Abstract
Clinical progress in multiple myeloma (MM), an incurable plasma cell (PC) neoplasia, has been driven by therapies that have limited applications beyond MM/PC neoplasias and do not target specific oncogenic mutations in MM. Instead, these agents target pathways critical for PC biology yet largely dispensable for malignant or normal cells of most other lineages. Here we systematically characterized the lineage-preferential molecular dependencies of MM through genome-scale clustered regularly interspaced short palindromic repeats (CRISPR) studies in 19 MM versus hundreds of non-MM lines and identified 116 genes whose disruption more significantly affects MM cell fitness compared with other malignancies. These genes, some known, others not previously linked to MM, encode transcription factors, chromatin modifiers, endoplasmic reticulum components, metabolic regulators or signaling molecules. Most of these genes are not among the top amplified, overexpressed or mutated in MM. Functional genomics approaches thus define new therapeutic targets in MM not readily identifiable by standard genomic, transcriptional or epigenetic profiling analyses.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
RNA-seq data that support the findings of this study are publicly available in the Gene Expression Omnibus (GEO) under accession code GSE186997. Previously published data that were reanalyzed here are available under accession codes GSE2113, GSE5900, GSE6477, GSE13591, GSE39754, GSE39925, GSE66293, GSE20540, GSE8958, GSE9067, GSE9367, GSE19748, GSE9782, GSE113031, GSE121912 and GSE79480. Molecular profiling data were derived for CCLE lines from the CCLE portal (https://portals.broadinstitute.org/ccle/data) or the Dependency Map portal (https://depmap.org/portal), for MM patient samples from MMRF Researcher Gateway (https://research.themmrf.org/) and for non-MM patient samples from the TCGA Research Network (https://portal.gdc.cancer.gov/, http://cancergenome.nih.gov/). Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding author on reasonable request.
Code availability
The analyses of our study involved standard workflows and sequential use of available code, for example, through R packages from CRAN (https://cran.r-project.org/) and Bioconductor (https://www.bioconductor.org) and R build-in functions for graphing, statistical tests and data analyses, for example, moderated t-test with the limma Bioconductor R package, Fisher’s exact test with the fisher.test R build-in function, survival analysis log-rank test the survival CRAN R package and gene expression analysis with edgeR Bioconductor R package. For processing large data matrices we used the data.table CRAN R package. For data visualization, for example, generation of heat maps with the ComplexHeatmap Bioconductor R Package, the circos plot with circlize Bioconductor R package and for dimensionality reduction visualization the tsne CRAN R package. We further used for data analysis and visualization the statistical and graphing software GraphPad Prism 9, heat maps with Morpheus (https://software.broadinstitute.org/morpheus/) and network analysis with StringDB (https://string-db.org/). RNA-seq raw data processing and generation of gene read counts were performed with STAR71.
References
Boise, L. H., Kaufman, J. L., Bahlis, N. J., Lonial, S. & Lee, K. P. The Tao of myeloma. Blood 124, 1873–1879 (2014).
Barwick, B. G., Gupta, V. A., Vertino, P. M. & Boise, L. H. Cell of origin and genetic alterations in the pathogenesis of multiple myeloma. Front. Immunol. 10, 1121 (2019).
Andrulis, M. et al. Targeting the BRAF V600E mutation in multiple myeloma. Cancer Discov. 3, 862–869 (2013).
Tsherniak, A. et al. Defining a cancer dependency map. Cell 170, 564–576 e16 (2017).
Shaffer, A. L. et al. IRF4 addiction in multiple myeloma. Nature 454, 226–231 (2008).
Hong, F. et al. CNPY2 is a key initiator of the PERK-CHOP pathway of the unfolded protein response. Nat. Struct. Mol. Biol. 24, 834–839 (2017).
Khatib, A. M. et al. Inhibition of proprotein convertases is associated with loss of growth and tumorigenicity of HT-29 human colon carcinoma cells: importance of insulin-like growth factor-1 (IGF-1) receptor processing in IGF-1-mediated functions. J. Biol. Chem. 276, 30686–30693 (2001).
Hawley, S. A. et al. Complexes between the LKB1 tumor suppressor, STRAD alpha/beta and MO25 alpha/beta are upstream kinases in the AMP-activated protein kinase cascade. J. Biol. 2, 28 (2003).
Tarumoto, Y. et al. LKB1, salt-inducible kinases, and MEF2C are linked dependencies in acute myeloid leukemia. Mol. Cell 69, 1017–1027 e6 (2018).
McMillin, D. W. et al. Tumor cell-specific bioluminescence platform to identify stroma-induced changes to anticancer drug activity. Nat. Med. 16, 483–489 (2010).
McMillin, D. W. et al. Compartment-specific bioluminescence imaging platform for the high-throughput evaluation of antitumor immune function. Blood 119, e131–e138 (2012).
McMillin, D. W., Negri, J. M. & Mitsiades, C. S. The role of tumour–stromal interactions in modifying drug response: challenges and opportunities. Nat. Rev. Drug Discov. 12, 217–228 (2013).
