Abstract
Body mass index (BMI) is used to measure body fat. We investigated the association between BMI and long-term clinical outcomes in patients with acute severe hypertension who visited the emergency department (ED). Cross-sectional study data were obtained from a single regional emergency medical center, including patients with elevated initial systolic blood pressure ≥ 180 mmHg or diastolic blood pressure ≥ 100 mmHg. The patients were classified into five groups according to BMI level (underweight, normal, overweight, obese class I, II and III). Among 4867 patients who presented with acute severe hypertension at the ED, 935 (19.21%) died within 3-years. In particular, 140 (44.59%) patients in the underweight group died from any cause, which was the highest among the five groups, and there was a reverse J-shaped association between BMI and 3-year all-cause mortality. Underweight patients had a significantly increased risk of all-cause mortality by 1.55-fold during the 3-year follow-up. Rather, obesity was associated with a reduction in the 3-year all-cause mortality. Comorbidities, including chronic kidney disease and acute hypertension-mediated organ damage, were independent predictors of all-cause mortality in patients who were not underweight. Underweight contributes to worsening long-term clinical outcomes in patients with acute severe hypertension. Clinicians should consider BMI as one of the physical examination parameters in patients with acute severe hypertension, and management including lifestyle modifications such as diet control and exercise should be undertaken considering BMI and comorbidities.
Similar content being viewed by others
Introduction
Hypertension is a well-known risk factor for cardiovascular disease (CVD) and all-cause mortality worldwide1. Effective lifestyle modification and anti-hypertensive drug treatment strategies can reduce blood pressure (BP) in hypertensive patients2. Nevertheless, BP control rates are still poor worldwide and are not satisfactory in Korea or across Europe3. In particular, acute and severe BP elevations due to uncontrolled hypertension are serious problems commonly encountered in patients visiting the emergency department (ED). According to our previous study, patients with acute severe hypertension, which was defined as systolic blood pressure (SBP) ≥ 180 mmHg or diastolic blood pressure (DBP) ≥ 100 mmHg, accounted for 59 out of 1000 ED visits at a single center and showed poor clinical outcomes, with a 1-year mortality rate of 8.8% and a 3-year mortality rate of 13.9%4.
Body mass index (BMI) is one of the markers of obesity and body fat5, which has a strong association with all-cause mortality. Most studies demonstrated a J- or U-shaped association with the lowest mortality in people with an optimal BMI (20–25 kg/m2) range6,7,8,9. However, the obesity paradox implies that overweight and mildly obese groups have a better prognosis for all-cause mortality10. Low BMI (< 18.5 kg/m2) may be a risk factor for CVD and all-cause mortality, which may be attributed to aging, sarcopenia, and poor nutritional status in the underweight population11. Although underweight and obesity are important clinical characteristics of patients with CVD, few studies have attempted to demonstrate the effect of BMI on all-cause death or cardiovascular outcomes in patients with acute severe hypertension.
In this study, we investigated the association of BMI level with all-cause mortality during long-term follow-up in patients with acute severe hypertension who visited the ED.
Method
Study population and data collection
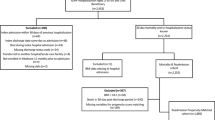
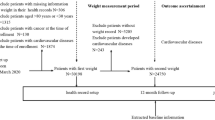
The data for this retrospective cohort study were obtained from a single regional emergency medical center: Hanyang University Guri Hospital, Guri, Gyeonggi-do, Korea. The study design and primary results were previously published4. The medical records of 172,105 patients who visited the ED between January 2016 and December 2019 were reviewed; 16,404 patients who had elevated initial SBP ≥ 180 mmHg or DBP ≥ 100 mmHg were enrolled in this study (Fig. 1). Of these, patients aged < 18 years who presented with acute trauma, certificates, or who visited the ED multiple times were excluded from this study. Among these 10,219 patients with acute severe hypertension, 4867 had available data regarding BMI. The National Emergency Department Information System (NEDIS) data were used to identify eligible patients who visited the ED. The system collects data, including initial vital signs and baseline clinical characteristics. This information on all patients visiting the ED is automatically transmitted from each hospital to a central government server called NEDIS. The patients were classified into five groups according to BMI level as follows; underweight group whose BMI < 18.5 kg/m2, normal group whose BMI between 18.5 kg/m2 and 22.9 kg/m2, overweight group whose BMI kg/m2 between 23 and 24.9 kg/m2, obese class I group whose BMI between 25 kg/m2 and 29.9 kg/m2, obese class II + III group whose BMI ≥ 30 kg/m2. The study was conducted in accordance with the Declaration of Helsinki, and was reviewed and approved by the Institutional Review Board of Hanyang University Guri hospital (GURI 2020-01-028). The institutional review board of Hanyang University Guri hospital waived the requirement for written informed consent.
