Abstract
Recently, patients with out-of-hospital cardiac arrest (OHCA) refractory to conventional resuscitation have started undergoing extracorporeal cardiopulmonary resuscitation (ECPR). However, the mortality rate of these patients remains high. This study aimed to clarify whether a center ECPR volume was associated with the survival rates of adult patients with OHCA resuscitated using ECPR. This was a secondary analysis of a retrospective multicenter registry study, the SAVE-J II study, involving 36 participating institutions in Japan. Centers were divided into three groups according to the tertiles of the annual average number of patients undergoing ECPR: high-volume (≥ 21 sessions per year), medium-volume (11–20 sessions per year), or low-volume (< 11 sessions per year). The primary outcome was survival rate at the time of discharge. Patient characteristics and outcomes were compared among the three groups. Moreover, a multivariable-adjusted logistic regression model was applied to study the impact of center ECPR volume. A total of 1740 patients were included in this study. The center ECPR volume was strongly associated with survival rate at the time of discharge; furthermore, survival rate was best in high-volume compared with medium- and low-volume centers (33.4%, 24.1%, and 26.8%, respectively; P = 0.001). After adjusting for patient characteristics, undergoing ECPR at high-volume centers was associated with an increased likelihood of survival compared to middle- (adjusted odds ratio 0.657; P = 0.003) and low-volume centers (adjusted odds ratio 0.983; P = 0.006). The annual number of ECPR sessions was associated with favorable survival rates and lower complication rates of the ECPR procedure.
Clinical trial registration: https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000041577 (unique identifier: UMIN000036490).
Similar content being viewed by others
Introduction
The number of patients experiencing out-of-hospital cardiac arrest (OHCA) is increasing1,2,3. Patients with OHCA who are refractory to conventional resuscitation have recently started undergoing extracorporeal cardiopulmonary resuscitation (ECPR), with previous studies showing that ECPR decreases in-hospital mortality compared with conventional resuscitation4,5.
Management of mechanical devices, including extracorporeal membrane oxygenation (ECMO), has a high complication rate6,7 and requires specialized knowledge and skills for effective and safe management. However, despite the difficulties of ECPR and post-resuscitation management with ECMO, there are no widely used guidelines for ECPR and ECMO management. Therefore, physicians administering ECPR must be proficient in ECMO circuit management and post-resuscitation care, and well trained in veno-arterial cannulation to prevent complications. Considerable experience and learning curves are required to improve ECPR management skills and may be related to the annual ECPR cases number performed at each hospital. Nonetheless, the association between annual center volume with in-hospital mortality in adult patients with OHCA resuscitated using ECPR has not been clarified. Therefore, this study aimed to investigate the effect of center ECPR volume on outcomes in patients with OHCA who underwent ECPR.
Materials and methods
Study design and cohort
To examine whether center ECPR volume was associated with survival rate at the time of discharge in patients with OHCA who underwent ECPR, we used a dataset from the SAVE-J II study cohort. The study design has been described in detail elsewhere8,9. In brief, this cohort derived from a retrospective multicenter study in Japan that included 36 university and community hospitals and enrolled 2,157 consecutive patients with OHCA aged ≥ 18 years who were resuscitated using ECPR between January 1, 2013, and December 31, 2018. In the SAVE-J II study, ECPR was defined as resuscitation with veno-arterial ECMO in patients with refractory cardiac arrest. Due to the retrospective design of this study, the implementation of ECPR lacked specific criteria and was depended on the judgement of each institution.
This study named Study of Advanced Cardiac Life Support for Ventricular Fibrillation with Extracorporeal Circulation in Japan was retrospectively approved by the Institutional Ethics Committee of Kagawa University (approval number: 2018-110, approved date: 15 April 2019) and that of each participating institution. This secondary analysis of de-identified data was approved by the Institutional Review Board of the Saiseikai Utsunomiya Hospital (approval number: 2023-06). The requirement for informed consent was waived by the ethics committee due to the retrospective nature of the study. This study was performed in accordance with the 1975 Declaration of Helsinki Guidelines for Clinical Research Protocols.
