Abstract
Study design:
Community-based, cross-sectional study.
Objectives:
This study aimed at examining and comparing the pharmacological treatments administered to traumatic and nontraumatic spinal-cord-injured patients (TSCI, NTSCI).
Setting:
The Interval Rehabilitation Center, Trois-Rivieres, Province of Quebec, Canada.
Methods:
Medical records from a cohort of 175 chronic spinal-cord-injured patients (94 TSCI and 81 NTSCI individuals) were thoroughly studied.
Results:
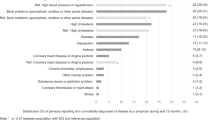
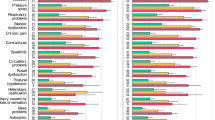
More than 19 classes and more than 300 drugs were found to be administered to SCI patients. Among them, drugs against bowel and bladder problems, blood clot or deep venous thrombosis, cardiovascular problems, depression or anxiety, stomach acidity, infections, pain, inflammation, sleeping problems and vitamin deficiency were the most commonly used (between 35 and 66% of all SCI patients). Differences between groups were found specifically for antidepressants and anxiolytics used mainly by TSCI patients whereas bisphosphonates, bronchodilators, lipid regulators and anti-inflammatory drugs were used mainly by NTSCI patients.
Conclusion:
The results revealed an unexpectedly large number of drugs that are prescribed to both groups of SCI patients. Given the existence of between-group differences and known risks of drug–drug interactions, it is suggested that recommendations for each group should be made to carefully examine either the necessity or the effectiveness of each treatment as well as the possibility of developing alternative strategies based on physical activity, nutrition and lifestyle to eventually reduce, hopefully, the number of pharmacological treatments administered to these individuals.
Similar content being viewed by others
Introduction
Traumatic spinal-cord-injured (TSCI) and nontraumatic spinal-cord-injured (NTSCI) patients typically undergo an irreversible loss of sensory and voluntary motor functions and experience multiple health problems (see companion article no. 1).1 SCI patients are known to receive a variety of pharmacological treatments for these health problems. However, differences between TSCI and NTSCI patients in this regard remain unclear. Given the increasingly clear specificity of these groups and subgroups of patients (for example, epidemiologically, functionally, biochemically, see companion articles),1, 2 it may be expected that pharmacological treatments administered to TSCI and NTSCI patients should be specifically adapted and, thus, different in each group and subgroups of SCI patients. Here, the main aim was to assess and directly compare in a relatively homogenous community (Trois-Rivieres City, Quebec, Canada), the list of drugs and drug classes prescribed to or used by TSCI and NTSCI patients. This article is the third of a series of three articles aimed to describe the epidemiological, clinical, functional (first article)1 and biochemical (second article)2 characteristics associated with TSCI and NTSCI patients.
Materials and methods
This protocol was approved by the institution from where the medical records were obtained (Interval Rehabilitation Center, Trois-Rivieres, Quebec, Canada) as well as by an independent ethic committee (International Review Board Services, Aurora, Ontario, Canada). We studied data from male (97) and female (54) patients (n=151) from the Interval Rehabilitation Center that have been SCI traumatically (82 patients; paraplegic incomplete (22 men and 7 women), paraplegic complete (13 men and 2 women), tetraplegic incomplete (14 men and 8 women) tetraplegic complete (9 men and 3 women) and unknown (2 men and 2 women) or nontraumatically (69 patients; paraplegic incomplete (16 men and 18 women), paraplegic complete (1 man and no woman), tetraplegic incomplete (19 men and 14 women) tetraplegic complete (no one) and unknown (1 man and no woman) for at least 1 year and typically less than 10 years. For additional methodological details, refer to companion articles.1, 2 All drugs assessed were classified by classes (utility) and reported as incidences.
