Abstract
The development of a post-abortion family plan is an integral part of comprehensive abortion care. In spite of this, it received insufficient attention as a means of breaking the cycle of repeated abortions, unintended pregnancies, and maternal deaths resulting from abortion. Therefore, this study examined post abortion modern contraceptive utilization among Ethiopian women as well as associated factors. The study was based on secondary data analysis of the Ethiopian Demographic and Health Survey 2016 data. A total weighted sample of 1236 reproductive age women was included. A multilevel mixed-effect binary logistic regression model was fitted to identify the significant associated factors of post abortion contraceptive use. Statistical significance was determined using Adjusted Odds Ratio (AOR) with 95% confidence interval. Overall prevalence of post abortion contraceptive use was observed to be 25.6% (95% CI: 23.24, 28.12). Women's age 15–24 (AOR = 2.34; 95% CI: 1.11, 4.93), and 25–34 (AOR = 1.94; 95% CI: 1.27, 2.98), married women (AOR = 2.6; 95% CI: 1.43, 4.96), women who had 1–4 (AOR = 4.13; 95% CI: 1.79, 9.57) and ≥ 5 number of children (AOR = 8.80; 95% CI: 3.30, 13.49), Being in metropolitan region (AOR = 9.14; 95% CI: 1.79, 12.48), women being in urban area (AOR = 1.85; 95% CI: 1.32, 2.24), and community media exposure (AOR = 1.75; 95% CI: 1.11, 3.56) were associated with post abortion modern contraceptive use. Post abortion modern contraceptive use in this study was low. Women age, current marital status, number of living children, residency, community media exposure, and region were significantly associated with post abortion modern contraceptive utilization. Therefore, it is better to provide ongoing health information about post-abortion family planning and its benefits, especially for people who live in rural and small peripheral regions, and public health policymakers should take both individual and community level factors into account when designing family planning programmes.
Similar content being viewed by others
Introduction
Post-abortion care involves various medical and related interventions to address women's health care needs after spontaneous and induced abortions1,2. Among its essential elements are emergency treatment for complications and contraceptives to prevent repeat abortions due to mistimed or unplanned pregnancies2. Post-abortion contraception refers to the use of family planning methods immediately following an abortion1,2.
Family planning services play a crucial role in reducing unmet family planning needs, increasing contraceptive usage, and preventing unintended pregnancy and unsafe abortion3. In addition it was investigated that there was appositive effects using ENG implants on improving quality of life, sexual function, and relief pelvic pain in women affected by endometriosis like ovarian cysts4,5. Positive changes in quality of life and sexual function were observed in postpartum women who used LNG-IUS6.
Globally, an estimated 121 million women experience unintended pregnancies each year, with 73.3 million women undergoing an abortion7. The majority of abortions occur in countries with low- and middle-incomes, and sub-Saharan Africa has a 27 abortion rate per 1000 women between 15 and 49 years8. Ethiopia is one of the countries with the highest number of abortions in sub-Saharan Africa, with 382,500 abortions annually9. Abortion has a direct contribution of 810 maternal deaths8,10. The number of deaths from unsafe abortion is also disproportionately high among women in sub-Saharan Africa, with 520 deaths per 100,000 women per year7.
To improve maternal health, the World Health Organization (WHO) recommends waiting six months to get pregnant after an abortion induced or spontaneous happened is important for maternal and child health11. By linking abortion care with family planning services, unmet need and subsequent unintended pregnancies are reduced12. According to studies conducted in Ethiopia, the prevalence of post-abortion family planning utilization varies greatly across the country, ranging from 45.8 to 91%13,14,15,16,17.
Several factors influence women's decisions to begin post-abortion family planning. According to studies conducted in Ethiopia, urban residence, higher maternal education level, occupation, undergoing spontaneous abortion, receiving post abortion family planning counseling, good knowledge of family planning, and availability of family planning are all significantly associated with post-abortion family planning uptake18,19,20,21,22.
In Ethiopia, a variety of strategies have been employed to increase the uptake of contraceptive methods over the last decade. Among the steps taken to increase contraceptive use was the implementation of health extension programs to change attitudes and improve awareness among the community23,24. Family planning as part of comprehensive package of post abortion care25 that is an important strategy to reduce maternal morbidity and mortality26 by breaking the cycle of repeated abortion and unintended pregnancy27. In spite of these efforts made at the national level, the proportion of women who use contraceptive methods remains low28.
