Abstract
Immune checkpoint inhibitors (ICIs) such as anti-PD-L1 antibodies are widely used to treat human cancers, and growing evidence suggests that ICIs are promising treatments for canine malignancies. However, only some canine oral malignant melanoma (OMM) cases respond to ICIs. To explore biomarkers predictive of survival in dogs with pulmonary metastatic OMM receiving the anti-PD-L1 antibody c4G12 (n = 27), serum concentrations of prostaglandin E2 (PGE2), cytokines, chemokines, and growth factors were measured prior to treatment initiation. Among 12 factors tested, PGE2, interleukin (IL)-12p40, IL-8, monocyte chemotactic protein-1 (MCP-1), and stem cell factor (SCF) were higher in OMM dogs compared to healthy dogs (n = 8). Further, lower baseline serum PGE2, MCP-1, and vascular endothelial growth factor (VEGF)-A concentrations as well as higher IL-2, IL-12, and SCF concentrations predicted prolonged overall survival. These observations suggest that PGE2 confers resistance against anti-PD-L1 therapy through immunosuppression and thus is a candidate target for combination therapy. Indeed, PGE2 suppressed IL-2 and interferon (IFN)-γ production by stimulated canine peripheral blood mononuclear cells (PBMCs), while inhibition of PGE2 biosynthesis using the COX-2 inhibitor meloxicam in combination with c4G12 enhanced Th1 cytokine production by PBMCs. Thus, serum PGE2 may be predictive of c4G12 treatment response, and concomitant use of COX-2 inhibitors may enhance ICI antitumor efficacy.
Similar content being viewed by others
Introduction
Cancer has become a major cause of death in domesticated dogs due to gains in lifespan. Like human cancers, canine cancers are usually treated by surgical excision, radiation, chemotherapy, or a combination of these measures. In addition, new treatment modalities are being developed to provide better veterinary care for canines. Immunotherapy is one promising strategy because the therapeutic effect is expected to be systemic but still cancer-specific. In humans, antibodies that inhibit immune checkpoint molecules, such as programmed cell death 1 (PD-1) and PD-ligand 1 (PD-L1), have demonstrated robust antitumor efficacies with acceptable safety profiles for various cancer types1,2,3. PD-1 is an inhibitory receptor that suppresses the effector functions of activated T cells. Its ligand, PD-L1, is often overexpressed in tumor cells, suggesting that the PD-1/PD-L1 pathway is a major mechanism for immune evasion by tumors4,5. In dogs, PD-1 expression is upregulated in lymphocytes infiltrating oral malignant melanoma (OMM), and PD-L1 is detected in tumor cells of various malignant cancers including OMM and osteosarcoma6,7,8,9,10,11,12,13,14,15,16. A recently developed canine chimeric anti-PD-L1 antibody (c4G12) demonstrated promising antitumor activity in dogs with OMM and the survival benefit was strongly suggested11,16. However, the majority of dogs with OMM did not respond to c4G1216, suggesting that other factors may limit ICI efficacy. These findings emphasize the need for further study on predictive biomarkers that can distinguish the subpopulation most likely to benefit from ICI therapy. In addition, studies are required to elucidate mechanisms limiting ICI antitumor activity and thereby identify possible targets for combination therapy.
Peripheral blood or serum/plasma biomarkers are considered preferable because sampling is easy and less invasive. To date, several serum factors have been identified that are predictive of ICI benefit among human cancer patients, including C reactive protein (CRP), interleukin (IL)-6, soluble PD-L1, and various cytokines and chemokines17,18,19,20,21. We previously reported that high baseline CRP in plasma was associated with poorer overall survival (OS) in dogs with pulmonary metastatic OMM receiving c4G12 treatment16; however, the predictive values of cytokines, chemokines, and other factors have not been investigated in canine cancer. Hence, to explore additional predictive biomarkers for ICI efficacy in dogs with OMM, we first measured serum concentrations of multiple immune modulators [prostaglandin E2 (PGE2), the cytokines interferon-γ (IFN-γ), IL-2, IL-6, IL-10, IL-12p40, and tumor necrosis factor-α (TNF-α), the chemokines IL-8 and monocyte chemotactic protein 1 (MCP-1), and the growth factors nerve growth factor-β (NGF-β), stem cell factor (SCF), and vascular endothelial growth factor-A (VEGF-A)] in healthy controls and dogs with pulmonary metastatic OMM prior to c4G12 treatment. The associations of serum concentrations with OS were assessed by univariate analysis. Next, we examined the clinical relevance and functions of PGE2 in canine cancers because PGE2 is a known suppressor of T cell responses in humans through binding to E prostanoid 2 (EP2) and EP4 receptors22 and inhibitors of its biosynthetic enzyme cyclooxygenase-2 (COX-2) are available for canine diseases with well-known efficacy and safety profiles. Overexpression of COX-2 has been reported in various canine cancers including transitional cell carcinoma, squamous cell carcinoma, and mammary cancer23, and the selective COX-2 inhibitor piroxicam24 has demonstrated clinical benefit against these canine cancers25,26,27. Recent preclinical studies using mouse cancer models have demonstrated that COX inhibition enhances immunotherapeutic efficacy of anti-PD-1 therapy28,29, however, suppressive functions of PGE2 in the canine immune system and contributions to cancer immune evasion remain unclear. Therefore, to assess the potential of COX-2 inhibition plus anti-PD-L1 antibody as combination therapy, we first confirmed COX2 mRNA expression and PGE2 upregulation in canine cancers, and then examined the immunosuppressive effects of PGE2 in cultures of canine peripheral blood mononuclear cells (PBMCs). Finally, the combinational effect of the selective COX-2 inhibitor meloxicam plus anti-PD-L1 antibody was investigated in PBMCs for possible applicability to canine cancer treatment.