Results
Bone and muscle loss
The results showed that drugs typically used for osteopenia and osteoporosis were administered to a significant number of TSCI and NTSCI patients (Table 1). Among these drugs, bisphosphonates, such as alendronate sodium (Fosamax) and risedronate (Actonel), raloxifene (Evista, estrogen receptor ligand), calcitonin salmon (Miacalcin), disodium pamidronate (Aredia) and calcium carbonate (Calcite), were prescribed to 13.2% of all SCI patients. However, clearly more NTSCI (20.3%) than TSCI patients (7.3%) received this class of medication. It is worth mentioning also that among all SCI patients, the incidence was particularly high in women (25.9% of all SCI women) compared with men (only 6.2% of all SCI men). In turn, no drugs against skeletal muscle loss or so-called muscle wasting were administered to these patients.
Bowel and bladder problems
We found several compounds normally used to treat bowel problems (typically constipation) as well as to improve bladder function (Tables 2 and 3). In fact, laxatives were by far the most often prescribed class of medication among all drugs and classes administered to these SCI patients. A total of 265 prescriptions were made for drugs such as docusate sodium (Docusate/Colace, 26.8%), senna glycosides (Senokot, 18.5%), bisacodyl (Dulcolax, 15.8) and glycerin suppository (13.6%). More TSCI patients (73.2%) were given laxatives compared with NTSCI patients (43.5%), suggesting that this particular problem was more often encountered after chronic TSCI. A total of 71 prescriptions for bladder function (specifically diuretics) were found among all SCI medical records (Table 3). Among all TSCI and NTSCI patients, respectively 40.2 and 34.8% of them received a diuretic such as oxybutynin chloride (Ditropan, 42.3% of all diuretics), hydrochlorothiazide (Apo-hydro, 16.9%) and tolterodine L-tartrate (Detrol, 8.5%). The subgroup that most often received diuretics was by far the complete TSCI paraplegic patients (73.3% of all TSCI paraplegics; Table 3).
Blood (anemia) and coagulation problems
Anemia is a well-recognized problem found after SCI typically in the acute and early chronic phases (see companion article no. 1). We found two classes of drugs administered to both TSCI and NTSCI patients, namely the iron supplements (Table 4) and anticoagulating compounds (Table 5). Approximately one patient out of ten (11.9%) received ferrous sulfate (FeSO4) or ferrous fumarate (Palafer) after TSCI (8%) and NTSCI (14%) (Table 4). In contrast, about one-third of all SCI patients (34.1% TSCI and 33.3% NTSCI) received anticoagulants such as heparin sodium (Heparin), enoxaparin sodium (Lovenox), warfarin sodium (Coumadin) or dalteparin sodium (Fragmin) (Table 5).
Cardiovascular problems and dyslipidemia
Cardiovascular problems include a rather large group of different drugs. In this study, it included treatments such as calcium channel blockers (for example, amlodipine besylate (Norvasc), diltiazem HCl (Cardizem), β-blockers (for example, bisoprolol fumarate (Monocor), metoprolol tartrate (Lopressor), angiotensin-converting enzyme inhibitors (ramipril (Altace), fosinopril sodium (Monopril), angiotensin II receptor antagonists and other antihypertensive drugs (α-2 agonists, diuretic/antihypertensive drugs) among the most popular ones (Table 6). Nearly one-third of all SCI patients (34.4%) received a drug for cardiovascular problems. Indeed a significant proportion of TSCI (29.3%) and NTSCI (40.6%) patients with nearly as many men and women received at least one of the so-called cardiovascular treatments. Their use did not apparently depend on the completeness or level of injury (ranging between 25.7 and 41.8% in each subgroup—for example, 33.3% of all complete SCI patients received at least one of these drugs). However, one of the main risk factors associated with cardiovascular problems is dyslipidemia. Consequently, it is not surprising to find that many SCI patients were also given drugs to control serum lipid levels. A significant number of SCI patients (16.6%) received at least one drug of this class (Table 7). Among the most popular treatments, we found fenofibrate (Lipidil) and statins, such as atorvastatin calcium (Lipitor, 66.7% of all drugs in this class), simvastatin (Zocor), pravastatin sodium (Pravachol) and rosuvastatin calcium (Crestor), used by 12.2% of TSCI and 21.8% of NTSCI patients (again, no complete NTSCI patients received drugs from this class).
