Abstract
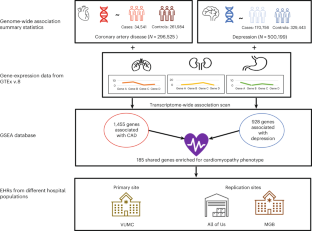
Depression and coronary artery disease (CAD) are highly comorbid conditions. Approximately 40% of individuals who have one diagnosis will also develop the other within their lifetime. Despite the high prevalence of the comorbidity, the specific genes and pathways remain unknown. Here, by mapping known variants to genes, we identified genes, followed by pathways, that are associated with both depression and CAD. Next, we investigated the phenotypic consequences of the shared pathways in an electronic health record (EHR)-based setting. We identified 185 genes that were significantly associated with both depression and CAD and were enriched for inflammatory and cardiomyopathy phenotypes. We observed an increased rate of prevalent cardiomyopathy cases in individuals with comorbid depression–CAD compared with those with CAD alone in three large EHR datasets. The results of our study implicate genetically regulated inflammatory mechanisms in depression–CAD. Our results also raise the hypothesis that depression-associated CAD may be enriched for cardiomyopathy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available from Vanderbilt University Medical Center with institutional restrictions that apply to the acquisition, use and dissemination of data. To request reasonable access to data for work conducted in a non-profit academic setting, please contact the Vanderbilt Institute for Clinical and Translational Research (research.support.services@vumc.org) and request an application to the Integrated Data Access and Services Core.
Code availability
The code for the analysis is available at https://bitbucket.org/davislabteam/depression-cad/src/master/.
References
Kendler, K. S., Gardner, C. O., Fiske, A. & Gatz, M. Major depression and coronary artery disease in the Swedish twin registry: phenotypic, genetic, and environmental sources of comorbidity. Arch. Gen. Psychiatry 66, 857–863 (2009).
Glassman, A. H. Depression and cardiovascular comorbidity. Dialogues Clin. Neurosci. 9, 9–17 (2007).
Sullivan, M. et al. Depression in coronary heart disease. What is the appropriate diagnostic threshold? Psychosomatics 40, 286–292 (1999).
O’Neil, A. et al. Depression is a risk factor for incident coronary heart disease in women: an 18-year longitudinal study. J. Affect. Disord. 196, 117–124 (2016).
Weeke, A., Juel, K. & Vaeth, M. Cardiovascular death and manic-depressive psychosis. J. Affect. Disord. 13, 287–292 (1987).
Dennis, J. et al. Genetic risk for major depressive disorder and loneliness in sex-specific associations with coronary artery disease. Mol. Psychiatry 26, 4254–4264 (2021).
Mazereeuw, G. et al. Platelet activating factors in depression and coronary artery disease: a potential biomarker related to inflammatory mechanisms and neurodegeneration. Neurosci. Biobehav. Rev. 37, 1611–1621 (2013).
McCaffery, J. M. et al. Common genetic vulnerability to depressive symptoms and coronary artery disease: a review and development of candidate genes related to inflammation and serotonin. Psychosom. Med. 68, 187–200 (2006).
Upadhyay, R. K. Emerging risk biomarkers in cardiovascular diseases and disorders. J. Lipids 2015, 971453 (2015).
Shimokawa, H., Aarhus, L. L. & Vanhoutte, P. M. Porcine coronary arteries with regenerated endothelium have a reduced endothelium-dependent responsiveness to aggregating platelets and serotonin. Circ. Res. 61, 256–270 (1987).
Brydon, L., Magid, K. & Steptoe, A. Platelets, coronary heart disease, and stress. Brain Behav. Immun. 20, 113–119 (2006).
Huang, M. et al. Longitudinal association of inflammation with depressive symptoms: a 7-year cross-lagged twin difference study. Brain Behav. Immun. 75, 200–207 (2019).
Beydoun, M. A. et al. White blood cell inflammatory markers are associated with depressive symptoms in a longitudinal study of urban adults. Transl. Psychiatry 6, e895 (2016).
Kim, J.-M. et al. Changes in pro-inflammatory cytokine levels and late-life depression: a two year population based longitudinal study. Psychoneuroendocrinology 90, 85–91 (2018).