Materials and methods
Canine samples
Animal care and use protocols were approved by the Institutional Animal Care and Use Committee of Hokkaido University (Approval number: 15–0149). All experiments were performed in accordance with relevant guidelines and regulations of the Faculty of Veterinary Medicine, Hokkaido University, which is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. The use of animals throughout the clinical study was approved by the ethics committee, Faculty of Veterinary Medicine, Hokkaido University. The reporting of the animal experiment in this study follows the recommendations in the ARRIVE guidelines. Serum samples from pulmonary metastatic OMM dogs (stage IV as defined by TNM-based staging30, n = 27) treated with the canine chimeric anti-PD-L1 antibody c4G1211 at the Veterinary Teaching Hospital of Hokkaido University were collected at baseline (on the first day of immunotherapy). The detailed dosage and duration of c4G12 therapy and the baseline characteristics of treated dogs were described elsewhere16. Plasma samples were obtained from tumor-bearing dogs (various tumor types, n = 21) examined at the Veterinary Teaching Hospital of Hokkaido University. For healthy dog samples, serum, plasma, and heparinized whole blood were collected from clinically healthy beagles housed at the Experimental Animal Facility, Faculty of Veterinary Medicine, Hokkaido University. Blood sampling was performed without anesthesia. Before sample collection, informed consent was obtained from the dogs’ owners.
Multiplex immunoassay and enzyme-linked immunosorbent assay (ELISA)
Serum concentrations of IFN-γ, IL-2, IL-6, IL-10, IL-12/IL-23p40, TNF-α, IL-8, MCP-1, NGF-β, SCF, and VEGF-A were quantified by bead-based multiplex immunoassays using Cytokine/Chemokine/Growth Factor 11-Plex Canine ProcartaPlex Panel 1 (Thermo Fisher Scientific, Waltham, MA) and the Luminex 200 System (Luminex, Austin, Texas). Data were analyzed using Bio-Plex Manager version 6.1 (Bio-Rad, Hercules, CA). PGE2 concentrations in plasma, serum and culture supernatant were quantified using the Prostaglandin E2 Express ELISA Kit (Cayman Chemical, Ann Arbor, MI). IL-2 concentrations in culture supernatant were quantified using the Canine IL-2 DuoSet ELISA kit, and IFN-γ concentrations using the Canine IFN-γ DuoSet ELISA kit (both from R&D Systems, Minneapolis, MN). The optical density was measured using the MTP-900 microplate reader (Corona Electric, Ibaraki, Japan). A heat map showing relative serum levels of each factor was generated using Heatmapper, a web-based tool previously described by Babicki et al. (http://www.heatmapper.ca/)31. Values below the lower limit of quantification (LLOQ) are marked as missing data.
Cell culture
The canine melanoma cell lines CMeC, LMeC, CMM-1, and CMM-232,33, were cultured as described previously6. The canine osteosarcoma cell lines POS34 and HMPOS35 were cultured in RPMI 1640 medium (Sigma-Aldrich, St. Louis, MO) supplemented with 10% fetal calf serum (FCS), 2 mM L-glutamine, 200 μg/mL streptomycin, and 200 U/mL penicillin (Thermo Fisher Scientific) at 37 °C under a 5% CO2 atmosphere. Canine PBMCs were purified from heparinized blood obtained from healthy beagles by density gradient centrifugation on Percoll (GE Healthcare UK, Buckinghamshire, UK) and cultured as described previously6. PBMCs were stimulated with 5 μg/mL Staphylococcal Enterotoxin B (SEB) (Sigma-Aldrich) and 1 μg/mL anti-canine CD28 antibody (eBioscience, San Diego, CA). In some experiments, cells were co-treated with 5 μM meloxicam (Sigma-Aldrich), 2.5 μM Prostaglandin E2 (Cayman Chemical), and/or 20 μg/mL canine chimeric anti-PD-L1 antibody c4G1211 as indicated. The same concentrations of DMSO (Nacalai Tesque, Kyoto, Japan) and dog IgG (Jackson ImmunoResearch, West Grove, PA) were used as negative controls.
Reverse transcription quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from canine cancer cell lines using TRI reagent (Molecular Research Center, Cincinnati, OH) and residual genomic DNA was digested by DNase I (Thermo Fisher Scientific) treatment. cDNA was synthesized from 1 μg of RNA using PrimeScript RTase (TaKaRa, Otsu, Japan) and oligo-dT primer in the presence of 20 U RNase inhibitor (Promega, Madison, WI). For estimation of COX2 expression (GenBank accession number NM_001003354.1), qPCR was conducted in a reaction mixture including the primers 5′-AAG CTT CGA TTG ACC AGA GCA G-3′ and 5′-TCA CCA TAA AGG GCC TCC AAC-3′, 1 μL cDNA, and SYBR Premix DimerEraser (TaKaRa) using the LightCycler480 System II (Roche Diagnostics, Mannheim, Germany). HPRT1 (GenBank accession number AY283372.1) was used as an internal control gene13. Relative COX2 mRNA expression level was calculated relative to HPRT1 expression.