Data collection
Data were collected using electronic medical records by experienced data collectors under principal investigator supervision. The following demographic and clinical characteristics were extracted: age, sex, initial BP at the ED, and traditional cardiovascular risk factors, including a history of hypertension, diabetes, dyslipidemia, chronic kidney disease (CKD), end-stage renal disease, smoking and alcohol consumption status. History of heart failure, ischemic stroke, hemorrhagic stroke, coronary artery disease, and peripheral artery disease was also extracted.
The following laboratory data were extracted: estimated glomerular filtration rate (eGFR) (mL/min/1.73 m2), B-type natriuretic peptide (BNP), and proteinuria in a dipstick urinalysis. In addition, diagnostic test findings to determine the presence of acute hypertension-mediated organ damage (HMOD) were obtained.
The primary outcome was the incidence of all-cause mortality during the 3-year follow-up (until March 15, 2021) according to the BMI level. The secondary outcomes were all-cause mortality within 1-month, 3-months and 1-year follow-up, hospital admission, and death at the ED according to BMI level. The incidence of mortality and its timing were extracted from the National Health Insurance Service in South Korea, and other outcome data were extracted from local medical records.
Definition
Obesity and overweight were defined according to the WHO guidelines for the Asia Pacific region and the Korean Society for the Study of Obesity Guideline for the management of obesity12. Acute HMOD was defined as hypertensive encephalopathy, cerebral infarction, intracerebral hemorrhage, retinopathy, acute heart failure, acute coronary syndrome (ACS), acute renal failure, and aortic dissection13. Hypertensive encephalopathy was defined as a severe increase in BP associated with other unexplained lethargy, seizures, cortical blindness, and coma13. Cerebral infarction and intracerebral hemorrhage were defined on the basis of neurological symptoms and brain imaging at the ED. Fundus examination confirmed retinopathy based on the presence of flame-like hemorrhages, cotton wool spots, or papilledema. Proteinuria was defined as a dipstick urinalysis result of ≥ 1 +14. BP was measured in the ED above the brachial artery using an automated BP machine, Spot Vital Signs LXi (Welch Allyn, Skaneateles Falls, NY, USA).
