Abstract
Invasive ductal carcinoma (IDC) often presents alone or with a co-existing ductal carcinoma in situ component (IDC + DCIS). Studies have suggested that pure IDC may exhibit different biological behavior than IDC + DCIS, but whether this translates to a difference in outcomes is unclear. Here, utilizing the National Cancer Database we identified 494,801 stage I-III breast cancer patients diagnosed with either IDC alone or IDC + DCIS. We found that IDC + DCIS was associated with significantly better overall survival (OS) compared to IDC alone (5-year OS, 89.3% vs. 85.5%, p < 0.001), and this finding persisted on multivariable Cox modeling adjusting for demographic, clinical, and treatment-related variables. The significantly superior OS observed for IDC + DCIS was limited to patients with invasive tumor size < 4 cm or with node negative disease. A greater improvement in OS was observed for tumors containing ≥25% DCIS component. We also found IDC + DCIS to be associated with lower T/N stage, low/intermediate grade, ER/PR positivity, and receipt of mastectomy. Thus, the presence of a DCIS component in patients with IDC is associated with favorable clinical characteristics and independently predicts improved OS. IDC + DCIS could be a useful prognostic factor for patients with breast cancer, particularly if treatment de-escalation is being considered for small or node negative tumors.
Similar content being viewed by others
Introduction
Ductal carcinoma in situ (DCIS) is an established precursor to invasive breast cancer and often co-exists pathologically with invasive ductal carcinoma (IDC)1,2,3. Currently, treatment paradigms for such cases of IDC with a DCIS component (IDC + DCIS) are similar to those for pure IDC alone, with the extent and characteristics of invasive disease driving clinical decisions4. It remains unclear, however, whether survival outcomes are similar for IDC when it presents alone or is accompanied by co-existing DCIS.
Studies have explored whether IDC + DCIS may be biologically distinct from IDC alone5,6,7,8,9. It has been hypothesized that tumors present as combined IDC + DCIS when the progression from pre-invasive DCIS to IDC is delayed – a sign of reduced biological aggressiveness6. In contrast, tumors presenting as IDC alone may have achieved invasive potential early in the process of carcinogenesis, leaving little or no evidence of the pre-invasive state. Indeed, prior studies have demonstrated that IDC + DCIS tumors are associated with favorable clinical characteristics such as smaller tumor size, lower tumor grade, lower Ki-67 staining, greater ER-positivity, and reduced risk of local recurrence when compared to IDC alone5,6,7,8,9. While trends towards improved overall survival (OS) have been previously observed with IDC + DCIS versus IDC alone5,6,9, the limited sample sizes of prior studies likely did not provide sufficient power to detect a statistically significant OS difference.
Here, we took advantage of the large data set available in the National Cancer Database (NCDB) to assess whether significant differences in OS exist between patients with IDC alone versus those with IDC + DCIS. The large sample size also enabled us to investigate whether the effect of DCIS on survival differed when patients were categorized by the size of their invasive tumor component, nodal stage, or extent of the DCIS component.
Methods
Data source
Patient data were obtained from the NCDB, which is a nationwide, hospital-based patient registry established as a joint project of the American College of Surgeons Commission on Cancer and the American Cancer Society. The NCDB captures approximately 70% of all new cancer diagnoses in the United States. A de-identified NCDB file was used to obtain data for this study. This work has not been verified by the American College of Surgeons or the American Cancer Society and these societies are not responsible for the methodology or conclusions drawn from this work.
Study population
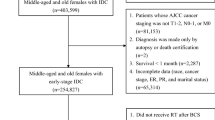
Clinical stage I-III breast cancer patients diagnosed from 2004 to 2013 were identified in the NCDB. Patients were required to have histologically-confirmed invasive ductal carcinoma and no prior cancer diagnosis. A total of 648,210 patients met these initial criteria. Figure 1 shows the inclusion and exclusion criteria that resulted in our main study cohort of 494,801 patients. All patients underwent lumpectomy or mastectomy with or without axillary lymph node dissection.