Statistical analysis
Paired data were compared by Wilcoxon signed rank test, unpaired data by Mann–Whitney U test, and > 2 group data by Steel–Dwass test. OS was compared between groups stratified according to the optimal cutoff value for each measured factor (high group > cutoff and low group ≤ cutoff) by Kaplan–Meier analysis. The optimal cutoff value for each factor was defined as that yielding the most significant split by log-rank test as described by Budczies et al. (Cutoff Finder)36. OS was defined as time in days from the first dose of c4G12 until death. All deaths except for one were considered tumor-related and euthanasia was performed in one dog due to disease progression16 (Supplementary Table 1). Receiver operating characteristic (ROC) curves for each serum factor were generated in relation to longer survival (OS > median) or tumor response as evidenced by diagnostic imaging16. Youden’s index was used to determine the cutoff value for calculation of sensitivity and specificity. Statistical analysis was performed using Fisher's exact test. All tests were performed using EZR statistical software37, and P < 0.05 (two-tailed) was considered statistically significant.
Results
Multiple serum factors are upregulated in dogs with pulmonary metastatic OMM
To examine whether serum levels of PGE2, various cytokines, chemokines, and growth factors are of clinical relevance in canine OMM, we first compared serum concentrations between healthy controls (n = 8) and dogs with pulmonary metastatic OMM (n = 27 among a cohort of 29 dogs16) before the first dose of c4G12 using ELISA and a bead-based immunoassay panel (Fig. 1a). The baseline characteristics of c4G12-treated dogs, treatment outcome, and serum concentration of each factor are shown in Supplementary Tables 1 and 2. Among these 12 factors tested, PGE2, IL-12p40, IL-8, MCP-1, and SCF were quantifiable in most dogs and the concentrations were significantly higher in OMM dogs than healthy control dogs (Fig. 1b). In addition, VEGF-A was measurable in 22 OMM dogs (81.5%) and five healthy dogs (62.5%), and serum concentration tended to be higher in OMM dogs (Fig. 1b). The serum concentrations of the other six measured factors were below the LLOQ in too many animals to allow statistical comparison.
Serum concentrations of several immune modulators are elevated in dogs with pulmonary metastatic oral malignant melanoma (OMM). (a) Heat map depicting the serum concentrations of each measured factor (as Z-Scores) in dogs with OMM prior to treatment (n = 27) and in healthy dogs (n = 8). Missing values (below the lower limit of quantitation [LLOQ]) are shown in dark green. (b) Comparison of serum concentration between OMM and healthy dogs. Red bars indicate the median values. Values below LLOQ are shown as open circles. Statistical analysis was performed using Mann–Whitney U test.
Baseline concentrations of serum factors are associated with overall survival in dogs with pulmonary metastatic OMM receiving anti-PD-L1 antibody therapy
To explore serum biomarkers predictive of clinical outcome among dogs with OMM receiving anti-PD-L1 therapy, the OMM group was dichotomized according to serum concentration of each factor and the OS was compared between high (> cutoff) and low (≤ cutoff) groups by Kaplan–Meier analysis. Higher serum levels of PGE2, MCP-1, and VEGF-A were associated with worse OS in animals receiving c4G12 therapy (P = 0.038, 5.7 × 10−5, and 0.014, respectively; Fig. 2). In contrast, higher serum IL-2, IL-12p40, and SCF were correlated with improved OS (P = 0.045, 0.034, and 0.012, respectively; Fig. 2). There were no significant associations between other serum factors (IFN-γ, IL-6, IL-10, TNF-α, IL-8, and NGF-β) and OS (P > 0.05, Fig. 2). To help interpret the predictive power of each serum factor, ROC analysis was performed in relation to longer survival (OS > median) or tumor response. Area under the curve (AUC), sensitivity, and specificity for each factor are shown in Tables 1 and 2. Partially consistent with the Kaplan–Meier analysis, PGE2 and IL-6 were significant predictors of longer survival (P = 0.033 and 0.031, respectively), whereas IL-2 and IL-6 predicted tumor response to c4G12 treatment (P = 0.030 and 0.013, respectively).
Baseline serum concentrations of several immune modulators are associated with overall survival (OS) in dogs with pulmonary metastatic OMM receiving c4G12 therapy. Dogs were dichotomized into subgroups based on the indicated cutoff value for (a) Prostaglandin E2 (PGE2), (b) interferon-γ (IFN-γ), (c) interleukin (IL)-2, (d) IL-6, (e) IL-10, (f) IL-12p40, (g) tumor necrosis factor-α (TNF-α), (h) IL-8, (i) monocyte chemotactic protein 1 (MCP-1), (j) nerve growth factor-β (NGF-β), (k) stem cell factor (SCF), and (l) vascular endothelial growth factor-A (VEGF-A), and Kaplan–Meier curves were constructed comparing each corresponding subgroup (high group > cutoff vs. low group ≤ cutoff). Statistical analysis was performed using log-rank test.
