Abstract
The aim of the study was a systematic evaluation of cognitive development in individuals with glutaric aciduria type 1 (GA1), a rare neurometabolic disorder, identified by newborn screening in Germany. This national, prospective, observational, multi-centre study includes 107 individuals with confirmed GA1 identified by newborn screening between 1999 and 2020 in Germany. Clinical status, development, and IQ were assessed using standardized tests. Impact of interventional and non-interventional parameters on cognitive outcome was evaluated. The majority of tested individuals (n = 72) showed stable IQ values with age (n = 56 with IQ test; median test age 11 years) but a significantly lower performance (median [IQR] IQ 87 [78–98]) than in general population, particularly in individuals with a biochemical high excreter phenotype (84 [75–96]) compared to the low excreter group (98 [92–105]; p = 0.0164). For all patients, IQ results were homogenous on subscale levels. Sex, clinical motor phenotype and quality of metabolic treatment had no impact on cognitive functions. Long-term neurologic outcome in GA1 involves both motor and cognitive functions. The biochemical high excreter phenotype is the major risk factor for cognitive impairment while cognitive functions do not appear to be impacted by current therapy and striatal damage. These findings implicate the necessity of new treatment concepts.
Similar content being viewed by others
Introduction
Glutaric aciduria type 1 (GA1; OMIM #231670) is a rare neurometabolic disorder of L-lysine metabolism caused by inherited deficiency of glutaryl-CoA dehydrogenase (GCDH) resulting in accumulation of glutaric acid (GA), 3-hydroxyglutaric acid and glutarylcarnitine especially within the brain. The GCDH gene is located on chromosome 19p13.2 encoding a flavin adenine dinucleotide dependent mitochondrial matrix protein catalysing the oxidative decarboxylation of glutaryl-CoA to crotonyl-CoA in the degradative pathway of L-lysine, L-hydroxylysine, and L-tryptophan. The estimated prevalence in Germany is 1:124.9301. Untreated individuals mostly develop striatal injury between the age 3–36 months which leads to a complex movement disorder (MD) with predominant dystonia due to bilateral striatal damage, manifesting acutely after acute encephalopathic crisis during potentially catabolic episodes such as febrile illness associated with high morbidity and mortality or insidiously without an apparent crisis2,3. Due to the primarily neurologic phenotype GA1 has been classified as a ‘cerebral organic aciduria’. Recently, however, also extra-neurological manifestations such as disturbance of kidney function have been reported1,4. Two biochemical subtypes in GA1, i.e., high excreter (HE) and low excreter (LE) have been arbitrarily defined depending on urinary concentrations of GA5, which is inversely correlated with residual enzymatic GCDH activity. Individuals with HE and LE subtype are thought to have a similarly high risk of striatal damage during infancy and the same a priori risk of developing a MD2,6. More recently, however, increased in vivo cerebral GA concentrations and progressive white matter abnormalities have been reported in HE patients, a finding of uncertain clinical relevance7. Metabolic treatment concepts have been developed during the last decades consisting of a low lysine diet with supplementation of a lysine-free, tryptophan-reduced, arginine-containing amino acid mixture and carnitine supplementation for maintenance treatment (MT) and transient emergency treatment (ET) during potentially catabolic episodes such as febrile illness or surgery. Implementation of GA1 into national newborn screening (NBS) programs facilitating early diagnosis as well as development and repetitive revision of evidence-based guideline recommendations have dramatically improved neurologic long-term outcome worldwide resulting in more than 90% asymptomatic individuals with GA1 without MD if treated in full accordance with the recommendations1,8,9,10,11,12,13.
In contrast to the significant motor phenotype, the clinical course in GA1 is not thought to typically include cognitive impairment14, but this has not been systematically studied before. Therefore, this study aims at prospectively investigating long-term cognitive development and functions of early diagnosed and treated individuals with GA1 in Germany over a period of over 20 years.
Methods
Study population
This national prospective multicentre observational study includes patients diagnosed with GA1 in Germany between January 1st, 1999, and February 29th, 2020. The study population comprised three subgroups: (1) individuals with GA1 correctly identified by NBS, (2) patients with false-negative NBS result identified by targeted metabolic work-up following the manifestation of characteristic neurological signs, and (3) previously undiagnosed women with GA1 identified by initially positive NBS results of their unaffected children (maternal GA1). Inclusion criteria comprised (1) confirmation of diagnosis by quantitative analysis of organic acids in urine (GA and 3-hydroxyglutaric acid) and/or GCDH mutation analysis and/or quantitative analysis of GCDH residual activity, and (2) written informed consent from patients and/or their parents.
Cognitive outcome
Development and cognition were evaluated using age-dependent standardized developmental and intelligence tests, performed by trained psychologists and medical staff. For patients up to age three years the Denver Developmental Screening Test and cognitive scale of Bayley Scales of Infant Development II or III were used. The Denver Developmental Screening Test categorizes development in four scales as ‘normal’ or ‘abnormal’ (personal-social, fine motor-adaptive, language, and gross motor)15. The results of Bayley Scales of Infant Development are numeric and distributed normally with a mean of 100 and SD of 1516. Patients aged three years up to adulthood were tested with IQ tests developed by David Wechsler (Wechsler Preschool and Primary Scale of Intelligence [HAWIVA-III, WPPSI-III/-IV], Wechsler Intelligence Scale for Children [HAWIK-IV, WISC-IV/-V], Wechsler Adult Intelligence Scale [WAIS-IV]), Nadeen and Alan Kaufmann (Kaufmann Assessment Battery for Children [K-ABC/K-ABC-II]), and Anna Snijders-Oomen (Snijders-Oomen Nonverbal Intelligence Test [SON-R 2.5–7]). Full scale and subscale IQ results, all normalized to mean 100 with SD 15, were used for analysis. Subscales of different IQ tests were attributed to cognitive factors according to the Cattel-Horn-Carroll theory (Table 1)17. For a cross-sectional analysis, the most recent test result of each patient was used. For individuals with more than one IQ test an additional longitudinal analysis was performed.