We aimed therefore, to find out the prevalence and what factors are associated with the use of post-abortion modern contraception among Ethiopian women of reproductive age. It is hoped that the study's findings will assist policymakers in developing interventions that will help reduce maternal mortality and morbidity by increasing the use of post abortion modern contraceptives.
Methods
Study design, period, and setting
The study was a multilevel analysis of data from recent EDHS, which was conducted by the Central Statistical Agency (CSA) in collaboration with the Federal Ministry of Health (FMoH) and the Ethiopian Public Health Institute (EPHI), which was a national representative sample conducted from January 18 to June 27, 201629.
There are nine regional states in Ethiopia (Tigray, Afar, Amhara, Oromia, Benishangul, Gambela, South Nation, Nationalities and Peoples’ Region (SNNPR), Harari, and Somali), and two administrative cities (Addis Ababa and Dire-Dawa), 611 Districts, and 15,000 Kebeles.
Data sources
The data were gained from the official database of the EDHS program, https://www.measuredhs.com after authorization was granted via online request by explaining the purpose of our study. We extracted dependent and independent variables from the woman record (IR file). EDHS is a nationally representative household survey conducted by face-to-face interviews on a wide range of populations. Study participants were selected using a two-stage stratified sampling technique. Enumeration Areas (EAs) were randomly selected in the first stage, while households were selected in the second stage30. A total of weighted sample of 1236 post aborted reproductive age women were included.
Variables and measurements
Dependent variable
The outcome variable was post-abortion modern contraceptive utilization. In the current study a woman was considered as modern contraceptive method utilizer if she had been using at least one of the modern contraceptives (female sterilization, male sterilization, IUCD, injectable, implants, pills, male condom, female condom, emergency contraception, and standard days method) during EDHS data collection period. Whereas a woman was considered to be non-utilizer of the modern contraceptive method if she had been using traditional methods like rhythm method, and withdrawal or if she had not been using any type of contraception during EDHS data collection period31.
Independent variables
Individual level variables
Age of respondents, educational status of respondents, current marital status, occupation of respondents, wealth index, media exposure, number of living children, visit health facility in the last 12 months, and religion were included.
Community level variables
Community level variables included residences and region was directly accessed from EDHS data sets. However, community level poverty, community level education, and community-level media exposure were constructed by aggregating individual-level characteristics at the cluster level32. They were categorized as high or low based on the distribution of the proportion values generated for each community after checking the distribution by using the histogram. The aggregate variable was not normally distributed and the median value was used as a cut-off point for the categorization32,33. Due to the non-normal distribution, we used the national median value to categorize these factors into high and low at community level. Poverty at the community level is calculated based on the proportion of households in the poorer and poorest quintiles. The proportion from a given community is grouped as low if it is less than 50% and as high if it is more than 50%. Community media exposure was categorized as low if the proportion of women exposed to media in the community was 0–26.8% and categorized as high if the proportion above 26.8%.
Data analysis
For data analysis Stata version 16 software was used. To ensure the representativeness of the EDHS sample and obtain reliable estimations and standard errors, data were weighted (v005/1000000) throughout analysis.
Four models fitted: the null model with no explanatory variables, model I with individual factors, model II with community factors, and model III with both individual and community factors. To compare and assess the fitness of nested models, we used the intra class correlation coefficient (ICC), the median odds ratio (MOR), and deviation (−2LLR). Model III was the best-fitting model due to its low deviance. In multivariable analysis, variables with a p-value less than 0.2 in bivariable analysis were used. Finally, in the multivariable analysis, adjusted odds ratios with 95% confidence intervals and p-values less than 0.05 were used to identify factors of post abortion modern contraceptive utilization.
Ethical approval and consent to participate
The study does not involve participants to provide information. Consent to participants is not applicable since the data is secondary and is available in the public domain. All the methods were conducted according to the Helsinki declarations. More details regarding EDHS data and ethical standards are available online at (http://www.dhsprogram.com). The study is not experimental study. Further explanation of how the DHS uses data and its ethical standards can be found at: http://goo.gl/ny8T6X.
