Abstract
Smoking has multiple detrimental effects on health, and is a major preventable cause of premature death and chronic disease. Despite the well-described effect of inhaled substances from tobacco smoke on cell toxicity, the association between smoking and suicidal erythrocyte death, termed eryptosis, is virtually unknown. Therefore, the blood samples of 2023 participants of the German National Cohort Study (NAKO) were analyzed using flow cytometry analysis to determine eryptosis from fluorescent annexin V-FITC-binding to phosphatidylserine-exposing erythrocytes. Blood analyses were complemented by the measurement of hematologic parameters including red blood cell count, hematocrit, hemoglobin, mean corpuscular cell volume (MCV) and mean corpuscular hemoglobin (MCH). Eryptosis was higher in smokers than in non- and ex-smokers, and positively associated with the number of cigarettes smoked daily (r = 0.08, 95% CI [0.03, 0.12]). Interestingly, despite increased eryptosis, smokers had higher red blood cell indices than non-smokers. To conclude, smokers were characterized by higher eryptosis than non-smokers, without showing any obvious detrimental effect on classic hematological parameters.
Similar content being viewed by others
Introduction
Smoking is a well-described risk factor for disease and a major preventable cause of premature death and chronic diseases worldwide1. In particular, it negatively impacts the vasculature and induces impairment of microcirculation2. Inhaled tobacco smoke comprises substances such as carbon monoxide (CO), formaldehyde, acetaldehyde, benzopyrenes, and nicotine which can enter the circulation3,4. Most of these substances are toxic and can cause tissue damage by inducing oxidative stress and inflammation5,6,7. In addition, CO binds to hemoglobin to form carboxyhemoglobin which reduces oxygen-carrying capacity and oxygen utilization8. Although smoking has cytotoxic and hypoxic effects, there is comparatively limited data on the relationship between smoking and the red blood cell system. Interestingly, a few observational studies found tobacco smoking associated with higher red blood cell indices such as red blood cell count, hematocrit, hemoglobin, and mean corpuscular volume (MCV)9,10. On the other hand, in vitro data indicate that smoking causes erythrocyte death. It was shown that treatment of red blood cells with cigarette smoke extract or CO can induce eryptosis11,12, a certain form of programmed cell death that is similar to classical apoptosis in numerous aspects13. Increased eryptosis was also observed in a small study comparing 21 healthy male smokers with 21 non-smokers14. Hallmarks of eryptosis are phosphatidylserine externalization13, which can be assessed by measuring the binding of fluorescent annexin V-FITC in flow cytometry analysis, and cell shrinkage15. Excessive eryptosis can cause anemia but also the derangement of microcirculation by adhesion of phosphatidylserine-exposing erythrocytes to endothelial cells16,17. Based on the findings of several observational studies indicating an association between smoking and increased red blood cell indices with other data, primarily obtained from in vitro experiments, observing eryptosis and shrinkage of erythrocytes, the current study aimed to investigate whether smoking and smoking habits are linked to significant changes in eryptosis in a large population-based cohort. Additionally, in the case of increased eryptosis, the study aimed to assess whether eryptosis is associated with anemia-like conditions or if it is linked to elevated red blood cell indices, which are observed in other cohorts.
Methods
Population and study design
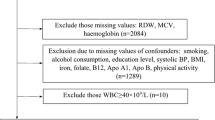
Blood samples from 2023 participants of the German National Cohort Study (NAKO) in the study center of Halle (Saale) were analyzed. The study design of the NAKO was described in detail elsewhere18,19,20,21, and the characteristics of the participants included in the current study were published previously 22. In brief, NAKO includes more than 205,000 adult participants across 18 study centers in different German states. The data collection and processing procedures are standardized and underlie extensive quality control protocols20.
Ethics statement
The current study was approved by the ethical review committee of the study center at MLU Halle-Wittenberg (L3 Project: Processing number: 2013–22) and was conducted in accordance with the Declaration of Helsinki.
