Abstract
Increased extracellular volume (ECV) by CMR is a marker of interstitial myocardial fibrosis and is associated with diastolic dysfunction in sickle cell anemia (SCA). Left atrial (LA) dysfunction and stiffness contribute to the development of diastolic heart failure in other settings. We aimed to evaluate LA function and stiffness associations with ECV, tricuspid regurgitation jet velocity (TRV) and exercise abnormalities in SCA. In a prospective study, individuals with SCA underwent CMR, echocardiography and exercise test. ECV was measured using MOLLI sequence. Atrial strain was studied in the 4- and 2-chamber views. LA stiffness was calculated as the ratio of echocardiographic E/e’-to-LA reservoir strain. Twenty-four participants with SCA were included (median age 20 years). ECV was increased in participant with SCA compared to our lab normal values (mean 0.44 ± 0.08 vs 0.26 ± 0.02, P < 0.0001). Six (25%) had LA LGE. ECV positively correlated with LA stiffness (r = 0.45, p = 0.04). There was a negative correlation between LA stiffness and %predicted VO2 (r = −0.50, p = 0.04). LA stiffness was moderately associated with increased TRV (r = 0.55, p < 0.005). LA stiffness is associated with ECV, exercise impairment and increased TRV. This study sheds insights on the interaction between LA function, RV hypertension, and myocardial fibrosis in SCA.
Similar content being viewed by others
Introduction
Sickle cell anemia (SCA) affects approximately 1 in 700 African-Americans, and as many as 100,000 individuals in the United States1. Cardiac complications are important causes of morbidity and mortality in SCA2,3. Diastolic dysfunction (DD) and pulmonary hypertension are known cardiac complications of SCA and are independent risk factors for early mortality4,5,6. DD is associated with microscopic, interstitial myocardial fibrosis in SCA mice and with diffuse myocardial fibrosis, assessed by cardiac MRI (CMR) using extracellular volume (ECV), in humans with SCA3,7,8.
Left atrial (LA) function has not been studied before in patients with SCA. Noninvasive comprehensive evaluation of LA function is now possible using strain Doppler echocardiography with reasonable accuracy9,10. Increased LA stiffness in patients with DD is associated with the development of heart failure and exercise impairment although that has not been studied in SCA9,11,12.
Here we sought to evaluate LA function in patients with SCA and determine any associations between LA stiffness and ECV, tricuspid regurgitation jet velocity (TRV) and exercise abnormalities.
Methods
Participants and study design
Participants with SCA were enrolled in a prospective, longitudinal CMR study to characterize SCA-related cardiomyopathy. Participants underwent a CMR and an echocardiogram and an optional CPET. The main exclusion criteria were chronic transfusion therapy and glomerular filtration rate <60 mL/min/1.73 m2. The study was approved by the Institutional Review Board of Cincinnati Children’s Hospital. Informed consent was obtained from adults or parents of minor participants13. All the methods were performed in accordance with the relevant guidelines and regulations.
CMR protocol and image analysis
CMR was performed on a 1.5 T scanner (Philips Ingenia, Best, Netherlands). ECV was measured from T1-maps acquired with a modified Look-Locker inversion recovery (MOLLI) sequence8. All planimetric and T1 analyses were done with Cvi42 (Circle Imaging; Alberta, Canada)13.
Participants, all of whom had abnormally increased ECV, were sub-classified by degree of elevation of ECV into two groups: first group (0.33–0.44) and second group (>0.44). The cutoff for ECV of 0.44 was the mean value for ECV in the entire SCA study population8. Baseline laboratory testing was obtained at the time of CMR including hemoglobin and N-terminal pro b-type natriuretic peptide (NT-proBNP).