Biochemical subtype
According to a previous definition based on residual enzymatic GCDH activity and urinary GA concentrations, the biochemical subtype was arbitrarily classified as HE if GA concentration in urine was higher than 100 mmol/mol creatinine, or as LE if GA was equal to or below 100 mmol/mol creatinine5. Further definitions of biochemical subtypes using clinical variables have not been established for GA1 due to the similar clinical course of both subgroups. For additional analysis, we delineated an intermediate biochemical subgroup of patients with initially elevated GA concentrations of 100–1000 mmol/mol creatinine rapidly declining below 100 mmol/mol creatinine after the start of metabolic treatment. Only those individuals whose GA concentrations remained above 100 mmol/mol GA were classified as HE.
Treatment
According to the current guideline recommendations9, metabolic MT consists of a (1) low-lysine diet (i.e. age- and weight-dependent calculated reduction of daily lysine intake) with supplementation of a lysine-free, tryptophan-reduced, arginine-fortified amino acid supplement maintaining a sufficient energy and micronutrient intake for patients up to age six years, (2) a liberalized protein-controlled diet for patients beyond age six years, and (3) life-long oral carnitine supplementation. Intermittent ET is recommended in every potentially catabolic situation and consists of transiently (1) high carbohydrate intake, (2) low to no protein intake, and (3) intensified carnitine supplementation. Treatment was assessed as adequate only if guideline recommendations were followed throughout the patient’s course. Patients were classified as being supervised by a metabolic centre if supervision had started during the neonatal period and continued until the last follow-up visit.
Neurologic manifestations
Based on the patients’ medical history and clinical examination, neurologic manifestations were classified as (1) major if patients developed MD, (2) minor if patients had fine motor or coordination deficits in the absence of MD, and (3) asymptomatic if none of these symptoms existed. MD was mild if it did not cause serious disability in daily life, moderate in the case of motor disability affecting daily life, but with some motor functions being preserved, and severe if only few or no motor skills were left. Onset-type of MD was assessed as (1) acute following encephalopathic crisis or subdural haemorrhage, or (2) insidious without apparent crisis.
Kindergarten and school
Attendance of kindergarten and school was classified as (1) regular kindergarten/school, (2) regular kindergarten/school with remedial teaching, and (3) kindergarten/school for children with special educational needs.
Statistical analysis
Statistical analysis was conducted using the statistical package R18. For all parameters, sample size, mean, median, SD, interquartile range (IQR), and range were calculated (Table 2). Independent variables for cognitive outcome analysis comprised (1) sex, (2) biochemical subtype, (3) neurologic manifestations, (4) adherence to recommended MT, and (5) adherence to recommended ET. Impact on full scale IQ and subscale results was investigated in a cross-sectional and a longitudinal analysis with multiple linear regression models and linear mixed effects models (R package lme4) using Satterthwaite’s method for estimating degrees of freedom19. Variable reduction in regression models was applied using a forward and backward stepwise procedure based on Akaike Information Criteria. We used classification and regression trees (R package rpart)20 analysis to identify subgroups with different IQ according to independent variables. Post-hoc comparisons in multiple regression models and classification and regression trees were applied with Tukey honestly significant difference method. We present data as boxplots which show IQR (box), median (horizontal line in box), and mean (triangle in box). Whiskers extend to the most extreme data point which is no more than 1.5 times the length of the box away from the box; points outside the range of whiskers can be considered as outliers.
Standard protocol approvals, registrations, and patient consents
The study was approved by the Institutional Ethics Committee of the coordinating centre (University Hospital Heidelberg, application no. S-525/2010) as well as all contributing study sites. All methods were performed in accordance with relevant guidelines and regulations. All patients and/or their parents gave written informed consent to participate in the study and to be included into the European registry and network for Intoxication type Metabolic Diseases (https://www.eimd-registry.org/)21.
Results
Study population and epidemiology
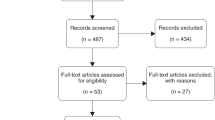
The study sample included 107 patients with confirmed GA1, 98 of whom were identified by NBS, while six patients were missed by NBS and three maternal patients were diagnosed due to positive NBS results of their unaffected offspring. According to the German Society of Newborn Screening (https://www.screening-dgns.de/), the study cohort comprised 97.2% (69 of 71) of individuals identified by the German NBS program between 2004 and 2017 (so far, no data have been reported for the time before and after this interval). Overall sensitivity of NBS during the study period was 94.2%, but differed between HE (n = 78, 100%) and LE patients (n = 18, 75%; n = 2 patients with unknown biochemical subtype). Ninety-three patients (95%) of the NBS group survived until last visit and five patients (5%) died, four of whom with severe or moderate dystonic MD, as previously reported1,22.
In the NBS group, results of cognitive tests were available for 72 patients. Fifty-eight patients had at least one IQ test (multiple testing in 22 individuals) and 14 infants had developmental tests (Denver Developmental Screening Test: n = 13, Bayley Scales of Infant Development: n = 3; multiple tests possible). Reasons for missing (IQ) tests comprised rejection by patients or parents (n = 12), non-acceptance of the offer by the metabolic centre (n = 4), logistic problems (n = 6), severity of MD (n = 6), death (n = 5), and young age not allowing application of IQ tests (n = 7).
