Abstract
The coexistence of heart failure is frequent and associated with higher mortality in patients with type 2 diabetes (T2DM), and its management is a critical issue. The WATCH-DM risk score is a tool to predict heart failure in patients with type 2 diabetes mellitus (T2DM). We investigated whether it could estimate outcomes in T2DM patients with heart failure with preserved ejection fraction (HFpEF). The WATCH-DM risk score was calculated in 418 patients with T2DM hospitalized for HFpEF (male 49.5%, age 80 ± 9 years, HbA1c 6.8 ± 1.0%), and they were divided into the “average or lower” (≤ 10 points), “high” (11–13 points) and “very high” (≥ 14 points) risk groups. We followed patients to observe all-cause death for 386 days (median). We compared the area under the curve (AUC) of the WATCH-DM score for predicting 1-year mortality with that of the Meta-Analysis Global Group in Chronic Heart Failure (MAGGIC) score and of the Barcelona Bio-Heart Failure Risk (BCN Bio-HF). Among the study patients, 108 patients (25.8%) had average or lower risk scores, 147 patients (35.2%) had high risk scores, and 163 patients (39.0%) had very high risk scores. The Cox proportional hazard model selected the WATCH-DM score as an independent predictor of all-cause death (HR per unit 1.10, 95% CI 1.03 to 1.19), and the “average or lower” risk group had lower mortality than the other groups (p = 0.047 by log-rank test). The AUC of the WATCH-DM for 1-year mortality was 0.64 (95% CI 0.45 to 0.74), which was not different from that of the MAGGIC score (0.72, 95% CI 0.63 to 0.80, p = 0.08) or that of BCN Bio-HF (0.70, 0.61 to 0.80, p = 0.25). The WATCH-DM risk score can estimate prognosis in T2DM patients with HFpEF and can identify patients at higher risk of mortality.
Similar content being viewed by others
Introduction
Heart failure (HF) is one of the major complications of diabetes mellitus (DM) and is strongly associated with the prognosis of diabetic patients. HF is observed in up to 22% of diabetic patients, and patients with DM or prediabetes have a two to four times higher risk of developing HF than those without them1,2,3,4. HF is also the strongest risk factor for death among cardiovascular or renal complications in patients with newly diagnosed type 2 diabetes mellitus (T2DM) 1,3,5. On the other hand, DM is present in 20 to 40% of HF patients4. Diabetic patients have comorbidities such as hypertension, hypertension, atrial fibrillation, anemia, iron deficiency, serum potassium disturbances, frailty, and CKD more frequently6,7,8. and concomitant DM increases mortality and hospitalization in patients with HF1,2,3,4,9. HF with preserved ejection fraction (HFpEF) is as common as HF with reduced ejection fraction (HFrEF) in T2DM patients, and the impact of DM on cardiovascular death or HF hospitalization is greater in HFpEF than in HFrEF9.
Whereas most glucose-lowering agents did not reduce the incidence of HF in T2DM patients in randomized control trials10, and SGLT2 inhibitors can reduce HF incidence, leading to fewer MACE and cardiovascular death in patients with T2DM11,12,13. SGLT2 inhibitors reduce cardiovascular death and HF hospitalization in both HFrEF14,15 and HFpEF16,17 patients with or without DM. Guidelines recommend empagliflozin or dapagliflozin in patients with T2DM and LVEF > 40% (HF with mildly reduced EF and HFpEF) to reduce the risk of HF hospitalization or CV death6,10. However, SGLT2 inhibitors are more expensive than traditional treatments. Guidelines recommend that DM treatment regimens need to be continuously reviewed for efficacy, side effects, and burden, and in some cases, reduction or discontinuation of medication should be considered for several reasons, including cost10. Patients suitable for expensive treatments should be appropriately selected.
For the risk stratification of patients with T2DM and HF, prediction of functional and clinical outcomes is as important as prediction of HF development. The WATCH-DM risk score is a novel risk score for predicting incident HF hospitalization in T2DM patients without baseline HF, using readily available clinical, laboratory, and electrocardiographic (ECG) variables18. Most of these variables are relevant to heart failure, and we hypothesized that this score might be associated with severity of disease and clinical outcomes in patients with established heart failure. Thus, we investigated whether the WATCH-DM score can predict prognosis in T2DM patients hospitalized with acutely decompensated HFpEF. We also compared its ability to predict all-cause mortality with other established risk scores.
