). Participants from Denmark found insertion (OR, 2.47; 95% CI, 1.05–5.80) and disposal (OR, 2.28; 95% CI, 1.00–5.17) of the catheters easier than those recruited in France, and fewer reported the need to touch the coated part of the catheter (OR, 0.15; 95% CI, 0.03–0.73).
Responses to questions on discretion and privacy. Participants completed a questionnaire, answering the following questions on the discretion and privacy associated with using both types of catheter using a five-point scale: (a) How do you experience the overall discretion of the catheters? (b) How do you experience the disposal of the catheters? (c) How do you experience the carrying of the catheters? (d) How do you experience the storing of the catheters? (n=30).
Responses to questions on ease of use. Participants completed a questionnaire, answering the following questions on the ease of use for both types of catheter using a five-point scale: (a) How do you experience the insertion of the catheters? (b) How do you experience the control of the catheters during insertion? (n=30).
The mean degree of resistance was rated lower when using the compact catheter (OR, 2.69; 95% CI, 1.12–6.49; P=0.0273); 16 participants (53.3%) reported no resistance for the compact catheter, compared with nine participants (30.0%) for the standard catheter. No stinging was reported by 24 (80.0%) and 23 participants (76.7%) for the compact catheter and standard catheter, respectively; 24 (80.0%) participants reported no pain for the compact catheter compared with 22 participants (73.3%) for the standard catheter. No difference was observed between the two catheters with regards to pain (P=0.6675) or stinging (P=0.6831). Most participants (70.0%; P=0.0285) preferred the compact catheter over the standard-length catheter. A significant difference was observed in favour of the compact catheter for influence on daily activities in the quality of life questionnaire (P=0.0323), although no difference was observed between the catheters for general satisfaction and overall quality of life.
Only two AEs were reported: one case of epididymitis for the standard catheter and one case of light discomfort during insertion for the compact catheter. Both of these AEs were classed as ‘possibly’ related to the catheter, but were mild in severity. Two occurrences of visual bleeding were reported for the compact catheter.
Discussion
The results of this study demonstrate that the compact hydrophilic-coated catheter is at least as safe and well tolerated as the standard hydrophilic-coated catheter for men with SCL and neurogenic bladder dysfunction, with no difference in discomfort or the frequency of AEs. Results from the secondary endpoints also indicate that participants found the compact catheter to be more discreet and easy-to-use than the standard-length catheter.
The primary endpoint, discomfort assessed by the participants on a VAS, was chosen because it is a very relevant measurement for people who regularly self-catheterise. Not only does discomfort affect an individual's general well being, it is also likely to be indicative of possible damage to the epithelial lining of the urethra. Although it is a subjective measure, it has been used successfully in other clinical trials comparing catheters.12, 14 The non-inferiority demonstrated in this trial is therefore a key clinically relevant result, together with the lack of any additional pain, resistance or stinging. This is important, as other results described here suggest that the compact catheter may have other advantages over the standard catheter.
The participant questionnaires completed at the end of each test period suggest that the compact catheter was viewed as more discreet, as demonstrated by the questions on discretion, disposal, carrying and storing. The control and insertion of the catheter was also considered to be better for the compact catheter, and the need to touch the coated part of the catheter was less.
These results confirm those observed in two recent studies of the same catheter.12, 15 In particular, a study in healthy volunteers by Bagi et al.12 comparing standard and compact catheters has shown no difference in discomfort, stinging or pain between the two catheters. Another study in women with a similar compact catheter also found that it was at least as efficient at emptying the bladder as more conventional female catheters.15 It is worth noting that both of these studies were short-term studies performed for only 1 day per catheter; however, this current study provides long-term evidence that compact catheters are suitable for individuals with neurogenic bladder dysfunction.
The compact catheter investigated in this study was well tolerated, as demonstrated by the low frequency of AEs reported for each catheter (one in each group). One potential concern is that there were three discontinuations from using the compact catheter due to perceived lack of efficacy. This has previously been reported with compact catheters for women16 and is an important issue for individuals who require self-catheterisation, as having confidence in the efficacy of the catheter is vital for an acceptable quality of life.6 Nevertheless, the majority of participants enrolled in this study preferred the compact catheter when asked, suggesting that it is safe and efficacious for most people with neurogenic bladder dysfunction. Furthermore, the compact catheter may be more hygienic than the standard catheter, as fewer participants reported the need to touch the coated part of the catheter. Importantly, no difference was observed in the residual urine detected using ultrasound in another recent study comparing the same compact catheter with the standard catheter.15
Covariate analysis revealed that participants recruited in Denmark reported a lower degree of discomfort during catheterisation than participants recruited in France. Furthermore, participants recruited in Denmark found insertion and disposal of the catheters easier, and fewer felt the need to touch the coated part of the catheter while catheterising. The reason for this geographical difference is unknown; however, it cannot be attributed to the Danish participants being more experienced IC users; the median time using catheters was greater in France than in Denmark. These variations could be attributed to cultural differences; however, as this trial was not designed to investigate these potential differences, it is difficult to speculate much further.
The main limitation of this study was its open-label design, which could have led to possible bias. Unfortunately, this was unavoidable because the two catheters were of different sizes and blinding was not possible; this is often the case for trials of medical devices and/or equipment, including catheters.
In conclusion, the new male compact hydrophilic-coated catheter is at least as acceptable to the user as the standard catheter with respect to the level of discomfort during catheterisation. Secondary endpoints also suggest that there are advantages of using the compact catheter, particularly with regards to discretion and ease of use.
References
Stöhrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol 2009; 56: 81–88.
Hansen RB, Biering-Sørensen F, Kristensen JK . Bladder emptying over a period of 10-45 years after traumatic spinal cord injury. Spinal Cord 2004; 42: 631–637.