Diabetes
Type II diabetes is well known to occur in chronic SCI patients. The results showed that 14.6% of all patients in this study received at least one treatment against type I (for example, insulin) or most typically against type II diabetes (that is, generally acting on hyperglycemia) including biguanides (metformin chloride), glibenclamide or sulfonylureas (Diabeta), pioglitazone (actos), gliclazide (diamicron), rosiglitazone (Avandia), sulfonylureas (tolbutamide, sympathomimetic drug) (Table 8). A clear difference was found between groups as 8.5% of TSCI and 21.7% of NTSCI patients received at least one of these drugs.
Depression
The results revealed that a significant proportion of SCI patients were treated for depression or anxiety (Table 9). Indeed, 38.4% of them received at least one antidepressant or anxiolytic drug. Interestingly, the proportion of patients receiving some of these drugs was greater in the TSCI group (50.0%) than the NTSCI group (24.6%). No clear differences between men and women or between injury level and completeness were found.
Respiratory problems (bronchodilators)
The control breathing and other respiratory problems (infection or inflammation related) are often found in tetraplegic and high paraplegic patients. Here, we identified that 13.9% of all SCI patients were given bronchodilators (generally β-2 agonists, anticholinergic drugs and/or corticosteroids) such as salbutamol sulfate (Ventolin, 51.6% of all bronchodilators), fluticasone/salmeterol (Advair), glucocorticoid (Pulmicort), terbutaline (Bricanyl), tiotropium (Spiriva) and others (Table 10). It was found that 8.5% of TSCI patients and 20.2% of NTSCI patients received at least one of these drugs.
Skin problems (inflammatory dermatosis)
We found in this study that treatments such as anti-inflammatory drugs were used to treat inflammatory dermatosis. Among them, we identified urea 20% (Uremol), corticosteroid (Betaderm), betamethasone valerate (Celestoderm), fluocinocide emollient cream (Tiamol) and desoximetasone (Topicort), which were occasionally administered to 9.7% of TSCI and 5.7% of NTSCI patients (Table 11).
Stomach acidity
Acid stomach problems were treated in a significant proportion of SCI patients (35.1%; Table 12). Proton pump inhibitors such as pantoprazole sodium (Pantoloc, 40% of the prescription in this class) and esomeprazole magnesium (Nexium) as well as other subtypes including ranitidine hydrochloride (Zantac, histamine antagonist) or aluminum hydroxide (Maalox) were among the most frequently found antacid treatments.
Thyroid problems
We found 7.2% of all patients were given levothyroxine (Synthroid), a synthetic thyroid hormone replacement treatment (Table 13). A comparable number of TSCI (4.8%) and NTSCI patients (10.1%) received at least one of these drugs.
Vitamin deficiency
A large proportion of SCI patients (29.8%) were given vitamin supplements probably to treat vitamin deficiencies. Among them, we found calcium carbonate (24.5% of all compounds in this class), multivitamins (Centrum and Fortamines 10, 17.8%), potassium chloride (16.4%), vitamin D (15.1%), vitamin B1 (12.3%) and others. More NTSCI (40.5%) than TSCI (20.7%) patients received one of these supplements (Table 14).