Results
Individual level factors
Out of the total respondents, 759 (61.39%) women were not attended formal education, 686 (55.46%) of respondents were employed, and 694 (56.15%) of the respondents had no media exposure about family planning. Among the participants, 683 (55.25%) had 1–4 number of alive children. Among the respondents 1064 (86.32%) were married. With regard to their economic status, 451 (36.50%) women were from the poor wealth quintiles (Table 1).
Community level factors
Of the respondents 976 (79.01%) were rural dwellers. Among the respondents 1081 (87.50%) were from large central region. About 736 (59.63%) of the respondents were from communities with low proportion of poverty level. Above half (52.41%) of women had media exposure and 94.41% of the respondents were in communities with low community education level (Table 2).
Post-abortion modern contraceptive utilization
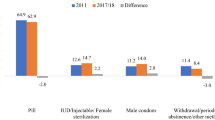
Overall, the prevalence of post abortion modern contraceptive utilization in Ethiopia was 25.60% (95% CI: 23.24, 28.12), with metropolitan region recording the highest prevalence of 32.84% (Fig. 1).
Factors associated with post-abortion modern contraceptive utilization
Study participants aged 15–24 years were 2.34 times more likely to use post abortion modern contraceptive (AOR = 2.34; 95% CI: 1.11, 4.93) as compared with those aged 35–49 years and the odds ratios of using post abortion modern contraceptive among aborted women in the age group of 25–34 were 1.94 times higher (AOR = 1.94; 95% CI: 1.27, 2.98) than those aged 35–49 years. Married participants were 2.6 times more likely to use post abortion modern contraceptive than unmarried participants with (AOR = 2.6; 95% CI: 1.43, 4.96).
Women who had 1–4 number of living children were 4.13 times modern contraceptive use (AOR = 4.13; 95% CI: 1.79, 9.57) than who had no children and women who had ≥ 5 living children were more likely to use modern contraceptive (AOR = 8.80 ; 95% CI: 3.30, 13.49) compared to women who had no living children.
Regarding community level factors, the odds of post abortion modern contraceptive utilization was high among women who had community media exposure (AOR = 1.75; 95% CI: 1.11, 3.56) compared with their counterparts. Women who were residing in urban area were 1.85 times contraceptive use than living in rural area (AOR = 1.85; 95% CI: 1.32, 2.24).
In addition, women in metropolitan region were 9.14 times more likely (AOR = 9.14; 95% CI: 1.79, 12.48) to use modern contraceptive compared to women in small peripheral region and women in large central region were 4.77 times more likely (AOR = 4.77; 95% CI: 1.18, 9.25) to use modern contraceptive compared to women in small peripheral region (Table 3).
Discussion
The actual clinical implication of low post-abortion modern contraceptive utilization is considered one of the main and leading reasons of induced abortion, spontaneous abortion, or stillbirth because the majority of post-abortion women are almost immediately at risk for pregnancy. Therefore, aim of this study was to investigate the prevalence and predictors of post abortion modern contraceptive utilization among reproductive age women in Ethiopia. Only one forth 25.6% (95% CI: 23.24, 28.12) of participants were using post abortion modern contraceptive. This finding is lower than studies conducted in Ethiopia14,17,19,34,35,36,37, and other countries such as Mexico38, Nepal39, and Pakistan40. Socioeconomic status, the proportion of married women, research sites, periods, sample sizes, counseling, the accessibility of contraceptives, participant misconceptions about family planning methods, and social norms may all contribute to these disparities.
Being 15–24 and 25–34 years were 2.34 and 1.94 times more likely to utilize post abortion contraceptive than their counterparts respectively. This finding is supported by the study conducted in Gambella41 and Bahir Dar35. This implies that the government should prioritize meeting the family planning needs of those groups in order to avoid early pregnancy and childbirth-related complications41,42. This study pointed out that married women were 2.6 times more likely to utilize post abortion contraceptives than their counterparts. This is supported by studies conducted in a different part of Ethiopia42,43,44. One possible explanation is that married women live with their husbands, making them more prone to sexual exposure.
The use of post abortion modern contraceptive methods was independently associated with the number of children. In comparison to a woman who had no children, women who had 1–4 children and women who had five and above children were four and nearly nine times more likely respectively, to have used post abortion modern contraception. Additionally, prior studies have shown that using modern contraceptives is more likely when there is adequate number of living children29,45,46. This could be because women without children may require children in order to have the optimal number of children47.