Tested individuals in the NBS group (39 females, 33 males) were diagnosed at a median (IQR, range) age of seven days (6–9, 2–84) and were tested at a median (IQR, range) age of 7.9 years (4.9–12.4, 0.7–19.1), with a cumulative follow-up time of 651.3 years. In 65 patients, positive NBS results were confirmed by GCDH mutation analysis and/or quantitative analysis of GCDH residual activity, and seven patients were diagnosed by quantitative analysis of organic acids in urine (GA and 3-hydroxyglutaric acid). Fifty-six patients (78%) were classified as HE subtype and 14 patients (19%) as LE subtype according to the previous definition5. A subgroup of 11 HE patients, in whom urinary GA excretion decreased below 100 mmol/mol creatinine after the start of metabolic therapy, was considered as intermediate subtype for additional analysis. The biochemical subtype remained unknown in two patients. Median (IQR) urinary GA concentration at last visit was 980 (554–1908) mmol/mol creatinine in HE patients, 7.5 (1.7–26) in intermediate patients, and 4 (0.6–10.3) in LE patients. Sixty-two patients (86%) attended kindergarten, 56 (90%) of whom attended regular kindergarten and six patients (10%; 4 of 6 with MD) attended kindergarten for special needs. Fifty-two patients (72%) attended school, 31 (60%) regular school (n = 5 with MD, n = 26 asymptomatic), while four patients (8%, 3 of 4 with MD) had additional remedial teaching in a regular school, and 13 patients (25%) attended a school for special education needs (n = 7 with MD, n = 3 with minor neurologic symptoms, n = 3 without motor symptoms). Three adult patients (6%) had successfully finished regular school (2 of 3 with MD), and the school career of one patient was unknown.
Clinical outcome
None of the NBS patients showed signs of MD at diagnosis. At last visit, motor functions were normal in 43 of 72 patients with cognitive tests (60%), while seven patients (10%) had minor neurologic abnormalities and 22 patients (31%) had complex MD, mostly dystonia (n = 21). Dystonia was usually mild (n = 11; 52%) or moderate (n = 8; 38%), while two patients (10%) developed severe dystonia. Onset-type of dystonia was acute after encephalopathic crisis (n = 5; 23%) or following minor head trauma with subsequent subdural haemorrhage (n = 2; 9%), and insidious in 15 patients (68%). In 11 patients, dystonia was accompanied by ataxia (n = 3), ataxia plus chorea (n = 2), ataxia plus spasticity (n = 2), chorea (n = 2) or spasticity (n = 1). Another symptomatic patient had isolated ataxia.
Fifty-three patients (74%) followed the guideline recommendations for MT, while 19 (26%) did not. Deviations from MT comprised non-adherence to treatment protocols (n = 8), prescribed treatment protocols deviating from current recommendations (n = 7), feeding problems (n = 3), and delayed start of treatment (n = 1). Full adherence to ET was found in 62 patients (86%), vs. non-adherence in n = 10 (14%). Sixty-two patients (86%) were followed by a paediatric metabolic centre, while ten patients (14%) were in care of local hospitals or resident paediatricians without metabolic focus.
Cognitive outcome in the NBS cohort
Detailed information is summarized in Table 2 and Supplementary Table 1.
Development in infants and young children (0–3 years)
Twenty-four patients were evaluated by Denver Developmental Screening Test. Median (IQR) age at last screening test was 2.4 (1.5–3.5) years. Fifteen patients (63%) showed normal development in all domains, whereas nine patients (27%, seven of whom had dystonic MD) showed isolated (n = 3), combined (n = 4) or global (n = 2) developmental delay (Table 2).
Test results of Bayley Scales of Infant Development were available for 19 patients at a median (IQR) test age of 2.2 (1.5–3) years. Results of the cognitive scale were in the lower average range (median [IQR] 93 [84–105]) and remained stable over time (p = 0.6883) but differed significantly between HE (n = 14; median [IQR] 89 [76–95]) and LE patients (n = 5; median [IQR] 107 [103–110]; p = 0.0174).
Cognitive functions are impaired compared to the general population
Overall, the median (IQR) IQ of tested individuals with GA1 was 87 (78–98) at the last documented IQ test (median [IQR] age 11 [14.1–19.1] years). Median IQ (IQR) of patients (n = 29) attending regular school was 95 (84–102), 70 (68–78) in patients (n = 4) with remedial teaching in a regular school, and 70 (61–81) in patients (n = 10) attending a school for special educational needs.
Biochemical HE phenotype is a risk factor for cognitive impairment
In analogy to the test results of Bayley Scales of Infant Development, the biochemical subtype had an impact on full scale IQ with LE patients (n = 12; median [IQR] 98 [92–105]) showing superior results compared to HE patients at last visit (n = 42; 84 [75–96]; p = 0.0164; Fig. 1A). The effect was emphasized in a longitudinal analysis of 22 patients using a linear mixed model showing different levels depending on the biochemical subtype of about one SD (estimate 0.9 SD = 13.5 IQ points; LE [n = 6]: median [IQR] IQ 102 [97–107] vs. HE [n = 16]: 87 [78–94]; p = 0.018; Fig. 1B). Additionally, this analysis revealed stable cognitive performance over time (p = 0.361; Fig. 1B).
Biochemical subtype and full scale IQ at last visit (A) and over different age groups (B). (A) Patients with biochemical HE phenotype (median [horizontal line in box] 84; IQR 75–96) had lower full scale IQ than patients with biochemical LE phenotype (median [IQR] 98 [92–105]; p = 0.0164). (B) Longitudinal analysis was conducted using linear mixed model, gray area indicate 95% confidence interval bands. IQ was stable over time (p = 0.361), but, depending on the biochemical subtype, at different levels (p = 0.018). Rugs on X-axis indicate individual measurements. Black triangles indicate mean IQ. HE high excreter, LE low excreter.