Rustad, E. H. et al. Revealing the impact of structural variants in multiple myeloma. Blood Cancer Discov. 1, 258–273 (2020).
Whyte, W. A. et al. Master transcription factors and mediator establish super-enhancers at key cell identity genes. Cell 153, 307–319 (2013).
Duan, S. et al. FBXO11 targets BCL6 for degradation and is inactivated in diffuse large B-cell lymphomas. Nature 481, 90–93 (2012).
Pasqualucci, L. et al. Inactivation of the PRDM1/BLIMP1 gene in diffuse large B cell lymphoma. J. Exp. Med. 203, 311–317 (2006).
Henske, E. P., Jozwiak, S., Kingswood, J. C., Sampson, J. R. & Thiele, E. A. Tuberous sclerosis complex. Nat. Rev. Dis. Primers 2, 16035 (2016).
Ozcan, U. et al. Loss of the tuberous sclerosis complex tumor suppressors triggers the unfolded protein response to regulate insulin signaling and apoptosis. Mol. Cell 29, 541–551 (2008).
Fedele, P. L. et al. IMiDs prime myeloma cells for daratumumab-mediated cytotoxicity through loss of Ikaros and Aiolos. Blood 132, 2166–2178 (2018).
Kronke, J. et al. Lenalidomide causes selective degradation of IKZF1 and IKZF3 in multiple myeloma cells. Science 343, 301–305 (2014).
Lu, G. et al. The myeloma drug lenalidomide promotes the cereblon-dependent destruction of Ikaros proteins. Science 343, 305–309 (2014).
Yamamoto, J. et al. ARID2 is a pomalidomide-dependent CRL4CRBN substrate in multiple myeloma cells. Nat. Chem. Biol. 16, 1208–1217 (2020).
An, J. et al. pSILAC mass spectrometry reveals ZFP91 as IMiD-dependent substrate of the CRL4CRBN ubiquitin ligase. Nat. Commun. 8, 15398 (2017).
Donovan, K. A. et al. Thalidomide promotes degradation of SALL4, a transcription factor implicated in Duaneradial ray syndrome. eLife 7, e38430 (2018).
Eichner, R. et al. Immunomodulatory drugs disrupt the cereblon–CD147–MCT1 axis to exert antitumor activity and teratogenicity. Nat. Med. 22, 735–743 (2016).
Hideshima, T. et al. p53-related protein kinase confers poor prognosis and represents a novel therapeutic target in multiple myeloma. Blood 129, 1308–1319 (2017).
Fischer, E. S. et al. Structure of the DDB1-CRBN E3 ubiquitin ligase in complex with thalidomide. Nature 512, 49–53 (2014).
Millrine, D., Tei, M., Gemechu, Y. & Kishimoto, T. Rabex-5 is a lenalidomide target molecule that negatively regulates TLR-induced type 1 IFN production. Proc. Natl Acad. Sci. USA 113, 10625–10630 (2016).
Fang, J. et al. A calcium- and calpain-dependent pathway determines the response to lenalidomide in myelodysplastic syndromes. Nat. Med. 22, 727–734 (2016).
Matyskiela, M. E. et al. A cereblon modulator (CC-220) with improved degradation of Ikaros and Aiolos. J. Med. Chem. 61, 535–542 (2018).
Sievers, Q. L. et al. Defining the human C2H2 zinc finger degrome targeted by thalidomide analogs through CRBN. Science 362, eaat0572 (2018).
Heider, M. et al. The IMiD target CRBN determines HSP90 activity toward transmembrane proteins essential in multiple myeloma. Mol. Cell 81, 1170–1186 e10 (2021).
Mitsiades, N. et al. Molecular sequelae of proteasome inhibition in human multiple myeloma cells. Proc. Natl Acad. Sci. USA 99, 14374–14379 (2002).
Mitsiades, C. S. et al. Inhibition of the insulin-like growth factor receptor-1 tyrosine kinase activity as a therapeutic strategy for multiple myeloma, other hematologic malignancies, and solid tumors. Cancer Cell 5, 221–230 (2004).
Barretina, J. et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 483, 603–607 (2012).
Dashevsky, O. et al. Use of olfactory receptor genes as controls for genome-scale CRISPR functional genomic studies to define treatment resistance mechanisms. Blood 136, 36–36 (2020).
Ferreira de Freitas, R. et al. Discovery of a potent and selective coactivator associated arginine methyltransferase 1 (CARM1) inhibitor by virtual screening. J. Med. Chem. 59, 6838–6847 (2016).
Shen, Y. et al. Discovery of a potent, selective, and cell-active dual inhibitor of protein arginine methyltransferase 4 and protein arginine methyltransferase 6. J. Med. Chem. 59, 9124–9139 (2016).
Cunningham, L. et al. Identification of benzodiazepine Ro5-3335 as an inhibitor of CBF leukemia through quantitative high throughput screen against RUNX1–CBFβ interaction. Proc. Natl Acad. Sci. USA 109, 14592–14597 (2012).
Zhao, C. et al. POU2AF1, an amplification target at 11q23, promotes growth of multiple myeloma cells by directly regulating expression of a B-cell maturation factor, TNFRSF17. Oncogene 27, 63–75 (2008).
