Abstract
Study design:
Prospective cross-sectional multidimensional study using clinical assessment and standard measures.
Objectives:
To determine the medical and social factors associated with parenting stress among mothers of children with spina bifida.
Setting:
Spina bifida clinics of two tertiary hospitals in urban Kuala Lumpur, Malaysia.
Methods:
A total of 81 mothers of children aged 1–18 years completed the Parenting Stress Index-Short Form (PSI/SF). Each child's adaptive skills were assessed using the Vineland Adaptive Behaviour Scales (VABS), Interview Edition. Medical and social data were obtained from direct interviews and case note reviews. Hierarchical multiple regression analysis was used to investigate factors that were determinants for high scores in the parental distress (PD), difficult child (DC) and parent–child dysfunctional interaction (P-CDI) subdomains of the PSI/SF. Results were expressed as beta coefficient (β) and 95% confidence intervals (95% CIs).
Results:
Single-parent families (β 8.6, 95% CI 3.4–13.9) and the need for clean intermittent catheterization of bladder (β 3.5, 95% CI 0.7–6.2) were associated with high PD scores. Clean intermittent catheterization (β 3.0, 95% CI 0.5–5.5) was associated with higher DC scores. Lower composite VABS scores (β −0.08, 95% CI −0.02 to −0.15) and mother as the sole caregiver (β 2.6, 95% CI 0.15–4.96) was associated with higher P-CDI scores.
Conclusion:
The need for clean intermittent catheterization was the only medical factor associated with parenting stress in mothers of children with spina bifida. This was mediated by single parenthood, caregiver status and the child's adaptive skills.
Similar content being viewed by others
Introduction
Spina bifida is the second most common congenital birth defect worldwide,1 caused by failure of closure of the neural tube during the early weeks of gestation. Long-term problems related to the disorder include ambulatory difficulties, bowel and bladder incontinence, hydrocephalus and shunt malfunction, skin breakdown and learning difficulties. Although the level of lesion correlates well with ambulation status, prognostication of other disabilities is more difficult.2 Each child and family requires multidisciplinary and often intensive management tailored to their needs over time. This places considerable strain on health and social resources, as well as physical, psychological and social demands on the patient and family.
Parents of children with spina bifida experience higher levels of psychological strain than parents of able-bodied children.3 Sources of stress among these parents include sudden impact life events (for example, at the time of diagnosis and surgery) as well as the repetitive, daily problems (for example, ambulation and incontinence problems) that contribute to chronic impact.4 These parents need to cope with large amounts of technical medical information, adjust to the new demands on their own daily routines and make important decisions about the medical, social and schooling needs of their children.5
Existing literature on parenting stress is largely based on Western (mainly Caucasian) middle-class participants.4, 5, 6, 7, 8 A meta-analysis has shown that spina bifida has a negative medium–large effect on parental psychological adjustment, with the most important effect on parent–child relationship.3 Mothers have been shown to be more at risk than fathers, probably because they often are the main caregivers and consequently are more exposed to illness-related situations.4, 9
Few studies have been done among Asian families having children with chronic disorders wherein the social and cultural outlook, as well as medical services, differs. Higher levels of parenting stress were noted among Malaysian mothers of children with cerebral palsy and mental retardation compared with controls, and this was mediated by ethnicity, socio-economic status, care-giving burden and child behaviour.10, 11 Although cerebral palsy and mental retardation result in chronic disability, some of the long-term problems outlined above are unique to spina bifida. Hence, the purpose of this study was to determine factors associated with parenting stress among mothers of children with spina bifida. We hypothesized that maternal parenting stress would be affected by the severity of the child's medical problems and functional status, but mediated by social and maternal factors.
Materials and methods
Patient selection
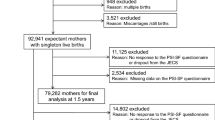
This was a prospective, cross-sectional, hospital-based study on mothers of children aged 1–18 years, attending the spina bifida clinics of the Paediatric Institute Kuala Lumpur and Universiti Kebangsaan Medical Centre Kuala Lumpur between 2003 and 2005. Both these clinics served as referral centres for children with spina bifida in the urban areas and surrounding suburbs. Only patients who had attended at least three clinic sessions (with complete multidisciplinary medical and social assessment) and whose family had already initiated treatment plans were included in the study. All the children's healthcare needs were government funded. Exclusion criteria included children of immigrant parents, mothers who were unable to read and complete the questionnaire, and those who declined to participate.