Methods
Study population
We retrospectively analyzed the data from the Prospective Multicenter Observational Study of Patients with Heart Failure with Preserved Ejection Fraction (PURSUIT-HFpEF), a multicenter, observational study enrolling consecutive patients hospitalized with acute decompensated HFpEF (left ventricular ejection fraction (LVEF) ≥ 50%) in 31 collaborating hospitals [UMIN-CTR ID: UMIN000021831]. Details of the entry criteria and data collection have been described elsewhere19. Briefly, patients admitted with acutely decompensated HFpEF were registered, and their clinical data, including medications, laboratory tests, and ECG, were collected on admission, at discharge, and 1 year after discharge. Acutely decompensated HFpEF was diagnosed based on the following criteria: (1) clinical symptoms and signs according to the Framingham Heart Study criteria, (2) LVEF on admission ≥ 50%, and (3) serum N-terminal pro-B type natriuretic peptide (NT-proBNP) ≥ 400 pg/mL or brain natriuretic peptide ≥ 100 pg/mL. T2DM was diagnosed based on clinical history or on fasting plasma glucose and/or hemoglobin A1c (HbA1c) during hospitalization based on the Japanese Clinical Practice Guideline for Diabetes 201920. Oral glucose tolerance testing was not mandatory for the present study.
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by each corresponding hospital’s Ethics Committee. Informed consent was obtained from each patient by one of the investigators before the study.
Data collection
We collected patient data, including risk factors and history of major comorbidities such as DM, hypertension, dyslipidemia, smoking, chronic kidney disease (CKD), history of HF hospitalization, prior myocardial infarction, prior stroke and malignancy, and history of percutaneous coronary intervention or coronary artery bypass graft (CABG). Blood tests, standard 12-lead ECG recording, chest radiography, and echocardiography were performed immediately after admission, before discharge, and 1 year after discharge. LVEF was determined by either the Teichholz method or the modified Simpson’s technique on admission but only by Simpson’s technique at discharge and 1 year after discharge. Study patients were followed up by direct contact or telephone interview to observe all-cause death, which was a primary endpoint of the PURSUIT-HFpEF registry19. For patients whose survival information could not be determined by these means, the data from National Vital Statistics of Japan, which includes all death records in Japan reported by prefectural public health centers, were used with the permission of the Ministry of Health, Labor and Welfare in accordance with the Statistics Act in Japan.
The WATCH-DM risk score and other heart failure risk scores
We calculated the WATCH-DM score as the sum of the scores obtained from the following factors18: age (0 to 6 points), body mass index (BMI, 0 to 5 points), systolic (0 to 3 points) and diastolic (0 to 2 points) blood pressure (BP), fasting plasma glucose (0 to 3 points), serum creatinine (0 to 5 points), high density lipoprotein cholesterol (HDL-c, 0 to 2 points), QRS width on ECG (0 or 3 points) and history of myocardial infarction (0 or 3 points) or CABG (0 or 2 points), all of which were measured or obtained at hospital discharge (Table 1). The original study estimated the risk of incident HF as very low (≤ 7 points), low (8–9 points), average (10 points), high (11–13 points) and very high (≥ 14 points)18. In the present study, we used the same risk classification was used tentatively to estimate the risk of HF outcomes. Due to the limited number of patients, we combined patients with very low to average risk as the “average or lower” risk group.
To compare the ability of the WATCH-DM risk score to predict 1-year mortality with other HF risk scores, we calculated the Meta-Analysis Global Group in Chronic Heart Failure (MAGGIC) risk score21 and the mortality risk using the Barcelona Bio-Heart Failure Risk (BCN Bio-HF) calculator22. We calculated the MAGGIC risk score as the sum of scores provided from the following factors: LVEF (0 point to all present patients with HFpEF), age (0 to 15 points), systolic BP (0 to 2 points), BMI (0 to 6 points), creatinine (0 to 8 points), New York Heart Association (NYHA) class (0 to 8 points), male sex (0 or 1 point), current smoker (0 or 1 point), DM (3 points for all present patients), diagnosis of chronic obstructive pulmonary disease (0 or 2 points), first diagnosis of heart failure in the 18 months (0 or 2 points), not on beta blockers (0 or 3 points) and not on renin–angiotensin–aldosterone blockers (0 or 1 point)21. We estimated 1-year mortality by the web-based BCN Bio-HF calculator (http://ww2.bcnbiohfcalculator.org/web/, accessed at September and October 2021) using age, sex, NYHA class, LVEF, serum sodium, estimated glomerular filtration rate (eGFR), hemoglobin, loop diuretic dose, beta blocker, angiotensin converting enzyme inhibitor/angiotensin-2 receptor blocker, and statin treatments22. We did not include biomarkers for the present analysis because NT-proBNP was not measured in some patients, and cardiac troponin T or ST-2 was not measured at all.
Statistical analysis
Continuous variables are expressed as the mean and standard deviation or median [the interquartile range (IQR)]. Categorical variables are expressed as absolute frequencies or relative percentages. We made comparisons by one-way ANOVA for continuous variables, and the significance of differences among groups was calculated with the Bonferroni correction. Categorical variables were compared with Fisher’s exact test. For the correlation between WATCH-DM score and continuous or ordinal values, Spearman's rank correlation coefficient was calculated. A Cox proportional hazard model for all-cause death was constructed including factors that showed significant differences (p < 0.05) among the 3 risk groups, although factors that were included by or highly related to the WATCH-DM score were not included. Event-free survival analysis was performed using the Kaplan‒Meier method with the log-rank test for group comparisons. We compared hazard ratios per unit of the WATCH-DM score between subgroups using Wald test.