Recruitment and data collection
Recruitment and data collection processes were described in detail elsewhere22. In brief, participants of this study were recruited during the regular first follow-up of NAKO participants from 04/10/2019 to 11/04/2021. During the informed consent process for NAKO, participants were asked if they were willing to participate in our subproject, and an additional 3 ml serum tube was collected. Out of a total of 3190 NAKO study participants examined during the study period an additional blood sample was obtained from 2174 individuals. Blood samples were collected from Monday to Thursday in the Halle study center and transferred to the Institute of Agricultural and Nutritional Sciences, where the blood samples were analyzed for eryptosis. Hematological parameters (erythrocyte count, hematocrit, hemoglobin, MCV, mean corpuscular hemoglobin concentration (MCH), and mean corpuscular hemoglobin concentration (MCHC)) were measured by the Central Laboratory of the University Hospital Halle (Saale).
Analytical methods
Flow cytometry analysis of annexin V-FITC-binding
Eryptosis was analyzed in fresh blood samples (maximum 24 h old) of the study participants by assessing phosphatidylserine exposure of erythrocytes as published elsewhere22. Phosphatidylserine exposure was measured by determining erythrocyte annexin V-FITC-binding serving as a proxy measure for eryptosis. In brief, 5 µl blood was added to 200 µl Ringer solution (pH 7.4; containing 125 NaCl mM, 5 mM KCl, 1 mM MgSO4, 32 mM HEPES, 5 mM glucose, and 1 mM CaCl2) to isolate the red blood cells. After centrifugation at 1800 g for 5 min, the supernatant was removed, and the washing step was repeated twice. Annexin V-FITC (BD Biosciences, Franklin Lakes, NJ, USA) was used at a 1:500 dilution to stain the erythrocytes resuspended in 250 µl of annexin V-FITC buffer (Ringer solution with 5 mM CaCl2) for 20 min at room temperature under protection from light. Ten µl of these samples were analyzed by flow cytometry (Cytoflex, Beckman Coulter, Brea, CA, USA) in duplicate. Annexin V-FITC-fluorescence intensity was determined at an excitation wavelength of 488 nm and an emission wavelength of 530 nm. Eryptosis (%) expresses the percentage of annexin V-FITC-binding cells of the gated erythrocyte population.
Measurement of hematological parameters
Erythrocyte count, hematocrit, hemoglobin, MCV, MCH, and MCHC were measured in the Central Laboratory of the University Hospital Halle (Saale) from whole blood samples on a Sysmex XN-9000 hematological analyzer. All analyses on the Sysmex XN-9000 analyzer were carried out according to the manufacturer’s instructions and manuals, with routine maintenance and internal as well as external quality control procedures.
Statistical analysis
All data analyses were performed with the R programming language for statistical computing23. Statistical models were implemented in the brms package24 as an interface to the probabilistic programming language Stan25 for gold-standard Bayesian inference. All analyses relied on weakly informative priors since the exploratory nature of this study implies a lack of prior information. All analyses used four MCMC chains, each with 1000 warmup samples, followed by 2000 draws from the posterior distribution. Each model was checked with appropriate diagnostics25. Unless specified otherwise, all results were reported as Bayesian posterior means with 95% credible intervals (CI). Mean comparisons used models without equal variance assumption, i.e., modeling separate variances per group. Throughout the manuscript, r denotes the Pearson correlation coefficient and d denotes Cohen’s effect size measure for mean comparisons. The data pre-processing protocol encompassed the removal of invalid blood samples (as described in22) and extreme eryptosis values (median ± 3 inter-quartile range on the log scale), resulting in a total sample size of n = 2023.
Consent to participate
Written informed consent was obtained from all participants.
Results
Characteristics of the study participants
For the sample of 2023 subjects (970 male, 1053 female) included in our analysis, basic characteristics and hematological parameters are depicted in Table 1. Among the participants, 1000 subjects identified themselves as non-smokers (defined as persons who have never smoked during their lifetime), 418 as smokers, and 605 as ex-smokers.