Study population
From all the patients in the SAVE-J II registry, the present study excluded those who did not meet the ECPR criteria, such as those who withdrew after cannulation and before turning the ECMO pump on due to the return of spontaneous circulation (ROSC), those who received ECPR after intensive care unit admission, those who achieved ROSC before cannulation, and those who were transferred to the participating institutions from another hospital, as it precluded the definition of center volume. We divided the remaining patients into three groups according to the tertile of center ECPR volume. As a result, three groups were defined as follows: (1) high-volume centers (HVC) (≥ 21 ECPR sessions/year), (2) medium-volume centers (MVC) (11–20 sessions/year), and (3) low-volume centers (LVC) (< 11 sessions/year). For adequate background comparison, we further excluded patients with non-cardiac conditions, including acute aortic syndrome/aortic aneurysm, hypothermia, primary cerebral disorder, infection, drug intoxication, trauma, suffocation, drowning, and other external causes, and patients with missing outcome data. Missing data were not replaced or estimated.
Outcome measurements
The primary endpoint of this study was survival rate at the time of discharge, and the secondary endpoints were the proportion of complications during ECPR cannulation and ECMO management and favorable neurological outcomes at the time of discharge. The complications of ECPR cannulation included malpositioning of the cannula, unsuccessful cannulation, and cannulation-related bleeding. Cannula malposition was defined as cannulation requiring correct positioning or cannulation of the wrong vessel, such as arterial-arterial or veno-veno cannulation. Unsuccessful cannulation was defined as a failure to complete cannulation. Cannulation-related bleeding included cannulation site bleeding and retroperitoneal hemorrhage requiring blood transfusion or surgical intervention/interventional radiology, and other forms of hemorrhage included intracerebral hemorrhage confirmed on computed tomography (CT), mediastinal hemorrhage, intra-abdominal organ hemorrhage, and gastrointestinal hemorrhage requiring blood transfusion or surgical and radiological intervention. Complications during ECMO management included hemorrhage, ischemia, and ECMO equipment problems. The Cerebral Performance Categories (CPC) scale was used to classify the neurological outcomes as follows: CPC 1, full recovery; CPC 2, moderate disability; CPC 3, severe disability; CPC 4, coma or vegetative state; and CPC 5, death. CPCs 1–2 were considered favorable outcomes, and CPCs 3–5 represented unfavorable outcomes10.
Statistical analysis
Continuous variables were expressed as medians with interquartile ranges. Categorical variables were expressed as numbers and percentages. Patient characteristics and outcomes were evaluated among the three groups using the Kruskal–Wallis test for continuous variables and the chi-square or Fisher’s exact test for dichotomous variables. Multivariate analysis to identify predictors of in-hospital mortality was performed using linear regression of clinically important variables clustered by ECPR center volume, such as age, gender, incidence of witnessed cardiac arrest, bystander cardiopulmonary resuscitation (CPR), and initial cardiac rhythm at the scene. Moreover, a multivariable-adjusted logistic regression model was applied to study the impact of center ECPR volume by using age, gender, incidence of witnessed cardiac arrest, bystander cardiopulmonary resuscitation (CPR), initial cardiac rhythm and as confound factors. Regression models were allied with adjusted odds ratios (AOR) and with 95% confidence intervals (CI). Differences were considered statistically significant for two-tailed P-values < 0.05. All analyses were performed using the R software (version 4.2.1; R Foundation for Statistical Computing, Vienna, Austria).
