Abstract
Study design
Explorative retrospective cohort study.
Objective
Secondary health conditions (SHCs) are common in people with spinal cord injury (SCI). To date, little is known about the effectiveness of long-term follow-up care in preventing SHCs. The objective of this study was to explore the therapeutic content of an interdisciplinary follow-up clinic by retrospective analyses of provided recommendations and collected data concerning SHCs.
Setting
Rehabilitation center Sint Maartenskliniek, The Netherlands.
Methods
All people with SCI, who visited one or more outpatient interdisciplinary follow-up clinics between January 2012 and October 2020 were included in this study. Treatment information was retrieved from their medical records.
Results
The 264 participants of the follow-up clinic received, after their first visit, an average of 3.9 recommendations regarding SHCs. Most recommendations were preventive in nature (43%), and were related to physical SHCs (61%). Most recommendations were followed by the participants (34% out of 40% that could be determined) and half of the underlying problems were solved (31% out of 62%). The bodyweight and respiratory function remained stable over time.
Conclusion
Participants of the interdisciplinary follow-up clinics received extensive recommendations on a variety of subjects, which most likely, reflects the interdisciplinary approach. Recommendations were followed-up to a large extent, resulting in solving half of the underlying SHCs. This way, worse SHCs were prevented by the recommendations. This findings, together with the stability of respiratory function and bodyweight, suggests the added value of the interdisciplinary follow-up clinic to usual care. More prospective research is necessary to investigate the (cost-)effectiveness.
Similar content being viewed by others
Introduction
Persons with spinal cord injury (SCI) are prone to develop secondary health conditions (SHCs), which cause an additional burden and limitation in participation [1,2,3]. In a large Dutch study focusing on health problems, on average eight different SCHs were found for each person with SCI [2]. The most common mentioned SHCs were problems with respect to; bladder regulation (71%), bowel regulation (61%), spasms (57%), pain (55%), oedema (49%), having or preventing pressure sores (36%), increasing weight (32%), excessive sweating (28%), contractures (23%), and problems with respiratory tract (19%) [2]. The SHCs are not only a burden to the people with SCI, they also cause high medical costs due to doctor visits or readmission to a hospital [4, 5].
In most Western countries, people with a SCI will be admitted to a specialized rehabilitation center shortly after their injury [6]. During inpatient rehabilitation, people with SCI are encouraged, by all members of the rehabilitation team, to develop new functional abilities and psychosocial coping skills. Further, they will learn how to deal with long-term consequences such as learning about self-management, health promotion and early intervention to manage SHCs if they do occur [7]. Once people with SCI are discharged from inpatient rehabilitation, in most countries, they mainly rely on ongoing support from the primary and community-care system for health-related questions [8]. For community-care professionals it is, however, difficult to have all necessary knowledge about SCI and the SHCs linked to SCI, as SCI is a relative rare disease (40–80 cases/million/year) [6]. While specialist’s knowledge is required, the specialists of the SCI rehabilitation center are no longer the first to respond to these health-related questions [9].
To bridge the gap between the specialists in the rehabilitation center and the community-care system there is, in some countries, a structured outpatient follow-up care by one or more specialists from the SCI rehabilitation center [10,11,12]. They vary in the number of disciplines involved (between one and four) and the way they are applied; home-based, where the professionals visit the people with SCI at home; by telemedicine; or by visits of people with SCI to the multidisciplinary team in the rehabilitation center [10, 11]. Most of the literature about follow-up care is, however, of older date.
Follow-up care for people with SCI in the Netherlands was, before 2005, formally organized as an (bi-)annual appointment to the physician, in one of the eight specialized SCI rehabilitation centers [13, 14]. The guidelines of SCI rehabilitation, formulated by the Dutch medical specialists association, recommended to plan a visit to the physician at least ones every 2 years [15]. Further, the consideration was given to plan this visit contemporary with other disciplines concerned with SCI care. While efforts in the last 15 years have focused on the organization of follow-up care in line with the guidelines, the therapeutic content is rarely investigated: not in the Netherlands nor in the rest of the world [11].
