Abstract
Study design:
An in vivo study using a spinal cord compression model in rats.
Objectives:
To evaluate the effect of adenosine on thermal hyperalgesia after spinal cord injury (SCI).
Summary of background data:
After SCI, some patients suffer dysesthesia that is unresponsive to conventional treatments. We previously established a rat thoracic spinal cord mild-compression model by which we were able to induce thermal hyperalgesia in the hind limbs.
Methods:
The thoracic spinal cord was compressed gently using a 20-g weight for 20 min. The withdrawal latency in response to thermal stimulation was monitored bilaterally in the hind limbs using Hargreaves’ Plantar test apparatus.
Results:
SCI-induced thermal hyperalgesia was mimicked by the intrathecal application of 8-cyclopentyl-1,3-dipropylxanthine (DPCPX), a selective adenosine A1 receptor antagonist. Hyperalgesia induced by SCI was significantly inhibited by the intrathecal application of 10–30 nmol chloro-adenosine (Cl-adenosine), a nonselective adenosine receptor agonist. The effect of Cl-adenosine (10 nmol) on hyperalgesia after SCI was blocked by the simultaneous application of DPCPX. Intrathecal application of R(−)N6-(2phenylisopropyl) adenosine (R-PIA; 10 nmol), a selective A1 receptor agonist, also inhibited SCI-induced hyperalgesia. In contrast, intrathecal application of CGS21680, a selective adenosine A2a receptor agonist, did not inhibit SCI-induced hyperalgesia.
Conclusions:
These results suggest that adenosine inhibits hyperalgesia through the stimulation of A1 receptors. Adenosine or adenosine A1 receptor agonists should be considered as candidates for new therapeutic methods for treating post-SCI dysesthesia.
Similar content being viewed by others
Introduction
After spinal cord injury (SCI), severe sensory disturbances occur, accompanied by motor deficiencies. Some patients with SCI complain of feeling several kinds of pain sensations. Allodynia, hyperalgesia and continuous spontaneous pain are typical chief complaints.1 Along with other types of neuropathic pain, spinal cord damage-induced pain is usually unresponsive to conventional treatments. The pain sensations are believed to be controlled by a balance between excitatory and inhibitory signals. The typical stimulatory signaling molecules are glutamate2, 3 and substance P,4 and the inhibitory signaling molecules are serotonin,5 noradrenaline6 and GABA (γ-amino-butyric acid).7 Adenosine, an endogenous neuromodulator, controls neuronal membrane potential through adenosine receptors. One of the actions of adenosine receptors is hyperpolarization of the cell membrane that inhibits the excitation of neurons.8 Several previous studies have shown that intrathecal adenosine receptor agonists inhibit pain behavior after peripheral nerve injuries such as L5–L6 spinal nerve ligation,9 sciatic nerve ligation,10 intrathecal strychnine injection,11 intrathecal administration of excitatory amino acids or substance P12 and photochemical SCI through laser irradiation.13 Until now, there has been no reported evidence of anti-hyperalgesic action of adenosine receptor agonists after mechanical spinal cord compression injury. The purpose of this study was to examine the effect of adenosine on hyperalgesia after a spinal cord compression injury.
Materials and methods
Animals
Female Wistar rats (Clea Japan, Tokyo, Japan), 250 g, were used for this study. Swartz et al.14 reported that the outcome of motor function after SCI in female rats was better than that in males. They also reported that the difference of outcome was not dependent on estrogen. We thought that gender difference may affect the mortality of the animals, and that female rats would be suitable for evaluation of sensory abnormality after SCI. When we observed the threshold against heat stimulation in normal and the sham animals, no changes in threshold was observed within 7 days,5 suggesting that estrous cycle did not affect pain sensation in this study. Therefore, we used female rats in this experiment. The experiments were performed according to the ethical recommendations of the Committee for Research and Ethical Issues of the International Association for the Study of Pain.15 The research protocol was accepted by the Ethical Committee for Animal Experiments of Ehime University (Ehime, Japan).
Spinal cord mild-compression model (SCI model)
Under general anesthesia using halothane, the rat spinal cord was carefully exposed by removing the vertebral lamina at the eleventh vertebra. Direct compression was performed using a 20-g weight, which consisted of very soft and rounded silicone at the point that made contact with the dura. The weight was gently placed on the thoracic spinal cord extraduraly for 20 min (SCI). We did not observe any serious damage, such as hyperextension, paresis of the hind limbs or histological hemorrhage accompanied by tissue destruction, at the point of compression. In some experiments, a laminectomy of the eleventh vertebra was performed without spinal cord compression (sham). In another set of experiments, the compression period was lengthened from 10 to 60 min. At 3 days after SCI, the animals were subjected to a pain evaluation.