The COX-2/PGE2 axis is a potential immune evasion mechanism in canine cancers
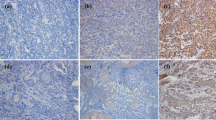
Based on the significant association between elevated serum PGE2 and shorter OS in OMM dogs receiving c4G12 therapy, we speculated that the COX-2/PGE2 pathway suppresses antitumor immunity and thus confers resistance against anti-PD-L1 therapy. Consistent with previous studies demonstrating high COX-2 expression in canine cancers including melanoma23, all canine melanoma cell lines (CMeC, LMeC, CMM-1, and CMM-2) and osteosarcoma cell lines (POS and HMPOS) examined had detectable COX2 mRNA expression (Fig. 3a). To verify that peripheral blood PGE2 levels are elevated in dogs with tumor, plasma concentration of PGE2 was measured in another cohort of dogs with various tumor (n = 21; see Supplementary Table 3 for details). Indeed, plasma PGE2 concentration was higher in tumor dogs compared to a healthy control group (n = 8; Fig. 3b), suggesting that PGE2 is generally upregulated in canine tumor, possibly through aberrant expression of COX-2 in tumor tissues.
PGE2 is a potential immunosuppressive factor in canine cancer. (a) COX2 mRNA expression in canine cancer cell lines. Total RNA was extracted from each cancer cell line and COX2 mRNA expression was measured by RT-qPCR. HPRT1 expression was used as an internal control. The mean values of triplicate measurement are shown. Error bars indicate the standard deviation (SD). (b) Plasma PGE2 concentration in dogs with tumors. Plasma samples were collected from healthy (n = 8) and tumor-bearing dogs (n = 21). Red bars indicate the median values. Statistical analysis was performed using Mann–Whitney U test. (c,d) Suppression of cytokine production from canine peripheral blood mononuclear cells (PMBCs) by PGE2. Canine PBMCs were cultured for 3 d with or without 2.5 μM PGE2, and concentrations of (c) IL-2 (n = 7) and (d) IFN-γ (n = 15) in the supernatant were measured by ELISA. Red bars indicate the median values. Statistical analysis was performed using Wilcoxon signed rank test.
To investigate the immunosuppressive potential of PGE2 in dogs, PBMCs from healthy dogs were cultured with the nonspecific T cell stimulators SEB and anti-CD28 antibody for 3 d in the presence of PGE2. PGE2 treatment significantly reduced IL-2 and IFN-γ production by stimulated canine PBMCs (Fig. 3c,d), suggesting that PGE2 is a potent suppressor of canine T cell responses.
Combined COX-2 inhibition and anti-PD-L1 antibody treatment enhances cytokine production from canine PBMCs
The selective COX-2 inhibitor meloxicam is used routinely for anti-inflammation and analgesia in veterinary practice. To assess whether PGE2 production from canine cancer cells is COX-2 dependent, the CMM-1 and HMPOS cell lines, both with relatively high baseline COX2 expression (Fig. 3a), were treated with meloxicam. PGE2 concentrations in the culture supernatant were significantly reduced after 3 d of meloxicam treatment compared to untreated control cells (Fig. 4a). In the tumor microenvironment, infiltrating immune cells can be an additional source of PGE238. Indeed, canine PBMCs stimulated in vitro with SEB and anti-CD28 antibody produced detectable amount of PGE2 that was significantly reduced by meloxicam (Fig. 4b).
The cyclooxygenase-2 (COX-2) inhibitor meloxicam reduces PGE2 production and enhances cytokine production by canine PBMCs with or without anti-programmed death ligand 1 (PD-L1) antibody treatment. (a,b) Suppression of PGE2 production by the COX-2 inhibitor meloxicam. Cells were cultured for 3 d with 5 μM meloxicam, and PGE2 concentration in the supernatant was measured by ELISA. (a) PGE2 production from canine cancer cell lines CMM-1 and HMPOS. Mean values of triplicate measurement are shown. Error bars indicate the SD. Statistical analysis was performed using Mann–Whitney U test. (b) PGE2 production from canine PBMCs (n = 7). Red bars indicate the median values. Statistical analysis was performed using Wilcoxon signed rank test. (c,d) Enhancement of cytokine production from canine PBMCs by meloxicam treatment. Canine PBMCs were cultured for 3 d with 5 μM meloxicam and/or 20 μg/mL anti-PD-L1 antibody c4G12, and (c) IL-2 (n = 11) and (d) IFN-γ (n = 15) concentrations in the supernatant were measured by ELISA. Each point represents the relative cytokine concentration compared to no treatment control prepared from the same individual. Red bars indicate the median values. Statistical analysis was performed using Steel–Dwass test (*P < 0.05).
To evaluate the immunostimulatory potential of meloxicam, PBMCs were treated with meloxicam alone or in combination with the anti-PD-L1 antibody c4G12. Both meloxicam and anti-PD-L1 antibody enhanced IL-2 production from stimulated canine PBMCs when applied individually, whereas the increase in IFN-γ production was not statistically significant. However, combination treatment further enhanced IL-2 production and significantly increased IFN-γ production (Fig. 4c,d), suggesting that dual blockade of PD-1/PD-L1 and COX-2/PGE2 pathways is a promising strategy to enhance antitumor immune responses in dogs.
