Abstract
Helicobacter pylori (H. pylori) screening and treatment is recommended for patients on chronic aspirin (ASA) therapy to reduce the risk of gastrointestinal bleeding. Coronary artery disease patients requiring combination antithrombotic therapy (dual antiplatelet therapy; DAPT, or dual pathway inhibition; DPI) are at an even higher risk of GI bleeding. Therefore, we aimed to evaluate the prevalence of H. pylori among patients referred for angiography and likely to receive DAPT or DPI. This single-center prospective observational study recruited patients undergoing coronary angiography and with the possibility of requiring DAPT or DPI. All included patients underwent H. pylori serology testing. Multivariable logistic regression was performed to determine predictors of seropositivity. 195 patients were included in the analysis. Mean age was 67 years, 50% had known prior CAD, and 49% underwent coronary intervention. H. pylori serology was positive in 36%. Chronic kidney disease (odds ratio [OR] 2.76; 95% confidence interval [CI] 1.24 to 6.15; p = 0.01) and chronic obstructive pulmonary disease (OR 2.52; 95% CI 1.14 to 5.55; p = 0.02) history were independent predictors of H. pylori seropositivity. Given the clinically significant prevalence of H. pylori seropositivity among patients referred for angiography, systematic screening strategies and eradication of H. pylori could significantly reduce the incidence of GI bleeding in patients requiring DAPT or DPI.
Similar content being viewed by others
Introduction
Helicobacter pylori (H. pylori) is both the most common chronic bacterial infection in humans and a significant cause of chronic gastritis, most peptic ulcers, and gastric adenocarcinoma and lymphoma1,2. A recent systematic review of H. pylori infection showed a prevalence of 37.1% in North America3 and it has been shown to affect up to 75% of individuals in specific populations4. Moreover, H. pylori infection is one of the most common cause of peptic ulcer disease5. Fortunately, eradication of H. pylori prevents recurrence and ulcer complications such as bleeding or perforation6.
Bleeding, most commonly gastro-intestinal (GI) bleeding7, is one of the most important adverse events associated with dual antiplatelet therapy (DAPT) and related antithrombotic regimens in patients with coronary artery disease (CAD). H. pylori infection has also been recognized as a risk factor for GI bleeding while on chronic daily ASA therapy8 and thienopyridine P2Y12-inhibitor antiplatelet therapy9. This risk is likely amplified with the use of novel, more potent P2Y12-inhibitor-based DAPT or when antiplatelet therapy must be combined with oral anticoagulation (dual-pathway inhibition; DPI). Some studies have also suggested that prolonged DAPT should be considered following acute coronary syndrome (ACS) for up to three years10,11, prolonging the period at increased of GI bleeding. The 2017 American College of Gastroenterology (ACG) guidelines recommend testing for H. pylori infection to reduce the risk of ulcer-related bleeding for those on chronic ASA therapy12. Despite this, such a strategy is still not common practice in those on antiplatelet monotherapy. Moreover, to our knowledge, systematic screening for H. pylori has not been prospectively evaluated for CAD patients receiving DAPT or DPI, who might derive even greater benefit from eradication therapy. In this study, we aimed to report the prevalence of positive H. pylori serology in an unselected population referred for coronary angiography and likely to required DAPT or DPI, as well as to determine clinical predictors of seropositivity.
Methods
Study design and setting
The HP-DAPT prevalence study was a single-center prospective observational study conducted at the Centre hospitalier de l’Université de Montréal (CHUM), a Canadian academic tertiary care center, between November 2018 and August 2019. Adult patients undergoing coronary angiography with the possibility of requiring DAPT or DPI afterwards were eligible for inclusion in this study, without restriction with regards to the acuity of the clinical presentation (unstable angina, NSTEMI, STEMI, and elective procedures included). Patients without the possibility of requiring DAPT or DPI post-procedure, such as those referred for diagnostic hemodynamic studies only, cardiac biopsy, or diagnostic angiography in anticipation of a surgical valve procedure, we excluded. Informed consent was obtained from all participants and all methods were carried out in accordance with the Declaration of Helsinki and its later amendments. The study protocol was approved by the institutional research ethics board of the CHUM.