Results
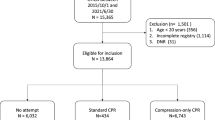
Of the 2157 adult patients with OHCA in the SAVE-J II cohort, 2,084 were finally enrolled to assess the influence of center ECMO volume. The patients were divided into three groups according to the tertiles of center ECPR volume: 766 (36.8%) patients from 5 HVCs, 614 (29.5%) from 7 MVCs, and 704 (33.8%) from 24 LVCs (see Additional Fig. 1 in Additional file 1). After excluding patietns with cardiopulmonary arrest caused by non-cardiac conditions or external causes and missing outcome data, 1740 patients were finally analyzed (Fig. 1). The comparison of the baseline patient characteristics between the three ECPR center volumes is shown in Table 1. On average, the median age of the patients was 60 years old, and the proportion of male patients was 83.9%. Although the groups showed no significant difference in the time from onset to hospital arrival, the time from hospital arrival to ECMO was shorter in the HVC group. Outcomes are shown in Table 2. The center ECPR volume was strongly associated with survival rate at the time of discharge and was the higher in HVC compared with those at MVC and LVC: 33.4%, 24.1%, and 26.8%, respectively (P = 0.001). The proportion of total ECMO complications was significantly lower in HVC (27.8%) than in MVC (37.6%) and LVC (34.8%; P = 0.010). Moreover, multivariate analysis was used to account for variations in the background characteristics of the patients and the center ECPR volume (Table 3). After adjusting for the patient characteristics, undergoing ECPR at HVCs was associated with increased likelihood of survival compared with MVC (AOR 0.657; 95% CI 0.500–0.863, P = 0.003) and LVC (AOR 0.983; 95% CI 0.541–0.901, P = 0.006). Furthermore, it was also significantly associated with ECMO complications compared with LVCs (AOR, 1.410; 95% CI 1.100–1.800, P = 0.006), while not being associated with neurological outcomes (Fig. 2).
Flowchart of study participants enrollment. ECPR extracorporeal cardiopulmonary resuscitation, ECMO extracorporeal membrane oxygenation, VA-ECMO veno-arterial ECMO, ICU intensive care unit, ROSC return of spontaneous circulation, HVC high-volume center, MVC medium-volume center, LVC low-volume center.
Discussion
This study investigated the association between the center volume, survival rate, and other outcomes in patients with OHCA who underwent ECPR. Hospitals with the highest annual volume of ECPR had significantly higher survival rates at discharge and lower complication rates during ECPR and ECMO management.
The association between mortality and center ECPR volume has been previously evaluated in limited cohort. Tonna et al. indicated that the hospital-level ECPR annual case volume was associated with in-hospital survival11. However, that study only showed that center ECPR volume was one of the factors associated with in-hospital mortality, and detailed information related to the difference in the annual number of patients receiving ECPR was not described. Moreover, although Watanabe et al. mentioned the center ECMO volume in their study, they did not examine the association between center ECMO volume and outcomes12. Therefore, our study is the first to investigate the relationship between patient background, prognosis, multiple complications, detailed multiple complication and ECPR center volume based on the annual number of ECPR cases. In this study, we used tertiles to define the ECPR central volume, as there is no standard for defining the ECPR central volume. However, the number of each ECMO center volume was not so different from these previous studies11,12.
On the other hand, this study had a higher proportion of the patients with non-shockable rhythm than other studies. Although some typical patients groups who can gain the better clinical outcome from ECPR are well known and previous studies had chosen these patients in the prospective studies5,13, in the real clinical practice, ECPR is widely performed by the physicians judgments such as the patients that initial waveform was pulseless electrical activity(PEA) due to the pulmonary embolism or in patients without the shockable rhythm who are judged as treatable due to hypothermia14,15. In fact, the main article of SAVE-J II study showed that 9.2% of the patients with initial waveform PEA and 3.9% of patients with asystole had favorable neurological outcomes8. Therefore, this study was a retrospective observational study, and I guess this is a real world data.
The results of this study have several possible explanations. First, the HVC group had a significantly shorter time from hospital arrival to ECMO initiation. Based on this, it is expected that a HVC may decide to start ECPR earlier or that the time from ECPR start to pumping is shorter due to a more extensive experiences with ECPR. Second, although some studies have recently shown that ECPR decreased mortality in patients with OHCA who are refractory to conventional resuscitation the mortality rate in patients with OHCA who have undergone ECPR remains high16,17. This is not only due to the severity of the patient’s background but also the high complication rates during ECPR and ECMO management6,18. A previous meta-analysis has reported that mechanical cardiac devices tend to cause severe or life-threatening bleeding and peripheral vascular complications6,19. It also showed that fewer complications lead to decreased mortality in patients with veno-arterial ECMO20. Therefore, appropriate management of mechanical devices is required to both reduce avoidable complications and deal with them adequately if they occur. Furthermore, in other complex or specialized procedures, such as cardiovascular surgery or organ transplantation, patient outcomes have been reported to be largely dependent on center volume21,22,23. Therefore, institutions with a high annual number of ECPR cases can increase and maintain their management skills, which may lead to higher survival and lower complication rates. Here, it is also necessary to mention the impact of hospital size on this result or the proportion of the ECPR from all cardiac arrest patients at each hospital. However, as this study only enrolled patients who underwent ECPR, it is impossible to show a relationship between hospital capacities and ECPR center volume. Therefore, it remains unclear whether the hospital with higher number of ECPR annual cases lead to better clinical outcomes due to the availability of hospital resources for treatment, or whether even relatively small hospitals with a high number of ECPR cases can achieve sufficient outcomes. As such, further studies in this point are warranted.
