Abstract
Kazakhstan has one of the lowest heart transplantation (HTx) rates globally, but there are no studies evaluating the outcomes of HTx. This study aimed to provide a comprehensive analysis of the national HTx program over a 12-year period (2012–2023). Survival analysis of the national HTx cohort was conducted using life tables, Kaplan‒Meier curves, and Cox regression methods. Time series analysis was applied to analyze historical trends in HTx per million population (pmp) and to make future projections until 2030. The number of patients awaiting HTx in Kazakhstan was evaluated with a regional breakdown. The pmp rates of HTx ranged from 0.06 to 1.08, with no discernible increasing trend. Survival analysis revealed a rapid decrease in the first year after HTx, reaching 77.0% at 379 days, with an overall survival rate of 58.1% at the end of the follow-up period. Among the various factors analyzed, recipient blood levels of creatinine and total bilirubin before surgery, as well as the presence of infection or sepsis and the use of ECMO after surgery, were found to be significant contributors to the survival of HTx patients. There is a need for public health action to improve the HTx programme.
Similar content being viewed by others
Introduction
According to the universal definition of heart failure (HF), it is characterized as a clinical syndrome marked by symptoms and/or signs stemming from structural and/or functional abnormalities in the heart1. Recognized as a global pandemic, HF reached an estimated worldwide prevalence of 64.3 million people in 20172 and is anticipated to increase due to extended life expectancy and enhanced survival of HF patients attributed to life-saving treatments3. The advanced stage of HF necessitates surgical intervention. Heart transplantation (HTx) is considered the gold standard among these interventions and is likely to enhance survival and improve quality of life in such patients4. In addition to HTx, a variety of ventricular assist devices are available, with left ventricular assist devices (LVADs) being the most commonly implanted5.
Despite the benefits of HTx, there is a shortage of hearts available for transplantation, and only a limited number of eligible patients receive these interventions. While there was a decline in HTx numbers from the 1990s to the early 2000s, the trend has been on the rise over the past decade6. According to data from the Global Observatory on Donation and Transplantation (GODT), 8988 hearts were transplanted globally in 2022, representing a 7% increase from 2021. The per million population (pmp) rates of HTx are highest in the Americas (5.1) and European region (3.5) and lowest in the African region, where they equal 0.0 in 20227.
Kazakhstan, a post-Soviet country in Central Asia, has one of the lowest HTx rates globally7. The country initiated its first heart transplantation in 2012 and concurrently launched an LVAD implantation program. Despite an early-stage analysis of the LVAD program8, there is a notable dearth of studies evaluating the national HTx program. Consequently, this study aims to comprehensively analyze the national HTx program over a 12-year period (2012–2023), focusing on both its outputs and outcomes. Specifically, this study aimed to elucidate outputs by examining historical trends in HTx and the population in need. The rates of LVAD implantation will be juxtaposed with those of HTx. Future projections until 2030 will be conducted to forecast the demand for these services. Furthermore, this study intends to scrutinize the number of patients awaiting HTx in Kazakhstan, with a regional breakdown. Additionally, this study aimed to assess the outcomes of the national HTx program by conducting a survival analysis of the national HTx cohort.
Methods
This study consists of two distinct stages: the analysis of HTx program outputs and outcomes. The primary source of data was the Republican Center for Coordination of Transplantation and High-Tech Services, hereafter referred to as the Transplantation Coordination Center, under the Ministry of Health (MoH) of Kazakhstan. Functioning as the national agency providing technical support to all hospitals performing organ transplantations in Kazakhstan, this center is responsible for maintaining the medical information system, specifically the Registry of Donors and Recipients, which encompasses data on donors and recipients for various organ transplantations.