Bränn, E. et al. Inflammatory markers in late pregnancy in association with postpartum depression—a nested case-control study. Psychoneuroendocrinology 79, 146–159 (2017).
Bremmer, M. A. et al. Inflammatory markers in late-life depression: results from a population-based study. J. Affect. Disord. 106, 249–255 (2008).
Martínez-Cengotitabengoa, M. et al. Peripheral inflammatory parameters in late-life depression: a systematic review. Int. J. Mol. Sci. 17, E2022 (2016).
Gheysarzadeh, A. et al. Serum-based microRNA biomarkers for major depression: miR-16, miR-135a, and miR-1202. J. Res. Med. Sci. 23, 69 (2018).
Schmidt, H. D., Shelton, R. C. & Duman, R. S. Functional biomarkers of depression: diagnosis, treatment, and pathophysiology. Neuropsychopharmacology 36, 2375–2394 (2011).
Nurden, A. T. The biology of the platelet with special reference to inflammation, wound healing and immunity. Front. Biosci. 23, 726–751 (2018).
Tsao, C.-W., Lin, Y.-S., Chen, C.-C., Bai, C.-H. & Wu, S.-R. Cytokines and serotonin transporter in patients with major depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 30, 899–905 (2006).
Pandey, G. N. et al. Hyperactive phosphoinositide signaling pathway in platelets of depressed patients: effect of desipramine treatment. Psychiatry Res. 105, 23–32 (2001).
van der Harst, P. & Verweij, N. Identification of 64 novel genetic loci provides an expanded view on the genetic architecture of coronary artery disease. Circ. Res. 122, 433–443 (2018).
Howard, D. M. et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat. Neurosci. 22, 343–352 (2019).
Barbeira, A. N. et al. Integrating predicted transcriptome from multiple tissues improves association detection. PLoS Genet. 15, e1007889 (2019).
Sealock, J. M. et al. Use of the PsycheMERGE network to investigate the association between depression polygenic scores and white blood cell count. JAMA Psychiatry 78, 1365 (2021).
Gidron, Y., Kupper, N., Kwaijtaal, M., Winter, J. & Denollet, J. Vagus–brain communication in atherosclerosis-related inflammation: a neuroimmunomodulation perspective of CAD. Atherosclerosis 195, e1–e9 (2007).
Chan, K. L., Cathomas, F. & Russo, S. J. Central and peripheral inflammation link metabolic syndrome and major depressive disorder. Physiology 34, 123–133 (2019).
Kempuraj, D. et al. Brain and peripheral atypical inflammatory mediators potentiate neuroinflammation and neurodegeneration. Front. Cell. Neurosci. 11, 216 (2017).
Sun, Y., Koyama, Y. & Shimada, S. Inflammation from peripheral organs to the brain: how does systemic inflammation cause neuroinflammation? Front Aging Neurosci 14, 903455 (2022).
Twig, G. et al. White blood cell count and the risk for coronary artery disease in young adults. PLoS ONE 7, e47183 (2012).
Zebrack, J. S., Muhlestein, J. B., Horne, B. D. & Anderson, J. L. C-reactive protein and angiographic coronary artery disease: independent and additive predictors of risk in subjects with angina. J. Am. Coll. Cardiol. 39, 632–637 (2002).
Lu, Q. et al. Intranuclear cardiac troponin I plays a functional role in regulating Atp2a2 expression in cardiomyocytes. Genes Dis. 15, 1689–1700 (2021).
Alimadadi, A., Munroe, P. B., Joe, B. & Cheng, X. Meta-analysis of dilated cardiomyopathy using cardiac RNA-seq transcriptomic datasets. Genes 11, 60 (2020).
Nakajima, K. et al. Brain-specific heterozygous loss-of-function of ATP2A2, endoplasmic reticulum Ca2+ pump responsible for Darier’s disease, causes behavioral abnormalities and a hyper-dopaminergic state. Hum. Mol. Genet. 30, 1762–1772 (2021).
Coste de Bagneaux, P. et al. A homozygous missense variant in CACNB4 encoding the auxiliary calcium channel beta4 subunit causes a severe neurodevelopmental disorder and impairs channel and non-channel functions. PLoS Genet. 16, e1008625 (2020).