Data collection, clinical endpoints and H. pylori eradication
Clinical data was abstracted from the medical record and included demographics, medical history, laboratory values, baseline medications, pre-procedure investigations, clinical presentation, coronary procedures performed and discharge medications. Available medical records for data collection included both the electronic medical record from our center, as well as any paper documentation that would have patients transferred from referring hospitals. All clinical variables were prospectively identified and defined. Blood samples for H. pylori serology testing were drawn at the time of vascular access for coronary angiography. Specific anti–H. pylori IgGs were measured by use of a commercial ELISA (H pylori IgG ELISA, Bio-Rad Platelia™). Titers were defined as positive if optical density ratio was > 1.10 according to manufacturer’s instructions.
The primary endpoint of interest was the prevalence of H. pylori seropositivity. A key secondary objective was to determine clinical predictors of H. pylori seropositivity. Patients who were found to have positive serology were informed by phone. The patient’s primary caregiver was also informed by mail after obtaining the patient’s consent to communicate the results of the serology. Patients without a primary caregiver were offered eradication therapy by the research team. Eradication therapy, whether organized by the primary caregiver or the research team, was guided by a clinical decision aid (Table 1) developed by the investigators in accordance with published guidelines13 that took into account possible drug-drug interactions with the cardiac medications prescribed, such that the eradication regimen was adapted to the patient’s prescribed cardiac regimen. The preferred cardiac management of the treating team was therefore never altered to accommodate H. pylori eradication.
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS, IBM, Version 25). Normally distributed data are presented as means ± standard deviation and categorical data as counts with percentages of the total. Continuous variables were compared using a t-test when normally distributed and categorical data with the χ2 test. The difference in medians is estimated using the Hodges-Lehmann method where appropriate. Given the exploratory nature of the analysis, a two-tailed α of 0.05 was used for all analyses. Univariate predictors of positive H. pylori serology were identified using logistic regression. A multivariate logistic regression model was created including all univariate predictors with a P value < 0.05.
Results
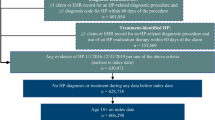
From November 2018 to August 2019 a total of 206 patients provided consent, but serology was performed in only 195 (Fig. 1). Reasons for not performing serology included failure to obtain a blood sample because coronary angiography was ultimately not performed (3 patients) and laboratory mishandling of study samples (8 patients; H. pylori serology is no longer routinely performed for patients over 65 years of age at our center and 8 samples were not recognized as being study samples). Baseline patient characteristics are presented in Table 2. The mean age was 67.3 years, and 70.8% of patients were men. The vast majority of the cohort were Caucasian (90.3%). A history of hypertension was documented in 74% and 36% had diabetes. Pre-existing CAD was noted in 50% of patients, with 31% and 19% having had previous percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), respectively. A total of 69% had a history of atherosclerotic vascular disease.
Angiographies were elective in half of patients, whereas NSTEMI was the leading cause of acute coronary syndrome presentation (Table 3). PCI was ultimately performed in 49% of patients. Slightly more than half of patients were discharged on two or more antithrombotic agents. There was no difference in the rates of antithrombotic agent class prescription at discharge between those with and without positive serology. Of note, H. pylori serology status was not known until after discharge in most cases.
Independent predictors of H. pylori seropositivity (Fig. 2) included a history of chronic kidney disease defined as an estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m2 calculated with Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (CKD; OR 2.76; 95% CI 1.24 to 6.15; p = 0.01) and chronic obstructive pulmonary disease (COPD; OR 2.52; 95% CI 1.14 to 5.55; p = 0.02). In contrast, patients with a history of dyspepsia, gastritis or esophagitis were less likely to be seropositive (OR 0.24; 95% CI 0.07 to 0.78; p = 0.02).
Predictors of H. pylori seropositivity based on multivariate analysis. COPD chronic obstructive pulmonary disease; CKD chronic kidney disease; GI gastrointestinal. A multivariate logistic regression model was created including all univariate predictors with a P value < 0.05. 95% confidence intervals are presented in this figure with the corresponding OR.
Discussion
In this first Canadian study of H. pylori prevalence among CAD patients, the rate of positive H. pylori serology was 36% in a contemporary all-comers cohort of patients with the possibility of requiring DAPT or DPI, suggesting that a significant portion of the treated CAD population in Canada is at an increase, yet modifiable risk of GI bleeding.