Echocardiographic studies
Transthoracic echocardiography was performed with a Philips iE-33 system (Philips Electronics; Andover, MA). Measurements were analyzed using Syngo Dynamics (Siemens Healthcare, Germany). Pulsed-wave Doppler was used to measure mitral and tricuspid inflow peak velocity at early (E) and late filling (A) between the leaflet tips. Tissue Doppler imaging was used to determine mitral and tricuspid valve annular velocities in early (e’) and late diastole (a’) at both the septal and lateral annulus. Continuous-wave Doppler sampling of the peak TRV was used from parasternal and apical windows8. Increasing color gain and decreasing the color Doppler Nyquist limit were used as needed to clarify the tricuspid regurgitation jet and obtain an adequate Doppler wave form. Agitated saline injection was also used as needed. The highest TRV was recorded.
LA function
LA function was studied using two dimensional speckle tracking imaging14,15. Offline and blinded analysis to clinical outcomes was performed using TOMTEC software. The apical four-chamber and two chamber views were optimized for visualization of the LA. Patients with inadequate image quality were excluded. LA ejection fraction and fractional area change were calculated from echocardiography16. LA areas and volumes were derived in the apical four-chamber and two-chamber views using two-dimensional (Simpson’s method) echocardiography. LA ejection fraction was calculated as = [(maximal LA volume in ventricular systole just before mitral valve opening − minimal LA volume after mitral valve closure)/ maximal LA volume in ventricular systole just before mitral valve opening]16. The strain measurements were performed using the QRS complex (R-R gating) as the initiation of the strain calculation. There are two peaks in the strain curve. The first peak corresponds to reservoir function (first peak between R wave and T wave) and the second to atrial contractile function (starting on the P wave); the difference between reservoir strain and atrial contractile strain values reflects conduit function15. Positive global strain rate at the beginning of left ventricular systole reflects reservoir function. Early negative diastolic strain rate reflects conduit function while late diastolic global strain rate reflects pump function (Fig. 1)14,15. The E/e′ ratio (average e′) was also used in conjunction with the reservoir function strain to derive a noninvasive dimensionless parameter of LA stiffness9.
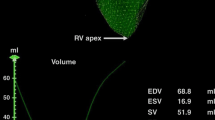
CPET
A maximal cardiopulmonary exercise was performed using an electronically braked cycle ergometer (Corival Load Cycle 400)13. Gas exchange at rest, during exercise, and during recovery was analyzed to determine measures of oxygen consumption (VO2), carbon dioxide production (VCO2), minute ventilation (VE), and VE/VCO2 slope17,18,19. Because peak VO2 is influenced by age, sex, and body weight, %predicted VO2 was used to account for these variables in our study20.
Reduced exercise capacity was defined as %predicted VO2 <80%. Mild impairment of exercise capacity was defined as %predicted VO2 60–80% while moderate-to-severe impairment was defined as %predicted VO2 <60%21.
Atrial late gadolinium enhancement (LGE)
LGE imaging was performed with a standard phase-sensitive inversion recovery sequence protocol 10 minutes after injection with gadolinium-diethylenetriamine penta-acetic acid8. LA LGE was assessed in the two chamber, three chamber and four chamber orientation (Fig. 2). The short axis stack did not extend to include the entire left atrium and thus quantification of fibrosis (Utah score) was not feasible16. Two cardiologists reviewed the images and agreed on the presence of LA LGE.
Statistical analysis
A student t-test or Mann-Whitney U test was used to compare 2 groups of continuous parametric or non-parametric variables, respectively, or Fisher’s exact test for categorical variables. Associations between normally distributed variables were calculated using the Pearson correlation coefficient. All P-values were two-tailed and differences were considered significant when P < 0.05. Statistical analyses were performed using JMP®, Version 12 from SAS Institute Inc. (Cary, NC).
Results
Patient characteristics and exercise performance
Twenty-six children and adults with SCA (homozygous HbSS) were enrolled, and 24 had adequate images to evaluate LA function by echocardiography and thus were included in the analysis. Twenty patients completed CPET. The median age was 20 years (range 7–61 years) (Table 1). ECV was increased in all SCA patients as compared to our lab normal control values (0.44 ± 0.08 vs 0.26 ± 0.02, P < 0.0001)8. Twelve patients had ECV > 0.44. There was no left or right ventricular LGE.