We constructed time-dependent receiver operating characteristic (ROC) curves of the risk scores for all-cause death at 1 year after hospitalization using the “time ROC” package (ver 0.4) for R. We compared the difference between the estimated area under the curves (AUC) of two risk scores for each time point, and the p value between them was obtained by calculating the variance of the difference using the independent and identically distributed (iid) representation of the AUC estimators. Youden’s J statistics was calculated as sensitivity + specificity − 1 for all points of an ROC curve using “cenROC” package (ver 2.0.0) for R23, and the maximum value of the index was used as a criterion for selecting the optimum cut-off point. All statistical analyses were performed using R (version 4.1.1) or R with a graphical user interface EZR (Saitama Medical Centre, Jichi Medical University, Japan).
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the ethics committee of each hospital according to the Ethical Guidelines for Medical and Health Research Involving Human Subjects issued by the Ministry of Health, Labor and Welfare in Japan. The study was conducted in accordance with the Declaration of Helsinki, the Ethical Guidelines for Medical and Health Research Involving Human Subjects, and other current legal regulations in Japan. Informed consent was obtained from each patient by one of the investigators before the study.
Results
Patient characteristics
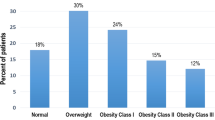
Among 1095 patients hospitalized for decompensated HFpEF and registered in PURSUIT-HFpEF between June 2016 and December 2020, 418 patients (38.2%) had T2DM. The mean age of the study patients was 80 ± 9 years, and 207 (49.5%) patients were male. The mean HbA1c was 6.8 ± 1.0%, and the mean BMI was 23.1 ± 4.4 kg/m2. Diabetes was diagnosed before hospitalization in 316 patients (75.6%), and it was newly diagnosed after hospitalization in 102 patients (24.4%).
The Watch-DM score
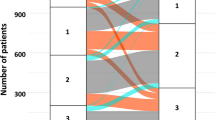
The mean WATCH-DM risk score in the study group was 12.8 ± 3.1 points, 108 patients (25.8%) had very low to average, 147 patients (35.2%) had high, and 163 patients (39.0%) had very high HF risk (Fig. 1). There were differences in clinical risk factors among groups, most of which were included in the WATCH-DM score: age (p < 0.0001), male sex (p = 0.003), BMI (p = 0.02), systolic (p = 0.02) and diastolic (p < 0.0001) BP, fasting plasma glucose (p = 0.003), serum creatinine (p < 0.0001) and LDL cholesterol (p = 0.002), whereas no difference was found in HbA1c (p = 0.70) and HDL cholesterol (p = 0.07) (Table 2).
Distribution of the WATCH-DM scores in the study group. The number of patients with each score is shown as a bar. The heart failure (HF) risk was determined as the 5-year incidental HF risk in the original article18: ≤ 7 points very low; 8–9 points, low; 10 points, average; 11–13 points, high; ≥ 14 points, very high risk.
NT-proBNP was measured in 359 patients (85.9%), and it was correlated with WATCH-DM score (ρ = 0.33, p < 0.0001). The “very high” risk group had a higher NT-proBNP value (1638 [774, 4848] ng/L) than the “average or lower” (696 [400, 1442] ng/L, p = 0.002) and the “high” risk (836 [386, 1665] ng/L, p = 0.003) groups.
There were differences in the rate of prescription of antiplatelets, anticoagulants, statins, digoxin, and calcium channel blockers among the risk score groups. Among diabetes medications, there were significant difference in the prescription of biguanides, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and insulin.
Table 3 demonstrates echocardiography parameters measured at discharge. Left ventricular diameters were significantly higher in patients with very high risk than those with average or lower risk. They also had larger left ventricular mass index than those with average or lower risk and higher E/e′ ratio than other two groups, whereas no differences were observed in other diastolic parameters.
Clinical outcomes and the WATCH-DM score
During the follow-up period of 386 [IQR 221 to 729] days, 77 patients (18.4%) died. We constructed a Cox proportional hazard model using sex, history of hypertension, CKD, dyslipidemia, LDL-cholesterol and the WATCH-DM score, which were significantly different among the 3 risk groups (Table 2), for all-cause mortality. We did not include age, BMI, systolic/diastolic BP, serum creatinine, or fasting plasma glucose because these factors were included in the WATCH-DM score. We did not include eGFR because creatine was used in the WATCH-DM score, while history of CKD was included in the analysis.