Correlation between smoking behavior and eryptosis
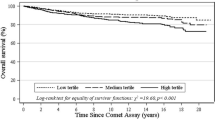
Group comparisons revealed that smokers showed moderately higher eryptosis as assessed from the percentage of phosphatidylserine-exposing erythrocytes than non-smokers and ex-smokers (Fig. 1), with posterior means [95% CI] as follows: non-smokers 0.95% [0.91%, 0.99%], ex-smokers 0.91% [0.86%, 0.96%], and smokers 1.08% [1.01%, 1.15%]. Specifically, smokers had a 14% higher percentage of eryptotic cells eryptosis than non-smokers (Cohen’s d = 0.19 [0.07, 0.31]), and a 19% higher percentage than ex-smokers (Cohen’s d = 0.22 [0.10, 0.35]). The percentage of eryptotic erythrocytes did not differ between ex-smokers and non-smokers (Cohen’s d = 0.05 [− 0.06, 0.14]).
Further analysis yielded a positive association between the number of cigarettes smoked daily and eryptosis rate (r = 0.08 [0.03, 0.12], Fig. 2a). Subgroup analysis of male (r = 0.07 [0.01, 0.14], Fig. 2b) and female subjects (r = 0.08 [0.02, 0.14], Fig. 2c) revealed a similar relationship between the numbers of cigarettes smoked daily and eryptosis in both sexes.
Correlation of eryptosis and the number of cigarettes per day in the total subcohort (n = 2013; a), and grouped by sex (b: 962 males; c: 1051 females). Lines indicate linear regression, and the blue ribbon around the regression line shows the uncertainty as 95% CI. The figure was created using R programming language.
As depicted in Fig. 3, the number of pack years, a cumulative exposure indicator of smoking burden, was not correlated with eryptosis in the total cohort (r = 0.02 [− 0.03, 0.06]; Fig. 3a) as well as in males (r = 0.01 [− 0.06, 0.07]; Fig. 3b) and females (r = 0.04 [− 0.02, 0.10]; Fig. 3c).
Next, we investigated whether the period of abstinence among ex-smokers showed an association with eryptosis. As a result, we found a negative association between the period of abstinence and eryptosis in ex-smokers (r = − 0.13 [− 0.20, − 0.05]). Since longer smoking cessation was associated with lower eryptosis, we hypothesized that the age of smoking cessation might also influence eryptosis. Indeed, the age at which smoking had been stopped was an additional predictive factor for eryptosis (difference of expected log-predictive density ELPD = 2.9 with a standard error of SE = 2.4). This means that both factors, the age at which the subject stopped smoking and the time having passed since smoking cessation, are important prediction factors associated with eryptosis in ex-smokers.
Hematological parameters
In addition, we investigated the relation of eryptosis and hematological parameters. As demonstrated in Fig. 4, eryptosis showed no association with erythrocyte count, hemoglobin, hematocrit, or MCV (Fig. 4a–d), while MCH and MCHC displayed a moderate positive correlation with eryptosis (Fig. 4e–f).
Correlation of eryptosis and hematological parameters of the total subcohort (cf. Table 1 for sample sizes of a–f). Lines indicate linear regression, and the blue ribbon around the regression line shows the uncertainty as 95% CI. The figure was created using R programming language. Tpt Teraparticle, MCV Mean corpuscular volume, MCH Mean corpuscular hemoglobin, MCHC Mean corpuscular hemoglobin concentration.
Table 2 shows the hematological parameters for current smokers, ex-smokers and non-smokers. Erythrocyte count and hematocrit did not differ between the three groups. In contrast, smokers exhibited higher values of hemoglobin, MCV, MCH, and MCHC than ex-smokers and non-smokers. As demonstrated in Table 3, there was no correlation between erythrocyte count and the number of cigarettes smoked per day, smoking duration and pack years within the group of current smokers. However, these parameters were moderately positively correlated with hematocrit, hemoglobin, MCV, and MCH, and negatively correlated with MCHC (Table 3).