However, if patients with OHCA are consolidated into an HVC, it might prolong the time from onset to ECMO and reduce flow time. The combination of expeditious coronary angiography and admission to an invasive heart center has been demonstrated to improve survival in patients with OHCA24, and another study showed that hospital survival is more strongly associated with post-resuscitation care than with acute resuscitation skills in the emergency room25. Accordingly, transportation to high-volume ECMO centers after the prompt introduction of ECPR at prehospital care or regional hospitals may lead to improved survival rates. Future studies are needed to examine how to balance expeditious arrest-to-cannulation times and the consolidation of ECPR.
Limitations
This study has some limitations. First, as this was a retrospective observational study, the inclusion criteria were not defined and the indications for performing ECPR, including patient selection and timing of ECMO insertion, varied by physiatrist and institution. Therefore, selection bias is inevitable and there might be some variation in the selection of patients undergoing ECPR between institutions. However, the survival rate of the patients undergoing ECPR in this study did not differ much compared to previous retrospective and prospective ECPR registries5,26. Nevertheless, this point should be acknowledged. Second, we used a Japanese cohort, and the Japanese emergency medical system and ECPR methods were different from those of American and European countries in terms of the transfer protocol, including the timing of drug administration, and facility standards for ECPR. Hence, further investigations with prospective large international cohorts are required.
Conclusions
We showed that patients with OHCA undergoing ECPR at HVCs have significantly higher survival rates than those undergoing the procedure at MVCs and LVCs, and that HVCs had a lower proportion of complications than LVCs.
Data availability
The dataset supporting the conclusions of this study is available from the corresponding author on reasonable request. The data are not publicly available because of privacy and ethical restrictions.
Abbreviations
- AOR:
-
Adjusted odds ratios
- CI:
-
Confidence interval
- CPC:
-
Cerebral performance categories
- CPR:
-
Cardiopulmonary resuscitation
- CT:
-
Computed tomography
- ECMO:
-
Extracorporeal membrane oxygenation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- HVC:
-
High-volume centers
- LVC:
-
Low-volume centers
- MVC:
-
Medium-volume centers
- OHCA:
-
Out-of-hospital cardiac arrest
- PEA:
-
Pulseless electrical activity
- ROSC:
-
Return of spontaneous circulation
References
Berdowski, J. et al. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 81, 1479–1487 (2010).
Sondergaard, K. B. et al. Bystander cardiopulmonary resuscitation and long-term outcomes in out-of-hospital cardiac arrest according to location of arrest. Eur. Heart J. 40, 309–318 (2019).
Virani, S. S. et al. Heart disease and stroke statistics-2020 update: A report from the American heart association. Circulation 141, e139–e596 (2020).
Ortega-Deballon, I. et al. Extracorporeal resuscitation for refractory out-of-hospital cardiac arrest in adults: A systematic review of international practices and outcomes. Resuscitation 101, 12–20 (2016).
Yannopoulos, D. et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. Lancet 396, 1807–1816 (2020).
Amin, A. P. et al. The evolving landscape of impella use in the united states among patients undergoing percutaneous coronary intervention with mechanical circulatory support. Circulation 141, 273–284 (2020).
Miller, P. E. et al. Clinical outcomes and cost associated with an intravascular microaxial left ventricular assist device vs intra-aortic balloon pump in patients presenting with acute myocardial infarction complicated by cardiogenic shock. JAMA Intern Med 182, 926–933 (2022).