Statistical analysis
All categorical data are presented as numbers and percentages, while statistics for continuous variables are presented as means and standard deviations. The Cochran–Mantel–Haenszel test was used to extract the trend of clinical outcomes, including mortality, hospital admission, and death at the ED, and categorical data of baseline characteristics according to BMI level. Linear regression was used to show the distribution of the means and the trend of continuous variables of baseline characteristics according to BMI. Kaplan–Meier survival analyses and log-rank tests were used to compare the cumulative survival probability according to BMI level. The restricted cubic spline curve showed a continuous adjusted association between BMI and the risk of all-cause mortality in patients with acute severe hypertension. Hazard ratio (HR) and respective 95% confidence intervals (CIs) for 3-year all-cause mortality in the underweight, overweight, and obese groups compared with the normal BMI group were calculated using multivariable Cox proportional hazards regression analyses. We investigated the association between BMI level and 3-year all-cause mortality, with and without adjustment for the selected confounders. Three models were used. In Model 1, age and sex were considered as possible confounders. Model 2 included factors which were thought to be clinically relevant (age, sex, and social history) and medical history with p < 0.05 at baseline, as follows: age, sex, smoking, alcohol consumption, and medical history of hypertension, diabetes mellitus, dyslipidemia, ischemic stroke, hemorrhagic stroke, chronic kidney disease, and end-stage renal disease. Model 3 included variables with p < 0.2 in the univariable Cox proportional hazards regression analyses, as follows: age, sex, smoking, alcohol consumption, and medical history of hypertension, diabetes mellitus, dyslipidemia, ischemic stroke, hemorrhagic stroke, coronary artery disease, heart failure, chronic kidney disease, and end-stage renal disease. To evaluate the risk factors for 3-year all-cause mortality of each BMI category, we performed the multivariable Cox proportional hazards regression analyses using the variables with p < 0.2 in the univariable analysis of each group. Additionally, we performed a subgroup analysis with the multivariable Cox proportional hazards regression analyses according to the age group (< 50, 50–59, 60–69, and ≥ 70 years), presence or absence of a history of diabetes mellitus, and patients without chronic disease, including heart failure, ischemic stroke, hemorrhagic stroke, and end-stage renal disease. Among the candidate variables, social history and medical history were missing for some patients. History of alcohol consumption and cigarette smoking was missing for 62 (1.3%) and 65 patients (1.3%), respectively, and end-stage renal disease, which had the highest missing data in the medical history, was missing for 31 patients (0.6%). We conducted the Cox proportional hazard regression with complete-case analysis, which involves restricting the analysis to individuals with no missing data. We tested the proportional hazards assumption for each variable in the multivariable models using the supremum test. All variables in the models were found to satisfy the proportional hazards assumption. All tests were two-tailed, and statistical significance was set at p < 0.05. All analyses were performed using the Statistical Analysis Software (version 9.4; SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
Among 4867 patients with acute severe hypertension at the ED, 314 (6.45%) patients in the underweight group, 1528 (31.40%) in the normal group, 1026 (21.08%) in the overweight group, 1530 (31.44%) patients in the obese class I group, and 469 (9.64%) patients in the obese class II + III group were analyzed in the present study. The baseline characteristics of the patients are presented in Table 1. The mean age of the total study population was 61.85 ± 16.45 years, and half were male (53.61%). The patients in the underweight group were the oldest, and most frequently female among the five groups. Patients in the obese class II + III group had the highest prevalence of current smokers and alcohol drinkers, and had the highest incidence of traditional cardiovascular risk factors, such as hypertension, diabetes mellitus, and dyslipidemia among the five groups. On the contrary, ischemic stroke and hemorrhagic stroke were the most common in the underweight group. In laboratory findings, the lower the BMI, the higher the BNP, and the higher the prevalence of proteinuria. In the diagnostic test findings to evaluate the presence of HMOD, cardiomegaly was significantly more common as BMI increased. There was no difference among the groups in the frequency of taking antihypertensive medication among patients with hypertension. The patterns of acute HMOD according to BMI are shown in Table 1. Acute coronary syndrome and hypertensive retinopathy showed a tendency to increase significantly as BMI increased, while acute heart failure showed a tendency to increase significantly as BMI decreased. There was no significant difference according to BMI in the other acute HMODs.
All-cause mortality according to BMI level in patients with acute severe hypertension
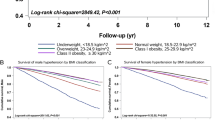
Of all the patients with data on mortality (n = 4867), a total of 935 (19.21%) patients died within 3 years (Table 2). The trend of primary outcome increased significantly as BMI decreased. In the underweight group, 140 (44.59%) patients died from any cause during the 3-year follow-up period. In the obese II + III group, 42 (8.96%) patients, lowest among the five groups, died from any cause during the 3-year follow-up. As a secondary outcome, the trend of all-cause mortality rates increased significantly as BMI decreased at 1-month, 3-month, and 1-year follow-ups. Indeed, 3461 (71.11%) patients were admitted, and one patient (0.02%) died in the ED. Underweight patients showed the highest admission rates among the five groups. Based on the BMI level, cumulative death-free survival probability was analyzed, and the results are shown in Fig. 2. Among the five groups according to BMI level, in unadjusted comparisons, the cumulative survival probability was significantly lower in the underweight group. The five groups according to BMI had significantly different probabilities of all-cause mortality (log-rank p < 0.001).