Discussion
Our study shows that in a large population-based cohort smokers exhibited moderately higher erythrocyte phosphatidylserine exposure than non-smokers and that the number of cigarettes smoked daily was positively correlated with this hallmark of eryptosis. Additionally, we demonstrated that the time of tobacco abstinence was associated with lower eryptosis with the age of smoking cessation having decisive impact.
The manifold detrimental effects of smoking are well characterized. The cardiovascular system is particularly affected26 as smoking induces vascular damage and may impair microcirculation2,26, conditions predisposing to myocardial infarction27 and stroke28,29. Since eryptotic red blood cells may adhere to vascular walls due to the interaction of phosphatidylserine on the erythrocyte surface with respective receptors on endothelial cells30, enhanced eryptosis may similarly compromize microcirculation31. The effect of smoking on eryptosis was, however, only moderate, and our study did not assess the contribution of eryptosis to an exacerbation of vascular pathologies. However, this contribution appears to be plausible.
Our study did not address the mechanism by which smoking triggers the cellular machinery ultimately resulting in eryptosis. Previous studies reported different mechanisms that may be effective: A pro-oxidative and pro-inflammatory milieu characterized by higher CRP levels and ROS formation, and reduced ROS scavenging capacity apparent from reduced erythrocyte glutathione levels may play a role14. Moreover, smokers are exposed to CO which has been demonstrated to directly stimulate eryptosis in vitro11. Finally, p38MAPK/Fas signaling has been shown to increase eryptosis in smokers12. Thus, it appears to be likely that these factors also account for higher eryptosis in stronger smokers observed in our study. However, other factors may also have an impact since the aforementioned ones may not fully clarify why quitting smoking earlier or for a longer period of time was linked to a reduction of eryptosis. It is tempting to speculate that general changes in lifestyle of individuals who quit smoking are in addition responsible for the observed effects.
An increased number of eryptotic red blood cells in smokers could in theory be expected to result in a reduced number of erythrocytes. However, our results are not indicative of anemia in smokers since erythrocyte count and other hematological parameters of smokers were not significantly different from those of non-smokers. However, we could not fully confirm the results from observational studies demonstrating higher red blood cell count, hematocrit, hemoglobin, and MCV in smokers than in non-smokers9,10. In line with those studies, we found moderately higher MCH and MCHC in smokers, in particular in those smoking a high number of cigarettes per day.
Higher eryptosis in smokers did not translate into a lower erythrocyte count. It must be kept in mind that enhanced erythropoiesis could, at least in theory, compensate higher eryptosis-dependent erythrocyte loss in smokers. Moreover, also a numerically small elevation in the percentage of phosphatidylserine-exposing erythrocytes can be expected to impede microcirculation due to the adhesion of these cells to the vascular wall. As a matter of fact, smokers do have impeded microcirculation2.
Strengths and limitations
The strength of our investigation is the relatively large population-based sample with rigorous assessment of smoking. However, smoking was retrospectively reported and can be subject to reporting bias. Since prospective outcome data are not available yet, we are currently not able to study if higher eryptosis is indeed associated with an increased risk of cardiovascular diseases. Additionally, the underlying mechanism of enhanced eryptosis in heavier smokers could not be examined with our study design.
To conclude, our observational study revealed that smokers exhibit more eryptosis than non-smokers or ex-smokers. The higher proportion of eryptotic erythrocytes in smokers was not associated with a reduced number of erythrocytes and anemia, respectively.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon request.
References
Gallucci, G. et al. Cardiovascular risk of smoking and benefits of smoking cessation. J. Thorac. Dis. 12, 3866–3876. https://doi.org/10.21037/jtd.2020.02.47 (2020).
Leone, A. & Landini, L. Vascular pathology from smoking: Look at the microcirculation!. Curr. Vasc. Pharmacol. 11, 524–530. https://doi.org/10.2174/1570161111311040016 (2013).