Chronic pain, sleep disorders and benzodiazepines
This class of drugs was among the most commonly prescribed compounds found in this study. A majority of SCI were (57.6%) given pain killers (often to reduce sleeping disorders) such as hydromorphone HCl (Dilaudil, 33.1% in this class), acetaminophen-codeine phosphate (Empracet, 17.6%), morphine sulfate (Morphine, 16.2%), codeine sulfate (Codeine, 7.4%) and others (Table 15). No clear differences between men and women or between subgroups associated with the extent or completeness of lesion were found. A comparable proportion of TSCI (58.5%) and NTSCI (56.5%) patients received drugs from this class. Benzodiazepines (Table 16) were often prescribed to treat sleeping problems. It constituted one of the most widely used class of medication in this study with 51% of all SCI patients who receive at least one of these drugs. Approximately as many TSCI (50% of this group) and NTSCI (52% of this group) patients were given this type of medication, strongly suggesting that sleeping problems were typically found in both groups of SCI patients.
Mild pain and fever
Almost 60% (59.6%) of all SCI patients were found to receive acetaminophen (Tylenol), acetylsalicylic acid (for example, Aspirin) or ibuprofen (Advil). Again, no clear differences between men and women or injury level/extent were found (Table 17).
Infections
Nearly one-third of all SCI patients received either an antibacterial (93 prescriptions), antifungal (16 prescriptions) or antiviral (3 prescriptions) medication (Table 18). Forty percent (40%) of TSCI and 34.8% of NTSCI patients were given one of these drugs. In this class of compounds, a clear trend was found to be associated with the extent of injury as most patients that received them had complete lesion (73.3 and 83.3% among the subgroups of patients with complete paraplegia and tetraplegia, respectively).
Inflammations
Drugs against inflammation were either nonsteroidal anti-inflammatory drugs (such as naproxen sodium (Anaprox), naproxen (Naprosyn), indomethacin (Indotec), corticosteroids (for example, dexamethasone (Decadron), cortisone acetate (Cortone), methylprednisolone acetate (Depo-Medrol), COX-2 selective inhibitors (that is, celecoxib (Celebrex) synthetic prostaglandins (for example, diclofenac sodium-misoprostol (Arthrotec) and misoprostol (Apo-Misoprostol) often used with nonsteroidal anti-inflammatory drugs). Approximately 31% of all SCI patients received at least one drug from this class of treatments. Interestingly, a clearly greater proportion of NTSCI patient (42% of this group) compared with TSCI patients (23% of this group) received these drugs (Table 19).
Discussion
This study is the first to describe an extensive list of drugs generally administered to SCI patients. More than 19 classes of compounds including more than 300 drugs were identified. Drug treatments against bowel and bladder problems, blood clot and deep vein thrombosis (DVT), cardiovascular problems, depression/anxiety, stomach acidity, infections, inflammation, sleep problems, pain and vitamin deficiency were clearly among the most commonly used classes of compounds (between 35 and 66% of all SCI patients). Other pharmacological classes (that is, against bone loss, anemia, dyslipidemia, diabetes, respiratory problems, dermatosis or thyroid problems) were also significantly used (that is, between 10 and 20% of all SCI patients). However, we found absolutely no medication given specifically for muscle atrophy or hormonal dysregulation, which are also well-known secondary complications generally found in chronic SCI patients (see companion article no. 1).1 Reasons for this remain unclear but may include incomplete medical records (for example, specific classes of drugs may not have been systematically reported in the records) or institution-based beliefs that some of the secondary complications should not be treated. Also, for some specific problems, such as anemia, that are generally recognized to be found in the acute hospitalization or early chronic phase (companion article no. 2)2, 3, 4, 5 pharmacological data may have been lacking in the rehabilitation-based medical records (normally covering the period between early chronic and late chronic phases). This said, drugs against coagulation (34% of all patients) were more extensively used than iron supplements (12% of all patients) although DVT is also generally found soon after trauma. However, in contrast with anemia, which is generally mild in SCI patients, DVT is a serious vascular complication that significantly increases the risks of pulmonary embolisms.6 Unfortunately, the incidence of pulmonary embolisms caused by DVT has been shown to remain elevated in SCI patients despite prophylaxic approaches,7, 8, 9 which is probably why medication was commonly used as shown in this study.