Jahn, L. et al. TCR-based therapy for multiple myeloma and other B-cell malignancies targeting intracellular transcription factor BOB1. Blood 129, 1284–1295 (2017).
Toman, I. et al. Expression and prognostic significance of Oct2 and Bob1 in multiple myeloma: implications for targeted therapeutics. Leuk. Lymphoma 52, 659–667 (2011).
Gowda, P. S. et al. Runx2 suppression by miR-342 and miR-363 inhibits multiple myeloma progression. Mol. Cancer Res. 16, 1138–1148 (2018).
Obeng, E. A. et al. Proteasome inhibitors induce a terminal unfolded protein response in multiple myeloma cells. Blood 107, 4907–4916 (2006).
Timms, R. T. et al. Genetic dissection of mammalian ERAD through comparative haploid and CRISPR forward genetic screens. Nat. Commun. 7, 11786 (2016).
Groen, R. W. et al. Reconstructing the human hematopoietic niche in immunodeficient mice: opportunities for studying primary multiple myeloma. Blood 120, e9–e16 (2012).
Kumar, S. K. et al. Venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma (BELLINI): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 21, 1630–1642 (2020).
Panobinostat approved for multiple myeloma. Cancer Discov. 5, OF4 (2015).
Raab, M. S. et al. The first-in-human study of the pan-PIM kinase inhibitor PIM447 in patients with relapsed and/or refractory multiple myeloma. Leukemia 33, 2924–2933 (2019).
Ishiguro, K. et al. DOT1L inhibition blocks multiple myeloma cell proliferation by suppressing IRF4-MYC signaling. Haematologica 104, 155–165 (2019).
Drew, A. E. et al. Identification of a CARM1 inhibitor with potent in vitro and in vivo activity in preclinical models of multiple myeloma. Sci Rep. 7, 17993 (2017).
Nagel, S. et al. Identification of a tumor suppressor network in T-cell leukemia. Leuk. Lymphoma 58, 2196–2207 (2017).
Sheffer, M. et al. Genome-scale screens identify factors regulating tumor cell responses to natural killer cells. Nat. Genet. 53, 1196–1206 (2021).
Dufva, O. et al. Single-cell functional genomics of natural killer cell evasion in blood cancers. Preprint at bioRxiv https://doi.org/10.1101/2022.08.22.504722 (2022).
Meyers, R. M. et al. Computational correction of copy number effect improves specificity of CRISPR–Cas9 essentiality screens in cancer cells. Nat. Genet. 49, 1779–1784 (2017).
McFarland, J. M. et al. Improved estimation of cancer dependencies from large-scale RNAi screens using model-based normalization and data integration. Nat. Commun. 9, 4610 (2018).
Dempster, J. M. et al. Extracting biological insights from the Project Achilles genome-scale CRISPR screens in cancer cell lines. Preprint at bioRxiv https://doi.org/10.1101/720243 (2019).
Cowley, G. S. et al. Parallel genome-scale loss of function screens in 216 cancer cell lines for the identification of context-specific genetic dependencies. Sci. Data 1, 140035 (2014).
Li, W. et al. MAGeCK enables robust identification of essential genes from genome-scale CRISPR/Cas9 knockout screens. Genome Biol. 15, 554 (2014).
McDonald, E. R. 3rd et al. Project DRIVE: a compendium of cancer dependencies and synthetic lethal relationships uncovered by large-scale, deep RNAi screening. Cell 170, 577–592 e10 (2017).
Goldman, M. J. et al. Visualizing and interpreting cancer genomics data via the Xena platform. Nat. Biotechnol. 38, 675–678 (2020).
Law, C. W., Chen, Y., Shi, W. & Smyth, G. K. voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol. 15, R29 (2014).
Barwick, B. G. et al. Multiple myeloma immunoglobulin lambda translocations portend poor prognosis. Nat. Commun. 10, 1911 (2019).
Zhang, Y. et al. Model-based analysis of ChIP–seq (MACS). Genome Biol. 9, R137 (2008).
Amemiya, H. M., Kundaje, A. & Boyle, A. P. The ENCODE Blacklist: identification of problematic regions of the genome. Sci Rep. 9, 9354 (2019).
Yang, W. et al. Genomics of Drug Sensitivity in Cancer (GDSC): a resource for therapeutic biomarker discovery in cancer cells. Nucleic Acids Res. 41, D955–D961 (2013).
Szklarczyk, D. et al. The STRING database in 2017: quality-controlled protein–protein association networks, made broadly accessible. Nucleic Acids Res. 45, D362–D368 (2017).
Erb, M. A. et al. Transcription control by the ENL YEATS domain in acute leukaemia. Nature 543, 270–274 (2017).
Nabet, B. et al. The dTAG system for immediate and target-specific protein degradation. Nat. Chem. Biol. 14, 431–441 (2018).