As previously reported, patients with SCA had significant exercise impairment (mean VO2 = 21.6 ± 6.1 ml/kg/min and mean %predicted VO2 = 57.0 ± 12.4%)13. Of the 18 patients who reached maximum exercise, 17 (94%) had reduced exercise capacity defined as %predicted VO2 <80%; of whom 5 (29%) had mild impairment (%predicted VO2 60–80%) and 12 (67%) had moderate-to-severe impairment (%predicted VO2 <60%). Hemoglobin positively correlated with exercise capacity (r = 0.45, p = 0.04).
Patients in the ECV >0.44 group had lower peak work rate on CPET (Table 2).
Atrial function and ECV
ECV negatively correlated with atrial ejection fraction (r = −0.42, p = 0.04). LA reservoir strain and positive global strain rate negatively correlated with ECV (r = −0.45, p = 0.02 and r = −0.40, p = 0.04). (Fig. 3) ECV was positively associated with LA stiffness (r = 0.45, p = 0.04). Patients in the ECV > 0.44 group had lower atrial ejection fraction, reservoir strain and positive strain rate as well as higher LA stiffness (Table 3). The ECV > 0.44 group had increased NT-Pro BNP and LA stiffness positively correlated with NT-pro BNP (r = 0.55, p = 0.003).
Atrial function and exercise capacity
There was a negative correlation between LA stiffness and %predicted VO2 (r = −0.50, p = 0.04) and a positive correlation between LA stiffness and VE/VCO2 slope at maximum exercise (r = 0.64, p = 0.02). (Fig. 4) Patients with moderate to severe exercise impairment had significantly higher LA stiffness as compared to patients with mild exercise impairment or normal exercise capacity (0.26 ± 0.10 vs 0.18 ± 0.05, p = 0.004).
LA function and tricuspid regurgitation jet velocity
There was a significant positive association of the LA stiffness and TRV (r = 0.55, p < 0.005). (Fig. 5)
Atrial function by echo and atrial volume by CMR
As expected, there was a strong correlation between CMR derived LA maximum volume and atrial end-diastolic (p = 0.008) and end systolic volumes by echocardiogram (p = 0.004). However, there was no association between atrial volume by CMR or echocardiogram and atrial function measures by echocardiogram. Absolute and indexed atrial volumes by CMR and echocardiogram did not correlate with exercise capacity or ECV.
Atrial late gadolinium enhancement
Six of the 24 participants (25%) had LA LGE (Fig. 2). When participants were dichotomized based on the presence of LA LGE we did not find a significant difference in exercise capacity or LA functional measures.
Discussion
We have shown that diffuse myocardial fibrosis, defined by increased ECV, in individuals with SCA is associated with LA dysfunction. LA stiffness was associated with both reduced exercise capacity and increased TRV, which is a predictor for early mortality in adults with SCA6,22. We also observed macroscopic LA fibrosis by LGE in 6 of the 24 participants. To our knowledge, this is the first report of impaired LA function in SCA and its association with diffuse myocardial fibrosis, exercise capacity and TRV.
LA enlargement is a predictor of adverse cardiovascular outcomes in other diseases23. In patients with SCA, chronic LA enlargement is common and is likely due to a combination of DD and the chronic increase in cardiac output to meet the oxygen demand8,13,24. In our study we found that the atrial function measures rather than the size of the LA correlated with ventricular fibrosis, TRV and exercise capacity which is likely due to the multifactorial etiology of LA enlargement. LA enlargement may result in LA mechanical and electrical remodeling25. Progressive atrial dilation may eventually reach a threshold fiber length where atrial shortening and contractility will begin to decline. In addition, LA enlargement is associated with an increased risk for arrhythmia26. With recent advances in non-invasive technologies, reliable assessment of the LA function is now possible using speckle tracking imaging25.
We found that with increasing left ventricular ECV (i.e., increasing ventricular interstitial fibrosis), the LA stiffness increases and atrial ejection fraction and reservoir function decrease. LA and the LV have a dynamic interaction which is described in many disease states27,28. Our previous work showed an association between ECV and DD in SCA8,13. It is also possible that chronic volume overload contributes to ventricular and atrial remodeling and impaired function29. Previous animal studies showed myocardial fibrosis and LA enlargement in SCA mice but not in mice with iron deficiency anemia suggesting that anemia and volume overload are not the main mechanism for LA enlargement and increased ECV in SCA30.