Association between BMI and all-cause mortality
Compared with patients with a normal BMI, those with a higher BMI were associated with a graded inverse association with mortality (Table 3). The overweight group was associated with a 41% lower risk in all-cause mortality, a 60% lower risk in the obese class I group, and a 69% lower risk in the obese class II + III group. In contrast, the underweight group had a 1.96-fold increased risk in all-cause mortality. Similar findings were observed in the adjusted analysis, which showed a significant, inverse association between BMI and all-cause mortality risk, and the underweight group was significantly associated with a 1.55-fold increase in all-cause mortality. Similar findings were also observed in the continuous analysis using restricted cubic splines with a reverse J-shaped association between BMI and the risk of all-cause mortality (Fig. 3). The nadir for all-cause mortality risk among patients with acute severe hypertension was estimated from model 3 to be 28.2 kg/m2. There was no serious violation of the proportional hazard assumption, as the p values for all adjusted covariates using the supremum test were greater than 0.05 (Supplementary Table S1).
Continuous association between BMI and all-cause mortality in acute severe HTN patients. Restricted cubic splines showing a continuous adjusted association between BMI and risk of all-cause mortality in patients with HTN crisis. The shaded area shows the 95% confidence interval for the estimated hazard ratio point associated with different BMI levels after adjusting for age, sex, hypertension, diabetes mellitus, dyslipidemia, ischemic stroke, hemorrhagic stroke, chronic kidney disease, end-stage renal disease, smoking, and alcohol consumption. (Reference BMI :18.5 kg/m2). BMI, body mass index; CI, confidence interval; HTN, hypertension.
Predictors for 3-year all-cause mortality of each BMI group
Table 4 shows the Cox proportional hazards regression analysis according to BMI level after adjusting for confounding factors. (Supplementary Table S2 shows the univariate analysis to evaluate the predictors of 3-year all-cause mortality in each BMI group.) Old age was independently associated with 3-year mortality in all groups stratified by BMI. Except for age, the predictors of long-term mortality were slightly different for each BMI level. Male sex and diabetes mellitus (HR 1.97, 95% CI 1.38–2.83, p < 0.001; HR 1.54, 95% CI 1.04–2.21, p = 0.018) were significant independent predictors of all-cause mortality in the underweight group. In the normal group, male sex, CKD, smoking, and the presence of acute HMOD at the ED were independent predictors. In the overweight group, ischemic stroke, CKD, and the presence of acute HMOD at the ED were independent predictors. Dyslipidemia, CKD, and the presence of acute HMOD at the ED were independent predictors of 3-year mortality in the obese class I group, whereas in the obese class II + III group, CKD and the presence of acute HMOD at the ED were significant predictors during the long-term follow-up.
Subgroup analysis for factors that may affect the association between underweight and all-cause mortality
Multivariable Cox proportional hazards regression analyses according to age groups (< 50, 50–59, 60–69, and ≥ 70 years) (Supplementary Table S3) revealed that underweight was associated with an increased risk of all-cause mortality in all the age groups except in the group under the age of 50 years. The results of stratified analysis according to the presence or absence of diabetes mellitus showed a similar trend to the results of overall patients. In addition, the results of patients without chronic disease, including heart failure, ischemic stroke, hemorrhagic stroke, and end-stage renal disease, showed that underweight was also associated with an increased risk of all-cause mortality.
Discussion
Based on the results of this study, underweight patients with acute severe hypertension had a significantly increased risk of 3-year all-cause mortality, and obese patients were associated with a reduction in 3-year all-cause mortality. There was a reverse J-shaped association between BMI and all-cause mortality, with the lowest mortality at 28 kg/m2. In particular, 44.59% of underweight patients died within 3 years. In addition, underweight patients showed the highest admission rates among the five groups. In the non-underweight groups, including normal, overweight, and obese groups, comorbidities including CKD and the presence of acute HMOD at the ED were important risk factors for 3-year all-cause mortality.