Shirasaki, R. et al. Functional genomics identify distinct and overlapping genes mediating resistance to different classes of heterobifunctional degraders of oncoproteins. Cell Rep. 34, 108532 (2021).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Acknowledgements
This work was supported by grants NIH R01 CA050947 (C.S.M.), CA179483 (C.S.M.), CA196664 (C.S.M. and R.W.J.G.), R01CA276156 (C.S.M.), CA180475 (J.D.L. and C.S.M.), CA192844 (L.H.B.), U01CA225730 (C.S.M.) and U01CA176058 (W.C.H); and by the de Gunzburg Myeloma Research Fund (C.S.M.), Leukemia and Lymphoma Society (LLS) Translational Research Program (C.S.M.), LLS Quest for Cure Program (C.S.M. and R.W.J.G.), LLS Scholar Award (C.S.M.), LLS Specialized Center for Research (J.D.L.), LLS Special Fellow Award (D.D.R.), Multiple Myeloma Research Foundation (MMRF) Answer Fund (C.S.M., J.D.L. and L.H.B.), MMRF Translational Network of Excellence (C.S.M.), MMRF Epigenetics Program Project grant (J.D.L. and C.S.M.), Shawna Ashlee Corman Investigatorship in Multiple Myeloma Research (C.S.M.), Cobb Family Myeloma Research Fund (C.S.M.), Paula and Rodger Riney Foundation (L.H.B.), Chambers Family Advanced Myeloma Research Fund (C.S.M.), International Waldenstrom’s Macroglobulinemia Foundation (C.S.M.), Department of Defense grant W81XWH-15-1-0012 (A.C. and C.S.M.), International Myeloma Foundation (G.M.M.), American-Australian Association (G.M.M.), Associazione Italiana per la Ricerca sul Cancro (S.G.), Claudia Adams Barr Program in Innovative Basic Cancer Research at Dana-Farber Cancer Institute (M.S., E.D. and C.S.M.), Dutch Cancer Society grant VU2011-5127 (R.W.J.G.) and Ludwig Center at Harvard (C.S.M.). Q.L.S. was supported by award number T32GM007753 from the National Institute of General Medical Sciences. B.G.B. was supported by an MMRF Research Fellow Award and an ASH Research Scholar Award. V.A.G. was supported by the American Cancer Society grant #IRG-14-188-01 to the Winship Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of General Medical Sciences or the National Institutes of Health. The authors thank S. Sarkar, M. A. Bariteau and M. Borah for technical assistance in experiments related to this study and J. Sorrell for administrative coordination. The authors apologize in advance for the inability to reference in our paper all possible studies in the literature that are directly relevant to our findings.
Author information
Authors and Affiliations
Contributions
C.S.M. conceived the study, which was designed by R.d.M.S, F.V., A.C.C., A.T. and C.S.M. R.d.M.S., M.S., R.M.M., J.G.B., J.M.M., J.M.D. and A.C.C. performed computational analyses and interpretation of results from essentiality screens. R.d.M.S., B.G.B., V.A.G., D.D.-R. and C.J.O. analyzed and interpreted results from genome-wide chromatin accessibility. R.d.M.S., B.G.B. and A.C.C. implemented software for data analysis and visualization. R.d.M.S, B.G.B., K.I., M.S., R.M.M., J.G.B., F.V. and A.C.C. processed and managed data. P.J.H. assisted with computational analyses. D.A. and J.L. provided, on behalf of the MMRF CoMMpass study, data on myeloma patient-derived samples, and these data were analyzed by R.d.M.S., B.G.B., J.D.L., L.H.B. and J.J.K. Q.L.S., B.L.E., N.P.K., N.S.G., J.E.B., V.A.G., L.H.B. and F.V. provided research reagents. R.S., S.L.D.-K, G.M.M., S.Y., Y.H., M.S., O.D., S.G., P.J.H., J.B.B., E.D., H.T., B.J.G., C.J.O. and R.W.J.G. performed experimental studies or assisted in generation of experimental data. J.D.L., A.J.A., L.H.B., J.J.K., N.V.D., J.E.B., N.S.G., R.W.J.G., W.C.H. and A.T. provided advisory or supervisory roles in various components of the experimental procedures, computational analyses and data interpretation. C.S.M., F.V., A.T., W.C.H., L.H.B. and J.D.L. are the senior authors of this study. C.S.M. supervised the overall study. R.d.M.S., B.G.B., J.D.L, L.H.B., F.V., A.T. and C.S.M. wrote the manuscript with assistance from other authors.