While H. Pylori infection prevalence varies between and within countries14, our results are consistent with previously reported Canadian data (38% seropositivity in the general population)3,15. A large Canadian multicenter study also reported an H. pylori infection prevalence of 30% using histological assessment in patients with dyspepsia16. To the best of our knowledge, ours is the first study to specifically evaluate H. pylori prevalence in a Canadian CAD population and confirms that global estimates of H. pylori prevalence likely also apply to the CAD subpopulation.
Other studies of H. pylori prevalence in CAD populations have shown a wide range of positivity rates. In the United States, a series of 890 patients undergoing coronary angiography showed a 56% prevalence of H. pylori seropositivity17, whereas, in Europe, a German study showed a 44% seropositivity rate, but a United Kingdom analysis showed 79%18,19, reinforcing that knowledge of local seropositivity rates (and antibiotic resistances) should inform clinical decision-making.
In our cohort, three clinical characteristics were found to be independent predictors of seropositivity: CKD, COPD or a history of upper GI complaints (dyspepsia, gastritis or esophagitis), with the latter being protective. However, in the H. pylori literature, the strongest predictor of H. pylori infection is low socioeconomic status (SES) and poor living conditions early in life20,21,22. Factors such as overcrowding, lack of running water and poor hygiene have been linked to a higher rate of H. pylori infection, which tends to occur mainly during childhood23. It is possible that questioning patients on SES during childhood might have revealed additional risk factors. H. pylori seropositivity also increases with age15 and ethnicity is a risk factor with blacks and Hispanics having higher rates of infection24. It may therefore be that CKD and COPD are in fact surrogates for the combined effects of childhood SES and age at the time of angiography in our cohort and not necessarily themselves on the causal pathway of H. pylori seropositivity.
The association seen between a history of upper GI complaints and seronegativity is at first glance surprising. However, while some patients will remain seropositive following successful eradication therapy, others will seroconvert over time, particularly if there is a long interval between eradication therapy and repeat serology25. Therefore, it is possible that patients with a remote history of dyspepsia, gastritis or esophagitis had previously benefit from eradication therapy in the past and subsequently lost their anti-H. pylori antibodies over time, which could explain our results. Unfortunately, data on prior eradication therapy were not collected in our study. Alternatively, it is also possible that patients with a history of upper GI complaints with or without a history of H. pylori infection might have been less likely to be referred for angiography or might have been less inclined to consent for this study. Additionally, one must consider that many patients in our cohort were referred from other centers and nearly all were referred by a cardiologist. It is therefore possible that the non-cardiovascular medical history may not have been complete in all cases. As such, a documented history of GI complaints could simply be a marker of better overall care or, possibly, better SES. In addition, while we cannot evaluate this scenario with our dataset, it is conceivable that CAD is itself a strong predictor of seroposivity, such that a history of GI complaints may not have the same predictive impact as would be expected in the general population. The apparent protective effect of this variable observed here may therefore indeed be spurious due to a so-called index event bias (also known as collider stratification bias)26,27. For all of these reasons, the effect of a history of upper GI symptoms in this population should be interpreted with great caution.
Our results are also limited by the modest sample size of our exploratory study. Approximately 3300 diagnostic or interventional coronary procedures are performed annually in our center. A larger sample size could lead to both a refinement of the estimate of seropositivity and a clearer understanding of its predictors.
H. pylori serology is an inexpensive minimally invasive test with good sensitivity, but modest specificity for active infection (it cannot differentiate between current and prior infection). Studies have shown sensitivities ranging from 76 to 84% and specificities from 79 to 90%28. As such, treating H. pylori solely based on positive serology is controversial. Either a confirmatory urea breath test or stool antigen test is usually recommended before initiating treatment to confirm active infection. However, in the case of CAD patients receiving either DAPT or DPI, such confirmatory tests may not be immediately useful, as proton pump inhibitor (PPI) therapy increases the false negative rate of both the urea breath test29,30 and the stool antigen test31. Therefore, performing these confirmatory tests requires stopping PPI therapy for two weeks, which may not be considered optimal in patients on DAPT or DPI. In our study population, the majority patients were discharged on 2 or more antithrombotic agents and the majority were co-prescribed a PPI for gastric protection. Stopping PPI therapy could therefore increase the risk of bleeding for both patients with and without H. pylori. On the other hand, treating all patients with positive H. pylori serology would be expected to expose some false-positive (for active infection) patients to an unnecessary prolonged antibiotic treatment.