Drugs
Chloro-adenosine (Cl-adenosine), a nonselective adenosine receptor agonist (1–100 nmol per 10 μl; Research Biochemicals Inc., Natick, MA, USA), and R(−)N6-(2phenylisopropyl) adenosine (R-PIA), a selective adenosine A1 receptor agonist (10nmol 10μl–1; Research Biochemicals Inc.) were dissolved in phosphate-buffered saline. 8-Cyclopentyl-1,3-dipropylxanthine (DPCPX), a selective adenosine A1 receptor antagonist (10 μg 10 μl–1; Research Biochemicals Inc.), 4-2-7-Amino-2-2-furyl)triazolotriazin-5-ylamino]ethyl)phenol (ZM243185), a selective adenosine A2a receptor antagonist (10 μg 10 μl–1; TOCRIS, Hung Road, Bristol, UK) and 4-2-6-Amino-9-N-ethyl-β-D-ribofuranuronamidosyl)-9H-purin-2-yl]amino]ethyl]benzenepropanoic acid (CGS21680), a selective adenosine A2a receptor agonist (10 nmol 10 μl–1; TOCRIS), were dissolved in dimethyl sulfoxide and diluted with phosphate-buffered saline. The doses of all agonists except Cl-adenosine were decided according to previous papers10, 13 that described intrathecal application. Antagonists were used at relatively high concentrations compared with agonists to achieve adequate blockade of the receptors.
Intrathecal application of drugs
All drugs (adenosine receptor agonists and antagonists) were applied intrathecally at 1 h before the pain measurements were taken. Intrathecal administration was performed under general anesthesia using halothane. Drug solutions were injected in 10 μl volumes into the subarachnoid space through the intervertebral foramen between L3 and L4 using a 27-gauge needle connected to a microsyringe with polyethylene tubing. The vehicle animals (SCI without drugs) and the control animals (no SCI) received 10 μl phosphate-buffered saline intrathecally at 1 h before the pain measurements.
Evaluation of thermal hyperalgesia
To evaluate the withdrawal threshold in response to thermal paw stimulation, we used Hargreaves’ plantar test apparatus (Ugo Basile, Varese, Italy). Rats were placed on a 2-mm thick glass floor, and a mobile infrared heat generator with an aperture of 10 mm in diameter was aimed at the rat's hind paw from beneath the floor. When the rats felt pain and withdrew their paw, the power was shut off and the reaction time (the withdrawal latency of the paw) was recorded automatically. Shortened withdrawal latencies in response to thermal stimulation were considered to indicate thermal hyperalgesia. Experiments were performed in a quiet room. The temperature of the glass floor was kept at 22.5–23.5 °C. Measurements of paw withdrawal latency began after the animals were placed in the box and were confirmed to be sitting still. The measurements were repeated three times at 5-min intervals on each paw. The averages of the three measurements were used as data. The data of the sham or normal animals were obtained in each series of the measurements to exclude the bias of measurement conditions (temperature and brightness of the room). Data of the drug application (Figures 4,5,6,7,8) are expressed as percentages of that in the sham animals (%Sham, the mean±s.e.m.).
Data analysis
For statistical analysis of the data, an analysis of variance followed by Fisher's protected least significant difference test was used. All statistical analyses were performed using the actual withdrawal latencies.