The regulation of organ acquisition and donor management in Kazakhstan is governed by the Transplant Act. This legislation aligns with the principles outlined by the International Society for Heart and Lung Transplantation (ISHLT)9. According to the Act, organs can be donated following brain death by individuals aged 18 years and older, provided that they have officially confirmed their willingness for postmortem organ donation during their lifetime. This declaration of intent can be made through the "electronic government" web portal or through a general practitioner. In cases where explicit consent from the individual is not available, organ donation is contingent upon the consent of their family10.
Presently, four hospitals in Kazakhstan conduct HTx, with the National Scientific Cardiac Surgery Center in Astana being the primary facility for the majority of HTx and LVAD implantations nationwide. The other three hospitals undertaking these surgical interventions are the Heart Center Shymkent, the Research Institute of Cardiology and Internal Diseases, and the National Scientific Center of Surgery named after Syzganov. The operations of the Transplantation Coordination Center, including the management of the Registry of Donors and Recipients, are governed by the Ministry of Health's directive11.
Analysis of the output parameters in the heart transplantation program
Analysis of data on HTx and LVAD implantation in Kazakhstan
The annual nationwide rates of HTx and LVAD implantation were computed per million population (pmp). This involved retrieving the number of HTx and LVAD implantations performed in Kazakhstan from the inception of these procedures in 2012 to the present year (2023) from the Registry. Population figures for Kazakhstan in the respective years were sourced from the Demographic Yearbook, a statistical compilation issued by the Bureau of National Statistics12. The aggregated data encompassing nationwide annual incidences of ischemic heart disease (IHD) and heart valve disease (HVD), along with the pmp rates of HTx and LVAD implantations, were organized in an Excel spreadsheet, indicating the reference year for the statistics.
Analysis of incidence rates of ischemic heart disease and heart valve disease
To augment the findings of our study regarding the rates of HTx and LVAD implantation and to generate forecast projections concerning future healthcare needs in the country, we obtained official statistics on the incidence rates of IHD and HVD in Kazakhstan. These two medical conditions represent the primary indications for HTx and LVAD implantation, in accordance with the national standard of care13. The MoH of Kazakhstan annually publishes a yearbook of national health statistics14. For our research, we retrieved data on the incidence of IHD and HVD spanning the years 1998 to 2022 from this resource. The electronic versions of these yearbooks are freely accessible on the website of the National Research Center for Health Development named after Salidat Kairbekova, and details on studies conducted utilizing this yearbook's information are available elsewhere15.
We downloaded yearbooks covering the period from 1998 to 2022 and extracted precalculated incidence rates of IHD and HVD from the "Health Indicators" subsection. The incidence of IHD specifically pertains to adults, defined as individuals aged 18 years and older, and is presented per 100,000 people. Similarly, the incidence of HVD is based on the total population, encompassing both adults and children, and is also presented per 100,000 people.
Time series analysis
The Expert Modeler function of SPSS was employed to automatically identify the best-fit epidemiological models for each type of predictive analysis: incidence rates of IHD and HVD, as well as pmp rates of HTx and LVAD implantation until 2030. The observed incidences from 1998 to 2022 were utilized for IHD and HVD, while the observed rates for HTx and LVAD implantation from 2012 to 2023 were employed. All projections were reported as estimates along with their 95% confidence intervals (CIs), and corresponding graphs were generated. The significance level for the best-fit epidemiological models was set at 0.05.
Geospatial analysis
The cumulative figures of all adult and pediatric patients awaiting heart transplantation across Kazakhstan's regions from the inception of the program to the end of 2023 were entered into an Excel spreadsheet. The population data for each region of Kazakhstan were acquired from the website of the Bureau of National Statistics to calculate the pmp rates16. To visualize regional variations in the rates of patients awaiting HTx, the Quantum Geographic Information System (QGIS) Version 3.26 "Buenos Aires" was used.