In the overall population, BMI and all-cause mortality are known to have a J-shaped association6,8. In Korean data that presented association between mortality and BMI in elderly population over 65 years of age using National Health Insurance System-Senior Database15, the risk of all-cause mortality was increased by 2.5-times in the underweight group with BMI of < 18.5 kg/m2, and 1.4-times in the group with BMI between 18.5 and 23 kg/m2, whereas the overweight and obese group with a BMI > 25 kg/m2 did not differ significantly in mortality risk from the reference group (BMI 23–25 kg/m2). This pattern was also observed in the association between BMI and death due to CVD. It is important to note that underweight adults with a BMI of less than 18.5, have a higher risk of mortality than adults with a normal BMI. To our knowledge, studies on the association between BMI and mortality in hypertensive patients are rare, and there are no studies specifically targeting patients with acute severe hypertension. Xu et al.16 demonstrated a U-shaped association between BMI and mortality in patients with hypertension using the Health Improvement Network primary care research database in the United Kingdom, which showed that the mortality risk was increased in the underweight group and there was no increase in risk in overweight and normal BMI groups, and then increased in the obese group with a BMI of 29 kg/m2 or higher. In hypertensive Chinese patients, Wei Yang et al.17 suggested an association between BMI and all-cause mortality as a reverse J-shape, and even after adjusting for potential confounding factors, the mortality rate of the underweight group increased 1.56-fold compared to normal, and the optimal BMI was 30–34.9 kg/m2. Our study is different from previous studies wherein analysis was conducted on patients who visited the ED with acute severe hypertension (initial SBP ≥ 180 mmHg or DBP ≥ 100 mmHg). Our study demonstrated that the underweight group had a 1.55-fold increase in all-cause mortality compared to the normal BMI group, and the relationship between BMI and mortality showed a reverse J-shaped association rather than a U-shaped or J-shaped association. We performed subgroup analysis to exclude the effects of old age and chronic disease status, including heart failure, ischemic stroke, hemorrhagic stroke, and end-stage renal disease, which were highly associated with underweight, and suggested an association between death and underweight. These results of stratified analysis according age did not change with our main results except for those under the age of 50 years, that is, the effect of underweight on 3-year mortality was predominantly found in elderly. In addition, the overweight and obese groups support the obesity paradox that lowered the risk of mortality in patients with acute severe hypertension. The BMI, which corresponds to the lowest risk of all-cause mortality in patients with acute severe hypertension, was estimated to be 28.0 kg/m2 even after correcting possible correction factors. Previous Asian studies have shown that the optimal BMI shifts upward, lowering the mortality rate of the overall population, which is consistent with the findings of our study17,18,19.
Obesity, a modifiable risk factor for CVD, is a determinant of adiposity; however, the proportion of lean mass is important. Body composition varies widely among individuals, even if they have the same BMI, because the composition of fat mass and lean mass is different and can affect health outcomes, including mortality20. Loss of lean mass is associated with a hyper-inflammatory status, insulin resistance, and cardiometabolic disorders21,22. In addition, a smaller lean mass is associated with worse exercise capacity and cardiorespiratory fitness, which could in turn lead to increased mortality22,23. A previous Korean study using the Korean National Health Insurance Service database showed that the risk of CVD increases as the severity of underweight increases24. Thus, the clinical significance of underweight with a small lean mass is important. The reduced lean mass leads to a lower cardiorespiratory fitness associated with peripheral muscular and cardiac dysfunction, which may play a crucial role in the pathophysiology of heart failure progression25,26. The importance of lean mass is also shown in the pattern of acute HMOD in the underweight group, and they had significantly more heart failure than the overweight and obese groups in our study.
Underweight can increase the mortality in patients with acute severe hypertension, rather than due to comorbidities other than age and diabetes. In contrast, CKD and acute HMOD were independent risk factors of all-cause mortality in patients with acute severe hypertension who were not in the underweight group. Renal function plays an important role in BP regulation, and renal dysfunction is also a predictor of poor cardiovascular outcome and death in hypertensive crisis27,28. In addition, HMOD consists of structural and functional changes in the arteries or organs and increases the risk of mortality and cardiovascular events in hypertensive patients1,29. Although obesity and overweight lower the mortality rate of patients with acute severe hypertension, active management is required for patients with these predictors.