Discussion
Immunotherapy is now recognized as the “fourth pillar of human cancer treatment”, with clinical importance equivalent to surgery, radiotherapy, and traditional chemotherapy. The applications of cancer immunotherapy are spreading, particularly as combination treatment, including with molecular-targeted drugs. In veterinary medicine, a few clinical studies, including from our group, have examined the efficacy of immune checkpoint blockade for dogs with cancer; however, as in human cancer2,3,39, only a subset of dogs responded well to ICI therapy11,16,40. The identification of biomarkers predictive of ICI response will not only optimize treatment efficacy but may also provide clues to the mechanisms underlying tumor immune evasion in dogs as well as humans. Indeed, dogs are an excellent animal model for human cancer research because they develop naturally occurring tumors that share many features with the corresponding human cancers, such as invasiveness and metastatic propensity, molecular aberrations, heterogeneity, and response/resistance to treatment41. As dogs are immunocompetent and genetically outbred, they could be especially useful for testing immunotherapy and precision medicine for cancers. Therefore, the identification of biomarkers and combination therapies for canine cancer may not only improve veterinary practice but also benefit human clinical oncology.
Serum PGE2, IL-12p40, IL-8, MCP-1, and SCF concentrations were higher in dogs with OMM than healthy controls, providing clues to the immunological changes associated with tumorigenesis and progression of OMM, including resistance to endogenous antitumor mechanisms. These findings are consistent with previous reports showing elevated serum IL-12p40 in osteosarcoma42, IL-8 in mammary tumor and osteosarcoma42,43,44, and MCP-1 in lymphoma, histiocytic sarcoma, urothelial carcinoma, and malignant melanoma45,46,47,48,49 compared to healthy dogs. Upregulation of these factors may reflect immunological responses in the tumor microenvironment, but the cellular and locoregional sources of these factors remain to be investigated.
Higher serum MCP-1 and VEGF-A concentrations were associated with poorer OS in OMM dogs receiving c4G12 therapy, in accordance with previous reports on human melanoma patients under ICI therapy21,50. MCP-1 is an inducible chemokine regulating macrophage infiltration into tumors51. In humans, both primary and metastatic melanomas, but not normal skin, express MCP-152, and antagonism of its receptor CCR2 enhanced the therapeutic efficacy of anti-PD-1 antibody in a murine melanoma model53. Considering the protumor propensity of tumor-associated macrophages54, it is plausible that canine OMM tissues overexpress MCP-1 and thereby attract monocytes/macrophages, which in turn create an immunosuppressive microenvironment and confer resistance to anti-PD-L1 therapy. Similarly, VEGF-A is also immunosuppressive in the tumor microenvironment55 in addition to acting as the primary driver of tumor angiogenesis. Numerous human clinical studies have revealed that anti-VEGF agents in combination with ICIs show promising efficacy against neoplasms such as renal cell carcinoma and hepatocellular carcinoma56. Although a similar immunosuppressive activity has not been demonstrated in dogs, VEGF overexpression has been demonstrated by immunohistochemistry in canine OMM57. Thus, combined VEGF targeting and ICI therapy warrants further investigation. The prolonged OS observed in OMM subgroups exhibiting high serum IL-2, IL-12p40, and SCF concentrations is also suggestive of a strong association between antitumor immune response and clinical outcome. Both IL-2 and IL-12 contribute to T cell activation, so the baseline serum concentrations of these cytokines may indicate antitumor immune status in OMM dogs. In contrast, the mechanistic implications of elevated SCF, a growth factor/cytokine involved in hematopoiesis through binding to its receptor c-Kit58, are still unclear as relevance of SCF to antitumor immunity has not been established. As a limitation of the survival analyses, only a small number of dogs (n = 27) were included, allowing only exploratory univariate analyses. Because the univariate analysis may contain multiple biases (e.g., breeds, age, and sex), the results should carefully be interpreted. Multivariate analyses of a larger cohort and validation in an independent cohort are needed to determine which of these aforementioned factors can be used as predictive biomarkers in veterinary practice. In addition, further investigation is needed to clarify whether these potential biomarkers are specific to anti-PD-L1 therapy or also applicable to other treatment modalities of canine OMM.
Prostaglandin E2 is a well-known mediator of acute local inflammation38. However, PGE2 also serves as an immunosuppressive factor in late or chronic phases by reducing T cell, NK cell, and dendritic cell functions and by promoting regulatory T cell development38. The PGE2 biosynthetic enzyme COX-2 is often upregulated in premalignant and malignant tissues59, and promotes cancer cell survival, metastasis, and angiogenesis59,60 as well as immune evasion61. Therefore, pharmacological targeting of COX-2 is considered a promising approach for cancer prevention and therapy59. Recently, crosstalk between the PD-1/PD-L1 and COX-2/PGE2 pathways was reported28,62,63. In mouse tumor models, COX inhibition by aspirin or celecoxib enhanced the efficacy of anti-PD-1 antibody28, implying that inhibition of the COX-2/PGE2 pathway could be a useful adjuvant to ICI treatment. Indeed, we previously reported that dual blockade of these pathways enhanced ICI therapeutic efficacy in cattle with bovine leukemia virus infection and in a mouse lymphoma model64,65, suggesting that this combination strategy is applicable across animal species and diseases.
To our knowledge, this is the first report to demonstrate that, in any animal species, baseline serum PGE2 concentration is associated with clinical outcome of ICI therapy and that PGE2 is a suppressor of canine immune cell activation. We also demonstrate that COX-2 inhibition plus anti-PD-L1 antibody treatment enhances immune cell activation, further supporting the potential of this combination therapy for treatment of canine cancers including OMM. Given that COX-2 overexpression is a common feature of various cancer types, that COX-2 inhibitors are already widely used in clinical practice with well-known and manageable side effects profiles, and that COX-2 activity is involved in malignant phenotype independent of immune suppression, we suggest that COX-2 inhibitors are broadly applicable, safe, and effective drugs for ICI combination therapy. Nonetheless, careful attention should be paid to possible side effects of the combination treatment. Treatment-related adverse events of c4G12 included pneumonitis, elevated liver enzymes and lipase, vomiting, and diarrhea16, while meloxicam treatment is reported to be associated with gastrointestinal (vomiting, diarrhea, and ulceration), urinary (azotemia and renal failure), hepatic (elevated liver enzymes), and dermatologic (pruritus) abnormalities66. Because gastrointestinal and hepatic toxicities are suggested for both treatments, frequency and severity of these events must be monitored in particular in future studies on the combination therapy.