Analysis of the outcome parameters in the heart transplantation program
Survival analysis was conducted to evaluate the outcome parameters of the national HTx program. Data on all HTx patients in Kazakhstan were acquired in a fully anonymized manner from the Transplantation Coordination Center. The dataset retrieved from the Registry for HTx patients included various details, such as the date of the HTx procedure, date of death (if applicable), age and sex, blood group and rhesus D (RhD) factor, as well as the weight and height of both the donor and recipient. The inclusion of the latter two variables facilitated the calculation of body mass index (BMI) using the following formula: weight in kilograms divided by height in meters squared. Additionally, information on the cause of death of heart donors was obtained from the registry. Currently, brain death serves as the sole parameter for organ acquisition10, and the causes of donor death are categorized into four broad groups: ischemic stroke, hemorrhagic stroke, brain injury, and neoplasm.
For heart recipients, more extensive data were available, including laboratory values before HTx surgery, such as hemoglobin, creatinine, glomerular filtration rate (GFR), total bilirubin, lactate dehydrogenase, sodium, potassium, white blood cell count, and C-reactive protein. Information related to previous cardiac surgeries, as well as coexisting pathologies such as arterial hypertension, hypothyroidism, pulmonary hypertension, and the type of cardiomyopathy, was also obtained from the registry. In addition, information on the length of postoperative hospital stay and postsurgical morbidity [infection/sepsis, rejection within hospital stay, hemodialysis, resternotomy, and extracorporeal membrane oxygenation (ECMO)] was available and extracted from the registry.
Life tables, Kaplan‒Meier analysis (K‒M analysis), and Cox regression were the three survival analysis methods employed in this study. The data sourced from the registry were organized in Excel spreadsheets, with the primary variables being the date of HTx, the date of death, or the conclusion of the follow-up period (30th November 2023). Given the unavailability of precise causes of death for HTx patients, overall survival was reported.
Life tables were generated to estimate cumulative survival at specific time intervals: 30 days, 90 days, 180 days, 360 days, 720 days, 1080 days, 1380 days, and 1740 days. The number of patients who survived and those who died at the end of each interval was documented. Cumulative mortality rates were calculated using the following formula: 100 − cumulative survival.
K‒M analysis was employed to assess the probability of surviving until the end of the follow-up, along with the mean and median survival of HTx patients, presented with 95% CIs. Since the cumulative survival at the end of the follow-up was 58.1%, only the mean survival time was reported. A graph depicting the overall survival curve during the study period was generated.
Multivariate Cox regression analysis was employed to assess the risk factors associated with mortality among HTx patients. The selection of factors was based on their independence from each other. These factors were categorized into two main groups, donor-related and recipient-related, and their respective effects were reported separately. The donor-related factors included age, sex, weight, height, blood group, RhD factor, and cause of death. Recipient-related factors were further subdivided into three categories: presurgical factors (such as age, sex, weight, height, blood group, RhD factor, history of previous cardiac surgeries including LVAD implantation, arterial hypertension, hypothyroidism, pulmonary hypertension, and type of cardiomyopathy—ischemic, dilated, or valvular), presurgical laboratory values (including hemoglobin levels (g/L), creatinine levels (mg/dL), GFR (mL/min), total bilirubin levels (mg/dl), lactate dehydrogenase levels (U/L), sodium levels (mmol/L), potassium levels (mmol/L), white blood cell count, and C-reactive protein levels (mg/L)), and postsurgical factors (such as length of postoperative hospital stay and postsurgical morbidity including infection/sepsis, rejection within hospital stay, requirement for hemodialysis, resternotomy, and ECMO). Adjusted hazard ratios (HRs) were computed for all variables, and the statistical significance level of the Cox regression model was set at 0.05. Survival analysis was performed using the "Survival" function in the Statistical Package for Social Sciences (SPSS) version 24.0 for Windows.