Corresponding authors
Ethics declarations
Competing interests
R.S. serves research funding from FIMECS and honoraria from Janssen Pharma. G.M.M. is an employee of Aculeus Therapeutics. N.V.D. is an employee of Genentech, a member of the Roche Group. A.J.A. has consulted for Anji Pharmaceuticals, Arrakis Therapeutics, AstraZeneca, Boehringer Ingelheim, Oncorus, Inc., Merck & Co., Inc., Mirati Therapeutics, Nimbus Therapeutics, Plexium, Revolution Medicines, Reactive Biosciences, Riva Therapeutics, Servier Pharmaceuticals, Syros Pharmaceuticals and T-knife Therapeutics. A.J.A. holds equity in Riva Therapeutics. A.J.A. has research funding from Bristol Myers Squibb, Deerfield, Inc., Eli Lilly, Mirati Therapeutics, Novartis, Novo Ventures, Revolution Medicines and Syros Pharmaceuticals. C.J.O. has received research support from Gilead, Scorpion Therapeutics and eFFECTOR Therapeutics. J.M.D. is a consultant and holds equity in Jumble Therapeutics. B.L.E. has received research funding from Celgene, Deerfield, Novartis and Calico and consulting fees from GRAIL. He is a member of the scientific advisory board and shareholder for Neomorph Inc., TenSixteen Bio, Skyhawk Therapeutics and Exo Therapeutics. J.E.B. is a Scientific Founder of Syros Pharmaceuticals, SHAPE Pharmaceuticals, Acetylon Pharmaceuticals, Tensha Therapeutics (now Roche) and C4 Therapeutics and is the inventor on intellectual property licensed to these entities. J.E.B. has recently served as an executive and shareholder in Novartis AG. N.K. is currently an employee of Kymera Therapeutics, Inc. N.S.G. is a founder, science advisory board member (SAB) and equity holder in Syros, C4, Allorion, Lighthorse, Voronoi, Inception, Matchpoint, CobroVentures, GSK, Shenandoah (board member), Larkspur (board member) and Soltego (board member). The Gray lab receives or has received research funding from Novartis, Takeda, Astellas, Taiho, Jansen, Kinogen, Arbella, Deerfield, Springworks, Interline and Sanofi. J.J.K. has received research funding from Amgen, Genentech and Janssen. J.M.M. has received research funding from the Dependency Map Consortium. W.C.H. is a consultant for Thermo Fisher, Solasta Ventures, MPM Capital, KSQ Therapeutics, Frontier Medicines, Tyra Biosciences, Function Oncology, Jubilant Therapeutics, Riva Therapeutics, RAPPTA Therapeutics, Calyx and Serinus Biosciences. L.H.B. is a consultant for and receives honoraria and research funding from AstraZeneca, and is a consultant for Genentech and Abbvie. J.D.L. receives research funding from Ipsen/Epizyme and is consultant for AstraZeneca. A.T. is a consultant for Cedilla Therapeutics, Foghorn Therapeutics and The Center for Protein Degradation (Deerfield), and is a SAB member and holds equity in Turbine Simulated Cell Technologies. F.V. receives research support from the Dependency Map Consortium, Bristol Myers Squibb, Novo Ventures and Riva Therapeutics, and has shares and is a consultant for Riva Therapeutics. C.S.M. serves on the Scientific Advisory Board of Adicet Bio and discloses consultant/honoraria from Genentech, Fate Therapeutics, Ionis Pharmaceuticals, FIMECS, Secura Bio and Oncopeptides, and research funding from Janssen/Johnson & Johnson, EMD Serono, Arch Oncology, Karyopharm, Sanofi, Nurix, BMS, H3 Biomedicine/Eisai, Springworks, Abcuro and Novartis. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Francesco Maura and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 MM-preferential dependencies in genome-scale CRISPR-based gene-editing screens.
a, Summary matrix of results for identification of MM-preferential dependencies in genome-scale CRISPR-based gene-editing screens from different releases of the Dependency Map program. The criteria used to identify MM preferential dependencies in the 20Q4v2 Dependency Map data were also applied in earlier releases (18Q3 to 20Q3). The matrix summarizes results for all genes that met these criteria in at least one of the releases. Black or white indicate, respectively, that a gene did vs. did not meet criteria for MM preferential dependency in the respective data release (gray signifies that CERES scores were not calculated for a given gene in the data release). b, MM-preferential dependencies clustered according to molecular pathways represented in this group of genes. Color-coded heatmaps for CERES scores following the format of Fig. 1a. Genes are clustered based on their related functional groups, pathways, or biological functions, based on aggregate information from the literature. c-d, Molecular pathways enriched for MM-preferential dependencies. c, Schematic representation of functional groups represented in the MM-preferential dependencies, such as transcription factors/co-factors, other regulators of transcriptional responses and chromatic signaling; kinases serving as upstream regulators of these pathways (for example, kinases activating NF-κB); or endoplasmic reticulum/Golgi regulators. d, Visualization of the direct (physical) and indirect (functional) associations of the MM-preferential dependencies, based on computational prediction, knowledge transfer between organisms, interactions aggregated from other (primary) databases or other resources integrated and visualized by the online STRING database (https://string-db.org/, v11.0)67.