The Cox proportional hazard model selected the WATCH-DM score as an independent predictor for all-cause death (hazard ratio (HR) per unit 1.10, 95% confidence interval (CI) 1.01 to 1.20, p = 0.006), together with dyslipidemia and CKD (Table 4). When the classification by the risk score was used for analysis instead of WATCH-DM score, it was selected as the only significant predictive factor (HR 1.52, 95% CI 1.07 to 2.1, p = 0.02), whereas dyslipidemia (p = 0.06) and CKD (p = 0.10) were not. The adjusted HR in the “very high risk” group, with the “average or lower” risk group as reference, was 2.29 [95% CI 1.05 to 5.01, p = 0.04], while the HR in the “high risk” was not statistically significant (HR 1.69 [95% CI 0.79 to 3.60, p = 0.17]).
Kaplan‒Meier curves showed the difference in all-cause mortality among the 3 groups (p = 0.047 by log-rank test), and the “very high” risk group had higher mortality than the “average or lower” risk group (p = 0.043) (Fig. 2).
Kaplan‒Meier curves for all-cause mortality. Death was observed in 12 patients with average or lower risk, in 27 patients with high risk and in 38 patients with very high risk during follow-up period (median 386 days, IQR 221 to 729 days). There were significant differences in mortality among the three groups (p = 0.047 by log-rank test). Patients with very high risk (≥ 14 points) had a higher mortality than those with average or lower risk (≤ 10 points, p = 0.043).
No significant difference was observed in hazard ratios between subgroups based on age, gender, BMI, glycemic control, risk factors, and use of statin, glucose lowering drugs, or insulin (Fig. 3).
Subgroup analysis of hazard ratio per unit of the WATCH-DM risk score. Hazard ratios for all-cause mortality per unit of the WATCH-DM score were compared between subgroups based on age, gender, BMI, glycemic control, use of glucose lowering drugs, insulin, or statin, and risk factors. There was no significant difference between all subgroups.
Comparison of the WATCH-DM score and the other risk scores
The MAGGIC score in the study group was 25.7 ± 5.6, and it was significantly correlated with WATCH-DM (ρ = 0.395, p < 0.001) (Fig. 4). The AUC of the WATCH-DM for all-cause death at 1 year was 0.64 (95% CI 0.45 to 0.74). The AUC of the MAGGIC score was 0.72 (95% CI 0.63 to 0.80), and there was no difference in AUC between the two scores (p = 0.08) (Fig. 4). The AUC for 1-year mortality prediction by the BCN Bio-HF calculator was 0.70 (95% CI 0.61 to 0.80), which was not different from that of the WATCH-DM risk score (p = 0.25). The maximum Youden’s J statistics for the WATCH-DM score, the MAGGIC score, and BCN Bio-HF was 0.168, 0.291 and 0.319, respectively. The optimal cutoff value of the WATCH-DM score determined by Youden’s J statistics was 13.5, which corresponded to a score that distinguished the “very high” risk group from the others.
Time-dependent ROC curves for the prediction of 1-year mortality. Time-dependent ROC curves of the WATCH-DM score (top, left), the MAGGIC score (top, right) and BCN Bio-HF (bottom) for all-cause death at 1 year after hospitalization. Vertical dotted lines (J) indicated maximum value of Youden's J statistics. The areas under the curve (AUCs) of the WATCH-DM score and MAGGIC score were 0.64 (95% CI 0.45 to 0.74) and 0.72 (95% CI 0.63 to 0.80), respectively. The AUC of BCN Bio-HF was 0.70 (95% CI 0.61 to 0.80), which was not different from that of the WATCH-DM risk score (p = 0.25).
Discussion
We investigated the ability of the WATCH-DM risk score to predict all-cause mortality in 418 T2DM patients hospitalized for decompensated HFpEF. During the follow-up period of 386 (median) days, all-cause death was observed in 77 patients, and the WATCH-DM score was selected as an independent predictor for all-cause death (HR per unit 1.10, 95% CI 1.01 to 1.20, p = 0.006), along with dyslipidemia and CKD. Significant differences in all-cause mortality were observed among the “average or lower’’ (≤ 10 points), the “high” and the “very high” (≥ 14 points) risk groups (p = 0.047 by log-rank test), and the very high risk group had higher mortality than the “average or lower" risk group (p = 0.043). The AUC for the prediction of all-cause mortality by the WATCH-DM score was not different from that of the MAGGIC score (p = 0.08) and that by the BCN Bio-HF calculator (p = 0.25). These results indicate that the WATCH-DM score was associated with all-cause mortality in T2DM patients with HFpEF, and a 1-point increase of the WATCH-DM score was associated with a 10% increase in mortality.