Ethics declaration
This study was conducted in strict accordance with the principles outlined in the Helsinki Declaration. Only completely anonymized data obtained from the Transplantation Coordination Center were analyzed. Prior to commencing the data collection, approval was obtained from the Local Commission on Bioethics of the Corporate Fund “University Medical Center” (hereafter referred to as the Ethics Committee). The Ethics Committee reviewed the case and waived the need for informed consent, as documented in the Minutes of the meeting of Ethics Committee #3 dated July 14, 2023.
Results
Output study
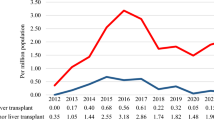
The first HTx and LVAD implantation in Kazakhstan occurred in 2012. Over the period of 2012–2023, 92 HTx and 493 LVAD implantations were performed. Specifically, there was one HTx in 2012, two in 2013, seven in 2014, nineteen in 2015, fifteen in 2016, nineteen in 2017, eight in 2018, nine in 2019, two in 2020, two in 2021, four in 2022, and four in 2023. Notably, the peak number of HTx procedures occurred between 2015 and 2017, while the lowest number of LVAD implantations was observed during the same period. Figure 1 illustrates a declining trend in the pmp rates of HTx and LVAD patients. The percentage of annual decline for HTx was 2.03% (95% CI, from − 19.11 to 18.66%, p = 0.408), and for LVAD implantation, it was 1.39% (95% CI, from − 4.44 to 1.76%, p = 0.173).
Table 1 provides estimates of the projected incidence rates of IHD and HVD, the major indications for HTx according to national standards of care13. The table also presents estimates of the projected per capita rates of HTx and LVAD implantation. The rate of IHD is projected to increase to 610.0 per 100,000 people (95% CI from 517.7 to 702.4) in 2025 and to increase to 671.3 (95% CI from 579.0 to 763.7) in 2030. However, according to projections, no growth is expected for HTx and LVAD implantations. Figure 2 indicates a steady increase in IHD incidence from 1998 to 2022, with this trend expected to continue. Conversely, the trends for HTx and LVAD implantation appeared stable.
From the inception of the HTx program to the end of 2023, 146 patients, comprising 139 adults and 7 children, awaited HTx in Kazakhstan. The Akmola, Karaganda, and West Kazakhstan regions had the highest per capita percentages of patients waiting for HTx (6.34, 5.90, and 5.78 pmp, respectively). In the North Kazakhstan region, there were no patients on the waiting list. However, Astana city had the highest percentage of patients waiting for HTx—52.22 pmp—as the majority of HTx procedures are performed there (Fig. 3).
A map illustrating the distribution of patients awaiting heart transplantation across Kazakhstan's regions from the inception of the program to the end of 2023, indicating the number per million population and the total number (in brackets). The map was produced utilizing Quantum Geographic Information System (QGIS) software, Version 3.26 'Buenos Aires'" (https://www.qgis.org/en/site/).
Outcome study
Table 2 shows the characteristics of the HTx donors and recipients. The median age of the donors was 43.0 years, while the median age of the recipients was 41.5 years. Given the policy in Kazakhstan, which prohibits children from being donors, there were no donors below the age of 18, although two recipients fell within that age group. The predominant age category for both donors (42.0%) and recipients (28.6%) was 30–50 years. None of the donors were underweight (defined as having a BMI < 18.5), while 1.8% of the recipients fell into this category. Generally, the median BMI of the donors was greater than that of the recipients (24.2 vs. 23.3). Blood group 0 predominated among donors (35.2%), whereas blood group A was most common among recipients (35.6%). The prevalence of negative RhD was lower among recipients than among donors (4.5% vs. 13.6%).
Survival analysis data were available for 88 of the 92 HTx patients. Table 3 presents the life table with survival and mortality rates for patients who underwent HTx. The 30-day cumulative survival rate was 94%, and the 360-day survival rate was 76%. The 1080-day (3-year) survival rate was 71%, and the 1740-day (5-year) survival rate was 65%. Correspondingly, the 30-day cumulative mortality was 6%, increasing to 24% at 360 days, 29% at 1080 days, and 35% at 1740 days.