Extended Data Fig. 2 Additional metrics of essentiality for MM preferential dependencies.
a-b, Ranks of CERES scores or DNA copy number-uncorrected ranks of sgRNA depletion for MM-preferential dependencies. Essentiality metrics are depicted in color-coded heatmaps similar in format to Fig. 1a, with results presented for MM lines as a matrix (each line in a separate column) while results for non-MM lines are stacked separately for each gene from lowest to highest essentiality (from left to right in each row). For each cell line, the top 3000 genes with the lowest CERES scores (in a) or with most pronounced sgRNA depletion based on MAGeCK rank aggregation (in b) are depicted in green or purple, respectively. For each cell line, the top 100 genes with highest CERES scores (in a) or highest MAGeCK ranks for sgRNA enrichment (in b) are depicted in purple and yellow/orange, respectively, according to the respective color-coded scales. c-d, Patterns of depletion for shRNAs targeting genes defined by CRISPR as MM-preferential dependencies. c, DEMETER2 scores are depicted as a matrix for MM (n = 13 cell lines; right) and as separate stacked plots for non-MM (n = 461 cell lines; left), according to the color-coded scale (black/blue for shRNA depletion; yellow/orange/brown for shRNA enrichment; white for DEMETER2 scores between -0.4 and +0.4; and gray for genes not examined in the shRNA screen of the respective cell line). d, DEMETER2 scores for key examples of MM-preferential dependencies are depicted (in rows) for both non-MM (left) and MM lines (right) as stacked bar graphs, according to the color-coded scale.
Extended Data Fig. 3 Patterns of expression of MM-preferential dependencies in MM vs non-MM cell lines.
RNA-Seq data (CCLE dataset) for MM-preferential dependencies in MM vs. non-MM cell lines. Transcript levels (log2(TPM + 1)) for each gene (row) across MM and non-MM cell lines are scaled by maximum value resulting in a value range between 0 and 1 and presented as stacked bar plots. Color bars on the side of the graph denote different clusters of genes, defined based on analyses of Fig. 3 (based on 2-sided limma t-test FDR and log2FC of differential expression of each gene in MM vs non-MM lines).
Extended Data Fig. 4 Patterns of transcript levels for MM-preferential dependencies in different biological or clinical contexts.
a, RNA-Seq data for MM-preferential dependencies in patient-derived tumor samples for MM vs. non-MM. Transcript levels (presented as stacked plots) for each gene (row) across MM (n = 591 samples; MMRF CoMMpass study, IA8 release) and non-MM (n = 11060 samples, TCGA; accessed from GDAC). Raw counts were voom normalized, negative voom values were set to zero, scaled by maximum value for each gene, resulting in a value range between 0 and 1. Concordant observations also obtained with other versions of MMRF and TCGA datasets. b, Comparative analyses of transcript levels for MM-preferential dependencies in different stages of myelomagenesis or settings with distinct differences in clinical or biological aggressiveness of MM. Heatmap summarizes results from comparisons performed between groups of samples within each of the gene expression profiling datasets indicated in the figure. Red and blue denote statistically significant (FDR < 0.05, Limma t-test, log2FC > 1.0 or < -1.0) up- or down-regulation, respectively, for a gene in a given group of samples vs. its indicated comparator group. Genes in gray do not have perfect match probes in the respective array. White indicates no statistically significant difference for a given comparison. Number of samples per group is indicated next to each comparison. c-e, Transcript levels of most MM-preferential dependencies do not consistently correlate with adverse clinical outcome. c, Overall survival (OS) or progression free survival (PFS) were examined for MM patients at high vs. intermediate vs. low tertiles of expression of each MM-preferential dependency in each dataset indicated in the graph (see Methods). Red and blue denote statistically significant (at FDR < 0.05, two-sided log-rank test) correlation of transcript levels for a given gene with adverse or favorable, respectively, clinical outcome (white indicates FDR > 0.05). d-e, Cumulative plots summarizing results of c, in terms of OS (d), or PFS (e), between MM patients with high vs. intermediate vs. low tertile of expression of each gene in each dataset indicated in the graph. For each potential FDR value (x-axis), the y-axis depicts, separately for OS or PFS in each dataset, the cumulative fraction of MM-preferential dependencies exhibiting FDR levels equal or lower to those depicted in each respective position of the x-axis. For all evaluated datasets, <25% of MM-preferential dependencies exhibit FDR < 0.05 for the correlation of transcript levels with PFS or OS. Number of patient samples in c-e is indicated for each dataset.
Extended Data Fig. 5 Genomic landscape of MM-preferentially essential genes.
a, Mutational and DNA copy number data for MM-preferential dependencies in MM vs. non-MM cell lines is included in heatmaps of CERES scores (similar to the format of Fig. 1a). Green stars represent non-synonymous mutations; while CNV gains and losses are depicted by ‘+’ or ‘-’, respectively. In stacked plots for non-MM cell lines, green stars are also stacked and are not linked with the CERES scores in respective lines. b, Rank of genes with most frequent CNV gains in MM patient tumor samples (N = 932 samples; N = 18,057 genes with CERES data (20Q4v2) and CNV data in CoMMpass study, IA15 release): MM-preferential dependencies are highlighted in red and their gene symbols are labeled for those MM-preferential dependencies ranked in the top 200 genes (genes are ranked on the x-axis on a log2 scale). c, Top hotspots for gain of structural variants (SVs) ranked based on their frequency in MM patient tumor samples (CoMMpass study), derived from analyses of Rustad et al.13. MM-preferential dependencies residing in 8 of these hotspots are highlighted, and those in bold have not been previously proposed as candidate drivers of the respective hotspots. Gray denotes hotspots which contain no genes evaluated in the genome-scale CRISPR screens. d, Heat maps for CERES scores in MM vs. non-MM lines of genes in each of the 8 SV gain hotspots of panel c that contain MM-preferential dependencies.