In conclusion, we have identified several serum factors including PGE2 as potential predictive biomarkers of prolonged survival in dogs with OMM receiving anti-PD-L1 therapy. Further, we identified the COX-2/PGE2 axis as a potential target to enhance the efficacy of ICI therapy in dogs. The overall consistency with human biomarker analyses and preclinical studies suggests that dogs could be a clinically relevant, large animal model for ICI therapy. The clinical study of this combination therapy for canine cancer is now in progress in our veterinary hospital.
References
Brahmer, J. R. et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: Safety, clinical activity, pharmacodynamics, and immunologic correlates. J. Clin. Oncol. 28, 3167–3175 (2010).
Topalian, S. L. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 366, 2443–2454 (2012).
Brahmer, J. R. et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N. Engl. J. Med. 366, 2455–2465 (2012).
Dong, H. et al. Tumor-associated B7–H1 promotes T-cell apoptosis: A potential mechanism of immune evasion. Nat. Med. 8, 793–800 (2002).
Iwai, Y. et al. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc. Natl. Acad. Sci. USA 99, 12293–12297 (2002).
Maekawa, N. et al. Expression of PD-L1 on canine tumor cells and enhancement of IFN-γ production from tumor-infiltrating cells by PD-L1 blockade. PLoS ONE 9, e98415 (2014).
Hartley, G. et al. Immune regulation of canine tumour and macrophage PD-L1 expression. Vet. Comp. Oncol. 15, 534–549 (2017).
Shosu, K. et al. Programmed cell death ligand 1 expression in canine cancer. In Vivo 30, 195–204 (2016).
Maekawa, N. et al. Immunohistochemical analysis of PD-L1 expression in canine malignant cancers and PD-1 expression on lymphocytes in canine oral melanoma. PLoS ONE 11, e0157176 (2016).
Kumar, S. R. et al. Programmed death ligand 1 is expressed in canine B cell lymphoma and downregulated by MEK inhibitors. Vet. Comp. Oncol. 15, 1527–1536 (2017).
Maekawa, N. et al. A canine chimeric monoclonal antibody targeting PD-L1 and its clinical efficacy in canine oral malignant melanoma or undifferentiated sarcoma. Sci. Rep. 7, 8951 (2017).
Hartley, G., Elmslie, R., Dow, S. & Guth, A. Checkpoint molecule expression by B and T cell lymphomas in dogs. Vet. Comp. Oncol. 16, 352–360 (2018).
Takeuchi, H. et al. Expression analysis of canine CMTM6 and CMTM4 as potential regulators of the PD-L1 protein in canine cancers. Front. Vet. Sci. 7, 330 (2020).
Ariyarathna, H., Thomson, N. A., Aberdein, D., Perrott, M. R. & Munday, J. S. Increased programmed death ligand (PD-L1) and cytotoxic T-lymphocyte antigen-4 (CTLA-4) expression is associated with metastasis and poor prognosis in malignant canine mammary gland tumours. Vet. Immunol. Immunopathol. 230, 110142 (2020).
Cascio, M. J. et al. Canine osteosarcoma checkpoint expression correlates with metastasis and T-cell infiltrate. Vet. Immunol. Immunopathol. 232, 110169 (2021).
Maekawa, N. et al. PD-L1 immunohistochemistry for canine cancers and clinical benefit of anti-PD-L1 antibody in dogs with pulmonary metastatic oral malignant melanoma. NPJ Precis. Oncol. 5, 10 (2021).
Iivanainen, S., Ahvonen, J., Knuuttila, A., Tiainen, S. & Koivunen, J. P. Elevated CRP levels indicate poor progression-free and overall survival on cancer patients treated with PD-1 inhibitors. ESMO Open 4, e000531 (2019).
Laino, A. S. et al. Serum interleukin-6 and C-reactive protein are associated with survival in melanoma patients receiving immune checkpoint inhibition. J. Immunother. Cancer 8, e000842 (2020).
Hardy-Werbin, M. et al. Serum cytokine levels as predictive biomarkers of benefit from ipilimumab in small cell lung cancer. Oncoimmunology 8, e1593810 (2019).
Zhou, J. et al. Soluble PD-L1 as a biomarker in malignant melanoma treated with checkpoint blockade. Cancer Immunol. Res. 5, 480–492 (2017).
Lim, S. Y. et al. Circulating cytokines predict immune-related toxicity in melanoma patients receiving anti-PD-1–based immunotherapy. Clin. Cancer Res. 25, 1557–1563 (2019).
Okano, M. et al. E prostanoid 2 (EP2)/EP4-mediated suppression of antigen-specific human T-cell responses by prostaglandin E2. Immunology 118, 343–352 (2006).
Doré, M. Cyclooxygenase-2 expression in animal cancers. Vet. Pathol. 48, 254–265 (2011).