Next, we evaluated whether cognitive performance of the biochemical intermediate group differed from HE patients with constantly high GA concentrations or LE patients with constantly low GA concentrations. Patients assigned to the intermediate group (n = 10; median [IQR] IQ 92 [84–101]) showed a similar test performance as LE patients (n = 12; 98 [92–105]; p = 0.6771). Classification and regression trees analysis classified LE and intermediate patients as one group (n = 22; median [IQR] IQ 97 [86–104]) with higher performance level compared to HE patients (n = 31; 82 [72–94]; p = 0.0053; Fig. 2).
Extended biochemical subtype and full scale IQ. Patients with intermediate subtype had similar results as LE patients (p = 0.677). Results of these two groups (median [horizontal line in box] IQ 97; IQR 86–104) differed from HE patients (median [IQR] IQ 82 [72–94]; p = 0.005). Black triangles indicate mean IQ. HE high excreter, LE low excreter.
Motor phenotype and severity of MD did not have an impact on IQ. Median (IQR) IQ of patients with MD (n = 15) was 89 (69–96), while it was 78 (66–89) in patients with minor neurologic abnormalities (n = 7), and 88 (81–101) in asymptomatic patients (n = 34). Classification and regression trees analysis confirmed the strong impact of the biochemical subtype on IQ while cognitive functions of patients with and without neurologic abnormalities did not differ (p = 0.4045; Fig. 3).
Biochemical subtype, neurologic abnormalities and full scale IQ. While biochemical subtype had a strong impact on full scale IQ, neurologic abnormalities did not. Patients with HE phenotype and minor neurologic abnormalities (median IQ [horizontal line in box] 78; IQR 66–89) had lower results than LE patients (median [IQR] IQ 98 [92–105]; p = 0.0278). Results of HE patients did not differ depending on neurologic abnormalities (p = 0.4045). Black triangles indicate mean IQ. HE high excreter, LE low excreter.
Treatment quality has no impact on cognitive functions
Effects of metabolic treatment on neurologic outcome of the cohort were published separately1. Full scale IQ did not differ between patients with and without adherence to recommended MT (with MT [n = 43]: median [IQR] 87 [80–99] vs. without [n = 13]: 84 [75–95]; p = 0.942) and ET (with ET [n = 50]: 88 [79–99] vs. without [n = 6]: 77 [68–94]; p = 0.9728). In patients beyond age six years (n = 44; median [IQR] age at last test 11.9 [8.1–15.9] years), IQ did not differ between 32 patients following a protein-controlled diet according to the guideline recommendations (median [IQR] 87 [77–100]), eight patients no longer following a diet (86 [74–94]) and four patients still continuing a calculated diet (79 [71–87]; p = 0.563; Fig. 4).
Maintenance treatment and full scale IQ in patients beyond age six years. Results did not differ between patients following recommended protein-controlled diet (median [horizontal line in box] IQ 87; IQR 77–100), patients continuing calculated diet beyond age six years (median [IQR] 79 [71–87]) and patients not complying to any diet (median [IQR] 86 [74–94]; p = 0.563). Black triangles indicate mean IQ.
Subscale analysis
Subscale analysis included 54 of 72 patients with an intelligence test, and complete datasets with results for full scale and all five subscales were available for 28 patients (Table 1, Supplement Table 1). Median (IQR) IQ results ranging from 89 (84–96) for crystallised intelligence to 96 (79–101) in short-term memory indicated homogenous performance on both subscale and full scale IQ levels (median [IQR] full scale IQ of this subset 89 [78–100]; fluid reasoning 95 [82–106]; visual processing 92 [82–102]; processing speed 92 [83–101]; p = 0.7406; Fig. 5). Analysing performance on subscale level for each biochemical subtype separately showed homogenous results for HE (p = 0.7184) and LE patients (p = 0.7676). However, results differed significantly depending on biochemical subtype for fluid reasoning (p = 0.0479), crystallised intelligence (p = 0.0433), short-term memory (p = 0.0689), and processing speed (p = 0.0047) with LE patients showing superior results compared to HE patients.
Patients missed by NBS
All six patients missed by NBS (5 female, 1 male) belonged to the LE group, and five of them were diagnosed by targeted metabolic work-up after acute onset of MD (n = 3 with moderate, n = 2 with severe dystonia) while one asymptomatic patient was identified by high-risk family screening following diagnosis of an index patient. Numeric results of Bayley Scales of Infant Development and IQ tests ranging from 95 to 120 were similar to LE patients correctly identified by NBS.
Maternal GA1 patients
Neurologic outcome of three maternal GA1 patients was reported previously1. Full scale IQ, available for two patients, was 82 and 106 respectively and was stable over time (79 and 82 in one patient). For another patient, only non-verbal tests could be performed, and results were in the lower average range or below-average (fluid reasoning/visual processing: IQ 72; processing speed: IQ 86).
Discussion
The major findings of this study investigating the long-term cognitive outcome of individuals with GA1 identified through NBS in Germany between 1999 and 2020 are that (1) clinical phenotype of individuals with GA1 does include cognitive impairment despite NBS, (2) the biochemical HE subtype is the major risk factor for cognitive impairment, while early diagnosis by NBS, quality of treatment, and striatal damage do not have a measurable impact on cognitive functions, (3) cognitive functions are individually stable over time, and (4) full scale and subscale IQ results are homogenous.