Measures
Information regarding the purpose and method of study was provided to the families. Mothers who consented were required to complete the self-administered Parenting Stress Index-Short Form (PSI/SF, Abidin)12 questionnaire, using either the original English, or translated Malay Language or Mandarin versions. The PSI/SF has 36 items, which make up three subscales: parental distress (PD), parent–child dysfunctional interaction (P-CDI) and difficult child (DC) domains. The PD subscale highlights the distress a parent is experiencing in her role as a parent. The P-CDI subscale focuses on the parent's perception that the child does not fulfil her expectations and their interactions are not reinforcing her role as a parent. The DC subscale focuses on some of the basic behavioural characteristics of children that make them difficult to manage. The total PSI score is obtained by summating the scores of the three subscales. A higher score indicates a higher level of stress experienced by the individual. Mothers who obtain a score ⩾90th percentile are said to be experiencing clinically significant levels of stress. Demographic data, medical history and physical examination data were obtained from a combination of direct interviews and case-note reviews.
To determine the child's personal and social adaptive skills, the mothers were interviewed by one of the two researchers (VC and NNAR), using the Vineland Adaptive Behaviour Scales (VABS), Interview Edition.13 Standardized scores (mean 100, s.d. 15) for four domains, that is: communication, daily living skills, socialization and motor skills, were obtained, with lower scores indicating greater dysfunction. The adaptive behaviour composite score (Composite VABS) was derived from the sum of three domain standard scores, namely communication, daily living skills and socialization. Poor adaptive skills were defined as standardized scores less than 85. The motor skills domain scores are only available for children up to 5 years 11 months 30 days (5–11–30), and therefore estimated motor skills standard scores were derived for children above 6 years (6-0-0) as formulated in the VABS manual.
Statistical analysis
Statistical analysis was done using SPSS for Windows version 15.0, 2006, SPSS Inc Chicago, IL, USA. Data were reported as means for normal data and median for non-normal data. Hierarchical stepwise multiple regression analysis was used to determine which variables were associated with higher PD, P-CDI and DC scores. The variables were entered in three blocks: child variables in block 1; socio-economic factors in block 2 and maternal factors in block 3 (Table 1). A P-value of less than 0.05 was considered statistically significant. All applicable institutional regulations concerning the ethical use of human volunteers was followed during the course of this research.
Results
A total of 81 children with spina bifida participated in the study. Table 2 shows the medical and socio-demographic characteristics of the children. In all, 6 (7.4%) children were from single-parent families. Also, 9 (11.1%) children had a closed myelomeningocoele, 50 (61.7%) an open lesion that had been repaired in early life, 19 (23.5%) a lipomyelomeningocoele and three (3.7%) sacral agenesis. Of the 34 children who had hydrocephalus, 30 (89.2%) required ventriculo-peritoneal shunts. Catheterization was performed by mothers in 88.9% of the children who needed clean intermittent catheterization (CIC) and 21 (45.7%) of these 46 children were still frequently wet. There were only five children performing self-catheterization; four aged 7–12 years and one aged above 12 years. In all, 39% of the patients had constipation and 30.1% reported faecal incontinence.
Table 3 shows the mother’s PSI/SF total and subdomain scores and the child's VABS scores. Table 4 shows the predictive factors from the multiple regression analysis for the three PSI/SF subdomain scores. Single-parent families and the need for CIC were associated with higher PD scores, accounting for 10.9 and 9.3% of the variance, respectively. The need for CIC was the only variable associated with higher DC scores (6.7% variance). There was no statistically significant difference in mean PSI scores between the five mothers of self-catheterizing children and the others. Lower composite VABS scores and mother as the sole caregiver were associated with higher P-CDI scores, accounting for 5.9 and 5.1% of the variance, respectively.
Discussion
This study shows that more than a third of mothers of children with spina bifida experience clinically significant levels of parenting stress as defined by Abidin. Two factors contributed significantly to parental distress scores: single-parent status and child requiring clean intermittent catheterization (CIC). Furthermore, the need for CIC was the sole significant factor in the DC subdomain.