Extended Data Fig. 6 Overlap or proximity of chromatin accessible regions with MM-preferential dependencies.
a, Plot of stitched regions of chromatin accessibility with average ATAC-seq signal (RPPM) across 22 MM cell lines shown in gray. Black lines denote the inflection point that denotes super-accessible (SA) regions. Regions within 100 kb of MM-preferential dependencies are denoted by red tick marks on the bottom and the odds ratio (OR) and P-value (two-sided Fisher’s exact test) of enrichment of MM-preferential dependencies found near super-accessible regions are shown. b, Heatmap of chromatin accessible regions within 100 kb of MM-preferential dependencies across 22 MM cell lines. c-f, Genomic plots of ATAC-seq for select examples of MM-dependencies (PRDM1, IRF4, POU2AF1, UBE2J1) that overlap with super-accessible (SA) regions. Each cell line is shown in a transparent gray and the average is shown in black. Note the proximity of IRF4 and DUSP22 and the multiple prominent areas of accessible chromatin within intronic regions of DUSP22. g, Hierarchical clustering of MM cell lines based on their CERES scores for MM preferential dependencies. MM cell lines are annotated for their status for genomic events, such as translocations targeting CCND1, CCND2, CCND3, MAF, MAFB, MMSET/NSD2, mutations for KRAS or NRAS, loss-of-function for TP53; or the functional status of their dependence (based in CRISPR data) on either MAF or MAFB.
Extended Data Fig. 7 Comparative analysis of CERES scores for MM preferential dependencies in MM vs other hematologic malignancies vs. solid tumors.
Results are presented in a manner similar to Fig. 1, with stacked bar plots for solid tumors (left); separate matrices for cell lines from non-MM hematologic malignancies (middle) vs. MM (right). Genes are included in 7 different clusters determined based on the criteria included in the color-coded bars on the right-hand side of the graph (FDR of comparison of CERES scores and difference in average CERES scores in MM vs. non-MM hematologic cell lines; Fisher’s test FDR for comparison of CERES ranks; absolute difference in % of MM vs. non-MM hematologic cell lines with CERES scores ≤ -0.4; and % of MM lines with CERES score ≤ -0.4). Results highlight that several MM-preferential dependencies are shared between MM and other hematologic malignancies, but many others are preferentially essential only for MM cell lines, a statement also supported by results of Extended Data Fig. 8.
Extended Data Fig. 8 MM-preferential dependencies with distinct vs. overlapping roles in MM vs. other hematologic neoplasias or solid tumors.
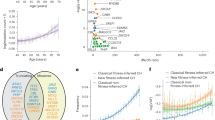
a, Heat map for MM-preferential dependencies, summarizing their potential roles as preferential dependencies for other malignancies. Color coding indicates the difference in average CERES score for each gene in a given tumor type vs. all others: black/blue or red/orange denote FDR < 0.05 and lower or higher, respectively, average CERES scores for a given gene in the respective neoplasia vs. all other cancer types. White denotes FDR > 0.05. b-c, t-SNE plots of cell lines (depicted as dots), from MM, leukemias, lymphomas or other neoplasias, clustered according to RNA-Seq profiles b, or CERES scores c, for MM-preferential dependencies. RPKM data in b from CCLE [2018] for lines with matching 20Q4v2 CERES scores (N = 15, 33, 16, 505 lines, respectively). In c, N = 19, 44, 20, 706 lines, respectively (20Q4v2). d, Numbers of CRISPR-defined preferential dependencies (y-axis; identified based on the same criteria applied for MM) vs. number of lines for each indicated tumor type (x-axis). e, Volcano plot of -log10FDR (Limma t-test) for comparison of CERES scores in MM vs non-MM hematopoietic cell lines (y-axis) vs. difference in average CERES scores in MM vs. non-MM cell hematopoietic lines (x-axis). MM-preferential dependencies (identified in this study by comparison of MM vs. all non-MM cell lines) are depicted in red and orange, respectively, if they did vs. did not exhibit significantly lower CERES scores in MM compared with non-MM hematopoietic lines. f-h, Dependencies with differential role in MM vs. solid tumors or vs. B-cell lymphomas. Volcano plots for comparisons of CERES scores in MM lines (N = 19) vs. f, all non-MM cell lines, from both hematologic malignancies and solid tumors (N = 768; also see Supplementary Table 1); g, only solid tumor cell lines (N = 701); h, B cell lymphoma lines (N = 13) (x-axis: difference in average CERES scores between respective groups; y-axis: -log10FDR, Limma t-test). Red dots in each plot indicate genes satisfying criteria for more pronounced essentiality in MM compared with the respective groups of cell lines; i, Venn diagram highlighting genes with differential role in MM vs. solid tumors or B-cell lymphomas, based on panels f-h. j, CERES scores for genes that do not meet criteria for MM-preferential dependencies (comparison of MM vs. all other non-MM lines), but are more essential in MM vs. solid tumors or B-cell lymphomas, based on panels f-h.