Moreover, typically recommended antibiotics against H. pylori infection are not always compatible certain P2Y12-inhibitors and direct oral anticoagulants (DOACs)13. Multiple regimens include macrolides, which are not compatible with either ticagrelor or any of the DOACs. Also, bismuth subsalicylate preparations have aspirin-like properties which can increase the risk of bleeding in the presence of other antithrombotic medication and should therefore be avoided or used with caution32. Therefore, screening for H. pylori and eradication as needed should ideally be performed prior to referral for elective coronary angiography whenever feasible. When not possible, such as in the case of an acute coronary syndrome, we believe that screening for H. pylori seropositivity should be considered at the time of admission, with discussion of the pros and cons of immediate eradication treatment according to the algorithm that we have proposed (Table 1).
Conclusion
Given the clinically significant prevalence of positive H. pylori serology in this prospective Canadian cohort of patients referred for diagnostic coronary angiography, strategies of systematic screening and eradication of H. pylori could significantly reduce the incidence of GI bleeding in patients requiring DAPT or DPI. A prospective randomized clinical trial comparing either broad H. pylori screening or screening of patients with H. pylori risk factors compared to usual care is warranted.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Saleem, N. & Howden, C. W. Update on the management of helicobacter pylori infection. Curr. Treat Opt. Gastroenterol. 18(3), 476–487 (2020).
Crowe, S. E. Helicobacter pylori Infection. N. Engl. J. Med. 380(12), 1158–1165 (2019).
Hooi, J. K. Y. et al. Global prevalence of helicobacter pylori infection: Systematic review and meta-analysis. Gastroenterology 153(2), 420–429 (2017).
Cheung, J. et al. Disease manifestations of Helicobacter pylori infection in Arctic Canada: Using epidemiology to address community concerns. BMJ Open 4, e003689 (2014).
Lanas, A. & Chan, F. K. L. Peptic ulcer disease. Lancet 390(10094), 613–624 (2017).
Wang, A. Y. & Peura, D. A. The prevalence and incidence of Helicobacter pylori-associated peptic ulcer disease and upper gastrointestinal bleeding throughout the world. Gastrointest. Endosc. Clin. N. Am. 21(4), 613–635 (2011).
Grove, E. L., Würtz, S. P., Jørgensen, N. R. & Vestergaard, P. Gastrointestinal events with clopidogrel: A nationwide population-based cohort study. J. Gen. Intern. Med. 28, 216–222 (2013).
Yeomans, N. D. et al. Prevalence and incidence of gastroduodenal ulcers during treatment with vascular protective doses of aspirin. Aliment Pharmacol. Ther. 22, 795–801 (2005).
Abraham, N. S. et al. ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: A focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. Circulation 122, 2619–2633 (2010).
Mauri, L. et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N. Engl. J. Med. 371, 2155–2166 (2015).
Bonaca, M. O. et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N. Engl. J. Med. 372, 1791–1800 (2015).
Chey, W. D., Leontiadis, G. I., Howden, C. W. & Moss, S. F. ACG clinical guideline: Treatment of helicobacter pylori infection. Am. J. Gastroenterol. 112, 212–239 (2017).
Fallone, C. A. et al. The toronto consensus for the treatment of helicobacter pylori infection in adults. Gastroenterology 151(1), 51-69.e14 (2016).
Sjomina, O., Pavlova, J., Niv, Y. & Leja, M. Epidemiology of Helicobacter pylori infection. Helicobacter 23(Suppl 1), e12514 (2018).
Veldhuyzen van Zanten, S. J., Pollak, P. T., Best, L. M., Bezanson, G. S. & Marrie, T. Increasing prevalence of helicobacter pylori infection with age: Continuous risk of infection in adults rather than cohort effect. J. Infect. Dis. 169(2), 434–437 (1994).
Thomson, A. B. et al. The prevalence of clinically significant endoscopic findings in primary care patients with uninvestigated dyspepsia: the Canadian Adult Dyspepsia Empiric Treatment - Prompt Endoscopy (CADET-PE) study. Aliment Pharmacol. Ther. 17(12), 1481–1491 (2003).