Results
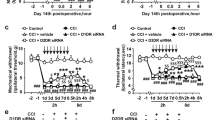
In the normal rats that did not undergo an operation, hyperalgesia was induced by the intrathecal application of 10 μg DPCPX, a selective antagonist of the adenosine A1 receptor (Figure 1). On the other hand, intrathecal application of 10 μg ZM243185, a selective antagonist of the adenosine A2a receptor, did not change the withdrawal latency (Figure 2). These results suggest that continuous stimulation of A1 receptors by endogenous adenosine suppresses activity of the pain pathway under normal physiological conditions. Figure 3 shows the effect of the duration of compression on thermal hyperalgesia. At 3 days after injury, significant heat hyperalgesia was observed in the hind paws of rats that underwent compression for 20 min (SCI), whereas rats that underwent 10, 40 and 60-min periods of compression did not experience significant hyperalgesia compared with the sham animals (0-min compression). As significant hyperalgesia was only observed in the 20-min compression group, we evaluated the effect of drugs only in these animals. Hyperalgesia induced by SCI was significantly inhibited by the intrathecal application of 10 nmol Cl-adenosine, the nonselective adenosine receptor agonist (Figure 4). Figure 5 shows the dose-dependent effect of Cl-adenosine on SCI-induced hyperalgesia. Cl-adenosine significantly inhibited SCI-induced hyperalgesia at concentrations between 10 and 30 nmol. The effect of Cl-adenosine (10 nmol) on hyperalgesia after SCI was blocked by the simultaneous application of DPCPX (Figure 6). This result suggests that the anti-hyperalgesic action of Cl-adenosine is mediated by the stimulation of A1 receptors. Intrathecal application of R-PIA (10 nmol), the A1 receptor agonist, inhibited SCI-induced hyperalgesia (Figure 7). On the other hand, intrathecal application of CGS21680, the selective adenosine A2a receptor agonist, did not inhibit SCI-induced hyperalgesia (Figure 8). These results suggest that adenosine inhibited SCI-induced hyperalgesia through the stimulation of A1 receptors.
Effect of intrathecal DPCPX (10 μg), a selective adenosine A1 receptor antagonist, on the response to thermal stimulation in rats. Thermal hyperalgesia thresholds (withdrawal latency) were measured at 1 h after injection. Data are expressed as the mean±s.e.m. (n=6). Statistical significance compared with control rats (10 μl phosphate-buffered saline (PBS) injection) is represented with an asterisk (*P<0.05).
Effect of intrathecal ZM243185 (10 μg), a selective adenosine A2a receptor antagonist, on the response to thermal stimulation in rats. Thermal hyperalgesia thresholds (withdrawal latency) were measured at 1 h after the injection. Data are expressed as the mean±s.e.m. (n=6). Intrathecal application of ZM243185 did not change the withdrawal latency.
Heat hyperalgesia produced by spinal cord compression. The rat thoracic spinal cord was gently compressed by a 20-g weight for the indicated durations. At 3 days after compression, the threshold of the response to heat stimulation was evaluated. Data are expressed as the mean±s.e.m. (n=6). Only 20 min of compression produced significant (*P<0.05) heat hyperalgesia compared with that in the sham animals (0 min).
The inhibitory effect of Cl-adenosine on SCI-induced hyperalgesia. At 3 days after performing compression for 20 min, the threshold of response to heat stimulation was evaluated with or without intrathecal application of Cl-adenosine. Thermal hyperalgesia thresholds (withdrawal latency) were measured at 1 h after injection. Data are expressed as percentages of that in the sham animals (%Sham, the mean±s.e.m. (n=6)). The thermal hyperalgesia threshold in the rats that received intrathecal Cl-adenosine (10 nmol) was significantly (**P<0.01) higher than that in the vehicle rats.
Dose-dependent effect of Cl-adenosine on SCI-induced hyperalgesia. Several concentrations (1–100 nmol) of Cl-adenosine were applied intrathecally after spinal cord injury. Data are expressed as percentages of that in the sham animals (%Sham, the mean±s.e.m. (n=6)). Thermal hyperalgesia was significantly (**P<0.01) inhibited by 10 and 30 nmol Cl-adenosine.
The inhibitory effect of Cl-adenosine on thermal hyperalgesia was blocked by DPCPX (adenosine A1 receptor antagonist). Data are expressed as percentages of that in the sham animals (%Sham, the mean±s.e.m. (n=6)). Application of DPCPX alone did not influence injury-induced hyperalgesia. However, the inhibitory effect of 10 nmol Cl-adenosine on thermal hyperalgesia induced by spinal cord injury was significantly (*P<0.05) impeded by the simultaneous application of 10 μg DPCPX.
SCI-induced hyperalgesia was inhibited by R-PIA (a selective adenosine A1 agonist). Thermal hyperalgesia thresholds (withdrawal latency) were measured at 1 h after injection of R-PIA. Data are expressed as percentages of that in the sham animals (%Sham, the mean±s.e.m. (n=6)). Intrathecal application of R-PIA (10 nmol) significantly (P<0.01) inhibited SCI-induced hyperalgesia. Statistical significance compared with vehicle rats (SCI and 10 μl phosphate-buffered saline (PBS) injection) is represented with an asterisk (**P<0.01).