The association between LA stiffness and TRV in this study is notable. Previous studies suggested that LA function is an important predictor of pulmonary hypertension in cases of LA volume overload such as mitral regurgitation31. In patients with LV diastolic dysfunction, LA stiffness is also associated with the development of symptomatic heart failure and pulmonary hypertension9. In SCA, both increased preload, due to chronic increased cardiac output, and afterload, due to left ventricular DD, result in atrial stiffness and may contribute to post-capillary pulmonary hypertension in this population4,24,32,33. Thus LA stiffness may be a significant marker of myocardial disease in SCA.
Impairment of exercise tolerance is common in children and young adults with SCA, but the degree to which cardiopulmonary disease contribute to this impairment is not known18,34,35. Our study demonstrates a negative association between LA stiffness and exercise capacity as measured by %predicted VO2 and with ventilation efficiency measured by VE/VCO2 slope. This suggests that increased LA stiffness may be associated with lower cardiac output or with increased pulmonary capillary wedge pressure and increased pulmonary congestion resulting in decreased exercise capacity4,32. LA stiffness index reflects the interaction between left ventricular compliance and LA reservoir function36. Interestingly, LA volume by CMR and echocardiogram did not correlate with ECV, TRV or exercise capacity in our study, likely because of the confounding effect of volume overload in SCA. The increase in LA stiffness and the decrease in LA compliance may be an early precursor for the development of elevated right ventricular pressure in SCA individuals with DD37,38. Further studies are needed to elucidate that.
We found LA LGE in 6 participants. LA LGE is linked to the development of atrial arrhythmia in other patient populations39. Dysrhythmias, including atrial arrhythmias, have been linked to premature death and are poorly understood in SCA2,40. In our study LA LGE did not correlate with LA strain or with any outcomes and this could be due to the small sample size and the technical limitations of our LA LGE technique. The LA LGE findings in our study should be interpreted with care, because our CMR was not originally obtained to evaluate for atrial LGE, which was an incidental finding. Many technical improvements are necessary to accurately assess LGE in the thin LA wall41. The significance of these findings will be the focus of future studies.
Our study has several limitations. First, this is a relatively small sample that may limit the interpretation of the correlations between variables and prevent the use of multivariate analysis. Despite the small sample size, the findings of this study are novel and can be the basis of larger confirmatory and mechanistic studies. Second, this study included a wide age range (6–60) years. As SCA is a life-long disease, including a wide age range was felt to be appropriate and necessary for an initial study, but multiple age subgroups were too small for meaningful analysis.
Third, our original study design was focused on ventricular evaluation. Short axis post contrast views of the LA were not acquired and quantitative assessment of LA LGE was not possible. In addition, our study does not address if LA stiffness is secondary to LV fibrosis-related DD, LA fibrosis, or both.
In summary, we have shown that LA stiffness is associated with elevated TRV and poor exercise capacity in children and adults with SCA. LA dysfunction is also associated with ventricular ECV, suggesting that LV diffuse interstitial myocardial fibrosis may lead to impaired LA function and subsequently to elevated pulmonary pressures (Fig. 6). The therapeutic targeting of both atrial stiffness and ventricular fibrosis to potentially ameliorate cardiac complications and improve outcomes in SCA are needed.
Change history
12 March 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Hassell, K. L. Population estimates of sickle cell disease in the U.S. Am J Prev Med 38, S512–521, https://doi.org/10.1016/j.amepre.2009.12.022 (2010).
Fitzhugh, C. D. et al. Cardiopulmonary complications leading to premature deaths in adult patients with sickle cell disease. American journal of hematology 85, 36–40, https://doi.org/10.1002/ajh.21569 (2010).
Bakeer, N. et al. Sickle cell anemia mice develop a unique cardiomyopathy with restrictive physiology. Proc Natl Acad Sci USA, https://doi.org/10.1073/pnas.1600311113 (2016).