Andrade, A. et al. Genetic associations between voltage-gated calcium channels and psychiatric disorders. Int. J. Mol. Sci. 20, 3537 (2019).
Kanehisa, M. et al. KEGG for linking genomes to life and the environment. Nucleic Acids Res. 36, D480–D484 (2007).
Xu, H. et al. A genome-wide association study of idiopathic dilated cardiomyopathy in African Americans. J. Pers. Med. 8, 11 (2018).
Good, J.-M. et al. ACTN2 variant associated with a cardiac phenotype suggestive of left-dominant arrhythmogenic cardiomyopathy. HeartRhythm Case Rep. 6, 15–19 (2020).
Haywood, N. J. et al. Hypertrophic cardiomyopathy mutations in the calponin-homology domain of ACTN2 affect actin binding and cardiomyocyte Z-disc incorporation. Biochem. J. 473, 2485–2493 (2016).
Tiso, N. Identification of mutations in the cardiac ryanodine receptor gene in families affected with arrhythmogenic right ventricular cardiomyopathy type 2 (ARVD2). Hum. Mol. Genet. 10, 189–194 (2001).
Patel, R. et al. Variants of trophic factors and expression of cardiac hypertrophy in patients with hypertrophic cardiomyopathy. J. Mol. Cell. Cardiol. 32, 2369–2377 (2000).
Yadav, M. L., Bhasker, A. N., Kumar, A. & Mohapatra, B. Identification and characterization of genetic variants of TGFB1 in patients with congenital heart disease. Meta Gene 31, 100987 (2022).
Bauer, R., MacGowan, G. A., Blain, A., Bushby, K. & Straub, V. Steroid treatment causes deterioration of myocardial function in the δ-sarcoglycan-deficient mouse model for dilated cardiomyopathy. Cardiovasc. Res. 79, 652–661 (2008).
Rutschow, D. et al. S151A δ-sarcoglycan mutation causes a mild phenotype of cardiomyopathy in mice. Eur J Hum Genet 22, 119–125 (2014).
Coughlin, S. S. Post-traumatic stress disorder and cardiovascular disease. Open Cardiovasc. Med. J. 5, 164–170 (2011).
Polimanti, R. et al. Understanding the comorbidity between posttraumatic stress severity and coronary artery disease using genome-wide information and electronic health records. Mol. Psychiatry 27, 3961–3969 (2022).
Stein, M. B. et al. Genome-wide association analyses of post-traumatic stress disorder and its symptom subdomains in the Million Veteran Program. Nat. Genet. 53, 174–184 (2021).
Pathak, G. A. et al. Genetically regulated multi-omics study for symptom clusters of posttraumatic stress disorder highlights pleiotropy with hematologic and cardio-metabolic traits. Mol. Psychiatry 27, 1394–1404 (2022).
Pathak, G. A. et al. Genetic liability to posttraumatic stress disorder symptoms and its association with cardiometabolic and respiratory outcomes. JAMA Psychiatry 81, 34–44 (2024).
Lynall, M.-E. et al. Peripheral blood cell-stratified subgroups of inflamed depression. Biol. Psychiatry 88, 185–196 (2020).
McNally, L., Bhagwagar, Z. & Hannestad, J. Inflammation, glutamate, and glia in depression: a literature review. CNS Spectr. 13, 501–510 (2008).
Troubat, R. et al. Neuroinflammation and depression: a review. Eur J Neurosci 53, 151–171 (2021).
Eitel, I. et al. Inflammation in takotsubo cardiomyopathy: insights from cardiovascular magnetic resonance imaging. Eur. Radiol. 20, 422–431 (2010).
Adamo, L., Rocha-Resende, C., Prabhu, S. D. & Mann, D. L. Reappraising the role of inflammation in heart failure. Nat. Rev. Cardiol. 17, 269–285 (2020).
Maisch, B., Ristic, A. D. & Pankuweit, S. Inflammatory cardiomyopathy and myocarditis. Herz 42, 425–438 (2017).
Krejci, J., Mlejnek, D., Sochorova, D. & Nemec, P. Inflammatory cardiomyopathy: a current view on the pathophysiology, diagnosis, and treatment. BioMed Res. Int. 2016, 4087632 (2016).