Thrul, J. et al. A scoping review and meta-analysis of the use of remote biochemical verification methods of smoking status in tobacco research. Nicotine Tob. Res. 25, 1413–1423. https://doi.org/10.1093/ntr/ntac271 (2023).
Talhout, R. et al. Hazardous compounds in tobacco smoke. Int. J. Environ. Res. Public Health 8, 613–628. https://doi.org/10.3390/ijerph8020613 (2011).
Carnevali, S. et al. Cigarette smoke extract induces oxidative stress and apoptosis in human lung fibroblasts. Am. J. Physiol. Lung Cell Mol. Physiol. 284, L955–L963. https://doi.org/10.1152/ajplung.00466.2001 (2003).
Sun, Y. et al. Acrolein induced both pulmonary inflammation and the death of lung epithelial cells. Toxicol. Lett. 229, 384–392. https://doi.org/10.1016/j.toxlet.2014.06.021 (2014).
Park, E. et al. Cigarette smoke extract may induce lysosomal storage disease-like adverse health effects. J. Appl. Toxicol. 39, 510–524. https://doi.org/10.1002/jat.3744 (2019).
Palmeri, R. & Gupta, V. Carboxyhemoglobin Toxicity (StatPearls Publishing, 2023).
Wang, Y. et al. Association between electronic cigarettes use and whole blood cell among adults in the USA—A cross-sectional study of National Health and Nutrition Examination Survey analysis. Environ. Sci. Pollut. Res. 29, 88531–88539. https://doi.org/10.1007/s11356-022-21973-6 (2022).
Shakiba, E. et al. Tobacco smoking and blood parameters in the Kurdish population of Iran. BMC Cardiovasc. Disord. 23, 401. https://doi.org/10.1186/s12872-023-03433-2 (2023).
Lang, E. et al. Carbon monoxide-sensitive apoptotic death of erythrocytes. Basic Clin. Pharmacol. Toxicol. 111, 348–355. https://doi.org/10.1111/j.1742-7843.2012.00915.x (2012).
Restivo, I. et al. Cigarette smoke extract induces p38 MAPK-initiated Fas-mediated eryptosis. Int. J. Mol. Sci. 23, 14730. https://doi.org/10.3390/ijms232314730 (2022).
Dreischer, P., Duszenko, M., Stein, J. & Wieder, T. Eryptosis: Programmed death of nucleus-free, iron-filled blood cells. Cells https://doi.org/10.3390/cells11030503 (2022).
Attanzio, A. et al. Increased eryptosis in smokers is associated with the antioxidant status and C-reactive protein levels. Toxicology 411, 43–48. https://doi.org/10.1016/j.tox.2018.10.019 (2019).
Föller, M. & Lang, F. Ion transport in eryptosis, the suicidal death of erythrocytes. Front. Cell Dev. Biol. 8, 597. https://doi.org/10.3389/fcell.2020.00597 (2020).
Lang, E. & Lang, F. Triggers, inhibitors, mechanisms, and significance of eryptosis: the suicidal erythrocyte death. BioMed. Res. Int. 2015, 513518. https://doi.org/10.1155/2015/513518 (2015).
Lang, F., Bissinger, R., Abed, M. & Artunc, F. Eryptosis—The neglected cause of anemia in end stage renal disease. Kidney Blood Press. Res. 42, 749–760. https://doi.org/10.1159/000484215 (2017).
German National Cohort Consortium. The German National Cohort: Aims, study design and organization. Eur. J. Epidemiol. 29, 371–382. https://doi.org/10.1007/s10654-014-9890-7 (2014).
Dragano, N. et al. Soziodemografische und erwerbsbezogene Merkmale in der NAKO Gesundheitsstudie. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 63, 267–278. https://doi.org/10.1007/s00103-020-03098-8 (2020).