This study aims to explore the therapeutic content of an outpatient interdisciplinary follow-up clinic, organized in a carousel model, by retrospective analyses of the recommendations given to the participants and of collected data concerning SHCs (bodyweight, respiratory functioning, and presence of pressure sores or wounds).
Methods
Design and setting
Explorative retrospective cohort study of all persons with SCI who visited the interdisciplinary follow-up clinics of the Sint Maartenskliniek, Nijmegen, the Netherlands. This study was reported in accordance with STROBE guidelines [16].
Intervention
In the last 15 years the department of SCI of the Sint Maartenskliniek, one of the eight specialized SCI rehabilitation centers in the Netherlands, developed a carousel model for follow-up care in accordance with the recommendation in the Dutch SCI rehabilitation guidelines [15]. This interdisciplinary follow-up clinic is current practice. The main goal of the interdisciplinary follow-up clinic is to help people with SCI to get old in a healthy way, by giving recommendations to the participants (and the community-care providers) how to prevent new SHCs or to control existing SHCs in order to prevent more serious or irreversible problems. Considered for participation in the interdisciplinary follow-up clinic were people with a motor complete SCI, wheelchair users, or other complex physical conditions. The interdisciplinary follow-up clinic consists of an (bi-)annual appointment, depending on individual preference of the visitor and necessity estimated by the team. For each interdisciplinary follow-up clinic five people with SCI, and their informal caregivers, are invited into the rehabilitation center. For every visitor five 30 min meetings are planned with respectively a physician, a specialized nurse, a physiotherapist, an occupational therapist and with a social worker or psychologist in random order. Hence, the “carousel” model. All five participants start at the same time, are welcomed by a nurse of the team and receive the schedule for the day. During the meetings with all five disciplines an assessment of potential problems is made. Meanwhile, information is provided regarding the hazards of potential SHCs and prevention strategies. The physicians focus on medication, physical complaints and overall physical functioning. The specialized nurse concentrates on bowel and bladder problems and management, nutrition, possible skin problems, and self-care. The physiotherapist measures respiratory function, and assesses functional activities like transfers, mobility of the legs, and sports activities. The occupational therapist focuses on the position in the wheelchair, devices (like wheelchairs and home adjustments) and possible changes in functionality of the upper limbs. The social worker or psychologist focuses on possible problems with financial bodies, home care, transportation, participation, work, and psychological adjustment to SCI. The nurse of the team weighs all participants. After the first three meetings there is a 30 min break were all participants can have something to drink and socialize with the other participants and team members. After a total of 3 h the participants are sent home. The team members share their findings and formulate their recommendations in a letter, which is sent to the general practitioner. The recommendations are also discussed by phone with the participants the week after their appointment.
Participants
For this study, cases were identified from the electronic patients files of the Sint Maartenskliniek. All people with SCI, that visited one of the interdisciplinary follow-up clinics in the period January 2012 to October 2020 were included in this study.
Procedure
All records of people with SCI who visited at least one of the interdisciplinary follow-up clinics were identified. Next, information about the treatment plan, as formulated in the letter to the general practitioner, was retrieved from their medical records. Records were classified by two members of the research team (TvD and ML’H) to reach consensus about the division of the recommendations to different domains and categories. Afterwards all records were classified by one person (ML’H) with a medical background and randomly controlled by the other team member. Data was processed anonymously. In case of multiple visits, every next visit the letter to the general practitioner was carefully read to see if the recommendations were followed by the participant, whether the underlying problem was resolved (as judged by the interdisciplinary team) and if not, whether a new recommendation by the interdisciplinary team was provided for the persisting SHC.