In regard to community level factors, urban women of reproductive age were about1.85 times more likely than rural women to use post abortion contraceptives. This finding is in line with secondary data analysis of Indian, Afghan, Nigerian, and Bangladeshi Demographic and Health Surveys, which showed that urban resident women were more likely than rural resident women to use contemporary contraceptives48,49,50,51. This could be caused by a variety of factors. Urban women tend to be more educated, earn more money, have better access to health facilities, and have better media access than rural women, all of which lead to higher modern contraceptive utilization rates. A number of rural women also depend on children to assist them in field work, which negatively impacts the use of modern contraceptives among them31,52,53,54,55,56.
Women who were exposed to the community media had a higher likelihood of using modern methods of contraception than women who were not. The finding is in line with the results29,48,57,58,59. This is due to the possibility that exposure to mass media could play a significant role in raising awareness and inspiring women to take contemporary contraceptive. In addition woman living in metropolitan region and large central of Ethiopia were 9 and 4.77 times more likely to use post abortion modern contraceptive compared to women in small peripheral region. There may be differences in access to health information and different availability of maternal health services, such as family planning60.
This study used most recent nationally representative data, which were collected with validated and standardized data collection tools. This also employed multilevel analysis (advanced model) that accounts the correlated nature of EDHS data in the determination of the estimate. Despite the above advantages, the cross sectional nature of the study does not show the cause and effect relationship between the outcome and the independent factors. Moreover, due to EDHS were secondary data, essential factors like attitude and knowledge about contraceptives, partner’s perspectives on contraceptives, and fear of side effects were not available in the EDHS.
Conclusion
Post-abortion modern contraceptives utilization in Ethiopia was low. Women age, current marital status, number of living children, residency, community media exposure, and region were significantly associated with post abortion modern contraceptive utilization. Therefore, it is better to provide ongoing health information about post-abortion family planning and its benefits, especially for people who live in rural and small peripheral regions, and public health policymakers should take both individual and community level factors into account when designing family planning programmes.
Data availability
Data for this study were sourced from Ethiopian Demographic and Health surveys (EDHS), which is freely available online at (https://dhsprogram.com).
References
WH Organization. Handbook on Health Inequality Monitoring: With a Special Focus on Low-and Middle-Income Countries. (World Health Organization, 2013).
WH Organization. WHO Recommendations for Augmentation of Labour. (World Health Organization, 2014).
Huber, D., Curtis, C., Irani, L., Pappa, S. & Arrington, L. Postabortion care: 20 years of strong evidence on emergency treatment, family planning, and other programming components. Glob. Health Sci. Pract. 4(3), 481–494 (2016).
Yisa, S. B., Okenwa, A. A. & Husemeyer, R. P. Treatment of pelvic endometriosis with etonogestrel subdermal implant (Implanon®). BMJ Sex. Reprod. Health. 31(1), 67–70 (2005).
Walch, K. et al. Implanon® versus medroxyprogesterone acetate: Effects on pain scores in patients with symptomatic endometriosis—A pilot study. Contraception 79(1), 29–34 (2009).
Caruso, S. et al. Sexual function and quality of life of women adopting the levonorgestrel-releasing intrauterine system (LNG-IUS 1.35 mg) after abortion for unintended pregnancy. Eur. J. Contracept. Reprod. Health Care. 23(1), 24–31 (2018).
Kumar, M. et al. Now is the time: A call for increased access to contraception and safe abortion care during the COVID-19 pandemic. BMJ Glob. Health 5(7), e003175 (2020).
Bearak, J. et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: Estimates from a comprehensive model for 1990–2019. Lancet Glob. Health 8(9), e1152–e1161 (2020).
Assefa, E. M. Knowledge, attitude and practice (KAP) of health providers towards safe abortion provision in Addis Ababa health centers. BMC Womens Health 19(1), 1–10 (2019).
Rahman, M. A., Halder, H. R. & Islam, S. M. S. Effects of COVID-19 on maternal institutional delivery: Fear of a rise in maternal mortality. J. Glob. Health. 2021, 11 (2021).