The total duration of follow-up for the HTx patients was 4,131 days. The first year after HTx, the survival rate decreased the most rapidly, dropping to 90.9% at 55 days, 85.2% at 110 days, and 77.0% at 379 days. From day 2570 until the end of the follow-up period, the cumulative survival rate remained at 58.1% (Fig. 4).
Cox regression analysis was utilized to evaluate the hazard ratio (HR) of lethal outcomes in HTx patients based on various influencing factors pertaining to both donors and recipients. None of the donor-related factors investigated demonstrated a significant impact on lethal outcomes, as indicated in Table 4. Conversely, recipient-related factors, such as blood levels of creatinine and total bilirubin, were found to significantly influence overall survival (HR 8.979 and 7.972, respectively). Additionally, postoperative risk factors, including the presence of infection or sepsis, as well as the application of ECMO, significantly affected overall survival (HR 9.463 and 3.491, respectively), as shown in Table 5.
Discussion
This study aimed to conduct a comprehensive analysis of the national HTx program in Kazakhstan spanning 12 years (2012–2023). The pmp rates of HTx ranged from 0.06 to 1.08, with no discernible increasing trend. Notably, the pmp rates of LVAD implantations were comparatively greater, fluctuating between 1.60 and 2.78. These rates mirrored the HTx figures, with periods of elevated HTx rates corresponding to decreased LVAD implantation rates. Forecast analysis indicated that without intervention, the expected incidence of HTx will not increase until 2030, despite a rise in the incidence of IHD, a major indication for HTx according to national standards of care. Survival analysis revealed a rapid decrease in the first year after HTx, reaching 77.0% at 379 days, and an overall survival rate of 58.1% at the end of the follow-up period. Among the various factors analyzed, recipient blood levels of creatinine and total bilirubin before surgery, as well as the presence of infection or sepsis and the use of ECMO after surgery, were found to be significant contributors to the survival of HTx patients. A detailed discussion of these findings is warranted.
In general, the pmp rates of HTx in Kazakhstan remained low, comparable to those observed in the Southeast Asian region during 2020–2023, where they equaled 0.2 in 20227. Among former Soviet Union countries, Kazakhstan and Ukraine exhibited similarly low HTx pmp rates (0.2). In contrast, other post-Soviet countries with available data reported higher HTx pmp rates: Belarus (5.6), Lithuania (3.7), Russia (1.7), and Latvia (1.1). Notably, Slovenia, the Czech Republic, and Croatia, which are also former Socialist block members, boasted some of the highest HTx pmp rates (11.4, 6.7, and 6.1, respectively, in 2020)7.
The HTx rate per million people is influenced by multiple factors, including the number of heart transplant centers per million inhabitants. As of the end of 2023, Kazakhstan had four heart transplant centers for a population of 20 million, resulting in an indicator of 0.2. This pmp rate of heart transplant centers in Kazakhstan is among the lowest globally compared to other regions: Eastern Mediterranean (22.1), Western Pacific (11.6), Southeast Asia (9.8), the Americas (2.9), and Europe (4.4). Only the African region exhibited a lower rate, with no registered heart transplant centers in 202216.
However, a key factor contributing to the low HTx pmp rate in Kazakhstan is the high rate of refusals for deceased donations. Among 47 countries reporting refusal rates, Kazakhstan ranks 4th, with a rate approaching 90%7. Families refusing to donate organs to deceased relatives cited various reasons, including denial of brain death, belief in a miracle, and fear of organ trade or unknown organ destinations17, with such fears being particularly pronounced in Kazakhstan. An incident in 2017–2018 involving accusations of Kazakhstani transplant surgeons engaging in the organ trade further heightened these fears, resulting in a lasting negative impact on organ transplantation rates in the country18.