Measures
Participants demographics (sex, age, and weight), SCI characteristics (level and completeness of injury, time since injury) and the presence of pressure sores or wounds were retrieved from the letter to the general practitioner. Some participants acquired the SCI many years ago, before standardized measuring of level and completeness, resulting in a loss of some aspects of the SCI in the medical records.
For participants with SCI level thoracic 6 or higher the respiratory function was determined, during their meeting with the physiotherapist, with a standardized spirometer a MicroPlus (from MicroDirect) or with a Micro I (from CareFusion), while seated in their wheelchair. Three repeated forced flow volume curves were made and the highest outcome of the forced vital capacity (FVC), peak expiratory flow (PEF), and forced expiratory volume in 1 s (FEV1), was used. FVC, PEF, and FEV1 were expressed as a percentage of the predicted values based on able-bodied persons of the same age, gender, height and ethnic background. Change in percent-predicted FVC, PEF, and FEV1 were calculated between the consecutively follow-up visits.
The interdisciplinary recommendations retrieved from the letter to the general practitioner, were divided into seven categories of physical problems: Pain, spasms, skin problems, bowel problems/management, bladder problems/management, respiratory problems, and medical intercurrent (all other medical problems not covered by the previous); and six categories of other problems: Splints, seating advice (position in wheelchair), functioning (transfers, standing, and arm functioning), devices, social issues, and psychological problems.
Each recommendation was divided into one of the following four categories: (1) preventive in nature that could be applied by the participant at home, (2) the recommendation concerned further rehabilitation treatment within the SCI department of the Sint Maartenskliniek, (3) the recommendation concerned other treatment (e.g., in a hospital or a recommendation or instruction that could be applied by a primary healthcare professional), and (4) or was a (medication) prescription or reimbursement healthcare insurance.
Statistical analyses
Descriptive statistics were performed for all collected variables. The continuous data were presented as means with Standard Deviation (SD). Categorical data were presented using counts and percentages. Change scores were calculated for bodyweight and respiratory function between the consecutive timepoints, and analyzed by paired samples t test, after testing for normality. Difference in presence of pressure sores or wounds was analysed with McNemar related-sample change test. P values lower than 0.05 were considered statistically significant. All analyses were conducted using SPSS for Windows (version 25) (IBM corp, Armonk, NY).
Results
A total of 264 persons with SCI visited the interdisciplinary follow-up clinics at least once during the inclusion period. The characteristics of the participants at the time of their first visit are described in Table 1.
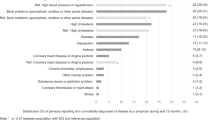
Table 2 shows the total number of recommendations given as a result of the first interdisciplinary follow-up clinic. For the 264 cases in this study a total of 1026 recommendations were given with an average 3.9/participant (range; 0–11). Most recommendations were preventive in nature that could be applied at home (42.5%) of which most were medical intercurrent (20.8%) followed by recommendation with respect to bladder problems (13.4). In general, almost two-third of the recommendations were related to physical SHCs (61.3%).
Table 3 shows the assessments collected during the consecutive interdisciplinary follow-up clinics. The number of participants that visited six, seven, and eight times the interdisciplinary follow-up clinic during the inclusion period were respectively 14, seven and one. Due to the small numbers these were not depicted in the table.
The percentage of pressure sores and wounds present in various parts of the body, varied between 15 and 24% of the population. There was a normal distribution for weight except for the first measurement, revealing two outliers. No significant changes were observed regarding average weight (p > 0.05) indicating stable weight over time, although there were large individual differences (range of weight change: −21.5 to +16.2 kg). All measurements of respiratory functions were normally distributed expect for FEV1 at the fourth follow-up clinic, based on one outlier. No significant changes were observed regarding FVC (p > 0.05) indicating stable average FVC over time, while the average PEF appears to improve at the fourth and fifth interdisciplinary follow-up clinic and the average FEV1 showed an improvement at the fifth. None of these finding changed after leaving out outliers from analyses.