Sachdev, V. et al. Diastolic dysfunction is an independent risk factor for death in patients with sickle cell disease. J Am Coll Cardiol 49, 472–479, https://doi.org/10.1016/j.jacc.2006.09.038 (2007).
Machado, R. F. et al. N-terminal pro-brain natriuretic peptide levels and risk of death in sickle cell disease. JAMA 296, 310–318, https://doi.org/10.1001/jama.296.3.310 (2006).
Gladwin, M. T. et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. The New England journal of medicine 350, 886–895, https://doi.org/10.1056/NEJMoa035477 (2004).
Riesenkampff, E., Messroghli, D. R., Redington, A. N. & Grosse-Wortmann, L. Myocardial T1 mapping in pediatric and congenital heart disease. Circ Cardiovasc Imaging 8, e002504, https://doi.org/10.1161/CIRCIMAGING.114.002504 (2015).
Niss, O. et al. Association between diffuse myocardial fibrosis and diastolic dysfunction in sickle cell anemia. Blood 130, 205–213, https://doi.org/10.1182/blood-2017-02-767624 (2017).
Kurt, M., Wang, J., Torre-Amione, G. & Nagueh, S. F. Left atrial function in diastolic heart failure. Circ Cardiovasc Imaging 2, 10–15, https://doi.org/10.1161/CIRCIMAGING.108.813071 (2009).
Hoit, B. D. Left atrial size and function: role in prognosis. Journal of the American College of Cardiology 63, 493–505, https://doi.org/10.1016/j.jacc.2013.10.055 (2014).
Habibi, M. et al. Cardiac Magnetic Resonance-Measured Left Atrial Volume and Function and Incident Atrial Fibrillation: Results From MESA (Multi-Ethnic Study of Atherosclerosis). Circ Cardiovasc Imaging 9, https://doi.org/10.1161/CIRCIMAGING.115.004299 (2016).
von Roeder, M. et al. Influence of Left Atrial Function on Exercise Capacity and Left Ventricular Function in Patients With Heart Failure and Preserved Ejection Fraction. Circ Cardiovasc Imaging 10, https://doi.org/10.1161/CIRCIMAGING.116.005467 (2017).
Alsaied, T. et al. Diastolic dysfunction is associated with exercise impairment in patients with sickle cell anemia. Pediatric blood & cancer 65, e27113, https://doi.org/10.1002/pbc.27113 (2018).
Rimbas, R. C., Dulgheru, R. E. & Vinereanu, D. Methodological Gaps in Left Atrial Function Assessment by 2D Speckle Tracking Echocardiography. Arquivos brasileiros de cardiologia 105, 625–636, https://doi.org/10.5935/abc.20150144 (2015).
Pathan, F., D’Elia, N., Nolan, M. T., Marwick, T. H. & Negishi, K. Normal Ranges of Left Atrial Strain by Speckle-Tracking Echocardiography: A Systematic Review and Meta-Analysis. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography 30, 59–70 e58, https://doi.org/10.1016/j.echo.2016.09.007 (2017).
Kuppahally, S. S. et al. Left atrial strain and strain rate in patients with paroxysmal and persistent atrial fibrillation: relationship to left atrial structural remodeling detected by delayed-enhancement MRI. Circ Cardiovasc Imaging 3, 231–239, https://doi.org/10.1161/CIRCIMAGING.109.865683 (2010).
Gitt, A. K. et al. Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation 106, 3079–3084 (2002).
Liem, R. I. et al. Reduced fitness and abnormal cardiopulmonary responses to maximal exercise testing in children and young adults with sickle cell anemia. Physiol Rep 3, https://doi.org/10.14814/phy2.12338 (2015).
Balady, G. J. et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation 122, 191–225, https://doi.org/10.1161/CIR.0b013e3181e52e69 (2010).
Arena, R. et al. Determining the preferred percent-predicted equation for peak oxygen consumption in patients with heart failure. Circulation. Heart failure 2, 113–120, https://doi.org/10.1161/CIRCHEARTFAILURE.108.834168 (2009).