The survival rates observed in this study for HTx patients align with international reports. However, it is important to note that our findings are based on a relatively small patient cohort, limiting the generalizability of our results. In the USA, the 10-year survival rate of HTx recipients who underwent surgery between 1990 and 2007 was reported to be 53%19. Italy reported that the overall survival of HTx patients who underwent surgery between 2012 and 2020 was 81.2% at 1 year and 79.6% at 8 years20. In China, the 1-year survival rate for HTx patients is 90.1%, with a 5-year survival rate of 84.0%21. The Registry of the International Society for Heart and Lung Transplantation reported global 1-year and 5-year survival rates of approximately 85% and 72.5%, respectively22. Global survival after HTx has improved in recent years, attributed to advances in medical care, although rates differ by region, with higher survival in North America than in Europe and other regions, possibly due to higher rates of heart transplantation from older donors23.
Apart from older donor age, various factors influence patient survival post-HTx. A study using data from the Spanish Heart Transplant Registry identified recipient age as a significant factor contributing to overall HTx patient survival24. Older recipient age is associated with multiple comorbidities and poor overall survival, necessitating careful patient selection23. Other risk factors include congenital heart disease (HR 1.65, 95% CI from 1.32 to 2.06), retransplantation (HR 1.50, 95% CI from 1.22 to 1.85), and restrictive cardiomyopathy (HR 1.36, 95% CI from 1.11 to 1.68)22. The diminished survival in these patient categories may be explained by an unfavorable immunological profile and suboptimal technical operative conditions, predisposing patients to early graft failure. In our study, recipient age was insignificant risk factor. Obtaining additional data, which may occur with increased HTx procedures in Kazakhstan, may reveal additional findings.
The incidence of CVD is increasing in Kazakhstan25. Despite efforts to enhance care quality26, there are disparities between regions, with rural populations having a lower CVD identification rate14, contributing to a greater burden of end-stage disease. This study revealed that 146 patients were awaiting HTx in 2023, and 14 others died without receiving it. With only 4 HTx procedures performed in the country during the same period, the rate of receiving HTx was 2.5% (4/160). International studies reported higher rates of patients awaiting HTx who actually received it: 66.7% in the USA27, 50% in the Netherlands28, and 41% in Iran29. It is evident that much needs to be done in Kazakhstan to increase the proportion of patients on the HTx waiting list who receive HTx.
This study has several limitations. The national cohort of HTx patients is relatively small, preventing robust conclusions on HTx survival rates and associated factors. However, data on all patients who underwent HTx in the country from the inception of the HTx program (2012) to the present (2023) were available, allowing meaningful observations on necessary improvements. Another limitation is that the National Registry of Donors and Recipients lacks many specific details related to donors and recipients, thereby limiting the analysis of associated risk factors. Additionally, data on the survival of patients who underwent LVAD implantation were not available, despite an earlier report on this issue8. We utilized the incidence rates of IHD to predict future trends and support the determination of the need to increase the rate of HTx in Kazakhstan. The data on end-stage heart failure were not available to us, and in addition to IHD, other disorders contribute to this condition. Given the many advances in the medical management of IHD30, fewer patients will reach the end stage and require HTx. Nevertheless, our projections show that there is no upward trend of HTx in Kazakhstan, necessitating public health action to improve this situation.
Data availability
The data used and analyzed during the current study are available from the corresponding author upon reasonable request from the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- CVD:
-
Cardiovascular disease
- GODT:
-
Global observatory on donation and transplantation
- HF:
-
Heart failure
- HR:
-
Hazard ratio
- HTx:
-
Heart transplantation
- HVD:
-
Heart valve disease
- IHD:
-
Ischemic heart disease
- LVAD:
-
Left ventricular assist device
- MoH:
-
Ministry of health
- pmp:
-
Per million population
- RhD:
-
Rhesus D antigen
- SPSS:
-
Statistical package for social sciences
- The USSR:
-
The union of the soviet socialist republic
- WHO:
-
World Health Organization
References
Bozkurt, B. et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 23(3), 352–380. https://doi.org/10.1002/ejhf.2115 (2021).