This study was based on a large multicenter registry study of patients with decompensated HFpEF, the PURSUIT-HFpEF study, which enrolled more than one thousand patients from 31 collaborating hospitals (1 university hospital and 30 regional core centers)19. The PURSUIT-HFpEF study was unique in that it enrolled a heterogeneous and large number of patients with broad inclusion criteria and few exclusion criteria to provide an accurate understanding of real-world patients with HFpEF. Detailed clinical data were collected using an electronic data capture system integrated with the electronic medical record, and clinical outcomes were followed as closely as possible, even using the national death certification system19. Survival data were compared using statistically appropriate methods, including time-dependent ROC curve analysis. We believe that one of the strengths of this study was the highly reliable data collection, which well reflected a real-world HFpEF population.
The predictive value of the MAGGIC score and BCN Bio-HF in diabetic patients with HFpEF has not been previously reported. To our knowledge, this study is the first to demonstrate how well these risk scores can predict all-cause mortality and to directly compare their predictive values in this complicated patient population.
The heart failure risk scores for diabetic patients
The management of heart failure in diabetic patients is more complicated than that in non-diabetic patients, and intensive glycemic control does not consistently correlate with improved clinical outcomes in HF patients with diabetes. While the risk of HF hospitalization tends to increase progressively with fasting blood glucose24,25, the association between HbA1c and mortality among patients with HF is consistently U-shaped, with the lowest mortality in individuals with HbA1c 7–8%26,27,28,29. HbA1c < 7% may be associated with worse prognosis in diabetic patients with HFpEF after adjustment for age, BMI, hemoglobin and NT-proBNP30.
Most of the risk scores for predicting HF prognosis have been derived from the data of HF patients with or without diabetes, and they may not adequately account for the influence of glycemic control. The presence of DM is used to calculate the MAGGIC score, but blood glucose or HbA1c is not included21. BCN Bio-HF does not use any factors related to DM or glycemic control22. The WATCH-DM score uses fasting plasma glucose for its calculation, reflecting the importance of metabolic factors in the development and prognosis of HF in diabetic patients.
The European Society of Cardiology guidelines for the management of cardiovascular disease in diabetic patients recommend that systematic survey for HF symptoms and/or signs of HF at each clinical encounter in all diabetic patients6. The WATCH-DM scores use factors that are commonly available in daily DM practice. Uniform assessment of the WATCH-DM score in the diabetes clinic would be useful in assessing the risk of incident HF in patients without HF and the prognostic risk in those with comorbid HF.
The present study did not show that the WATCH-DM score is superior to the MAGGIC score and BCN Bio-HF in predicting prognosis of T2DM patients with HFpEF. AUC of the WATCH-DM score was 0.65, which was classified as satisfactory but not optimal. Recently, Zhang et al. reported similar results on the predictive value of the WATCH-DM score in diabetic patients with HFpEF in a single-center study31. Their results showed a similar AUC value for the prediction of all-cause mortality (AUC = 0.67, 95% CI 0.59–0.74) to the present one, while it was lower than that for cardiovascular death (0.71, 95% CI 0.63–0.78). They reported that the WATCH-DM score did not stratify the risk of all-cause or cardiovascular mortality in non-diabetic patients with HFpEF31, suggesting the heterogeneity of HFpEF phenotypes between diabetic and non-diabetic patients and the need for more effective risk scores specified for HFpEF patients with T2DM.
Improving prognostic prediction in T2DM patients with HFpEF
If WATCH-DM is not superior to other risk scores, are there ways to improve its predictive power?
The coefficients assigned to the variables within the WATCH-DM score were derived to predict the occurrence of incident HF regardless of LVEF, not for evaluating clinical outcomes in HFpEF. Among the present study patients, 108 patients (25.8%) had average or lower risk, while 5-year incident HF risk of incident HF was 1.1% for the very low-, 3.6% for the low-, and 4.7% for the average risk group18, which implied that the WATCH-DM score may underestimate the risk of HFpEF. While a linear relationship between BP and prognosis is observed in the general population, its relation may be inversed or J-shaped in patients with HF32. Systolic BP of 120–129 mmHg had the lowest cardiovascular event risk and < 120 mmHg was associated with a higher incidence of all-cause mortality in patients with HFpEF33,34. A U-shaped relationship was also observed between BMI and clinical outcomes including mortality in HFpEF35,36,37. Inclusion of these variables in a linear fashion may have reduced the prognostic value of the WATCH-DM score. Optimizing the coefficients for the variables may improve predictive value of the risk score, although this requires a much larger study cohort than the present study group.
The MAGGIC risk score and the BCN-Bio calculator include medications as factors for calculation. The WATCH-DM score does not include any medication as a factor, and which may be one of the reasons why the WATCH-DM score did not outperform other HF risk scores. Adding the use of SGLT2 inhibitors, which are recommended for both T2DM and HFpEF, would improve predictivity of the WATCH-DM score. The present data were collected before SGLT2 inhibitors were recommended for the treatment of HFpEF, and the number of patients taking SGLT2 inhibitors or GLP-1 receptor agonists was so small that their effects could not be properly analyzed.