Effect of CGS21680 on SCI-induced hyperalgesia. Thermal hyperalgesia thresholds (withdrawal latency) were measured at 1 h after the injection of CGS21680. Data are expressed as percentages of that in the sham animals (%Sham, the mean±s.e.m. (n=6)). Intrathecal application of 10 nmol CGS21680, a selective adenosine A2a receptor agonist, did not affect SCI-induced hyperalgesia.
Discussion
After SCI, residual sensory abnormalities often interfere with the patient's daily activities.16 In the experimental neuroscience fields, mechanical allodynia and thermal hyperalgesia have been evaluated as sensory abnormalities after several types of nerve injuries. However, a model for testing sensory abnormalities after experimental SCI has not been well established. We previously established a model for rat hyperalgesia after spinal cord compression injury.5 Our method aims to model ischemia-induced hyperalgesia. When a 20-gweight is slowly placed on the thoracic spinal cord, almost complete ischemia can be achieved by minimum force.17 In this study, we performed experiments to determine what durations of compression produce thermal hyperalgesia in the hind limbs of the rats. As a result, we found that compression for 20 min produces stable hyperalgesia in the hind limbs of the rats (Figure 3). In the sham animals, hyperalgesia was not detected at any point during the experimental period. Significant hyperalgesia was observed in SCI animals from the second to the fifth day after compression.5 The withdrawal latency returned to normal on the following day after the compression procedure. The reason why longer compression periods did not produce hypersensitivity against thermal stimulation is still unclear. One possible explanation is that mild injury produced interruption of some descending signals, such as the serotonergic or noradrenagic inhibitory pathways, but higher damage interrupted both the ascending and descending sensory pathways. We might find an appropriate damage (20 g compression for approximately 20 min) that interrupt only descending inhibitory pathway. In the clinical field, it is well known that abnormal sensations, including, hyperalgesia or allodynia, were often observed in the patients with incomplete paraplesia after spinal cord damage. Our model resembles patients with incomplete paraplesia. We believe that our mild-compression-induced hyperalgesia model is useful for the evaluation of therapeutic agents for pain after SCI.
Adenosine has been a candidate to be a therapeutic agent for neuropathic pain. Belfrage et al.18, 19 tested the effect of systemic and intrathecal adenosine infusion on patients with chronic neuropathic pain. They showed that adenosine infusion alleviates spontaneous neuropathic pain, tactile allodynia and pin prick hyperalgesia in these patients. Adenosine exerts an effect as a cell modulator in influencing cells through several receptor-mediated effects. A1 and A2 receptors are found in the central nervous system associated with neurons as well as with glial cells. High-affinity A1 and A2a receptors are activated by nanomolar concentrations of adenosine. The A2 receptors are coupled to adenylcyclase, stimulating cAMP elevation that is inhibited by A1 receptors. The functionally important regulation of membrane in channels seems to be the domain of A1 receptors. Activation of adenosine A1 receptor enhances K+ and Cl− conductance in neurons, leading to membrane hyperpolarization and postsynaptic reduction of neuronal Ca2+ influx through voltage- and N-methyl D-aspartate receptor-dependent channels. This counteracts, through synaptic and extrasynaptic receptors, nerve cell depolarization.8 Li and Eisenach20 reported that capsaicin-induced glutamate release from rat spinal synaptosomes was inhibited by adenosine and adenosine A1 receptor agonists. These studies suggest that the hyperpolarizing effect of adenosine can inhibit excitation of sensory nerves and ameliorate neuropathic pain at the spinal cord level. In the present study, we showed the anti-hyperalgesic effect of adenosine A1 agonist using our original pain model induced by spinal cord compression. Adenosine A1 receptor should be an attractive target of pain therapy for patients with spinal cord damage.
When we consider the possibilities of clinical use, some ideas to achieve enhancement of adenosine signals emerges. One is simple application of adenosine A1 agonists in the spinal cord level similar to our present experiments. The other possibility is increase in extracellular adenosine concentration in the spinal cord. Adenosine is catabolized by adenosine deaminase and adenosine kinase. Therefore, the application of the inhibitors of such enzymes can increase adenosine concentration in the spinal cord. Moreover, released extracellular adenosine is re-uptaken into the cells. This reuptake mechanism inhibited extracellular adenosine signals. The adenosine reuptake inhibitor, such as propentofilline,8 may enhance adenosine signals. These compounds that enhance stimulation of adenosine A1 receptors may provide an avenue for the development of novel therapeutic methods against neuropathic pain after SCI.