Acute severe hypertension is associated with adverse outcomes and high utilization of healthcare services. In this context, understanding the prognostic factors of all-cause mortality in patients presenting with acute severe hypertension is pivotal in improving the medical care for hypertensive patients while reducing the healthcare burden. In the setting of the ED, it is not possible to perform complete workup in patients with acute severe hypertension because of the difficulty in evaluating indicators for predicting mortality. As this study indicated that diagnostic examination as well as BMI are predictors of mortality, more aggressive follow-up and treatment are required for underweight patients.
Our study had several limitations. First, this was a retrospective study. Patients who visited the ED were not obligated to measure height and weight; therefore, only 47.6% of all patients with acute severe hypertension were available for BMI data; therefore, the possibility of selection bias cannot be excluded. In addition, there were missing data on variables highly related to BMI, such as alcohol consumption, smoking status, exercise, and drug history. We conducted an analysis on all patients with BMI data (n = 4867), despite missing other data. In particular, the obese I group showed that dyslipidemia reduced the risk of mortality, possibly because the information on whether or not dyslipidemia was based on medical record investigations, and having dyslipidemia may mean that the patient is already taking a lipid-lowering drug. If there were data on drug history, an interpretation would have been possible. These missing data and variables that were poorly measured or unmeasured could act as confounders in our results. A prospective study will be needed to develop a protocol that includes all factors that can affect BMI in the future. Second, this study was a single-center experience, which may not be representative of the entire population. Third, because there was no available data on the cause of death from the National Health Insurance Service, cardiovascular mortality could not be determined in this study. However, the data provided by the National Health Insurance Service on all-cause mortality and the date of death are accurate and reliable. Fourth, since echocardiography, fundoscopy, chest, and abdominal CT were performed only in a small number of patients owing to the ED environment and condition, the interpretation of the results of the analysis, to classify by BMI category, is limited.
In conclusion, although high BMI is known to be an important cardiovascular risk factor, underweight rather than overweight and obesity contributes to a worse long-term clinical outcome in patients with acute severe hypertension. Depending on whether the acute severe hypertensive patients are underweight, overweight, or obese, clinicians should make an appropriate approach and management including lifestyle modifications such as diet control and exercise considering their comorbidities and BMI itself.
Data availability
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 39, 3021–3104 (2018).
Lee, H. Y. et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: Part II-diagnosis and treatment of hypertension. Clin. Hypertens. 25, 20 (2019).
Kim, H. C. et al. Korea hypertension fact sheet 2020: analysis of nationwide population-based data. Clin. Hypertens. 27, 8 (2021).
Kim, B. S. et al. Clinical characteristics, practice patterns, and outcomes of patients with acute severe hypertension visiting the emergency department. J. Hypertens. 39, 2506–2513 (2021).
Park, J. H. et al. Burden of disease attributable to obesity and overweight in Korea. Int. J. Obes. (Lond.) 30, 1661–1669 (2006).
Aune, D. et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ 353, i2156 (2016).
Berrington de Gonzalez, A. et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 363, 2211–2219 (2010).
Global, B. M. I. M. C. et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388, 776–786 (2016).
Bhaskaran, K., Dos-Santos-Silva, I., Leon, D. A., Douglas, I. J. & Smeeth, L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3.6 million adults in the UK. Lancet Diabetes Endocrinol. 6, 944–953 (2018).
Romero-Corral, A. et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet 368, 666–678 (2006).
Park, D., Lee, J. H. & Han, S. Underweight: another risk factor for cardiovascular disease?: A cross-sectional 2013 Behavioral Risk Factor Surveillance System (BRFSS) study of 491,773 individuals in the USA. Medicine (Baltimore) 96, e8769 (2017).
Seo, M. H. et al. 2018 Korean Society for the Study of Obesity Guideline for the Management of Obesity in Korea. J. Obes. Metab. Syndr. 28, 40–45 (2019).
van den Born, B. H. et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur. Heart J. Cardiovasc. Pharmacother. 5, 37–46 (2019).