Natriuretic peptide has a high prognostic value in diabetic patients as well as in HF patients. Left ventricular diastolic dysfunction is frequently observed in asymptomatic diabetic patients, and it can be effectively detected by increased natriuretic peptide38. Serial monitoring of NT-proBNP in T2DM patients may be useful to identify patients at highest risk of HF39, and guidelines recommend measurement of a natriuretic peptide in asymptomatic diabetic patients on at least a yearly basis to identify the earliest HF stages and implement strategies to prevent transition to symptomatic HF2. The addition of natriuretic peptide levels to the WATCH-DM risk score was associated with greater improvement in the prediction of the incident HF40. Prediction of clinical outcomes by the WATCH-DM score may be improved by addition of natriuretic peptide.
The TRS-HFDM (Thrombolysis in Myocardial Infarction [TIMI] risk score for heart failure in diabetes) risk scores was recently developed to predict HF risk in T2DM patients41,42. While the TRS-HFDM score was developed to predict HF hospitalization in patients with and without a prior HF history, it could predict incident HF events as well as the WATCH-DM among T2DM patients without previous HF hospitalization43.
Ceramides are associated with the development of diabetes and its complications including heart disease. The Ceramide risk score has been developed for clinical use based on ceramide concentrations and their ratios44, and it can predict major adverse cardiovascular events independent of coronary artery disease or conventional risk factors45,46. Elevated ceramide level are linked to insulin resistance47 which may be related to cardiac function in HF patients48,49. It should be investigated whether new risk scores such as the TRS-HFDM score or the ceramide score could predict clinical outcomes in T2DM patients with HFpEF.
Study limitations
The present study was a retrospective study from a registery database with a limited number of patients, and therefore, there could be some bias which could affect the present results. Oral glucose tolerance testing was not mandatory in the PURSUIT-HFpEF registry and DM may have been underdiagnosed, resulting in a higher WATCH-DM score in the study group. Patients with very high risk were more likely to receive antiplatelets and statins than other groups. The number of patients taking particular glucose-lowering drugs such as SGLT2 inhibitor or GLP-1 receptor agonists were so small that their effects could not be properly analyzed. Patients at higher risk tended to have lower rates of atrial fibrillation, though not statistically significant, and this may be due to selection bias.
Ethnic differences exist in the mortality and morbidity of T2DM50 and HFpEF51,52,53. The mean BMI was only 23.1 kg/m2, and the mean age was 80 years in the present study patients. Their characteristics were different from those of typical Western patients, and it is unclear whether the present results are applicable to patients outside of East Asia. A recent study demonstrated that treatment with semaglutide reduced body weight and improved symptoms and physical activity in patients with HFpEF and BMI ≥ 30 kg/m2, indicating the importance of BMI in the pathophysiology of HFpEF54. The low BMI in the study group has made the contribution of this important factor to the risk score almost negligible.
Difference in characteristics and outcomes of HF patients has also been observed between urban and rural areas55,56. All of the participating hospitals of the PURSUIT-HF study were located in a single urban region of Japan, which may introduce some bias in patient background.
Despite these study limitations, the present study suggested the possible role of the WATCH-DM score in the management of T2DM patients with HFpEF. The present study was a small-scale, retrospective proof-of-concept study. A large-scale, prospective study is required to establish the way to predict clinical outcomes in this challenging patient population.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Dunlay, S. M. et al. Type 2 diabetes mellitus and heart failure: a scientific statement from the American Heart Association and the Heart Failure Society of America: This statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation. 140, E294-324 (2019).
Pop-Busui, R. et al. Heart failure: An underappreciated complication of diabetes. A consensus report of the American Diabetes Association. Diabetes Care. 45, 1670–1690 (2022).
McAllister, D. A. et al. Incidence of hospitalization for heart failure and case-fatality among 3.25 million people with and without diabetes mellitus. Circulation. 138, 2774–2786 (2018).
Seferović, P. M. et al. Type 2 diabetes mellitus and heart failure: A position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 20, 853–872 (2018).
Zareini, B. et al. Type 2 Diabetes mellitus and impact of heart failure on prognosis compared to other cardiovascular diseases: A nationwide study. Circ. Cardiovasc. Qual. Outcomes. 13, 386–394 (2020).
Marx, N. et al. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur. Heart J. 44, 4043–4140 (2023).
McHugh, K. et al. Heart failure with preserved ejection fraction and diabetes: JACC State-of-the-Art review. J. Am. Coll. Cardiol. 73, 602–611 (2019).
Jankauskas, S. S. et al. Heart failure in diabetes. Metabolism. 125, 154910 (2021).
MacDonald, M. R. et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur. Heart J. 29, 1377–1385 (2008).
Elsayed, N. A. et al. 9. Pharmacologic approaches to glycemic treatment: Standards of care in diabetes-2023. Diabetes Care. 46, S140-157 (2023).
Zinman, B. et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 373, 17–18 (2015).