Deep phenotyping in GA1: Unravelling the long-term impact on cognitive functions
Research on rare diseases is also the history of scientific clinical endpoint evolution and precise exploration of the clinical phenotype. Early studies on GA1 focussed on acute manifestation of a complex MD with predominant dystonia, demonstrating a similarly high risk of striatal damage for untreated HE and LE individuals and a dramatic decline of encephalopathic crises in patients identified by NBS and early treated23. The phenotypic spectrum was extended by insidious-onset dystonia, which is still observed in screened individuals not adhering to or not receiving recommended MT1,10. Anthropometric and MRI studies elucidated phenotypic differences between the two biochemical phenotypes; HE individuals more often than LE individuals developed macrocephaly and progressive white matter abnormalities with unclear clinical relevance24,25. Recently, chronic kidney dysfunction, which was not impacted by recommended therapy or the neurologic phenotype, was identified as a first non-neurologic disease manifestation1,4, and malignant brain tumours and audiological manifestations were described in single patients26,27.
It had been hypothesized that the clinical phenotype of GA1 individuals does not typically include cognitive impairment regardless of severe dystonic MD14. Thirty years later, it is still unclear whether this hypothesis holds true. Earlier case reports and small case series supported the notion of unaffected cognitive functions in NBS patients28,29,30,31, and cross-sectional analysis of computer-based testing of developmental functions and cognitive performances showed similar results in GA1 patients and healthy controls while dystonic patients showed impairment in tests measuring motor speed, but not in tests with higher cognitive load28. In contrast, cognitive decline was described in adult patients32, and deficits in short- and long-term memory were recently demonstrated in Gcdh-deficient mice, an animal model for GA1 with complete loss of enzymatic GCDH activity33.
In this large prospectively followed cohort of early diagnosed individuals with GA1, we clearly demonstrate that neurologic long-term outcomes in GA1 do not only include significant motor dysfunction as previously reported1,2, but, as a new observation, also cognitive impairment independent from motor phenotype, found in one third (17/52) of early diagnosed patients requiring special education in school, and depicting an additional socio-economic burden. To identify affected patients requiring supportive treatment, the current guideline recommendations integrate developmental and IQ-assessment into the clinical long-term monitoring of GA1 patients9. We found stable intellectual performance over time in all age groups from early infancy to adulthood, and no significant correlation of the neurologic (motor) phenotype with cognition. Furthermore, we did not detect a ‘GA1-specific’ subscale pattern, e.g., cognitive performance was homogenous on subscale level, which is in line with a previous study29. This finding indicates that affected patients need a generalized and combined approach of supportive treatments and special education in kindergarten or school, and no subscale-specific approach. Consequently, full scale IQ is an appropriate tool for intellectual assessment in GA1, similarly to other intoxication type metabolic diseases, such as ornithine transcarbamylase deficiency34.
The HE phenotype is the major risk factor for impaired cognitive outcome
Cognitive function and information processing require structural and functional integrity of cortex, basal ganglia, and thalamus35. Besides irreversible striatal damage found in symptomatic patients, GA1 patients are known to develop characteristic and highly dynamic MRI abnormalities (yet, of unclear clinical relevance) that may be present at birth, diminish under treatment (e.g., pallidal hyperintensity, frontotemporal hypoplasia) or progress with age (e.g., white matter abnormalities)36.
The two biochemical phenotypes in GA1 have been defined more than two decades ago5. Individuals with a HE subtype show a (virtually) complete loss of GCDH activity in contrast to up to 30% residual enzyme capacity found in LE subtype. The biochemical subtype is known to correlate with the genotype and residual enzyme activity, but not to predict the clinical phenotype6,37. Interestingly, patients with a hypothesized ‘intermediate’ biochemical subtype in our study showed similar cognitive results and long-term GA concentrations as individuals with LE subtype thus extending the range of initial biochemical abnormalities found in LE subtype as provided by a previous definition5.
However, recent MRI and 1H-magnetic resonance spectroscopy studies have observed discrepancies between HE and LE individuals, such as progressive periventricular white matter abnormalities in HE patients7,24,36, and progressive subependymal nodules in late diagnosed adults of the HE group, that had been explained by chronic neurotoxicity1,24. Lately, malignant brain tumours have been reported in three HE patients not receiving recommended therapy27. A recent study also reported on larger head circumferences in HE compared to LE patients25. In fact, the clinical impact of these observations is still unknown. Our study clearly demonstrates poorer cognitive outcome of individuals with HE phenotype compared to LE patients and the general population and thus, a first significant impact of the biochemical subtype on the clinical course. However, pathomechanism and aetiology of the diverse distribution of chronic neurotoxicity patterns among the two subtypes remain unclear. Accumulating GA and 3-hydroxyglutaric acid affect cellular functions on multiple levels impairing Krebs cycle enzymes38, interfering with anaplerotic transport processes between astrocytes and neurons39 as well as glutamatergic and GABAergic neurotransmission40, thus inducing brain energy impairment38, and generating increased amounts of reactive oxygen species41,42. Post-mortem studies showed massive accumulation of GA and 3-hydroxyglutaric acid43, which was explained by intracerebral de novo synthesis and entrapment of toxic metabolites due to limited permeability of the blood–brain barrier for dicarboxylic acids44, corresponding to the similarly high a priori risk of striatal damage in both HE and LE patients2,3. As an additional possible mechanism explaining differences between individuals with HE and LE subtype, selective glutarylation of more than 30 mitochondrial proteins exclusively localized in astroglial cells of Gcdh-deficient mice was recently demonstrated resulting in reduced catalytic activity, stability and protein–protein interaction of glutamate dehydrogenase and brain-specific carbonic anhydrase 5b. This process, in combination with elevated cerebral neurotoxic metabolites, may alter glial cell metabolism and coupling of astrocytes and neurons by harming anaplerotic transfers, increasing glutamate levels in the synaptic cleft, and affecting the formation of enzymatic supercomplexes which results in disturbed cerebral energy and neurotransmitter metabolism45,46. However, the specific dysfunctional effect of glutarylated proteins on mitochondrial function and its potential involvement in developing chronic and progredient whiter matter changes remains to be elucidated. It is also unclear whether increased cerebral concentrations of neurotoxic metabolites and progressive white matter abnormalities in HE patients are the cause of the poorer cognitive outcome in this study. Progression of white matter abnormalities might also affect cognition. Even if in this study no decline of cognitive performance over time was detected, extended long-term period remains unclear as this study covers only twenty years.