Extended Data Fig. 9 Pattern of essentiality for genes downstream of IRF4 or IKZF1/IKZF3.
CERES scores for genes previously defined as a, IRF4 target genes in MM cells5 or b, genes that are downregulated by loss-of-function of IKZF1 or IKZF3 (GSE113031) are depicted in a heatmap format (similar to Fig. 1) and in clusters of genes which (i) can be considered ‘core essential’ genes (for example, CERES < -0.4 in ≥90% of cell lines across cancers); (ii) meet all criteria for MM-preferential dependencies vs. other genes that have CERES scores < -0.4 in (iii) >50% of MM cell lines tested, (iv) 30-50% of MM cell lines tested; (v) <30% of MM cell lines tested; or (vi) none of the MM cell lines tested.
Extended Data Fig. 10 Molecular and functional studies of POU2AF1 and ER-associated dependencies.
a-b, Immunoblotting analyses to confirm that protein levels of POU2AF1 are decreased with Doxy-inducible CRISPR interference (a, KMS11 cells) and increased with CRISPR activation (b, LP-1 cells) compared to cells with sgRNAs for control OR genes. Beta-actin a, or vinculin b, were probed as loading controls in the same respective membrane concurrently with POU2AF1. c, Relative numbers of viable LP-1 cells with CRISPR-based activation of POU2AF1 vs. a control OR gene (day 12 after end of transduction with sgRNAs for POU2AF1; results qualitatively concordant with those at later time-point in Fig. 6b). CTG assay, mean +/− s.e.m. results; n = 6 independent replicate cell cultures per condition; one-way ANOVA and Tukey’s post-hoc test (detailed results included in Source Data), p < 0.001 for each POU2AF1 sgRNA vs. OR12D2 sgRNA). d, Immunoblotting for UBE2J1 after doxy-inducible CRISPR-based KO of UBE2J1 (or a control OR gene). Vinculin was probed as loading control concurrently with the staining for UBE2J1. Each experiment in a-d was performed once. e, UBE2J1, its dislocon complex partners SEL1L, SYVN1, and other ER-related MM preferential dependencies are among the top ‘hits’ in two genome-scale screens (using retroviral gene-trap mutagenesis and CRISPR gene-editing)45 for genes involved in ERAD regulation (in KBM7 haploid cells). f, In vitro bortezomib treatment (24 h) of KMS18 cells with Doxy-inducible CRISPR KO of SYVN1 or control OR genes. (CTG; mean +/− s.e.m.; n = 8 independent replicate cell cultures for drug-free control and n = 4 independent replicate cell cultures per drug dose for each KO; 2-way ANOVA (p < 0.001); detailed results of Tukey post-hoc tests included in Source Data). g-h, Patterns of CERES scores in MM (n = 19) and non-MM (n = 770) lines for g, ER/ERAD/Golgi-related genes and h, select ER genes. Results are presented similar to format of Fig. 1. Highlighted gene symbols include MM-preferential dependencies (red); examples of core essential genes (green); and genes which do not meet all criteria for MM-preferential dependencies but are recurrently essential for MM cell lines and are linked with the function of the ER glycoprotein quality control system (blue) and the ER translocon system (purple).
Supplementary information
Supplementary Information
Supplementary Figs. 1–8 and legends to Supplementary Figs. 1–8.
Supplementary Table 1
One file with multiple tabs, namely Supplementary Table 1 with data, Supplementary Table 2 with list of reagents resources and Supplementary Table 3 with list of sgRNAs and primers.
Source data
Source Data Fig. 1
Source data for Fig. 1.
Source Data Fig. 2
Source data for Fig. 2.
Source Data Fig. 3
Source data for Fig. 3.
Source Data Fig. 4
Source data for Fig. 4.
Source Data Fig. 5
Source data for Fig. 5.
Source Data Fig. 6
Source data for Fig. 6.
Source Data Fig. 7
Source data for Fig. 7.Fig. DataFig.6
Source Data Fig. 8
Source data for Fig. 8.
Source Data Extended Data Fig. 1
Source data for Extended Data Fig. 1.
Source Data Extended Data Fig. 2
Source data for Extended Data Fig. 2.
Source Data Extended Data Fig. 3
Source data for Extended Data Fig. 3.
Source Data Extended Data Fig. 4
Source data for Extended Data Fig. 4.
Source Data Extended Data Fig. 5
Source data for Extended Data Fig. 5.
Source Data Extended Data Fig. 6
Source data for Extended Data Fig. 6.
Source Data Extended Data Fig. 7
Source data for Extended Data Fig. 7.
Source Data Extended Data Fig. 8
Source data for Extended Data Fig. 8.
Source Data Extended Data Fig. 9
Source data for Extended Data Fig. 9.
Source Data Extended Data Fig. 10
Source data for Extended Data Fig. 10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Matos Simoes, R., Shirasaki, R., Downey-Kopyscinski, S.L. et al. Genome-scale functional genomics identify genes preferentially essential for multiple myeloma cells compared to other neoplasias. Nat Cancer 4, 754–773 (2023). https://doi.org/10.1038/s43018-023-00550-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-023-00550-x