Peters, A. et al. Framework and baseline examination of the German National Cohort (NAKO). Eur. J. Epidemiol. 37, 1107–1124. https://doi.org/10.1007/s10654-022-00890-5 (2022).
Schipf, S. et al. Die Basiserhebung der NAKO Gesundheitsstudie: Teilnahme an den Untersuchungsmodulen, Qualitätssicherung und Nutzung von Sekundärdaten. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 63, 254–266. https://doi.org/10.1007/s00103-020-03093-z (2020).
Ewendt, F. et al. Association between vitamin D status and eryptosis–results from the German National Cohort Study. Ann. Hematol. 102, 1351–1361. https://doi.org/10.1007/s00277-023-05239-w (2023).
R Core Team (2021) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria.
Bürkner, P.-C. brms: An R package for Bayesian multilevel models using Stan. J. Stat. Softw. 80, 1–28. https://doi.org/10.18637/jss.v080.i01 (2017).
Stan Development Team (2022) Stan Modeling Language Users Guide and Reference Manual.
Messner, B. & Bernhard, D. Smoking and cardiovascular disease: Mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler. Thromb. Vasc. Biol. 34, 509–515. https://doi.org/10.1161/ATVBAHA.113.300156 (2014).
Iversen, B., Jacobsen, B. K. & Løchen, M.-L. Active and passive smoking and the risk of myocardial infarction in 24,968 men and women during 11 year of follow-up: The Tromsø Study. Eur. J. Epidemiol. 28, 659–667. https://doi.org/10.1007/s10654-013-9785-z (2013).
Jarlstrup, N. S. et al. The impact of the Danish National Smoking Ban From 2007 on the incidence of eight smoking-related diseases: A nationwide register-based interrupted time series analysis. Nicotine Tob. Res. 25, 648–656. https://doi.org/10.1093/ntr/ntac257 (2023).
Pan, B. et al. The relationship between smoking and stroke: A meta-analysis. Medicine (Baltimore) 98, e14872. https://doi.org/10.1097/MD.0000000000014872 (2019).
Borst, O. et al. Dynamic adhesion of eryptotic erythrocytes to endothelial cells via CXCL16/SR-PSOX. Am. J. Physiol. Cell Physiol. 302, C644–C651. https://doi.org/10.1152/ajpcell.00340.2011 (2012).
Lang, F. et al. Ceramide in suicidal death of erythrocytes. Cell Physiol. Biochem. 26, 21–28. https://doi.org/10.1159/000315102 (2010).
Acknowledgements
We thank F. Reipsch, Ch. Leibelt, H. Giese, and S. Ross for technical assistance. This study was supported by a Grant to M.F. from Deutsche Stiftung für Herzforschung e.V. (F04/18). M.S. was supported by the Cyber Valley Research Fund (Grant Number: CyVy-RF-2021-16). M.S. and P.-C.B. were supported by Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy—EXC-2075—390740016 (the Stuttgart Cluster of Excellence SimTech). This project was conducted with data from the German National Cohort (NAKO) (www.nako.de). NAKO is funded by the Federal Ministry of Education and Research (BMBF) [Project funding reference numbers: 01ER1301A/B/C, 01ER1511D and 01ER1801A/B/C/D], several German states and Helmholtz Association, the participating universities and the institutes of Leibniz Association. We thank all participants who took part in the NAKO study and the staff of this research initiative.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by Franz Ewendt, Marvin Schmitt, Alexander Kluttig, Wim Wätjen, and Paul-Christian Bürkner. The first draft of the manuscript was written by Gabriele Stangl, Michael Föller, Marvin Schmitt, and Franz Ewendt. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
M.F. received honoraria from Kyowa Kirin without a relationship to this study. The other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schmitt, M., Ewendt, F., Kluttig, A. et al. Smoking is associated with increased eryptosis, suicidal erythrocyte death, in a large population-based cohort. Sci Rep 14, 3024 (2024). https://doi.org/10.1038/s41598-024-53258-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53258-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.