Wiviott, S. D. et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 380, 347–357 (2019).
Zelniker, T. A. et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 393, 31–39 (2019).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424 (2020).
McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 381, 1995–2008 (2019).
Anker, S. D. et al. Empagliflozin in heart failure with a preserved ejection fraction. N. Engl. J. Med. 385, 1451–1461 (2021).
Solomon, S. D. et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N. Engl. J. Med. 387, 1089–1098 (2022).
Segar, M. W. et al. Machine learning to predict the risk of incident heart failure hospitalization among patients with diabetes: The WATCH-DM Risk Score. Diabetes Care. 42, 2298–2306 (2019).
Suna, S. et al. Study protocol for the PURSUIT-HFpEF study: A prospective, multicenter, observational study of patients with heart failure with preserved ejection fraction. BMJ Open. 10, e038294 (2020).
Araki, E. et al. Japanese clinical practice guideline for diabetes 2019. Diabetol. Int. 11, 165–223 (2020).
Pocock, S. J. et al. Predicting survival in heart failure: A risk score based on 39 372 patients from 30 studies. Eur. Heart J. 34, 1404–1413 (2013).
Lupón, J. et al. Development of a novel heart failure risk tool: The Barcelona Bio-Heart Failure risk calculator (BCN Bio-HF calculator). PLoS ONE. 9, e85466 (2014).
Beyene, K. M. & El Ghouch, A. Time-dependent ROC curve estimation for interval-censored data. Biom J. 64, 1056–1074 (2022).
Held, C. et al. Glucose levels predict hospitalization for congestive heart failure in patients at high cardiovascular risk. Circulation. 115, 1371–1375 (2007).
Lind, M. et al. The relationship between glycemic control and heart failure in 83,021 patients with type 2 diabetes. Diabetologia. 55, 2946–2953 (2012).
Aguilar, D., Bozkurt, B., Ramasubbu, K. & Deswal, A. Relationship of hemoglobin A1C and mortality in heart failure patients with diabetes. J. Am. Coll. Cardiol. 54, 422–428 (2009).
Elder, D. H. et al. Mean HbA1c and mortality in diabetic individuals with heart failure: A population cohort study. Eur. J. Heart Fail. 18, 94–102 (2016).
Lawson, C. A. et al. Association between type 2 diabetes and all-cause hospitalization and mortality in the UK general heart failure population: Stratification by diabetic glycemic control and medication intensification. JACC Heart Fail. 6, 18–26 (2018).
McAlister, F. A. et al. Association between glycated haemoglobin levels and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease: A secondary analysis of the TECOS randomized clinical trial. Eur. J. Heart Fail. 22, 2026–2034 (2020).
Lejeune, S. et al. Diabetic phenotype and prognosis of patients with heart failure and preserved ejection fraction in a real life cohort. Cardiovasc. Diabetol. 20, 48 (2021).
Zhang, X. et al. WATCH-DM risk score predicts the prognosis of diabetic phenotype patients with heart failure and preserved ejection fraction. Int. J. Cardiol. 385, 34–40 (2023).
Maeda, D. et al. Blood pressure in heart failure management and prevention. Hypertens. Res. 46, 817–833 (2023).
Tsimploulis, A. et al. Systolic blood pressure and outcomes in patients with heart failure with preserved ejection fraction. JAMA Cardiol. 3, 288–297 (2018).
Selvaraj, S. et al. Systolic blood pressure in heart failure with preserved ejection fraction treated with sacubitril/valsartan. J. Am. Coll. Cardiol. 75, 1644–1656 (2020).
Haass, M. et al. Body mass index and adverse cardiovascular outcomes in heart failure patients with preserved ejection fraction: Results from the Irbesartan in Heart Failure with Preserved Ejection Fraction (I-PRESERVE) trial. Circ. Heart Fail. 4, 324–331 (2011).
Li, S. et al. Association of body mass index and prognosis in patients with HFpEF: A dose-response meta-analysis. Int. J. Cardiol. 361, 40–46 (2022).
Seko, Y. et al. Association between body mass index and prognosis of patients hospitalized with heart failure. Sci. Rep. 10, 16663 (2020).
Remmelzwaal, S. et al. Natriuretic peptides for the detection of diastolic dysfunction and heart failure with preserved ejection fraction—A systematic review and meta-analysis. BMC Med. 18, 290 (2020).
Jarolim, P., White, W. B., Cannon, C. P., Gao, Q. & Morrow, D. A. Serial measurement of natriuretic peptides and cardiovascular outcomes in patients with type 2 diabetes in the EXAMINE trial. Diabetes Care. 41, 1510–1515 (2018).
Segar, M. W. et al. Incorporation of natriuretic peptides with clinical risk scores to predict heart failure among individuals with dysglycaemia. Eur. J. Heart Fail. 24, 169–180 (2022).