Dyslipidemia is generally known to occur progressively in TSCI patients. For instance, we found in the companion article no. 2 that abnormal lipid levels (that is, high triglyceride, total cholesterol, low-density lipid cholesterol) tend to be worst in NTSCI patients (for example, high total cholesterol even in late chronic NTSCI patients and higher LDL in late NTSCI patients compared with late TSCI ones). Accordingly, the results showed that drugs such as atorvastatin calcium were indeed commonly administered to NTSCI (22% of the group) and to a lesser extent to TSCI patients (12% of the group).
Regarding drugs against bone loss, it was rather surprising to find that a significant, but yet, a rather small proportion of patients (13% on average) were given bisphosphonates. Indeed, osteopenia and osteoporosis are generally considered to be widely found among chronic SCI patients (studied essentially in TSCI patients) as it has been reported that nearly all complete SCI individuals experience a significant loss of bone mineral tissue (up to 30% in the femora) leading to a marked increase of fracture incidence within 1 year after injury.10, 11, 12, 13, 14 Consequently, we did not expect only 13% of the patients to receive bisphosphonates as a much greater proportion should have been experiencing extensive bone loss. Unfortunately, dual-energy X-ray absorptiometry data were not available in the records studied. In addition, our study results showed clearly that more NTSCI patients (20% of this group) compared with TSCI patients (7% of the TSCI group) were given bisphosphonates, strongly suggesting that bone loss was probably more common (or to a greater level) in NTSCI than TSCI patients.
It was also particularly surprising to find that bronchodilators were more commonly given to NTSCI (20.2% of them) than TSCI (8.5% of them) patients. Indeed, to the best of our knowledge, pulmonary problems have been essentially studied in TSCI patients although our study results strongly support the idea that pulmonary problems are greater (or more commonly found) in NTSCI patients. However, the opposite trend was found with antidepressant and anxiolytic drugs that were found, here, to be mainly given to TSCI patients (50.0% of this group) and to a lesser extent to NTSCI individuals (24.6% of the NTSCIs).
Infections and pain (either chronic or mild) are typically found in SCI patients.15, 16, 17 Here, the results showed that almost as many patients from both groups TSCI and NTSCI were found to use these classes of treatments. These drugs were clearly found to be among the most commonly used classes of drugs in SCI patients (for example, drugs against infections were used by 75% of the complete SCI patients).
All and all, a wide variety of drugs were found to be prescribed to SCI patients. Moreover, additional drugs (not listed in the Results section) were also found, although only occasionally, to be given to these patients such as tadalafil (Cialis), sildenafil citrate (Viagra), conjugated estrogens (Premarin), naratriptan HCl (Amerge), sumatriptan (Imitrex), gout therapy (Colchicine), allopurinol (Zyloprim), botulinum toxin type A (Botox), ondansetron (Zofran), betahistine dihydrochloride (Serc), barbiturates (Phenobarbital), zopiclone (Rhovane), methylphenidate HCl (Ritalin), cyproheptadine HCl (Periactin), probaclac (Bifilact), hydrocortisone acetate-zinc sulfate (Anusol-HC), benzoylperoxide (Benzogel), calcium carbonate (Tums) and so on.
Conclusion
This study strongly supports the idea that different pharmacological approaches are occasionally used for TSCI and NTSCI patients. Although, some classes of drugs expected to be used by SCI patients were not given to these patients (for example, hormonal replacement therapy), an unexpectedly large number of classes and drugs were nonetheless routinely prescribed to both groups of patients (with some between-group differences). Recommendations should be made by experts to carefully examine either the necessity or the effectiveness of each treatment as well as the possibility of developing alternative strategies based on physical activity, nutrition and lifestyle.
References
Rouleau P, Ayoub E, Guertin PA . Traumatic and non traumatic spinal cord-injured patients in Quebec, Canada. Part 1—epidemiological, clinical and functional characteristics. World Scientific Journal (in revision).