White, S. L. et al. Diagnostic accuracy of urine dipsticks for detection of albuminuria in the general community. Am. J. Kidney Dis. 58, 19–28 (2011).
Lee, S. H. et al. Association between body mass index and mortality in the Korean elderly: A nationwide cohort study. PLoS ONE 13, e0207508 (2018).
Xu, W., Shubina, M., Goldberg, S. I. & Turchin, A. Body mass index and all-cause mortality in patients with hypertension. Obesity (Silver Spring) 23, 1712–1720 (2015).
Yang, W. et al. Association between body mass index and all-cause mortality in hypertensive adults: Results from the China Stroke Primary Prevention Trial (CSPPT). Nutrients 8, 384 (2016).
Chung, W. S., Ho, F. M., Cheng, N. C., Lee, M. C. & Yeh, C. J. BMI and all-cause mortality among middle-aged and older adults in Taiwan: a population-based cohort study. Public Health Nutr. 18, 1839–1846 (2015).
Lee, J. S. et al. Obesity can benefit survival-a 9-year prospective study in 1614 Chinese nursing home residents. J. Am. Med. Dir. Assoc. 15, 342–348 (2014).
Lee, D. H. et al. Predicted lean body mass, fat mass, and all cause and cause specific mortality in men: Prospective US cohort study. BMJ 362, 2575 (2018).
Li, C. W. et al. Circulating factors associated with sarcopenia during ageing and after intensive lifestyle intervention. J. Cachexia Sarcopenia Muscle 10, 586–600 (2019).
O’Donovan, G. et al. Cardiovascular disease risk factors in habitual exercisers, lean sedentary men and abdominally obese sedentary men. Int. J. Obes. (Lond) 29, 1063–1069 (2005).
Lee, D. C. et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation 124, 2483–2490 (2011).
Kwon, H. et al. Incidence of cardiovascular disease and mortality in underweight individuals. J. Cachexia Sarcopenia Muscle 12, 331–338 (2021).
Carbone, S. et al. Lean mass abnormalities in heart failure: The role of sarcopenia, sarcopenic obesity, and cachexia. Curr. Probl. Cardiol. 45, 100417 (2020).
Carbone, S. et al. Obesity paradox in cardiovascular disease: where do we stand?. Vasc. Health Risk Manag. 15, 89–100 (2019).
Derhaschnig, U. et al. Decreased renal function in hypertensive emergencies. J. Hum. Hypertens. 28, 427–431 (2014).
Szczech, L. A. et al. Acute kidney injury and cardiovascular outcomes in acute severe hypertension. Circulation 121, 2183–2191 (2010).
Oh, J. S., Lee, C. H., Park, J. I., Park, H. K. & Hwang, J. K. Hypertension-mediated organ damage and long-term cardiovascular outcomes in Asian hypertensive patients without prior cardiovascular disease. J. Korean Med. Sci. 35, e400 (2020).
Author information
Authors and Affiliations
Contributions
H-JK contributed to conceptualization, study design, data collection, and data interpretation, drafted the article, was a major contributor in writing the manuscript. BSK was responsible for study design, data collection, data interpretation, manuscript preparation, and also was an equally major contributor in writing the manuscript. JHL contributed to data analysis and data interpretation. J-HS was responsible for study design, data interpretation, and manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, HJ., Kim, B.S., Lee, J.H. et al. Impact of underweight on 3-year all-cause mortality in patients with acute severe hypertension: a retrospective cohort study. Sci Rep 12, 4798 (2022). https://doi.org/10.1038/s41598-022-08892-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08892-9
This article is cited by
-
Interaction between depressive symptoms and obesity-related anthropometric measures on multimorbidity among community-dwelling older adults: evidence from India
BMC Public Health (2024)
-
Association between D-dimer and long-term mortality in patients with acute severe hypertension visiting the emergency department
Clinical Hypertension (2023)
-
Association between B-type natriuretic peptide and long-term mortality in patients with acute severe hypertension visiting the emergency department
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.