WH Organization. International Travel and Health: Situation as on 1 January 2007 (World Health Organization, 2007).
Ceylan, A., Ertem, M., Saka, G. & Akdeniz, N. Post abortion family planning counseling as a tool to increase contraception use. BMC Public Health 9(1), 1–7 (2009).
Abate, E., Smith, Y. R., Kindie, W., Girma, A. & Girma, Y. Prevalence and determinants of post-abortion family planning utilization in a tertiary Hospital of Northwest Ethiopia: A cross sectional study. Contracept. Reprod. Med. 5(1), 1–6 (2020).
Asrat, M., Bekele, D. & Rominski, S. D. Post-abortion contraceptive acceptance and choice among women receiving abortion care at Saint Paul’s Hospital, Addis Ababa, Ethiopia: A cross-sectional study. Lancet Glob. Health 6, S37 (2018).
Baynes, C., Yegon, E., Lusiola, G., Achola, J. & Kahando, R. Post-abortion fertility desires, contraceptive uptake and unmet need for family planning: Voices of post-abortion care clients in Tanzania. J. Biosoc. Sci. 53(6), 908–923 (2021).
Muche, A., Bewket, B., Ayalew, E. & Demeke, E. Utilization of post abortal contraceptive use and associated factors among women who came for abortion service at Debre Berhan Hospital, Debre Berhan, Ethiopia March 2019: institution based cross sectional study. Clin. J. Obstet. Gynecol. 2(1), 025–033 (2019).
Muchie, A., Getahun, F. A., Bekele, Y. A., Samual, T. & Shibabaw, T. Magnitudes of post-abortion family planning utilization and associated factors among women who seek abortion service in Bahir Dar Town health facilities, Northwest Ethiopia, facility-based cross-sectional study. PLoS ONE 16(1), e0244808 (2021).
Kokeb, L., Admassu, E., Kassa, H. & Seyoum, T. Utilization of post abortion contraceptive and associated factors among women who came for abortion service: a hospital based cross sectional study. J. Fam. Med. Dis. Prev. 1(10.23937), 2469–5793 (2015).
Prata, N., Bell, S., Holston, M., Gerdts, C. & Melkamu, Y. Factors associated with choice of post-abortion contraception in Addis Ababa, Ethiopia. Afr. J. Reprod. Health 15(3), 55–62 (2011).
Amentie, M., Abera, M. & Abdulahi, M. Utilization of family planning services and influencing factors among women of child bearing age in Assosa district, Benishangul Gumuz regional state, West Ethiopia. Sci. J. Clin. Med. 4(3), 52 (2015).
Zemene, A., Feleke, A., Alemu, A., Yitayih, G. & Fantahun, A. Factors influencing utilization of post abortion care in selected Governmental Health Institutions, Addis Ababa. Ethiopia. Fam Med Med Sci Res. 3(115), 2327–72.100015 (2014).
Dejenie Seyoum, A.G., & Gizaw, Z. Assessment of Post Abortion Contraceptive Intention and Associated Factors Among Abortion Clients in Gondar Town, North West Ethiopia, 2013 (2014).
Sedlander, E. et al. Understanding modern contraception uptake in one Ethiopian community: A case study. Reprod. Health 15(1), 1–8 (2018).
Kahsay, Z. H., Hiluf, M. K., Shamie, R., Tadesse, Y. & Bazzano, A. N. Pregnant Women’s intentions to deliver at a health Facility in the Pastoralist Communities of Afar, Ethiopia: An application of the health belief model. Int. J. Environ. Res. Public Health 16(5), 888 (2019).
Tripney, J., Kwan, I. & Bird, K. S. Postabortion family planning counseling and services for women in low-income countries: A systematic review. Contraception 87(1), 17–25 (2013).
Opoku, B. Contraceptive preferences of post-abortion patients in Ghana. J. Women’s Health Care. 1(2), 2167–2420 (2012).
Seid, A., Gebremariam, A. & Abera, M. Integration of family planning services within post abortion care at health facilities in dessie—North East Ethiopia. Sci. Technol. Arts Res. J. 1(1), 38–46 (2012).
Fantay Gebru, K., Mekonnen Haileselassie, W., Haftom Temesgen, A., Oumer Seid, A. & Afework, M. B. Determinants of stunting among under-five children in Ethiopia: a multilevel mixed-effects analysis of 2016 Ethiopian demographic and health survey data. BMC Pediatr. 19(1), 1–13 (2019).