Implications for long-term treatment?
In combination with ET, low lysine diet has been demonstrated to be an effective treatment for early diagnosed GA1 patients up to age six years, and previous studies including a recent meta-analysis with over 600 patients have demonstrated the positive effect of metabolic MT and ET on neurologic motor outcome with the vast majority of patients with full adherence to recommended therapy being prevented from striatal injury and remaining asymptomatic1,8. Other forms of dietary treatment or experimental therapeutic approaches in animal models, such as inhibition of upstream enzymes, have been less effective or failed to prevent the clinical phenotype13,47,48,49. Effectiveness of dietary treatment in patients beyond age six years receiving a liberalized protein-controlled diet is less clear, but a stable clinical and anthropometric long-term disease course up to adulthood has recently been reported25,50. However, prospective studies during the last decades have shown that the effect of dietary treatment in GA1 seems to be limited since (1) white matter changes are already found in patients identified by NBS while still following a low lysine diet, (2) MT may not stop or slow the progression of white matter changes7, and (3) chronic renal abnormalities are found in both HE and LE patients regardless the quality of therapy1. In line with this, our study did not detect an impact of therapy on cognitive outcome. Whether further restriction of lysine intake could prevent cognitive impairment in HE patients seems doubtful. Since lysine intake below the minimal requirement affects normal growth and neurological development and increases the risk of insidious-onset dystonia, a deviation from recommended dietary management should not be considered as safe1,25.
Study limitations
Systematic and prospective evaluation of cognitive development is challenging in a rare metabolic disease such as GA1. However, our study population comprised the largest cohort worldwide that has been systematically analysed for cognitive functions in GA1. In addition, the study design included both, a cross-sectional analysis as well as a longitudinal design, which is considered the most high-quality design for developmental research. Nevertheless, we have to admit some limiting factors. First, we had to use a diversity of different neuropsychological tests including their revisions and adaptations of standard values as this study covers a long period of time of over 20 years. Second, the heterogeneous study cohort comprised different cultural backgrounds which may affect comprehensive performance in specific language-based but also non-verbal cognitive subtests. This may impact IQ test results that are standardized to a German reference population and may be a limitation in interpreting the data. Third, cognitive assessment of very young patients is generally difficult. And fourth, the limited number of patients with severe motor disabilities may result in a potential underestimation of the effect of severe MD on cognitive functions.
In summary, this study shows that neurologic impairment in GA1 is not only limited to motor deficits but is also related to cognitive functions. With HE patients being at risk for a poorer outcome, more effective long-term treatment concepts particularly for this subgroup are needed.
Data availability
The datasets of this study are not publicly available due to existing data protection laws. Data ownership is incumbent upon the members of the E-IMD consortium making data available for specific research purposes upon request.
Change history
12 October 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-00137-5
Abbreviations
- ET:
-
Emergency treatment
- GA:
-
Glutaric acid
- GA1:
-
Glutaric aciduria type 1
- GCDH:
-
Glutaryl-CoA dehydrogenase
- HE:
-
High excreter
- LE:
-
Low excreter
- MD:
-
Movement disorder
- MT:
-
Maintenance treatment
- NBS:
-
Newborn screening
References
Boy, N. et al. Newborn screening: A disease-changing intervention for glutaric aciduria type 1. Ann. Neurol 83, 970–979 (2018).
Kolker, S. et al. Natural history, outcome, and treatment efficacy in children and adults with glutaryl-CoA dehydrogenase deficiency. Pediatr. Res 59, 840–847 (2006).
Strauss, K. A., Puffenberger, E. G., Robinson, D. L. & Morton, D. H. Type I glutaric aciduria, part 1: natural history of 77 patients. Am. J. Med. Genet. C Semin. Med. Genet. 121C, 38–52 (2003).
Kolker, S. et al. The phenotypic spectrum of organic acidurias and urea cycle disorders. Part 1: the initial presentation. J. Inherited Metab. Dis. 38, 1041–1057 (2015).
Baric, I. et al. Sensitivity and specificity of free and total glutaric acid and 3-hydroxyglutaric acid measurements by stable-isotope dilution assays for the diagnosis of glutaric aciduria type I. J. Inherit. Metab. Dis. 22, 867–881 (1999).
Christensen, E., Ribes, A., Merinero, B. & Zschocke, J. Correlation of genotype and phenotype in glutaryl-CoA dehydrogenase deficiency. J. Inherit. Metab. Dis. 27, 861–868 (2004).
Harting, I. et al. (1)H-MRS in glutaric aciduria type 1: Impact of biochemical phenotype and age on the cerebral accumulation of neurotoxic metabolites. J. Inherit. Metab. Dis. 38, 829–838 (2015).
Boy, N. et al. Impact of newborn screening and quality of therapy on the neurological outcome in glutaric aciduria type 1: A meta-analysis. Genet. Med. 2, 2 (2020).
Boy, N. et al. Proposed recommendations for diagnosing and managing individuals with glutaric aciduria type I: Second revision. J. Inherit. Metab. Dis. 40, 75–101 (2017).