Inoue, A. et al. Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: a retrospective large cohort multicenter study in Japan. Crit Care 26, 129 (2022).
Shibahashi, K. et al. Comparison of sedation using propofol versus midazolam in patients admitted to the intensive care unit after extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: a multicentre observational study. Eur. Heart J. Acute Cardiovasc. Care 12, 246–256 (2023).
Ajam, K. et al. Reliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: A cohort study. Scand. J. Trauma Resusc. Emerg. Med. 19, 38 (2011).
Tonna, J. E. et al. The association of modifiable postresuscitation management and annual case volume with survival after extracorporeal cardiopulmonary resuscitation. Crit. Care Explor. 4, e0733 (2022).
Watanabe, M. et al. The impact of different targeted temperatures on out-of-hospital cardiac arrest outcomes in patients receiving extracorporeal membrane oxygenation: A nationwide cohort study. Crit. Care 26, 380 (2022).
Suverein, M. M. et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N. Engl. J. Med. 388, 299–309 (2023).
Carroll, B. J. et al. Percutaneous management of high-risk pulmonary embolism. Circ. Cardiovasc. Interv. 16, e012166 (2023).
Ledoux, A. & Saint Leger, P. Therapeutic management of severe hypothermia with veno-arterial ECMO: Where do we stand? Case report and review of the current literature. Scand. J. Trauma Resusc. Emerg. Med. 28, 30 (2020).
Belohlavek, J. et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA 327, 737–747 (2022).
Halter, M. et al. Association between hyperoxemia and mortality in patients treated by eCPR after out-of-hospital cardiac arrest. Am. J. Emerg. Med. 38, 900–905 (2020).
Leick, J. et al. Door-to-implantation time of extracorporeal life support systems predicts mortality in patients with out-of-hospital cardiac arrest. Clin. Res. Cardiol. 102, 661–669 (2013).
Kim, Y. et al. Outcomes of mechanical circulatory support for acute myocardial infarction complicated by cardiogenic shock. Catheter. Cardiovasc. Interv. 99, 658–663 (2022).
Tanaka, D. et al. The impact of vascular complications on survival of patients on venoarterial extracorporeal membrane oxygenation. Ann. Thorac. Surg. 101, 1729–1734 (2016).
Dobaria, V. et al. Impact of center volume on outcomes of surgical repair for type A acute aortic dissections. Surgery 168, 185–192 (2020).
Chen, C. W. et al. Transplant volume is associated with graft acceptance threshold and center resource availability. J. Card. Fail. 26, 522–526 (2020).
Kopp, W. et al. Center volume is associated with outcome after pancreas transplantation within the eurotransplant region. Transplantation 101, 1247–1253 (2017).
Tranberg, T. et al. Distance to invasive heart centre, performance of acute coronary angiography, and angioplasty and associated outcome in out-of-hospital cardiac arrest: A nationwide study. Eur. Heart J. 38, 1645–1652 (2017).
Girotra, S. et al. Association of hospital-level acute resuscitation and postresuscitation survival with overall risk-standardized survival to discharge for in-hospital cardiac arrest. JAMA Netw. Open 3, e2010403 (2020).
Bougouin, W. et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: A registry study. Eur. Heart J. 14, 21 (2020).
Funding
This work was supported by Japan Society for the Promotion of Science (JSPS) KAKENHI (Grant‑in‑Aid for Scientific Research [C]) Grant Number JP19K09419.
Author information
Authors and Affiliations
Consortia
Contributions
Authors KM and TO were involved in the conception and design. KM wrote the main manuscript text and prepared figures. All authors were involved the drafting of the paper, reviewing it critically for intellectual content; and the final approval of the version to be published. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Misumi, K., Hagiwara, Y., Kimura, T. et al. Impact of center volume on in-hospital mortality in adult patients with out‑of‑hospital cardiac arrest resuscitated using extracorporeal cardiopulmonary resuscitation: a secondary analysis of the SAVE-J II study. Sci Rep 14, 8309 (2024). https://doi.org/10.1038/s41598-024-58808-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-58808-y
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.