Patients were excluded if any of the following parameters were coded as unknown: clinical T or N stage, pathologic surgical margin status, tumor grade, estrogen receptor (ER) and progesterone receptor (PR) status, receipt of any treatment variables (radiation, chemotherapy, or hormone therapy), or if it was unknown whether a DCIS component was present (using the CS Site-Specific Factor 6 variable within the NCDB participant user file). Patients with positive margins were excluded, as the NCDB dataset did not specify whether this referred to positive invasive or in situ margins. Her2 was not consistently reported within the NCDB prior to 2010, thus unknown Her2 status was not used as an exclusion criterion.
Statistical analysis
Univariable logistic regression was used to calculate unadjusted odds ratios (ORs) for the diagnosis of IDC alone versus IDC + DCIS based on categorized baseline clinical and pathologic factors. Factors included patient age (<60 vs. ≥60 years), race/ethnicity (white vs. non-white); Charlson-Deyo co-morbidity score (0 vs. ≥1); clinical T stage (T1 vs. T2, T3, or T4) and N stage (N0 vs. N1, N2, or N3); ER (positive vs. negative), PR (positive vs. negative), and Her2 (negative vs. positive or unknown) receptor status; surgical type (partial mastectomy vs. mastectomy); and tumor grade (low/intermediate vs. high). As the extent of surgery could affect the available tissue for pathological examination, surgical type was included in the Cox regression. Other treatment variables (radiation therapy, chemotherapy, hormone therapy), were excluded from OR calculations as these treatments are typically prescribed after the diagnosis of IDC alone or IDC + DCIS would have been made. Factors with a trend towards significance (p < 0.10) were included in a multivariable regression analysis. A factor was considered to be a statistically significant predictor of diagnosis of IDC alone versus IDC + DCIS if p < 0.05. Patients with missing data (eg. Her2 status) were included in univariable and multivariable analyses using an “unknown” dummy variable. A sensitivity analysis was performed in which patient age was either used as a continuous variable or dichotomized at age 40, 50, 70, or 80 to evaluate the impact on results of the multivariable Cox regression.
OS was compared between IDC alone and IDC + DCIS groups using the Kaplan-Meier method and log-rank test. Univariable and multivariable Cox regressions were used to calculate unadjusted and adjusted hazard ratios (HRs) for survival, respectively. As described above, all clinical and pathologic variables with p < 0.10 on univariable analysis were included in the multivariable model. The proportional hazards assumption was checked graphically using log-log survival plots.
To further examine survival differences between patients with IDC alone versus IDC + DCIS, four additional analyses were performed. The first was conducted on patients with known size of the invasive tumor component, excluding any tumors ≥7 cm as it was felt these large tumor sizes represented coding errors. Patients were categorized to the following invasive tumor size groups: <1 cm, 1 to <2 cm, 2 to <3 cm, 3 to <4 cm, 4 to <5 cm, or 5 to <7 cm. A second analysis was performed by categorizing patients based on clinical node status: N0, N1, N2, or N3. A third analysis evaluated patients when grouped into the following 3 biologic subtypes: (1) ER or PR positive, Her2 negative; (2) triple negative; (3) Her2 positive. Finally, a fourth analysis was performed among patients for which the extent of DCIS was known to be “minimal” or “extensive” (defined as a DCIS component of <25% or ≥25% of the total tumor size, respectively). While an extensive intraductal component (EIC) has been associated with higher rates of local recurrence when margins are positive10,11,12,13, our study cohort was limited to patients with negative margins. Of note, the CS Site-Specific Factor 6 variable in the NCDB either codes patients by known invasive tumor component size or by extent of DCIS, but not both. Thus, the IDC + DCIS patients analyzed by invasive tumor size or by extent of DCIS represented independent cohorts. For the first three subgroup analyses, independent multivariable Cox regressions were performed to calculate adjusted HRs (aHRs) for IDC + DCIS versus IDC alone for each group. The Kaplan-Meier method and log-rank test were used for the fourth subgroup to compare OS between patients with a minimal DCIS component, extensive DCIS, or IDC alone.
STATA/SE version 13.1 (Stata Corp, College Station, TX) was used for all statistical analyses. All tests were two-sided, and a p value of <0.05 was considered statistically significant.