Heringer, J. et al. Use of guidelines improves the neurological outcome in glutaric aciduria type I. Ann Neurol 68, 743–752 (2010).
Kolker, S. et al. Diagnosis and management of glutaric aciduria type I–revised recommendations. J. Inherit. Metab. Dis. 34, 677–694 (2011).
Kolker, S. et al. Guideline for the diagnosis and management of glutaryl-CoA dehydrogenase deficiency (glutaric aciduria type I). J. Inherit. Metab. Dis. 30, 5–22 (2007).
Strauss, K. A. et al. Glutaric acidemia type 1: Treatment and outcome of 168 patients over three decades. Mol. Genet. Metab.s 2, 2 (2020).
Morton, D. H., Bennett, M. J., Seargeant, L. E., Nichter, C. A. & Kelley, R. I. Glutaric aciduria type I: a common cause of episodic encephalopathy and spastic paralysis in the Amish of Lancaster County, Pennsylvania. Am. J. Med. Genet. 41, 89–95 (1991).
Flehmig, I., Schloon, M., Uhde, J. & Bernuth, H. Denver-Entwicklungsskalen (Harburger Spastikerverein, 1973).
Lennon, E. M., Gardner, J. M., Karmel, B. Z. & Flory, M. J. Bayley Scales of Infant Development. In Language, Memory, and Cognition in Infancy and Early Childhood (eds Benson, J. B. & Haith, M. M.) (Academic Press, 2008).
Schneider, W. J. & McGrew, K. S. The Cattell-Horn-Carroll model of intelligence. Contemporary intellectual assessment: Theories, tests, and issues 3rd edn, 99–144 (The Guilford Press, 2012).
R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria [computer program] 2017.
Satterthwaite, F. An approximate distribution of estimates of variance components. Biometr. Bull. 2, 110–114 (1946).
Breiman, L., Friedman, J. H., Olshen, R. A. & Stone, C. J. Classification and Regression Trees (Wadsworth Inernat. Group, 1984).
Kolker, S. et al. Networking across borders for individuals with organic acidurias and urea cycle disorders: The E-IMD consortium. JIMD Rep 22, 29–38 (2015).
du Moulin, M. et al. Glutaric aciduria type 1 and acute renal failure: Case report and suggested pathomechanisms. JIMD Rep. 2, 2 (2017).
Kolker, S. et al. Decline of acute encephalopathic crises in children with glutaryl-CoA dehydrogenase deficiency identified by newborn screening in Germany. Pediatr. Res. 62, 357–363 (2007).
Boy, N. et al. Extrastriatal changes in patients with late-onset glutaric aciduria type I highlight the risk of long-term neurotoxicity. Orphanet. J. Rare Dis. 12, 77 (2017).
Martner, E. M. C. et al. Impact of interventional and non-interventional variables on anthropometric long-term development in glutaric aciduria type 1: A national prospective multi-centre study. J. Inherit. Metab. Dis. 44, 629–638 (2021).
Chen, Y. C. et al. Audiological and otologic manifestations of glutaric aciduria type I. Orphanet J. Rare Dis. 15, 337 (2020).
Serrano Russi, A. et al. Malignant brain tumors in patients with glutaric aciduria type I. Mol. Genet. Metab. 2, 2 (2018).
Boy, N. et al. A cross-sectional controlled developmental study of neuropsychological functions in patients with glutaric aciduria type I. Orphanet J. Rare Dis. 10, 163 (2015).
Brown, A., Crowe, L., Beauchamp, M. H., Anderson, V. & Boneh, A. Neurodevelopmental profiles of children with glutaric aciduria type I diagnosed by newborn screening: A follow-up case series. JIMD Rep 18, 125–134 (2015).
Tsai, F. C. et al. Experiences during newborn screening for glutaric aciduria type 1: Diagnosis, treatment, genotype, phenotype, and outcomes. J. Chin. Med. Assoc. 80, 253–261 (2017).
Zayed, H. et al. Clinical, biochemical, neuroradiological and molecular characterization of Egyptian patients with glutaric acidemia type 1. Metab. Brain Dis. 34, 1231–1241 (2019).
Kulkens, S. et al. Late-onset neurologic disease in glutaryl-CoA dehydrogenase deficiency. Neurology 64, 2142–2144 (2005).
Busanello, E. N. et al. Neurodevelopmental and cognitive behavior of glutaryl-CoA dehydrogenase deficient knockout mice. Life Sci. 92, 137–142 (2013).
Buerger, C. et al. Impairment of cognitive function in ornithine transcarbamylase deficiency is global rather than domain-specific and is associated with disease onset, sex, maximum ammonium, and number of hyperammonemic events. J. Inherit. Metab. Dis. 42, 243–253 (2019).
Leisman, G. & Melillo, R. The basal ganglia: Motor and cognitive relationships in a clinical neurobehavioral context. Rev. Neurosci. 24, 9–25 (2013).
Harting, I. et al. Dynamic changes of striatal and extrastriatal abnormalities in glutaric aciduria type I. Brain 132, 1764–1782 (2009).
Zschocke, J., Quak, E., Guldberg, P. & Hoffmann, G. F. Mutation analysis in glutaric aciduria type I. J. Med. Genet. 37, 177–181 (2000).
Sauer, S. W. et al. Bioenergetics in glutaryl-coenzyme A dehydrogenase deficiency: A role for glutaryl-coenzyme A. J. Biol. Chem. 280, 21830–21836 (2005).
Lamp, J. et al. Glutaric aciduria type 1 metabolites impair the succinate transport from astrocytic to neuronal cells. J. Biol. Chem. 286, 17777–17784 (2011).
