Abstract
Background:
Spinal cord tumors are rare and fortunately affect only a minority of the population. These tumors are classified based on their anatomic location in relation to the dura mater and spinal cord as epidural, intradural extramedullary or intradural intramedullary. Intradural extramedullary Ewing's sarcoma is extremely rare.
Purpose:
Here, we are reporting a case of intradural extramedullary Ewing's sarcoma. This is the fourth such case to be reported in English literature.
Methods:
A 26-year-old gentleman presented to us with low backache and progressive paraparesis from a spinal tumor. Magnetic resonance imaging showed multiple intradural, extramedullary mass lesions extending from the T11 to S2 level. Neither osteolytic nor osteosclerotic changes were seen in the vertebral bodies. Extraskeletal Ewing's sarcoma was diagnosed histopathologically. He was treated by surgery, local radiotherapy and chemotherapy. Two months after treatment, he developed a new skip lesion in the spine at T6–T7 level. The new lesion was treated with local radiotherapy and chemotherapy.
Results:
Presently, the patient has completed treatment and is clinically doing fine.
Conclusion:
Intradural extramedullary Ewing's sarcoma is a rare aggressive neoplasm with high propensity for skip metastasis.
Similar content being viewed by others
Introduction
Spinal cord tumors are rare and fortunately affect only a minority of the population. These tumors are classified based on their anatomic location in relation to the dura mater and spinal cord as epidural, intradural extramedullary or intradural intramedullary. Ewing's sarcoma (ES) in this location is confined to case reports only. Till date, there are only three cases of intradural extramedullary ES reported in English literature.1, 2 Here, we present the fourth case of intradural extramedullary ES.
Case report
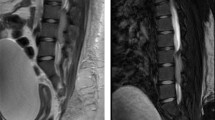
A 26-year-old gentleman presented to us with complaints of low backache of 2 months and weakness in both lower limbs of 20 days. He was initially evaluated by the neurosurgeon. Physical examination revealed grade 2 motor power in both lower limbs. Sensations were intact. There was incontinence of urine and constipation. There was no bony abnormality, deformity or tenderness in the spine. Upper limbs were normal. Other systems were normal. His complete blood counts and liver and renal functions were within normal limits. Magnetic resonance imaging (MRI) of whole spine showed multiple intradural extramedullary minimally enhancing mass lesions from T11 to S2 vertebral levels with compression of conus and involving cauda equina (Figure 1) (also see Supplementary Figure 1). Neither osteolytic nor osteosclerotic changes were seen in the vertebral bodies.
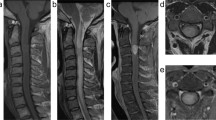
He subsequently underwent laminoplasty of T11–S2 spine with complete gross tumor excision. Post-operatively, the motor power in the lower limbs recovered. Histopathological examination revealed a malignant round cell tumor with vacuolated scant cytoplasm, round to oval nuclei, delicate nuclear chromatin and inconspicuous nucleoli (Figure 2). Immunohistochemically the tumor cells were positive for MIC-2 (Supplementary Figure 2) and negative for leucocyte common antigen (LCA) (Supplementary Figure 3). Finally, a diagnosis of extradural ES was made. Metastatic workup, including chest X-ray, ultrasound abdomen, bone scan and bone marrow biopsy, was normal.
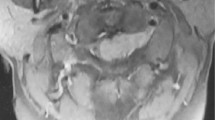
Further, he received six cycles of chemotherapy with Vincristine, Doxorubicin and Cyclophosphamide (VAC) alternating with Ifosfamide, Cisplatin and Etoposide (ICE) three weekly and post-operative radiation to a dose of 50 Gy in 25 fractions. MRI performed after 2 months showed a solid enhancing intradural extramedullary lesion in the dorsal spine T6–T7 levels with cord compression at T6/T7 suggestive of a new lesion (Figure 3 and Supplementary Figure 4). Clinically the patient was absolutely stable. Chest X-ray, ultrasound abdomen and bone scan were repeated and were all normal.