Zhu, J. et al. Prospective study of pathogen burden and risk of myocardial infarction or death. Circulation 103(1), 45–51 (2001).
Koenig, W. et al. Infection with Helicobacter pylori is not a major independent risk factor for stable coronary heart disease: Lack of a role of cytotoxin-associated protein A-positive strains and absence of a systemic inflammatory response. Circulation 100(23), 2326–2331 (1999).
Whincup, P. et al. Prospective study of potentially virulent strains of Helicobacter pylori and coronary heart disease in middle-aged men. Circulation 101(14), 1647–1652 (2000).
Hunt, R. H., Sumanac, K. & Huang, J. Q. Review article: should we kill or should we save Helicobacter pylori?. Aliment Pharmacol. Ther. 15(Suppl 1), 51–59 (2001).
Webb, P. M. et al. Relation between infection with Helicobacter pylori and living conditions in childhood: Evidence for person to person transmission in early life. BMJ 308(6931), 750–753 (1994).
Kivi, M., Johansson, A. L., Reilly, M. & Tindberg, Y. Helicobacter pylori status in family members as risk factors for infection in children. Epidemiol. Infect. 133(4), 645–652 (2005).
Mendall, M. A. et al. Childhood living conditions and Helicobacter pylori seropositivity in adult life. Lancet 339(8798), 896–897 (1992).
Everhart, J. E., Kruszon-Moran, D., Perez-Perez, G. I., Tralka, T. S. & McQuillan, G. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J. Infect. Dis. 181(4), 1359–1363 (2000).
Cutler, A. F., Prasad, V. M. & Santogade, P. Four-year trends in Helicobacter pylori IgG serology following successful eradication. Am. J. Med. 105(1), 18–20 (1998).
Choi, H. K., Nguyen, U. S., Niu, J., Danaei, G. & Zhang, Y. Selection bias in rheumatic disease research. Nat. Rev. Rheumatol. 10(7), 403–412 (2014).
Dahabreh, I. J. & Kent, D. M. Index event bias as an explanation for the paradoxes of recurrence risk research. JAMA 305, 822–823 (2011).
Chey, W. D. & Wong, B. C. Practice parameters committee of the American college of gastroenterology. American college of gastroenterology guideline on the management of helicobacter pylori infection. Am. J. Gastroenterol. 102(8), 1808–1825 (2007).
Laine, L., Estrada, R., Trujillo, M., Knigge, K. & Fennerty, M. B. Effect of proton-pump inhibitor therapy on diagnostic testing for Helicobacter pylori. Ann. Intern. Med. 129(7), 547–550 (1998).
Bravo, L. E., Realpe, J. L., Campo, C., Mera, R. & Correa, P. Effects of acid suppression and bismuth medications on the performance of diagnostic tests for Helicobacter pylori infection. Am. J. Gastroenterol. 94(9), 2380–2383 (1999).
Gatta, L. et al. Effect of proton pump inhibitors and antacid therapy on 13C urea breath tests and stool test for Helicobacter pylori infection. Am. J. Gastroenterol. 99(5), 823–829 (2004).
Lexicomp. (n.d.). Bismuth subsalicylate: Drug information. UpToDate. Retrieved from 15 May 2021, from https://www.uptodate.com/contents/bismuth-subsalicylate-drug-information.
Funding
This project was supported by a research grant from AstraZeneca Canada for this specific study. The sponsor did not have access to the data or the manuscript prior to publication. Dr. Brian J. Potter is supported by a Fonds de recherche du Québec-Santé career award (267436).
Author information
Authors and Affiliations
Contributions
B.J.P., A.M., S.M. and D.B. conceived the original idea and protocol. K.H. and Y.S. carried out data collection. K.H. performed statistical analysis. J.N. and K.Huard designed eradication therapy practical guide. K.H., K.H. and B.J.P wrote the manuscript. B.J.P., A.M. and S.M. provided critical feedback.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huard, K., Haddad, K., Saada, Y. et al. Prevalence of H. pylori among patients undergoing coronary angiography (The HP-DAPT prevalence study). Sci Rep 12, 16591 (2022). https://doi.org/10.1038/s41598-022-17034-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17034-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.