The 208 participants that visited the second interdisciplinary follow-up clinic received a total of 794 recommendations during their first follow-up clinic. Of these recommendations, 34% were followed-up by the participants, 7% were not, and from almost 60% it was unfortunately not registered if the recommendation were carried out. Of the problems underlying the recommendations, 31% were solved, 30% were not solved and in 38% of the cases it was not registered. Of the 786 recommendations given during the second interdisciplinary follow-up clinic, 175 (22%) were new recommendations given for the problems not being solved. This pattern was similar in later interdisciplinary follow-up clinics.
Discussion
The objective of this study was to explore the therapeutic content of an interdisciplinary follow-up clinic addressing SHCs following SCI, by retrospective analyses of the recommendations given to the participants and of collected data concerning SHCs. The participants of the interdisciplinary follow-up clinic received an average of 3.9 recommendations. Most of these recommendations (42.5%) were preventive in nature that could be applied at home. Of these preventive recommendations, most were medical intercurrent of origin, followed by recommendations with respect to bladder problems/managements, devices and functioning. Most recommendations were related to a physical SHCs. These findings align with the goals of the interdisciplinary follow-up clinic which is to give recommendations regarding how to prevent new SHCs form occurring, or to control existing SHCs, in order to prevent more serious or irreversible problems.
The distribution of the recommendations related to SHCs, correspond largely to the most experienced health problems of community dwelling people with SCI in the Netherlands; this is bladder regulation, bowel regulation, pain, and spasms [2]. An explanation that the recommendations and the previous found health problems do not fit exactly could be found in the purpose of the interdisciplinary follow-up clinic, which was to prevent SHCs and not to solve all SHCs. Some of these SHCs may be present for longer time, without the possibility of new treatment or preventive options to control the SHC. The interdisciplinary follow-up clinic is an addition to community care, which people with SCI primarily visit in case of SHC. The average number and diversity of the recommendations suggest and point towards an added value of the interdisciplinary nature of the clinic and the specific knowledge of the professionals.
As part of the interdisciplinary follow-up clinic most people were weighed, and respiratory functions were measured if participants had a lesion above thoracic 6. The average bodyweight remained stable, although there were large individual differences. This is in contrast with literature, describing increased body weight over time [2, 3, 17, 18]. Also the respiratory function was stable or even improving over time for the participants who frequently visited the interdisciplinary follow-up clinic. There might be a bias in these findings as not all participants visited the interdisciplinary follow-up clinic more than once. The finding of a stable respiratory function is in contrast with former studies of people with SCI in the chronic phase, where a decline of respiratory functioning was shown over an average of 7.5 years [19]. In that study was concluded that one of the significant determinants of the longitudinal decline was an increase in bodyweight, beside smoking and wheezing [19]. The participants in this study had, on average, a stable bodyweight, further they were given recommendations regarding adequate respiratory management, including respiratory muscle training. These findings point towards the preventive value of the interdisciplinary follow-up clinic as described in this paper.
The idea for multidisciplinary follow-up care for people with SCI is not new, and is applied in different ways in different parts of the world [10, 11], also in other diagnostic groups [20,21,22]. A structured way of organizing the follow-up care, especially in an interdisciplinary approach, has the advantage of covering most important areas of SHCs and combining the available expertise. For the participants of the follow-up clinic described in this paper, an extra dimension was the possibility they had to socialize with the other participants and team members during the break, sharing information and experiences.
However, from this retrospective study we do not know if there were more or other recommendations given as a result of the interdisciplinary follow-up clinic compared to other forms of follow-up care (for instance only visiting a physician). It seems, however, plausible that it is not possible for one discipline as for the primary care to cover the full pallet of recommendations, apparently needed to cover the wide variation in SHCs following SCI. This is closely related to the aspect is the cost-effectiveness of the interdisciplinary follow-up clinic. Former research has investigated the direct healthcare costs of people with SCI; on average $21450,- per patient per year [23]. From the current study it seems plausible that the interdisciplinary follow-up clinic prevents weight gain and decline in respiratory function. Further, at least 31% (out of 61% that could be determined) of the underlying problems were solved with the recommendations from the interdisciplinary team, presumably preventing SHCs. A cost-effectiveness study, using a comparative effectiveness design, could study the intervention as reflected in this study in comparison to a care-as-usual (only primary care) cohort [24].