Abate, M. G. & Tareke, A. A. Individual and community level associates of contraceptive use in Ethiopia: A multilevel mixed effects analysis. Arch. Public Health 77(1), 1–12 (2019).
Corsi, D. J., Neuman, M., Finlay, J. E. & Subramanian, S. Demographic and health surveys: A profile. Int. J. Epidemiol. 41(6), 1602–1613 (2012).
Gebre, M. N. & Edossa, Z. K. Modern contraceptive utilization and associated factors among reproductive-age women in Ethiopia: Evidence from 2016 Ethiopia demographic and health survey. BMC Womens Health 20(1), 1–14 (2020).
Liyew, A. M. & Teshale, A. B. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016; A multilevel analysis. BMC Public Health 20(1), 1–11 (2020).
Getaneh, T., Negesse, A., Dessie, G., Desta, M. & Moltot, T. Predictors of unmet need for family planning in Ethiopia 2019: A systematic review and meta analysis. Arch. Public Health. 78(1), 1–11 (2020).
Abebe, A. M., Wudu Kassaw, M. & Estifanos, S. N. Postabortion contraception acceptance and associated factors in Dessie Health Center and Marie Stopes International Clinics, South Wollo Northeast, Amhara region, 2017. Int. J. Reprod. Med. 2019, 1327351 (2019).
Mekuria, A., Gutema, H., Wondiye, H. & Abera, M. Postabortion contraceptive use in Bahir Dar, Ethiopia: A cross sectional study. Contracept. Reprod. Med. 4(1), 1–6 (2019).
Tesfaye, G. & Oljira, L. Post abortion care quality status in health facilities of Guraghe zone, Ethiopia. Reprod. Health 10(1), 1–7 (2013).
Chukwumalu, K., Gallagher, M. C., Baunach, S. & Cannon, A. Uptake of postabortion care services and acceptance of postabortion contraception in Puntland, Somalia. Reprod. Health Matters 25(51), 48–57 (2017).
Becker, D., Olavarrieta, C. D., Garcia, S. G. & Harper, C. C. Women’s reports on postabortion family-planning services provided by the public-sector legal abortion program in Mexico City. Int. J. Gynecol. Obstet. 121(2), 149–153 (2013).
Khanal, V., Joshi, C., Neupane, D. & Karkee, R. Practices and perceptions on contraception acceptance among clients availing safe abortion services in Nepal. Kathmandu Univ. Med. J. 9(3), 179–184 (2011).
Azmat, S. K., Hameed, W., Ishaque, M., Mustafa, G. & Ahmed, A. Post-abortion care family planning use in Pakistan. Pak. J. Public Health. 2(2), 4 (2012).
Abamecha, A., Shiferaw, A. & Kassaye, A. Assessment of Post Abortion Contraceptive Intention and Associated Factors Among Abortion Clients in Gambella Health Facilities, Gambella Town, South West Ethiopia. Gambella Town, South West Ethiopia (2016).
Motuma, V. S. et al. Postabortion family planning and associated factors among women attending abortion service in Dire Dawa Town Health Facilities, Eastern Ethiopia. Front. Reprod. Health. 4, 860514 (2022).
Bizuneh, A. D. & Azeze, G. G. Post-abortion family planning use, method preference, and its determinant factors in Eastern Africa: A systematic review and meta-analysis. Syst. Rev. 10(1), 1–14 (2021).
Moges, Y., Hailu, T., Dimtsu, B., Yohannes, Z. & Kelkay, B. Factors associated with uptake of post-abortion family planning in Shire town, Tigray, Ethiopia. BMC Res. Notes 11(1), 1–6 (2018).
Idris, H. Factors affecting the use of contraceptive in Indonesia: Analysis from the National Socioeconomic Survey (Susenas). KEMAS J. Kesehatan Masyarakat. 15(1), 117–123 (2019).
Devita, V. D., Rosliza, A. & Suriani, I. Prevalence of modern contraceptive use among reproductive women with hypertension and diabetes in a government hospital in BATAM, Indonesia and its socio-demographic determinants. Int. J. Public Health Clin. Sci. 5(4), 297–378 (2018).