References
Werhagen L, Budh CN, Hultling C, Molander C . Neuropathic pain after traumatic spinal cord injury--relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord 2004; 42: 665–673.
Ferreira SH, Lorenzetti BB . Glutamate spinal retrograde sensitization of primary sensory neurons associated with nociception. Neuropharmacology 1994; 33: 1479–1485.
Fundytus ME . Glutamate receptors and nociception: implications for the drug treatment of pain. CNS Drugs 2001; 15: 29–58.
Holland LN, Goldstein BD . Examination of tonic nociceptive behavior using a method of substance P-receptor desensitization in the dorsal horn. Pain 1994; 56: 339–346.
Horiuchi H, Ogata T, Morino T, Takeba J, Yamamoto H . Serotonergic signaling inhibits hyperalgesia induced by spinal cord damage. Brain Res 2003; 963: 312–320.
Jones SL . Descending noradrenergic influences on pain. Prog Brain Res 1991; 88: 381–394.
Xu TL, Pang ZP, Li JS, Akaike N . 5-HT potentiation of the GABAA response in the rat sacral dorsal commissural neurons. Br J Pharmacol 1998; 124: 779–787.
Schubert P, Rudolphi KA, Fredholm BB, Nakamura Y . Modulation of nerve and glial function by adenosine: role in the development of ischemic damage. Int J Biochem 1994; 26: 1227–1236.
Lee YW, Yaksh TL . Pharmacology of the spinal adenosine receptor which mediates the antiallodynic action of intrathecal adenosine agonists. J Pharmacol Exp Ther 1996; 277: 1642–1648.
Cui JG, Sollevi A, Linderoth B, Meyerson BA . Adenosine receptor activation suppresses tactile hypersensitivity and potentiates spinal cord stimulation in mononeuropathic rats. Neurosci Lett 1997; 223: 173–176.
Khandwala H, Zhang Z, Loomis CW . Inhibition of strychnine-allodynia is mediated by spinal adenosine A1- but not A2-receptors in the rat. Brain Res 1998; 808: 106–109.
Keil II GJ, DeLander GE . Altered sensory behaviors in mice following manipulation of endogenous spinal adenosine neurotransmission. Eur J Pharmacol 1996; 312: 7–14.
Sjölund KF, von Heijne M, Hao JX, Xu XJ, Sollevi A, Wiesenfeld-Hallin Z . Intrathecal administration of the adenosine A1 receptor agonist R-phenylisopropyl adenosine reduces presumed pain behaviour in a rat model of central pain. Neurosci Lett 1998; 243: 89–92.
Swartz KR, Fee DB, Joy KM, Roberts KN, Sun S, Scheff NN et al. Gender differences in spinal cord injury are not estrogen-dependent. J Neurotrauma 2007; 24: 473–480.
Zimmermann M . Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983; 16: 109–110.
Jensen MP, Chodroff MJ, Dworkin RH . The impact of neuropathic pain on health-related quality of life: review and implications. Neurology 2007; 68: 1178–1182.
Hamamoto Y, Ogata T, Morino T, Hino M, Yamamoto H . Real-time direct measurement of spinal cord blood flow at the site of compression: relationship between blood flow recovery and motor deficiency in spinal cord injury. Spine 2007; 32: 1955–1962.
Belfrage M, Sollevi A, Segerdahl M, Sjölund KF, Hansson P . Systemic adenosine infusion alleviates spontaneous and stimulus evoked pain in patients with peripheral neuropathic pain. Anesth Analg 1995; 81: 713–717.
Belfrage M, Segerdahl M, Arnér S, Sollevi A . The safety and efficacy of intrathecal adenosine in patients with chronic neuropathic pain. Anesth Analg 1999; 89: 136–142.
Li X, Eisenach JC . Adenosine reduces glutamate release in rat spinal synaptosomes. Anesthesiology 2005; 103: 1060–1065.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Horiuchi, H., Ogata, T., Morino, T. et al. Adenosine A1 receptor agonists reduce hyperalgesia after spinal cord injury in rats. Spinal Cord 48, 685–690 (2010). https://doi.org/10.1038/sc.2009.194
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.194
Keywords
This article is cited by
-
Different analgesic effects of adenosine between postoperative and neuropathic pain
Journal of Orthopaedic Science (2013)