Clean intermittent catheterization
Clean intermittent catheterization is a well-established technique used in the management of children with bladder dysfunction and therefore in many children with spina bifida. First introduced by Lapides14 in 1972, its main purpose is to protect the kidneys from permanent upper tract damage. It also has the added advantage of improving continence, albeit not completely, in many of these children. To achieve the desired results, CIC should be performed as often as 4–6 h everyday. Children with normal intelligence and manipulative skills do learn to catheterize themselves, but usually at around the age of 6 years.15 Therefore, until such time that this is achieved, the responsibility of catheterization falls on the parent or caregiver. Indeed even when the procedure is taken over by the child, many parents find that the responsibility of ensuring that their child complies with the schedule of CIC and the anxiety this produces remains with the parent.16, 17
Rendeli et al.18 have shown that parents of non-continent spina bifida children had significantly lower quality of life scores (parental emotional category) when compared with those of continent spina bifida children. However, their study did not analyse the CIC subgroup (17 of the 26 incontinent children had CIC done by a parent) per se. Thus, it is not known whether it was the incontinence itself or the need for CIC in these children that was contributing to the lower scores. Conversely, Macias et al.,8 in their study of parenting stress in children with special health-care needs (neural tube defects, developmental–behavioral disabilities and perinatal intraventricular haemorrhage), showed no significant difference in the parental stress scores within the neural-tube defect group, despite an overall greater stress level in those whose children had toileting problems. They postulated that when problems with toileting are expected due to the nature of the disability or disease, parents experience less stress than when the child appears physically normal. In their cohort, toileting problems included encopresis as well as daytime and nocturnal urinary incontinence, and the use of CIC among the neural-tube defect group itself was not evaluated. Other problems that have been reported by parents performing CIC include an aversion to catheterizing their child, pain inflicted on insertion of catheter (in some children) and reluctance of the child to be catheterized.16, 17 Furthermore, the need for strict adherence to its regular timing and daily schedule leads to the feeling of ‘life being dominated by it’ and affects the caregiver's free time and social life. Parents have reported making extra trips during school-break to attend to their child's CIC. As the mother is the primary caregiver in many instances, she is continually exposed to these demands on her time and emotional well-being.4
In our study, 56.8% of spina bifida children required CIC and the majority had this performed by the mother. Even though 45.7% were still wet, the results suggest that the need for CIC itself rather than the incontinence contributed to maternal perception that the child is ‘difficult’ and that her parental role is stressful. Thus, there is a need to explore further which aspects of CIC contribute to stress.
Single-parent status
Although only 7% of our families were single-parent families, this factor contributed significant maternal stress in the PD domain. Marital status has been consistently linked to personal well-being, even in adults without handicapped children,19 while the presence of a significant adult companion improved maternal self-reports of well-being, satisfaction and competence in mothers of children with spina bifida.20 Vermais et al.4 too showed that the presence of a partner correlated with fewer psychological symptoms in parents of children with spina bifida. Thus, it is possible that the loneliness, lack of physical and emotional support, and lack of respite from the care-giving needs of the spina bifida child that accompanies the absence of adult companionship in a marriage have given rise to the increased stress scores in our single-parent families.
Mother as the sole caregiver
In our cohort, the mother being the sole caregiver (60% of families) was associated with higher parenting stress scores in the P-CDI domain. Vermais et al.4 found that mothers had higher PSI scores than fathers in families with a spina bifida child. Mothers in their study also felt more restricted by their parenting role, less competent as a parent and more socially isolated than the mothers in the non-clinical reference group. Though most studies of this nature indicate that mothers are the primary caregivers, none have measured the difference in stress levels among mothers with help and those without help in the care-giving role. The child's primary caregiver is likely to be exposed to more illness-related situations and demands than other helpers/family members. Given the daily hassles and length of time needed for routine bladder and bowel procedures, as well as the increased time spent assisting the child who has restricted mobility, it is not surprising that mothers who are the sole caregivers would perceive the mother–child interaction as negative. Here it must be explained further that in our cultural and social context, extended families that include grandparents and even parents’ siblings may be a part of the family units. It is also not uncommon for families to employ live-in domestic helpers. Thus, it was pertinent to differentiate mothers who were the sole caregivers from those with help.
Adaptive skills
Mothers of children with lower composite VABS scores had higher stress scores in the P-CDI domain. As the composite score included communication skills, daily living skills and socialization skills, we postulate that the child with poorer adaptive skills in these three domains requires much more assistance from the primary caregiver (the mother solely in 60.5%) than a child with purely poor motor adaptive skills, and this inevitably leads to greater demands on the mother both emotionally and psychologically.
Limitations
The mothers in this study were recruited only from those attending two urban hospitals. The representation of mothers from other rural/district hospitals was thus not available. Parents who live in urban areas may have other stressors that contribute to parenting stress: for example, the higher cost of living and therefore need for a two-person income, inner-city transportation difficulties for disabled persons and the greater life-style expectations and demands of other children in the family. Furthermore, fathers were not included in the interviews to determine their contribution to care-giving, support or lack of support to their spouse and their acceptance/expectations of their child's disability, as well as their partner's role as the main caregiver. The availability and utilization of support groups and other community services for the handicap were also not explored. This too can contribute to alleviating stress.
Conclusion
Although social factors such as single parenthood and caregiver status are known stressors in any chronic disability, the need for CIC has not been identified as a stressor in the literature on spina bifida. In our local Malaysian setting, community support from outside the family circles is not very well established, thus making it difficult to address the issues of single parents and sole caregivers. However, factors associated with and arising from performing CIC can and need to be explored further. With this knowledge we can then make appropriate recommendations to optimize its compliance and reduce parental stress from this essential procedure, hence ensuring the long-term protection of the renal unit.