We aim to continuously improve the interdisciplinary outpatient follow-up care, to better meet the healthcare needs and solving the SHC of persons with SCI. To be sure to cover all possible SHCs, a screening with a questionnaire could be introduced. The expectation is that, by such screening methods, participants will be better prepared, the risk of missing information (e.g., medication) will be minimalized and will result in better tailored recommendations. Moreover, we observed in this study a lot of missing information regarding if recommendations were followed by the participants, whether the underlying problem was solved or if there was given a new recommendation for the same underlying problem, in the letters to the general practitioner. A standardized letter to the general practitioner could help to minimize the missing information. All these suggestions could contribute to a better monitoring, prevention and possibly solving SHCs following SCI, which is the goal of this interdisciplinary follow-up care model.
Limitations
In the current study only people that showed up were taken into account. These participants might be different form the people with SCI that do not show up or declined to visit the interdisciplinary follow-up clinic. To this respect, it would be interesting to investigate if people with SCI that are readmitted to the rehabilitation center for treatment of pressure sores were visiting the interdisciplinary follow-up clinics on a regular base.
Further, in the letters to the general practitioner the information if recommendations were followed or the underlying problem was solved or if there was given a new recommendation for the same underlying problem, was mostly missing, and might have biased the results.
Conclusion
A follow-up care program organized in an interdisciplinary carousel additional to community care, brings forth an extensive number of recommendations. The high number and diversity of the recommendations, reflect the complexity of SHCs in people with SCI which is in need of specialist knowledge and preferably provided in an interdisciplinary manner. This explorative study suggests that an interdisciplinary follow-up care model as presented in this study adds to primary care. As far as could be determined these recommendations were followed relatively well by the participants, resulting in solving underlying problems and preventing worse such as an increase in bodyweight or decrease in respiratory functioning. Altogether, these findings suggests the added value of the interdisciplinary follow-up clinic in preventing SHCs, justifying a more widely use of life long follow-up care for people with SCI. More research is necessary to investigate the impact and cost-effectiveness of the interdisciplinary follow-up clinic.
Supplier
SPSS for windows, version 25; IBM.
MicroDirect; Spirometer MicroPlus, version MS03, Lewiston, Great Britain.
CareFusion; Spirometer Micro I, version 2.02, San Diego, CA United States of America.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Battalio SL, Jensen MP, Molton IR. Secondary health conditions and social role satisfaction in adults with long-term physical disability. Heal Psychol. 2019;38:445–54.
Bloemen-Vrencken JHA, Post MWM, Hendriks JMS, de Reus ECE, de Witte LP. Health problems of persons with spinal cord injury living in the Netherlands. Disabil Rehabil. 2005;27:1381–9.
Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013;51:882–92.
Gabbe BJ, Nunn A. Profile and costs of secondary conditions resulting in emergency department presentations and readmission to hospital following traumatic spinal cord injury. Injury. 2016;47:1847–55.
Munce SEP, Wodchis WP, Guilcher SJT, Couris CM, Verrier M, Fung K, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51:64–9.
Chhabra HS. ISCoS text book on comprehensive management of spinal cord injuries. New Delhi: Wolters Kluwer; 2015.
Wade DT. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil. 2020;34:571–83.
Dunn M, Love L, Ravesloot C. Subjective health in spinal cord injury after outpatient healthcare follow-up. Spinal Cord. 2000;38:84–91.
Cox RJ, Amsters DI, Pershouse KJ. The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin Rehabil. 2001;15:600–6.