Streppa, H. K., Jones, C. J. & Budsberg, S. C. Cyclooxygenase selectivity of nonsteroidal anti-inflammatory drugs in canine blood. Am. J. Vet. Res. 63, 91–94 (2002).
Knapp, D. W., Richardson, R. C., Bottoms, G. D., Teclaw, R. & Chan, T. C. K. Phase I trial of piroxicam in 62 dogs bearing naturally occurring tumors. Cancer Chemother. Pharmacol. 29, 214–218 (1992).
Knapp, D. W. et al. Piroxicam therapy in 34 dogs with transitional cell carcinoma of the urinary bladder. J. Vet. Intern. Med. 8, 273–278 (1994).
Schmidt, B. R., Glickman, N. W., DeNicola, D. B., De Gortari, A. E. & Knapp, D. W. Evaluation of piroxicam for the treatment of oral squamous cell carcinoma in dogs. J. Am. Vet. Med. Assoc. 218, 1783–1786 (2001).
Zelenay, S. et al. Cyclooxygenase-dependent tumor growth through evasion of immunity. Cell 162, 1257–1270 (2015).
Tang, H. et al. Inhibition of COX-2 and EGFR by melafolone improves anti-PD-1 therapy through vascular normalization and PD-L1 downregulation in lung cancer. J. Pharmacol. Exp. Ther. 368, 401–413 (2019).
Goldschmidt, M. H. et al. Histological classification of epithelial and melanocytic tumors of the skin of domestic animals. in World Health Organization International Histological Classification of Tumors in Domestic Animals. III (1998).
Babicki, S. et al. Heatmapper: web-enabled heat mapping for all. Nucleic Acids Res. 44, W147–W153 (2016).
Ohashi, E. et al. Effect of retinoids on growth inhibition of two canine melanoma cell lines. J. Vet. Med. Sci. 63, 83–86 (2001).
Ohashi, E. et al. Effect of natural and synthetic retinoids on the proliferation and differentiation of three canine melanoma cell lines. J. Vet. Med. Sci. 64, 169–172 (2002).
Kadosawa, T., Nozaki, K., Sasaki, N. & Takeuchi, A. Establishment and characterization of a new cell line from a canine osteosarcoma. J. Vet. Med. Sci. 56, 1167–1169 (1994).
Barroga, E. F., Kadosawa, T., Okumura, M. & Fujinaga, T. Establishment and characterization of the growth and pulmonary metastasis of a highly lung metastasizing cell line from canine osteosarcoma in nude mice. J. Vet. Med. Sci. 61, 361–367 (1999).
Budczies, J. et al. Cutoff Finder: A comprehensive and straightforward Web application enabling rapid biomarker cutoff optimization. PLoS ONE 7, e51862 (2012).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 48, 452–458 (2013).
Kalinski, P. Regulation of immune responses by prostaglandin E2. J. Immunol. 188, 21–28 (2012).
Iwai, Y., Hamanishi, J., Chamoto, K. & Honjo, T. Cancer immunotherapies targeting the PD-1 signaling pathway. J. Biomed. Sci. 24, 26 (2017).
Igase, M. et al. A pilot clinical study of the therapeutic antibody against canine PD-1 for advanced spontaneous cancers in dogs. Sci. Rep. 10, 18311 (2020).
Gardner, H. L., Fenger, J. M. & London, C. A. Dogs as a model for cancer. Annu. Rev. Anim. Biosci. 4, 199–222 (2016).
Allende, C., Higgins, B. & Johns, J. Comparison of serum cytokine concentrations between healthy dogs and canine osteosarcoma patients at the time of diagnosis. Vet. Immunol. Immunopathol. 227, 110084 (2020).
Gelaleti, G. B., Jardim, B. V., Leonel, C., Moschetta, M. G. & de Campos-Zuccari, D. A. P. Interleukin-8 as a prognostic serum marker in canine mammary gland neoplasias. Vet. Immunol. Immunopathol. 146, 106–112 (2012).
de Andrés, P. J. et al. Increased levels of interleukins 8 and 10 as findings of canine inflammatory mammary cancer. Vet. Immunol. Immunopathol. 152, 245–251 (2013).
Perry, J. A., Thamm, D. H., Eickhoff, J., Avery, A. C. & Dow, S. W. Increased monocyte chemotactic protein-1 concentration and monocyte count independently associate with a poor prognosis in dogs with lymphoma. Vet. Comp. Oncol. 9, 55–64 (2011).
Calvalido, J. et al. Comparison of serum cytokine levels between dogs with multicentric lymphoma and healthy dogs. Vet. Immunol. Immunopathol. 182, 106–114 (2016).
Nikolic Nielsen, L., Kjelgaard-Hansen, M. & Kristensen, A. T. Monocyte chemotactic protein-1 and other inflammatory parameters in Bernese Mountain dogs with disseminated histiocytic sarcoma. Vet. J. 198, 424–428 (2013).
Shimizu, N. et al. Evaluation of urinary and serum level of chemokine (C-C motif) ligand 2 as a potential biomarker in canine urothelial tumours. Vet. Comp. Oncol. 17, 11–20 (2019).
Hutchison, S. et al. Characterization of myeloid-derived suppressor cells and cytokines GM-CSF, IL-10 and MCP-1 in dogs with malignant melanoma receiving a GD3-based immunotherapy. Vet. Immunol. Immunopathol. 216, 109912 (2019).