Stelken, A. M. et al. Prognostic value of cardiopulmonary exercise testing using percent achieved of predicted peak oxygen uptake for patients with ischemic and dilated cardiomyopathy. Journal of the American College of Cardiology 27, 345–352 (1996).
Mehari, A. et al. Hemodynamic predictors of mortality in adults with sickle cell disease. American journal of respiratory and critical care medicine 187, 840–847, https://doi.org/10.1164/rccm.201207-1222OC (2013).
Tsang, T. S. et al. Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J Am Coll Cardiol 47, 1018–1023, https://doi.org/10.1016/j.jacc.2005.08.077 (2006).
Niss, O. et al. Cardiomyopathy With Restrictive Physiology in Sickle Cell Disease. JACC Cardiovasc Imaging, https://doi.org/10.1016/j.jcmg.2015.05.013 (2016).
Blume, G. G. et al. Left atrial function: physiology, assessment, and clinical implications. European journal of echocardiography: the journal of the Working Group on Echocardiography of the European Society of Cardiology 12, 421–430, https://doi.org/10.1093/ejechocard/jeq.175 (2011).
Okamoto, M. et al. Effects of volume loading on left atrial systolic time intervals. Journal of clinical ultrasound: JCU 19, 405–411 (1991).
Thomas, L. et al. Compensatory changes in atrial volumes with normal aging: is atrial enlargement inevitable? J Am Coll Cardiol 40, 1630–1635 (2002).
Abhayaratna, W. P. et al. Left atrial reservoir function as a potent marker for first atrial fibrillation or flutter in persons> or = 65 years of age. Am J Cardiol 101, 1626–1629, https://doi.org/10.1016/j.amjcard.2008.01.051 (2008).
Henein, M. Y., Holmgren, A. & Lindqvist, P. Left atrial function in volume versus pressure overloaded left atrium. Int J Cardiovasc Imaging 31, 959–965, https://doi.org/10.1007/s10554-015-0638-6 (2015).
Bakeer, N. et al. Sickle cell anemia mice develop a unique cardiomyopathy with restrictive physiology. Proceedings of the National Academy of Sciences of the United States of America 113, E5182–5191, https://doi.org/10.1073/pnas.1600311113 (2016).
Ratanasit, N., Karaketklang, K. & Krittayaphong, R. Left atrial volume index as an independent determinant of pulmonary hypertension in patients with chronic organic mitral regurgitation. BMC Cardiovasc Disord 16, 141, https://doi.org/10.1186/s12872-016-0306-3 (2016).
Sachdev, V. et al. Echocardiographic markers of elevated pulmonary pressure and left ventricular diastolic dysfunction are associated with exercise intolerance in adults and adolescents with homozygous sickle cell anemia in the United States and United Kingdom. Circulation 124, 1452–1460, https://doi.org/10.1161/CIRCULATIONAHA.111.032920 (2011).
Shen, J. et al. Evaluation of left atrial function in patients with iron-deficiency anemia by two-dimensional speckle tracking echocardiography. Cardiovasc Ultrasound 14, 34, https://doi.org/10.1186/s12947-016-0078-z (2016).
Hostyn, S. V., Carvalho, W. B., Johnston, C. & Braga, J. A. Evaluation of functional capacity for exercise in children and adolescents with sickle-cell disease through the six-minute walk test. Jornal de pediatria 89, 588–594, https://doi.org/10.1016/j.jped.2013.04.005 (2013).
van Beers, E. J. et al. Exercise tolerance, lung function abnormalities, anemia, and cardiothoracic ratio in sickle cell patients. American journal of hematology 89, 819–824, https://doi.org/10.1002/ajh.23752 (2014).
Nagueh, S. F. et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17, 1321–1360, https://doi.org/10.1093/ehjci/jew082 (2016).
Machino-Ohtsuka, T. et al. Left atrial stiffness relates to left ventricular diastolic dysfunction and recurrence after pulmonary vein isolation for atrial fibrillation. Journal of cardiovascular electrophysiology 22, 999–1006, https://doi.org/10.1111/j.1540-8167.2011.02049.x (2011).