Tschöpe, C. et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat. Rev. Cardiol. 18, 169–193 (2021).
Eitel, I. et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 306, 277–286 (2011).
Scally, C. et al. Myocardial and systemic inflammation in acute stress-induced (takotsubo) cardiomyopathy. Circulation 139, 1581–1592 (2019).
Rroku, A., Grahl, S., Landmesser, U. & Heidecker, B. A case report of myocardial inflammation in takotsubo syndrome. A chicken-or-the-egg phenomenon. Int. J. Cardiol. Heart Vasc. 39, 100958 (2022).
Lonsdale, J. et al. The Genotype-Tissue Expression (GTEx) project. Nat. Genet. 45, 580–585 (2013).
Bowton, E. et al. Biobanks and electronic medical records: enabling cost-effective research. Sci. Transl. Med. 6, 234cm3 (2014).
The All of Us Research Program Investigators. The ‘All of Us’ Research Program. N. Engl. J. Med. 381, 668–676 (2019).
Acknowledgements
This research is supported by the American Heart Association Fellowship AHA827137 (K.S.), National Institute of Mental Health R56MH120736 (L.K.D.), National Institute of Mental Health R01 H118233 (L.K.D. and J.W.S.), National Institutes of Health 1F31MH124306-01A1 (J.M.S.), and National Institutes of Health 1R01HL140074 (Q.S.W.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the paper. The de-identified EHR used at VUMC was supported by the National Center for Research Resources, Grant UL1 RR024975-01, and is now at the National Center for Advancing Translational Sciences, Grant 2 UL1 TR000445-06. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The dataset(s) used for the analyses described were obtained from Vanderbilt University Medical Center’s BioVU, which is supported by numerous sources: institutional funding, private agencies and federal grants. These include the NIH-funded Shared Instrumentation Grant S10RR025141, and CTSA grants UL1TR002243, UL1TR000445 and UL1RR024975. Genomic data are also supported by investigator-led projects that include U01HG004798, R01NS032830, RC2GM092618, P50GM115305, U01HG006378, U19HL065962 and R01HD074711, and additional funding sources listed at https://victr.vumc.org/biovu-funding/. The All of Us Research Program is supported by grants through the National Institutes of Health, Office of the Director: Regional Medical Centers: 1 OT2 OD026549, 1 OT2 OD026554, 1 OT2 OD026557, 1 OT2 OD026556, 1 OT2 OD026550, 1 OT2 OD026552, 1 OT2 OD026553, 1 OT2 OD026548, 1 OT2 OD026551 and 1 OT2 OD026555; IAA#: AOD 16037; Federally Qualified Health Centers: HHSN 263201600085U; Data and Research Center: 5 U2C OD023196; Biobank: 1 U24 OD023121; The Participant Center: U24 OD023176; Participant Technology Systems Center: 1 U24 OD023163; Communications and Engagement: 3 OT2 OD023205 and 3 OT2 OD023206; and Community Partners: 1 OT2 OD025277, 3 OT2 OD025315, 1 OT2 OD025337 and 1 OT2 OD025276. In addition to the funded partners, the All of Us Research Program would not be possible without the contributions made by its participants.
Author information
Authors and Affiliations
Contributions
K.S. and L.K.D. conceptualized and designed the work. K.S., J.M.S., T.M.-F., P.S. and H.L. implemented the computational procedures and performed data analysis. N.J.C., J.W.S., Q.S.W. and E.C.H. provided important clinical and intellectual insights. All authors read, edited and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
J.W.S. is a member of the Scientific Advisory Board of Sensorium Therapeutics (with equity) and has received an honorarium for an internal seminar Tempus Labs. He is a principal investigator of a collaborative study of the genetics of depression and bipolar disorder sponsored by 23andMe for which 23andMe provides analysis time as in-kind support but no payments. The other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Janitza Montalvo-Ortiz and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary methods and results.
Supplementary Tables
Supplementary Tables 1–10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, K., Lee, H., Sealock, J.M. et al. Genes associated with depression and coronary artery disease are enriched for cardiomyopathy and inflammatory phenotypes. Nat. Mental Health (2024). https://doi.org/10.1038/s44220-024-00219-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44220-024-00219-z