Consortium for Spinal Cord Medicine. Bladder Management for Adults with Spinal Cord Injury: A Clinical Practice Guideline for Health Care Providers. Paralyzed Veterans of America: Washington, DC, 2006 (ISBN: 0-929819-19-5).
Lapides J, Diokno AC, Silber SJ, Lowe BS . Clean, intermittent self-catheterisation in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Shaw C, Logan K, Webber I, Broome L, Samuel S . Effect of clean intermittent self-catheterization on quality of life: a qualitative study. J Adv Nurs 2008; 61: 641–650.
van Achterberg T, Holleman G, Cobussen-Boekhorst H, Arts R, Heesakkers J . Adherence to clean intermittent self-catheterization procedures: determinants explored. J Clin Nurs 2008; 17: 394–402.
De Ridder DJ, Everaert K, Fernández LG, Valero JV, Durán AB, Abrisqueta ML et al. Intermittent catheterisation with hydrophilic-coated catheters (SpeediCath) reduces the risk of clinical urinary tract infection in spinal cord injured patients: a prospective randomised parallel comparative trial. Eur Urol 2005; 48: 991–995.
Liu CW, Attar KH, Gall A, Shah J, Craggs M . The relationship between bladder management and health-related quality of life in patients with spinal cord injury in the UK. Spinal Cord 2010; 48: 319–324.
Chartier-Kastler E, Denys P . Intermittent catheterisation with hydrophilic catheters as a treatment of chronic neurogenic urinary retention. Neurourol Urodyn 2011; 30: 21–31.
Logan K, Shaw C, Webber I, Samuel S, Broome L . Patients’ experiences of learning clean intermittent self-catheterization: a qualitative study. J Adv Nurs 2008; 62: 32–40.
Kohler TS, Yadven M, Manvar A, Liu N, Monga M . The length of the male urethra. Inter-national Braz J Urol 2008; 34: 451–456.
Bagi P, Hannibalsen J, Permild R, Stilling S, Looms D . Safety of a new compact male intermittent catheter: a randomised, cross-over, single blind study in healthy male volunteers. Urol Int (e-pub ahead of print 27 Januray 2011).
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al., ASIA Neurological Standards Committee 2002. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Stensballe J, Looms D, Nielsen PN, Tvede M . Hydrophilic-coated catheters for intermittent catheterisation reduce urethral micro trauma: a prospective, randomised, participant-blinded, crossover study of three different types of catheters. Eur Urol 2005; 48: 978–983.
Domurath B, Kutzenberger J, Kurze I, Knoth HS . Residual urine after intermittent catheterization in males using a newly developed catheter (SpeediCath Compact Male) and a conventional catheter for males (SpeediCath). Spinal Cord (in press).
Biering-Sørensen F, Hansen HV, Nielsen PN, Looms D . Residual urine after intermittent catheterization in females using two different catheters. Scand J Nephrol Urol 2007; 41: 341–345.
Acknowledgements
We would like to thank Dr A Even-Schneider (neurourology unit, HR Poincaré, Garches, France), Linda Goodall (Clinic for Spinal Cord Injuries, Hornbæk, Denmark), Katrine Nymand (Clinic for Spinal Cord Injuries, Hornbæk, Denmark), Hanne Vest Hansen (Clinic for Spinal Cord Injuries, Hornbæk, Denmark), Marie-Christine Bonneton (Hospital Henry Gabrielle, France), Mireille Bonnin (Hospital Henry Gabrielle, France) and Susanne Døssing (Paraplegifunktionen, Viborg, Denmark) for their valuable assistance during the study. We would also like to acknowledge Carsten Henrik Wachmann for assistance with the statistical analysis, supported by Coloplast and Anna Karina Busch, PhD of Coloplast A/S for technical review and assistance with editing the manuscript. Medical writing assistance, including co-ordination of drafting the manuscript and consolidation of comments, was provided by Tom Newton of Elements Communications Ltd, UK, supported by Coloplast. Clinical trial registration number (ClinicalTrials.gov): NCT00990093.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Emmanuel Chartier-Kastler has been a trial investigator for Coloplast, Astellas, Allergan, Ipsen Biotech, Medtronic and AB Sciences. He has also received speaker's fees from Coloplast, Astellas and Medtronic and has been a consultant for Astellas, Allergan and Zambon. Alain Ruffion received compensation as member of advisory boards from Astra Zeneca, Colopast, Allergan and Ipsen Bitoech and has been a trial investigator for Medtronic, Allergan and Astellas. He has given lectures in meetings organised by Takeda, Ipsen and Coloplast. Fin Biering-Sørensen has given educational lectures for personnel in Coloplast. He is a member of Coloplast Clinical Advisory Board for Spinal Cord Injuries and Chair of the Coloplast symposium on late complications after spinal cord lesion. Two nurses in the Clinic for Spinal Cord Injuries, Hornbæk had the time they used on the study funded by Coloplast. Kathleen Charvier, David Goossens and Inger Lauge declare no potential conflict of interest.
Rights and permissions
About this article
Cite this article
Chartier-Kastler, E., Lauge, I., Ruffion, A. et al. Safety of a new compact catheter for men with neurogenic bladder dysfunction: a randomised, crossover and open-labelled study. Spinal Cord 49, 844–850 (2011). https://doi.org/10.1038/sc.2011.5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.5
Keywords
This article is cited by
-
Outcome comparison of different approaches to self-intermittent catheterization in neurogenic patients: a systematic review
Spinal Cord (2017)
-
Voiding Dysfunction and Upper Tract Deterioration after Spinal Cord Injury
Current Bladder Dysfunction Reports (2013)
-
Hydrophilic catheters are safe and effective for men with spinal cord injury
Nature Reviews Urology (2011)