Khattak, M. A. et al. Role of serum vascular endothelial growth factor (VEGF) as a potential biomarker of response to immune checkpoint inhibitor therapy in advanced melanoma: Results of a pilot study. Front. Oncol. 10, 1041 (2020).
Mantovani, A. et al. Chemokines in the recruitment and shaping of the leukocyte infiltrate of tumors. Semin. Cancer Biol. 14, 155–160 (2004).
Graves, D. T., Barnhill, R., Galanopoulos, T. & Antoniades, H. N. Expression of monocyte chemotactic protein-1 in human melanoma in vivo. Am. J. Pathol. 140, 9–14 (1992).
Tu, M. M. et al. Inhibition of the CCL2 receptor, CCR2, enhances tumor response to immune checkpoint therapy. Commun. Biol. 3, 720 (2020).
Noy, R. & Pollard, J. W. Tumor-associated macrophages: From mechanisms to therapy. Immunity 41, 49–61 (2014).
Yang, J., Yan, J. & Liu, B. Targeting VEGF/VEGFR to modulate antitumor immunity. Front. Immunol. 9, 978 (2018).
Lee, W. S., Yang, H., Chon, H. J. & Kim, C. Combination of anti-angiogenic therapy and immune checkpoint blockade normalizes vascular-immune crosstalk to potentiate cancer immunity. Exp. Mol. Med. 52, 1475–1485 (2020).
Taylor, K. H. et al. Expression of vascular endothelial growth factor in canine oral malignant melanoma. Vet. Comp. Oncol. 5, 208–218 (2007).
Broudy, V. C. Stem cell factor and hematopoiesis. Blood 90, 1345–1364 (1997).
Dannenberg, A. J., Lippman, S. M., Mann, J. R., Subbaramaiah, K. & DuBois, R. N. Cyclooxygenase-2 and epidermal growth factor receptor: Pharmacologic targets for chemoprevention. J. Clin. Oncol. 23, 254–266 (2005).
Hashemi Goradel, N., Najafi, M., Salehi, E., Farhood, B. & Mortezaee, K. Cyclooxygenase-2 in cancer: A review. J. Cell. Physiol. 234, 5683–5699 (2019).
Göbel, C. et al. Functional expression cloning identifies COX-2 as a suppressor of antigen-specific cancer immunity. Cell Death Dis. 5, e1568 (2014).
Chen, J. H. et al. Prostaglandin E2 and programmed cell death 1 signaling coordinately impair CTL function and survival during chronic viral infection. Nat. Med. 21, 327–334 (2015).
Prima, V., Kaliberova, L. N., Kaliberov, S., Curiel, D. T. & Kusmartsev, S. COX2/mPGES1/PGE2 pathway regulates PD-L1 expression in tumor-associated macrophages and myeloid-derived suppressor cells. Proc. Natl. Acad. Sci. USA 114, 1117–1122 (2017).
Sajiki, Y. et al. Prostaglandin E2-induced immune exhaustion and enhancement of antiviral effects by anti-PD-L1 antibody combined with COX-2 inhibitor in bovine leukemia virus infection. J. Immunol. 203, 1313–1324 (2019).
Sajiki, Y. et al. Enhanced immunotherapeutic efficacy of anti-PD-L1 antibody in combination with an EP4 antagonist. ImmunoHorizons 4, 837–850 (2020).
Metacam (meloxicam) [package insert] (Boehringer Ingelheim Vetmedica, Inc, 2014).
Funding
This work was supported by the Grant-in-Aid for Scientific Research (Grant Numbers 16K15042, 19H03114, 19K15969, and 21K1498301) and Grant-in-aid for JSPS Fellows (Grant Number 15J01989) from the Japan Society for the Promotion of Science (JSPS) and by Japan Agency for Medical Research and Development (AMED) under Grant Number: JP21am0101078. This work was also supported by Clinical Research Promotion Fund 2020 by Hokkaido University Veterinary Teaching Hospital. Funders had no role in the study design, data collection and analysis, decision to publish, and manuscript preparation.
Author information
Authors and Affiliations
Contributions
N.M., S.K., T.O., S.M., and K.O. designed and supervised the project. N.M., Y.A., Y.S., T.D., K.W. and H.T. performed the experiments. N.M., S.K., Y.A., and Y.S. analyzed the data. T.D., S.T., K.H., S.K., H.O., Y.K., and Y.S. provided materials, reagents and/or analysis tools. N.M., S.K., and Y.A. prepared the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
S Konnai, KO, SM, TO, NM, and Y Suzuki are authors of a patent application that covers materials and techniques described in this paper (PCT/JP2018/27041). All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maekawa, N., Konnai, S., Asano, Y. et al. Exploration of serum biomarkers in dogs with malignant melanoma receiving anti-PD-L1 therapy and potential of COX-2 inhibition for combination therapy. Sci Rep 12, 9265 (2022). https://doi.org/10.1038/s41598-022-13484-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-13484-8
This article is cited by
-
Identification of ONECUT3 as a stemness-related transcription factor regulating NK cell-mediated immune evasion in pancreatic cancer
Scientific Reports (2023)
-
Comparative oncology: overcoming human cancer through companion animal studies
Experimental & Molecular Medicine (2023)
-
Expansion of platform physiologically-based pharmacokinetic model for monoclonal antibodies towards different preclinical species: cats, sheep, and dogs
Journal of Pharmacokinetics and Pharmacodynamics (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.