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392(10159), 1789–1858. https://doi.org/10.1016/S0140-6736(18)32279-7 (2018).
Savarese, G. et al. Global burden of heart failure: A comprehensive and updated review of epidemiology. Cardiovasc. Res. 118(17), 3272–3287. https://doi.org/10.1093/cvr/cvac013 (2023).
Masarone, D. et al. The ABC of heart transplantation-part 1: Indication, eligibility, donor selection, and surgical technique. J. Clin. Med. 12(16), 5217. https://doi.org/10.3390/jcm12165217 (2023).
Han, J. J., Acker, M. A. & Atluri, P. Left ventricular assist devices. Circulation 138(24), 2841–2851. https://doi.org/10.1161/CIRCULATIONAHA.118.035566 (2018).
Chambers, D. C. et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult lung and heart-lung transplantation Report-2019; Focus theme: Donor and recipient size match. J. Heart Lung Transpl. 38(10), 1042–1055. https://doi.org/10.1016/j.healun.2019.08.001 (2019).
Global Observatory on Donation and Transplantation. International Report on Organ Donation and Transplantation activities. (2022). https://www.transplant-observatory.org/. Accessed 10 Dec 2023.
Pya, Y. et al. Initial 3-year outcomes with left ventricular assist devices in a country with a nascent heart transplantation program. ESC Heart Fail. 3(1), 26–34. https://doi.org/10.1002/ehf2.12066 (2016).
Holm, A. M. et al. International society for heart and lung transplantation statement on transplant ethics. J. Heart Lung Transplant. 41(10), 1307–1308. https://doi.org/10.1016/j.healun.2022.05.012 (2022).
Order of the Minister of Health of the Republic of Kazakhstan dated December 21, 2020 ҚP ДCM-308/2020. https://adilet.zan.kz/rus/docs/V2000021859. Accessed 2 April 2024.
Order of the Minister of Health of the Republic of Kazakhstan dated November 30, 2020 #KR DSM-226/2020. https://transplant.kz/images/226-30-11-2022rus.pdf. Accessed 9 Dec 2024.
Agency for Strategic Planning and Reforms of the Republic of Kazakhstan. Bureau of National Statistics. Statistical collections. https://stat.gov.kz/. Accessed 2 Dec 2023.
Clinical Protocol for Heart Transplantation. https://diseases.medelement.com/disease/%D1%82%D1%80%D0%B0%D0%BD%D1%81%D0%BF%D0%BB%D0%B0%D0%BD%D1%82%D0%B0%D1%86%D0%B8%D1%8F-%D1%81%D0%B5%D1%80%D0%B4%D1%86%D0%B0-2017/15630. Accessed 10 Dec 2023.
Salidat Kairbekova National Research Center for Health Development. Statistical Yearbooks “Public Health in the Republic of Kazakhstan and Activities of Healthcare Facilities”. http://www.rcrz.kz/index.php/ru/statistika-zdravookhraneniya-2. Accessed 12 Dec 2023.
Glushkova, N. et al. Examining disparities in cardiovascular disease prevention strategies and incidence rates between urban and rural populations: Insights from Kazakhstan. Sci. Rep. 13(1), 20917. https://doi.org/10.1038/s41598-023-47899-8 (2023).
Global Observatory on Donation and Transplantation. Global Report on Organ Donation and Transplantation 2020. https://www.transplant-observatory.org/wp-content/uploads/2022/07/2020-Global-report-para-web. Accessed 12 Dec 2023.
Ghorbani, F. et al. Causes of family refusal for organ donation. Transplant. Proc. 43(2), 405–406. https://doi.org/10.1016/j.transproceed.2011.01.031 (2011).