References
Detrait ER, George TM, Etchevers HC, Gilbert JR, Vekemans M, Speer MC . Human neural tube defects: developmental biology, epidemiology and genetics. Neurotoxicol Teratol 2005; 27: 515–524.
Ong LC, Lim YN, Sofiah A . Malaysian children with spina bifida: relationship between functional outcome and level of lesion. Singapore Med J 2002; 43: 12–17.
Vermais IPR, Janssens JMAM, Bosman AMT, Gerris JRM . Parents’ psychological adjustment in families of children with Spina bifida: a meta-analysis. BMC Pediatr 2005; 5: 32. Available at http://www.biomedcentral.com/1471-2431/5/32.
Vermais IPR, Janssens JMAM, Mullaart RA, Vincks A, Gerris JRM . Parents’ personality and parenting stress in families of children with spina bifida. Child: Care Health Dev 2008; 34: 665–674.
Macias MM, Clifford SC, Saylor CF, Kreh SM . Predictors of parenting stress in families of children with spina bifida. Children's Health Care 2001; 30: 57–65.
Holmbeck GN, Gorey-Ferguson L, Hudson T, Seefeldt T, Shapera W, Turner T et al. Maternal, paternal and marital functioning in families of pre-adolescents with spina bifida. J Pediatr Psychol 1997; 22: 167–181.
Holmbeck GN, Greenlet RN, Coakley RM, Greco J, Hagstrom J . Family functioning in children and adolescents with spina bifida. An evidence-based review of research and interventions. Dev Behav Pediatr 2006; 27: 249–277.
Macias MM, Roberts KM, Saylor CF, Fussell JJ . Toileting concerns, parenting stress and behavior problems in children with special health care needs. Clin Pediatr 2006; 45: 415–422.
Dorner S . The relationship of physical handicap to stress in families with an adolescent with spina bifida. Dev Med Child Neurol 1975; 17: 765–776.
Ong LC, Afifah I, Sofiah A, Lye MS . Parenting stress among mothers of Malaysian children with cerebral palsy: predictors of child and parent related stress. Ann Trop Paediatr 1998; 18: 301–307.
Ong LC, Chandran V, Peng R . Stress experienced by mothers of Malaysian children with mental retardation. J Pediatr Child Health 1999; 35: 358–362.
Abidin RR . Parenting Stress Index-Short Form: Test Manual. Pediatric Psychology Press: Charlottesville, VA, 1990.
Sparrow SS, Balla DA, Cichetti DV . Vineland Adaptive Behavior Scales. Interview Edition-Survey Form Manual. American Guidance Service, Inc: Circle Pines, MN, 1984.
Lapides J, Diokno AC, Silber SJ, Lowe BS . Clean intermittent self-catheterisation in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Robinson RO, Cockram M, Strode M . Severe handicap in spina bifida: no bar to intermittent self-catheterisation. Arch Dis Child 1985; 60: 760–776.
Borzyskowski M, Cox A, Edwards M, Owen A . Neuropathic bladder and intermittent catheterization: social and psychological impact on families. Dev Med Child Neurol 2004; 46: 160–167.
Edwards M, Borzyskowski M, Cox A, Badcock J . Neuropathic bladder and intermittent catheterization: social and psychological impact on children and adolescents. Dev Med Child Neurol 2004; 46: 168–177.
Rendeli C, Ausili E, Tabacco F, Caliandro P, Aprile I, Tonali P et al. Assessment of health status in children with spina bifida. Spinal Cord 2005; 43: 230–235.
Coombs RH . Marital status and personal well-being. A literature review. Family Relations 1991; 40: 97–102.
Fagan J, Schor D . Mothers of children with spina bifida: factors related to maternal psychological functioning. Am J Orthopsychiatry 1993; 63: 146–152.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kanaheswari, Y., Razak, N., Chandran, V. et al. Predictors of parenting stress in mothers of children with spina bifida. Spinal Cord 49, 376–380 (2011). https://doi.org/10.1038/sc.2010.125
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.125
Keywords
This article is cited by
-
Early Vs. Expectant Management of Spina Bifida Patients—Are We All Talking About a Risk Stratified Approach?
Current Urology Reports (2019)
-
Long-term outcome of transanal irrigation for children with spina bifida
Spinal Cord (2015)
-
The effects of transanal irrigation as a stepwise bowel management program on the quality of life of children with spina bifida and their caregivers
Spinal Cord (2013)
-
Predictors of parenting stress in mothers of children with spina bifida
Spinal Cord (2011)