Kolker, S. et al. Ca(2+) and Na(+) dependence of 3-hydroxyglutarate-induced excitotoxicity in primary neuronal cultures from chick embryo telencephalons. Pediatr. Res. 52, 199–206 (2002).
Kolker, S. et al. Potentiation of 3-hydroxyglutarate neurotoxicity following induction of astrocytic iNOS in neonatal rat hippocampal cultures. Eur. J. Neurosci. 13, 2115–2122 (2001).
Kolker, S., Ahlemeyer, B., Krieglstein, J. & Hoffmann, G. F. Contribution of reactive oxygen species to 3-hydroxyglutarate neurotoxicity in primary neuronal cultures from chick embryo telencephalons. Pediatr. Res. 50, 76–82 (2001).
Funk, C. B. et al. Neuropathological, biochemical and molecular findings in a glutaric acidemia type 1 cohort. Brain 128, 711–722 (2005).
Sauer, S. W. et al. Intracerebral accumulation of glutaric and 3-hydroxyglutaric acids secondary to limited flux across the blood-brain barrier constitute a biochemical risk factor for neurodegeneration in glutaryl-CoA dehydrogenase deficiency. J. Neurochem. 97, 899–910 (2006).
Dimitrov, B. et al. Organic acidurias: Major gaps, new challenges, and a yet unfulfilled promise. J. Inher. Metab. Dis. 2, 2 (2020).
Schmiesing, J. et al. Disease-linked glutarylation impairs function and interactions of mitochondrial proteins and contributes to mitochondrial heterogeneity. Cell Rep. 24, 2946–2956 (2018).
Biagosch, C. et al. Elevated glutaric acid levels in Dhtkd1-/Gcdh- double knockout mice challenge our current understanding of lysine metabolism. Biochim. Biophys. Acta Mol. Basis Dis. 1863, 2220–2228 (2017).
Leandro, J. et al. DHTKD1 and OGDH display substrate overlap in cultured cells and form a hybrid 2-oxo acid dehydrogenase complex in vivo. Hum. Mol. Genet. 29, 1168–1179 (2020).
Leandro, J. et al. Deletion of 2-aminoadipic semialdehyde synthase limits metabolite accumulation in cell and mouse models for glutaric aciduria type 1. J. Inherit. Metab. Dis. 2, 2 (2020).
Boy, N. et al. Low lysine diet in glutaric aciduria type I–effect on anthropometric and biochemical follow-up parameters. J. Inherit. Metab. Dis. 36, 525–533 (2013).
Acknowledgements
The authors thank the patients and their families for their participation in this study, and particularly the German patient supporting group ‘Glutaric aciduria e.V.’ (URL: www.glutarazidurie.de). The study was supported by grants from the German Ministry of Education and Research (BMBF; Metabnet; #01GM0305; 2003–2006, to SK); Kindness for Kids Foundation (GAIN: 2006–2008 and GAIN2: 2009–2010, both to SK), Munich, Germany; European Union (E-IMD; 2011–2014, to SK); Dietmar Hopp Foundation, St. Leon-Rot, Germany (LZO [2005–2009], NGS 2020 [2015–2020], and NGS 2025 [2020–2024], all to GFH and SK). None of the sponsors did at any time influence the design and conductance of the study, nor did they influence data analysis, interpretation and publication of results.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
S.K. initiated the study. E.M.C.M., S.K., and N.B. contributed to the conception and design of the study. Co-authors E.M.C.M., E.T., P.G., K.A.S., F.R., S.R., I.M., A.M.D., P.F., S.C.G., J.K., M.R.B., S.B., C.H., A.D., M.L., A.N., G.F.H., C.M., M.W., S.F.G,. E.M.M., S.K. and N.B. contributed to the acquisition and analysis of data and revised the manuscript for intellectual content. E.M.C.M., S.F.G., S.K., and N.B. contributed to drafting the text and preparing the figures.
Corresponding author
Ethics declarations
Competing interests
E. M. C. Märtner, E. Thimm, P. Guder, K. A. Schiergens, F. Rutsch, S. Roloff, I. Marquardt, A. M. Das, P. Freisinger, S. C. Grünert, J. Krämer, M. R. Baumgartner, S. Beblo, C. Haase, A. Dieckmann, M. Lindner, A. Näke, G. F. Hoffmann, C. Mühlhausen, M. Walter, S. F. Garbade, E. M. Maier, S. Kölker, and N. Boy declare no disclosures relevant to the manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article Nikolas Boy was incorrectly affiliated with ‘Division of Paediatric Neurology and Metabolic Medicine, Department of General Paediatrics, Centre for Paediatrics and Adolescent Medicine, University Hospital Heidelberg, 69120, Heidelberg, Germany’. The correct affiliation is ‘Division of Child Neurology and Metabolic Medicine, Centre for Child and Adolescent Medicine, University Hospital Heidelberg, Heidelberg, Germany’.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Märtner, E.M.C., Thimm, E., Guder, P. et al. The biochemical subtype is a predictor for cognitive function in glutaric aciduria type 1: a national prospective follow-up study. Sci Rep 11, 19300 (2021). https://doi.org/10.1038/s41598-021-98809-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98809-9
This article is cited by
-
Biochemical and molecular features of chinese patients with glutaric acidemia type 1 from Fujian Province, southeastern China
Orphanet Journal of Rare Diseases (2023)
-
Evaluierung und Optimierung des Neugeborenenscreenings mittels strukturierter Langzeitbeobachtung – am Beispiel der angeborenen Stoffwechselerkrankungen
Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2023)
-
Does glutaric aciduria type 1 affect hearing function?
Metabolic Brain Disease (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.