Naigino, R. et al. HIV status disclosure and associated outcomes among pregnant women enrolled in antiretroviral therapy in Uganda: A mixed methods study. Reprod. Health 14(1), 1–11 (2017).
Fenta, S. M. & Gebremichael, S. G. Predictors of modern contraceptive usage among sexually active rural women in Ethiopia: A multi-level analysis. Arch. Public Health. 79(1), 1–10 (2021).
Ezeh, O. K., Agho, K. E., Dibley, M. J., Hall, J. & Page, A. N. The impact of water and sanitation on childhood mortality in Nigeria: Evidence from demographic and health surveys, 2003–2013. Int. J. Environ. Res. Public Health 11(9), 9256–9272 (2014).
Haq, I., Sakib, S. & Talukder, A. Sociodemographic factors on contraceptive use among ever-married women of reproductive age: Evidence from three demographic and health surveys in Bangladesh. Med. Sci. 5(4), 31 (2017).
Dey, A. K. Socio-demographic determinants and modern family planning usage pattern—An analysis of National Family Health Survey-IV data. Int. J. Commun. Med. Public Health 6(2), 738 (2019).
Tekelab, T., Melka, A. S. & Wirtu, D. Predictors of modern contraceptive methods use among married women of reproductive age groups in Western Ethiopia: A community based cross-sectional study. BMC Womens Health 15(1), 1–8 (2015).
Johnson, O. E. Determinants of modern contraceptive uptake among Nigerian women: Evidence from the national demographic and health survey. Afr. J. Reprod. Health 21(3), 89–95 (2017).
Osmani, A. K., Reyer, J. A., Osmani, A. R. & Hamajima, N. Factors influencing contraceptive use among women in Afghanistan: secondary analysis of Afghanistan Health Survey 2012. Nagoya J. Med. Sci. 77(4), 551 (2015).
Adebowale, A. S., Gbadebo, B. & Afolabi, F. R. Wealth index, empowerment and modern contraceptive use among married women in Nigeria: Are they interrelated?. J. Public Health 24(5), 415–426 (2016).
Adebowale, S. A., Adedini, S. A., Ibisomi, L. D. & Palamuleni, M. E. Differential effect of wealth quintile on modern contraceptive use and fertility: Evidence from Malawian women. BMC Womens Health 14(1), 1–13 (2014).
Agbadi, P., Tagoe, E., Akosua, A.F. & Owusu, S. A Multilevel Analysis of Predictors of Modern Contraceptive Use Among Reproductive Age Women in Sierra Leone: Insight from Demographic and Health Surveys. (Center for Open Science, 2019).
Rutaremwa, G. et al. Predictors of modern contraceptive use during the postpartum period among women in Uganda: A population-based cross sectional study. BMC Public Health 15(1), 1–9 (2015).
Nsanya, M. K., Atchison, C. J., Bottomley, C., Doyle, A. M. & Kapiga, S. H. Modern contraceptive use among sexually active women aged 15–19 years in North-Western Tanzania: Results from the Adolescent 360 (A360) baseline survey. BMJ Open 9(8), e030485 (2019).
Ababa A. Ethiopia. Abstract. https://wfpha.confex.com/wfpha/2012/webprogram.Paper10587html[GoogleScholar] (2013).
Acknowledgements
We are grateful to the EDHS programs, for the permission to use all the relevant EDHS data for this study.
Author information
Authors and Affiliations
Contributions
T.B.B. conceived the idea for this study, involved in the data extraction, analysis, interpretation of the finding and writing the original draft. S.M.F., E.A.F., B.A., T.A.B., and A.A.K. assisted in the analysis of the study. A.E., A.F.Z., T.T.T., S.M.W., D.B.A., and W.D.N. writing the review and editing the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Belachew, T.B., Negash, W.D., Asmamaw, D.B. et al. Prevalence and predictors of post-abortion modern contraceptive utilization among reproductive age women in Ethiopia. Sci Rep 13, 15932 (2023). https://doi.org/10.1038/s41598-023-42911-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42911-7
This article is cited by
-
Factors associated with modern contraceptive utilization among reproductive age women in Kenya; evidenced by the 2022 Kenyan demographic and health survey
Contraception and Reproductive Medicine (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.