Rouleau P, Guertin PA . Traumatic and non-traumatic spinal cord-injured patients in Quebec, Canada. Part 2: biochemical profile. Spinal Cord 2010 (e-pub ahead of print 11 May 2010; doi:10.1038/sc.2010.42).
Gurcay E, Bal A, Gurcay AG, Cakci A . Evaluation of blood and serum markers in spinal cord injured patients with pressure sores. Saudi Med J 2009; 30: 413–417.
Perkash A, Brown M . Anemia in patients with traumatic spinal cord injury. J Am Paraplegia Soc 1986; 9: 10–15.
Huang CT, DeVivo MJ, Stover SL . Anemia in acute phase of spinal cord injury. Arch Phys Med Rehabil 1990; 71: 3–7.
Waring WP, Karunas RS . Acute spinal cord injuries and the incidence of clinically occurring thromboembolic disease. Paraplegia 1991; 29: 8–16.
Chen D, Apple DF, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury—current experience of model systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Deep K, Jiagajinni MV, Mclean AN, Fraser MH . Prophylaxis of thromboembolism in spinal injuries—results of enoxaparin used in 276 patients. Spinal Cord 2001; 39: 88–91.
Kadyan V, Clinchot DM, Mitchell GL, Colachis SC . Surveillance with duplex ultrasound in traumatic spinal cord injury on initial admission to rehabilitation. J Spinal Cord Med 2003; 26: 231–235.
Ragnarsson KT, Sell GH . Lower extremity fractures after spinal cord injury: a retrospective study. Arch Phys Med Rehabil 1981; 62: 418–423.
Garland DE, Stewart CA, Adkins RH, Hu SS, Rosen C, Liotta FJ, Weinstein DA . Osteoporosis after spinal cord injury. J Orthop Res 1992; 10: 371–378.
Wilmet E, Ismail AA, Heilporn A, Welraeds D, Bergmann P . Longitudinal study of the bone mineral content and of soft tissue composition after spinal cord section. Paraplegia 1995; 33: 674–677.
Lazo MG, Shirazi P, Sam M, Giobbie-Hurder A, Blacconiere MJ, Muppidi M . Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord 2001; 39: 208–214.
Sabo D, Blaich S, Wenz W, Hohmann M, Loew M, Gerner HJ . Osteoporosis in patients with paralysis after spinal cord njury. A cross sectional study in 46 male patients with dual-energy X-ray absorptiometry. Arch Orthop Trauma Surg 2001; 121: 75–78.
Salle JY, Ginies P, Perrouin-Verbe B, Ventura M . Pain management: what's the more efficient model? Ann Phys Rehabil Med 2009; 52: 203–209.
Everaert K, Lumer N, Kerckhaert W, Willaert P, Van Driel M . Urinary tract infections in spinal cord injury: prevention and treatment guidelines. Acta Clin Belg 2009; 64: 335–340.
Burns SP . Acute respiratory infections in persons with spinal cord injury. Phys Med Rehabil Clin N Am 2007; 18: 203–216.
Acknowledgements
We thank the Interval Rehabilitation Center for its collaboration and devoted work in retrieving the corresponding medical files and, occasionally, some missing information. We acknowledge the support from Nordic Life Science Pipeline and NeuroSpina Therapeutics for this 3-year study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rouleau, P., Guertin, P. Traumatic and nontraumatic spinal-cord-injured patients in Quebec, Canada. Part 3: pharmacological characteristics. Spinal Cord 49, 186–195 (2011). https://doi.org/10.1038/sc.2010.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.70
Keywords
This article is cited by
-
Prescription medication cost, insurance coverage, and cost-related nonadherence among people with spinal cord injury in Canada
Spinal Cord (2020)
-
Special considerations in the urological management of the older spinal cord injury patient
World Journal of Urology (2018)
-
Vitamin D and spinal cord injury: should we care?
Spinal Cord (2016)
-
Medication profile and polypharmacy in adults with pediatric-onset spinal cord injury
Spinal Cord (2015)