Shaikh, A. Y. et al. Speckle echocardiographic left atrial strain and stiffness index as predictors of maintenance of sinus rhythm after cardioversion for atrial fibrillation: a prospective study. Cardiovasc Ultrasound 10, 48, https://doi.org/10.1186/1476-7120-10-48 (2012).
Higuchi, K. et al. The Spatial Distribution of Late Gadolinium Enhancement of Left Atrial Magnetic Resonance Imaging in Patients With Atrial Fibrillation. JACC Clin Electrophysiol 4, 49–58, https://doi.org/10.1016/j.jacep.2017.07.016 (2018).
Maisel, A., Friedman, H., Flint, L., Koshy, M. & Prabhu, R. Continuous electrocardiographic monitoring in patients with sickle-cell anemia during pain crisis. Clinical cardiology 6, 339–344 (1983).
Siebermair, J., Kholmovski, E. G. & Marrouche, N. Assessment of Left Atrial Fibrosis by Late Gadolinium Enhancement Magnetic Resonance Imaging: Methodology and Clinical Implications. JACC Clin Electrophysiol 3, 791–802, https://doi.org/10.1016/j.jacep.2017.07.004 (2017).
Acknowledgements
This study is supported by the NIH-NHLBI Excellence in Hemoglobinopathy Research Award (EHRA) program (U01HL117709) (PM and CTQ). ON and TA were recipients of the U01HL117709 Translational Research Scholar Award. TA was the recipient of Cincinnati Children’s Strauss Research Award. This study is supported by the National Institution of Health Excellence in Hemoglobinopathy Research Award (EHRA) program (U01HL117709) (PM and CTQ). ON and TA ware recipients of the U01HL117709 Translational Research Scholar Award. TA was the recipient of the Arnold Strauss Research Award from Cincinnati Children’s hospital. We thank Sandy Knecht, Katie Lehmkuhl, Stephanie Stewart, Lauren Longshore and Kaylee Wright who performed the echocardiogram and exercise stress testing. We also thank Courtney Little, Eileen Beckman and Amy Shova for assistance with recruitment of participants and collection of clinical data.
Author information
Authors and Affiliations
Contributions
All author participated in study design and approved the final draft. Tarek Alsaied did data echo collection and analysis, wrote first draft. Omar Niss did hematology data collection and analysis, reviewed and appraised the first draft. Justin Tretter helped with MRI data collection, helped with study design and approved final draft. Adam Powell collected exercise data, analyzed it and helped with manuscript writing. Clifford Chin helped in the study design, analyzed exercise data and edited the manuscript. Robert J. Fleck helped in the study design, analyzed MRI data and edited the manuscript. James F. Cnota helped in the study design, analyzed echo data and edited the manuscript. Punam Malik helped in the study design, analyzed hematology data and edited the manuscript. Charles T. Quinn helped in the study design, analyzed hematology data and edited the manuscript. Sherif F. Nagueh helped in the study design, analyzed echo data and edited the manuscript. Michael D. Taylor helped in the study design, analyzed MRI data and edited the manuscript. Wojciech M. Mazur helped in the study design, analyzed MRI and echo data and edited the manuscript. He was the senior author on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alsaied, T., Niss, O., Tretter, J.T. et al. Left atrial dysfunction in sickle cell anemia is associated with diffuse myocardial fibrosis, increased right ventricular pressure and reduced exercise capacity. Sci Rep 10, 1767 (2020). https://doi.org/10.1038/s41598-020-58662-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-58662-8
This article is cited by
-
Evaluation of cardiac fibrosis and subclinical cardiac changes in children with sickle cell disease using magnetic resonance imaging, echocardiography, and serum galectin-3
Pediatric Radiology (2023)
-
Cardiac pathophysiology in sickle cell disease
Journal of Thrombosis and Thrombolysis (2021)
-
Atrial Reservoir Strain is Associated with Decreased Cardiac Index and Adverse Outcomes Post Fontan Operation
Pediatric Cardiology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.