Chemotherapy was restarted. He received a total of total 12 cycles of chemotherapy. Local radiotherapy was delivered to a dose of 50 Gy over 25 fractions to the recurrent lesion. Presently, he has completed the treatment and, 6 months after treatment, he is clinically stable.
Discussion
Intramedullary spinal cord tumors account for approximately 2% of adult and 10% of pediatric central nervous system neoplasms.3 Uesaka et al.1 reported an intradural extramedullary ES in C7–T1 location in an 11-year-old girl treated by subtotal resection. Bouffet et al.2 in their series of 35 children with spinal metastases described two cases of intradural ES. First case was a 9½-year-old boy with the lesion in T11–T12 and L3–L5 location treated by radiotherapy and chemotherapy. He survived for 4 months. The second case was a 16-year-old boy with disease in L2–L3 and T4–T6 location with lung and brain metastases treated by chemotherapy and radiotherapy. He survived for 5 months.
Histological diagnosis is the only means of distinguishing ES from other tumors in or around the spine. The workup includes MRI of spine, X-ray of chest, ultrasound of abdomen, bone scan and bone marrow biopsy. MRI has revolutionized the diagnosis of intraspinal tumors, allowing for early detection and improved localization.
Owing to its rarity, there are no standard treatment guidelines for these cases. Extrapolating the results of treatment of ES at other sites, we can think that local treatment with either surgery or radiotherapy should be followed by chemotherapy for adequate control of disease. ES is generally responsive to radiotherapy and chemotherapy. Excellent microsurgical expertise and careful recognition of tumor plane are essential to remove the tumor while retaining neurological functions.4 Predictors of good surgical outcome for intramedullary spinal cord tumors are histological grade, surgical margins and neurological status of the patient before surgery.5
ES of the bone is known for skip metastases in the bone. The occurrence of skip metastasis in our case of spinal extradural ES leaves us with a caution to image the entire neuraxis thoroughly in these cases. The positron emission tomography scan may be of help to detect these skip metastases.
References
Uesaka T, Amano T, Inamura T, Ikezaki K, Inoha S, Takamatsu M et al. Intradural, extramedullary spinal Ewing's sarcoma in childhood. J Clin Neurosci 2003; 10: 122–125.
Bouffet E, Marec-Berard P, Thiesse P, Carrie C, Risk T, Jouvet A et al. Spinal cord compression by secondary epi- and intradural metastases in childhood. Childs Nerv Syst 1997; 13: 383–387.
Traul DE, Shaffrey ME, Schiff D . Part I: spinal-cord neoplasms–intradural neoplasms. Lancet Oncol 2007; 8: 35–45.
Peng L, Qi ST, Chen Z, Fen WF, Fang LX, Huang LJ et al. Radical microsurgical treatment of intramedullary spinal cord tumors. Chin Med J (Engl) 2006; 119: 1343–1347.
Nakamura M, Ishii K, Watanabe K, Tsuji T, Takaishi H, Matsumoto M et al. Surgical treatment of intramedullary spinal cord tumors: prognosis and complications. Spinal Cord [e-pub ahead of print: 2 October 2007].
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
The authors state no conflict of interest.
Supplementary Information accompanies the paper on the Spinal Cord website (http://www.nature.com/sc).
Rights and permissions
About this article
Cite this article
Haresh, K., Chinikkatti, S., Prabhakar, R. et al. A rare case of intradural extramedullary Ewing's sarcoma with skip metastasis in the spine. Spinal Cord 46, 582–584 (2008). https://doi.org/10.1038/sc.2008.8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.8
Keywords
This article is cited by
-
Primary extraskeletal intradural Ewing sarcoma with acute hemorrhage: a case report and review of the literature
Journal of Medical Case Reports (2024)
-
Intradural extramedullary metastasis: a review of literature and case report
Spinal Cord Series and Cases (2019)
-
Primary extraosseous intradural spinal Ewing’s sarcoma: report of two cases
Acta Neurochirurgica (2013)
-
Primary intradural Ewing’s sarcoma of the cauda equina presenting with acute bleeding
Acta Neurochirurgica (2010)