Berg, D. D. et al. Heart failure risk stratification and efficacy of sodium-glucose cotransporter-2 inhibitors in patients with type 2 diabetes mellitus. Circulation. 140, 1569–1577 (2019).
Elharram, M. et al. Prediction of heart failure outcomes in patients with type 2 diabetes mellitus: Validation of the thrombolysis in myocardial infarction risk score for heart failure in diabetes (TRS-HFDM ) in patients in the ACCORD trial. Diabetes Obes. Metab. 23, 782–790 (2021).
Segar, M. W. et al. Validation of the WATCH-DM and TRS-HFDM risk scores to predict the risk of incident hospitalization for heart failure among adults with type 2 diabetes: A multicohort analysis. J. Am. Heart Assoc. 11, e024094 (2022).
Laaksonen, R. et al. Plasma ceramides predict cardiovascular death in patients with stable coronary artery disease and acute coronary syndromes beyond LDL-cholesterol. Eur. Heart J. 37, 1967–1976 (2016).
Meeusen, J. W. et al. Plasma ceramides. Arterioscler. Thromb. Vasc. Biol. 38, 1933–1939 (2018).
Vasile, V. C. et al. Ceramide scores predict cardiovascular risk in the community. Arterioscler. Thromb. Vasc. Biol. 41, 1558–1569 (2021).
Mandal, N. et al. Role of ceramides in the pathogenesis of diabetes mellitus and its complications. J. Diabetes Complicat. 35, 107734 (2021).
Yang, C. D. et al. Insulin resistance is associated with heart failure with recovered ejection fraction in patients without diabetes. J. Am. Heart Assoc. 11, e026184 (2022).
Gudenkauf, B. et al. Insulin resistance is associated with subclinical myocardial dysfunction and reduced functional capacity in heart failure with preserved ejection fraction. J. Cardiol. 83, 100–104 (2024).
Pearson-Stuttard, J. et al. Variations in comorbidity burden in people with type 2 diabetes over disease duration: A population-based analysis of real world evidence. EClinicalMedicine. 52, 101584 (2022).
Ziaeian, B. et al. Race/ethnic differences in outcomes among hospitalized medicare patients with heart failure and preserved ejection fraction. JACC Heart Fail. 5, 483–493 (2017).
Pandey, A. et al. Sex and race differences in lifetime risk of heart failure with preserved ejection fraction and heart failure with reduced ejection fraction. Circulation. 137, 1814–1823 (2018).
MacDonald, M. R. et al. Regional variation of mortality in heart failure with reduced and preserved ejection fraction across Asia: Outcomes in the ASIAN-HF Registry. J. Am. Heart Assoc. 9, e012199 (2020).
Kosiborod, M. N. et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N. Engl. J. Med. 389, 1069–1084 (2023).
Gamble, J. M. et al. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ. Heart Fail. 4, 317–323 (2011).
Aboumrad, M. et al. Rural-urban trends in health care utilization, treatment, and mortality among US veterans with congestive heart failure: A retrospective cohort study. J. Rural Health. 39, 844–852 (2023).
Acknowledgements
The authors thank Nagisa Yoshioka, Kyoko Tatsumi, Satomi Kishimoto, Noriko Murakami, and Sugako Mitsuoka for their excellent assistance with data collection and all PURSUIT-HFpEF study participants for their support of the present study.
Funding
This work was funded by Roche Diagnostics K.K. and Fuji Film Toyama Chemical Co. Ltd.
Author information
Authors and Affiliations
Consortia
Contributions
K.I. formulated the research question, analyzed the data, and wrote the manuscript. T.O. and A.O. formulated the research question and provided support in the data analysis. Y.K., N.T., M.O. and K.F. provided support in the data collection and contributed to the discussion. M.S., T.Y., M.Y., T.H., A.N., Y.Y., Y.N. and S.T. provided support in the data collection as investigators of PURSUIT-HFpEF. Y.S., S.H. and D.N. collected long-term follow-up data as main investigators of PURSUIT-HFpEF and reviewed and edited the manuscript. Y.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
KI received honoraria from AstraZeneca, Eli Lilly, Boehringer Ingelheim and Ono Pharmacy. NT received an honorarium from AstraZeneca. SH received research support from Roche Diagnostics, Toyama Chemical, and Acterlion Pharmaceutical and honoraria from Daiichi Sankyo Company, Bayer, Astellas Pharma, Pfizer Pharmaceuticals, and Boehringer Ingelheim. YS received a research grant from Acterlion Pharmaceutical and honoraria from Astellas Pharma, Daiichi Sankyo Company, and Otsuka Pharmaceutical. The remaining authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iwakura, K., Onishi, T., Okamura, A. et al. The WATCH-DM risk score estimates clinical outcomes in type 2 diabetic patients with heart failure with preserved ejection fraction. Sci Rep 14, 1746 (2024). https://doi.org/10.1038/s41598-024-52101-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52101-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.