Spreyermann R, Lüthi H, Michel F, Baumberger ME, Wirz M, Mäder M. Long-term follow-up of patients with spinal cord injury with a new ICF-based tool. Spinal Cord. 2011;49:230–5.
Bloemen-Vrencken JHA, De Witte LP, Post MWM. Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation. Spinal Cord. 2005;43:462–75.
Leochico CFD, Valera MJS. Follow-up consultations through telerehabilitation for wheelchair recipients with paraplegia in a developing country: a case report. Spinal Cord Ser Cases. 2020;6. https://doi.org/10.1038/s41394-020-0310-9.
van Asbeck FWA. Textbook of spinal cord injury rehabilitaion. 2nd ed. Houten: Bohn Stafleu van Loghum; 2007.
van Asbeck FWA, van Nes IJW. Textbook of spinal cord injury rehabilitation. Assen: Koninklijke van Gorcum; 2016.
Nazorg na dwarslaesierevalidatie - Richtlijn - Richtlijnendatabase. Federatie medische specialisten; 2017 https://richtlijnendatabase.nl/richtlijn/dwarslaesierevalidatie/nazorg_na_dwarslaesierevalidatie.html.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. UroToday Int J. 2009;2:20–2.
Dallmeijer AJ, Van Der Woude L, Van Kamp GJ, Hollander AP. Changes in lipid, lipoprotein and apolipoprotein profiles in persons with spinal cord injuries during the first 2 years post-injury. Spinal Cord. 1999;37:96–102.
De Groot S, Post MWM, Postma K, Sluis TA, Van Der Woude LHV. Prospective analysis of body mass index during and up to 5 years after discharge from inpatient spinal cord injury rehabilitation. J Rehabil Med. 2010;42:922–8.
Stolzmann KL, Gagnon DR, Brown R, Tun CG, Garshick E. Longitudinal change in FEV1 and FVC in chronic spinal cord injury. Am J Respir Crit Care Med. 2008;177:781–6.
Verberne DPJ, Kroese MEAL, Staals J, Ponds RWHM, van Heugten CM. Nurse-led stroke aftercare addressing long-term psychosocial outcome: a comparison to care-as-usual. Disabil Rehabil. 2020;0:1–9.
Allison R, Shelling L, Dennett R, Ayers T, Evans PH, Campbell JL. The effectiveness of various models of primary care-based follow-up after stroke: a systematic review. Prim Health Care Res Dev. 2011;12:214–22.
Fens M, Vluggen TP, Van Haastregt JC, Verbunt JA, Beusmans GH, Van Heugten CM. Multidisciplinary care for stroke patients living in the community: a systematic review. J Rehabil Med. 2013;45:321–30.
French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D. Health care costs for patients with chronic spinal cord injury in the veterans health administration. J Spinal Cord Med. 2007;30:477–81.
Verberne DPJ, Van Mastrigt GAPG, Ponds RWHM, Van Heugten CM, Kroese MEAL. Economic evaluation of nurse-led stroke aftercare addressing long-Term psychosocial outcome: a comparison to care-as-usual. BMJ Open. 2021;11:1–13.
Acknowledgements
We would like to thank Minke ter Stal and Mirke L’Herminez for their effort to retrieve all the information from the medical records of the participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Medical Ethics Committee of the University Medical Center Radboud declared that this study (retrospective cohort study with anonymized data) did not need formal ethical approval under the Dutch law regulating medical research in human beings (reference number: 2021-7379). In accordance with local requirements, the Medical Ethics Committee of the Sint Maartenskliniek approved the conduct of this study in their center.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Diemen, T., Verberne, D.P.J., Koomen, P.S.J. et al. Interdisciplinary follow-up clinic for people with spinal cord injury: a retrospective study of a carousel model. Spinal Cord Ser Cases 7, 86 (2021). https://doi.org/10.1038/s41394-021-00451-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00451-0