Sputnik Kazakhstan. Thousands of Patients are Doomed: Organ Transplant Operations have been Reduced in Kazakhstan. (2019). https://ru.sputnik.kz/20191221/transplantatsiya-kazakhstan-prekraschenie-12345885.html. Accessed 12 Dec 2023.
Suarez-Pierre, A. et al. Long-term survival after heart transplantation: A population-based nested case-control study. Ann. Thorac. Surg. 111(3), 889–898. https://doi.org/10.1016/j.athoracsur.2020.05.163 (2021).
Bifulco, O. et al. Marginal versus standard donors in heart transplantation: Proper selection means heart transplant benefit. J. Clin. Med. 11(9), 2665. https://doi.org/10.3390/jcm11092665 (2022).
Sun, Y. F. et al. Current status of and O2inions on heart transplantation in China. Curr. Med. Sci. 41(5), 841–846. https://doi.org/10.1007/s11596-021-2444-9 (2021).
Lund, L. H. et al. The registry of the international society for heart and lung transplantation: Thirty-third adult heart transplantation report-2016; focus theme: Primary diagnostic indications for transplant. J. Heart Lung Transplant. 35(10), 1158–1169. https://doi.org/10.1016/j.healun.2016.08.017 (2016).
Khush, K. K. et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: Thirty-eighth adult heart transplantation report-2021; Focus on recipient characteristics. J. Heart Lung Transplant. 40(10), 1035–1049. https://doi.org/10.1016/j.healun.2021.07.015 (2021).
López-Vilella, R. et al. Impact of donor-recipient age on cardiac transplant survival: Subanalysis of the Spanish Heart Transplant Registry. Rev. Espanol. Cardiol. 74(5), 393–401. https://doi.org/10.1016/j.rec.2020.02.016 (2021).
Mukasheva, G. et al. Incidence and mortality of cardiovascular disease in the Republic of Kazakhstan: 2004–2017. Iran J. Public Health. 51(4), 821–830. https://doi.org/10.18502/ijph.v51i4.9243 (2022).
Adilet. The MoH Order Approving the Regulations for Hospitals and Clinics that Provide Cardiac, Interventional Cardiac, and Cardiac Surgical Treatment. https://adilet.zan.kz/rus/docs/V2300032010#z29. Accessed 13 Dec 2023.
US Department of Health and Human Services. Scientific Registry of Transplant Recipients. OPTN/SRTR 2021 Annual Data Report: Heart. https://srtr.transplant.hrsa.gov/annual_reports/2021/Heart.aspx. Accessed 13 Dec 2023.
Roest, S. et al. Waiting list mortality and the potential of donation after circulatory death heart transplantations in the Netherlands. Netherlands Heart J. 29(2), 88–97. https://doi.org/10.1007/s12471-020-01505-y (2021).
Amin, A. et al. Outcome of heart transplant candidates based on a high volume heart transplant center experience in Iran. Int. J. Organ Transplant. Med. 13(2), 17–25 (2022).
Virani, S. S. et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: A report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 148(9), e9–e119. https://doi.org/10.1161/CIR.0000000000001168 (2023).
Funding
This research was funded by the Committee of Science of the Ministry of Science and Higher Education of the Republic of Kazakhstan (Grant title: Noninvasive methods for the diagnosis of transplant rejection as a predictor of long-term graft survival, Grant No. BR21882206).
Author information
Authors and Affiliations
Contributions
Study conception and design: Y.S. Acquisition of data: A.B., S.S. Analysis and interpretation of data: A.A., A.S., S.N. Drafting of the work: Y.S., Y.P. Critical Revision of the manuscript: All authors. Statistical analysis: Y.S., G.M. Study supervision: Y.P. Final approval of the manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Semenova, Y., Shaisultanova, S., Beyembetova, A. et al. Examining a 12-year experience within Kazakhstan’s national heart transplantation program. Sci Rep 14, 10291 (2024). https://doi.org/10.1038/s41598-024-61131-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61131-1
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.