Ethics approval and informed consent
The National Cancer Database provides a Participant Use Data File (PUF) which is compliant with the Health Insurance Portability and Accountability Act (HIPAA). Data in the PUF are de-identified with regards to the patient and treatment facility. Institutional Review Board (IRB) approval was not required.
Results
Patient and tumor characteristics
We identified a total of 494,801 stage I-III breast cancer patients with either IDC alone or IDC + DCIS who met study inclusion criteria (Fig. 1). Patient demographic and clinical-pathologic characteristics are shown in Table 1. Median follow-up was 4.5 years. Fewer patients were diagnosed with IDC alone (168,838 patients; 34%) than with IDC + DCIS (325,963 patients; 66%). The median age for the study cohort was 59.7 years. The majority of patients were white (74.9%), with T1 (65.8%) and N0 (82.7%) tumors, with receptor status ER positive (78.3%), and PR positive (68.9%). Among patients with known Her2 status, the majority had Her2 negative disease (83.3%). Partial mastectomy was performed in 61.6% of patients while 38.4% received mastectomy. The majority of patients received radiation therapy (65.9%) and hormonal therapy (73.7%). Approximately one half of patients (48.9%) received chemotherapy. The receipt of radiation and systemic therapies in the setting of partial or total mastectomy are presented for node-positive and node-negative patients in Supplementary Table 1.
Factors associated with the presence of a dcis component
Factors which were statistically associated with IDC + DCIS diagnosis versus IDC alone on multivariable analysis included: age <60 years, lower T and N stage, ER positivity, PR positivity, and lower tumor grade (Table 2). Patients who underwent mastectomy versus partial mastectomy were more likely to have a diagnosis of IDC + DCIS. Patient race/ethnicity and Charlson-Deyo co-morbidity score were not significant on multivariable analysis (Table 2).
Overall Survival for patients with IDC alone versus IDC + DCIS
In the primary cohort, the presence of IDC + DCIS was associated with significantly improved OS compared to IDC alone on univariable analysis (5-year OS, 89.3% vs. 85.5, p < 0.001; hazard ratio [HR], 0.74; 95% CI, 0.73–0.75, p < 0.001) (Fig. 2). A total of 14 variables were included in our multivariable Cox survival model: tumor histology (IDC vs. IDC + DCIS), age, race/ethnicity, Charlson-Deyo score, clinical T and N stage, ER status, PR status, Her2 status, surgery type, radiation therapy receipt, chemotherapy receipt, hormone therapy receipt, and tumor grade. When adjusting for these factors, IDC + DCIS remained associated with improved OS (HR 0.91, 95% CI 0.89–0.92, p < 0.001) (Table 3). Sensitivity analysis showed IDC + DCIS to remain significantly associated with improved OS when age was analyzed as a continuous variable or dichotomized at cut-points of 40, 50, 60, 70, or 80 years (data not shown).
Survival outcomes based on invasive tumor size and nodal status
For patients in whom the invasive tumor size was known (85.3% of the cohort; 422,227 patients) we repeated the analysis using our multivariable model after categorizing patients into one of six invasive tumor size groups: <1 cm, 1 to <2 cm, 2 to <3 cm, 3 to <4 cm, 4 to <5 cm, or 5 to <7 cm (Supplementary Table 2). As shown in Fig. 3a, OS was better for IDC + DCIS compared to IDC alone for the categories of patients with invasive tumor size less than 4 cm (<1 cm: HR, 0.87; 95% CI, 0.82–0.91; p < 0.001; 1 to <2 cm: HR, 0.89; 95% CI, 0.86–0.92; p < 0.001; 2 to <3 cm: HR, 0.94; 95% CI, 0.90–0.97; p < 0.001; 3 to <4 cm: HR, 0.95; 95% CI, 0.91–0.99; p = 0.049). For invasive tumors categorized as 4 cm or larger, survival outcomes between patients with IDC + DCIS and IDC alone were not statistically different.
Survival trends based on tumor size and nodal status. Adjusted hazard ratios illustrating the effect of IDC alone vs. IDC + DCIS on overall survival when patients were categorized by (a) size of invasive component and (b) nodal stage. Abbreviations: CI, confidence interval; DCIS, ductal carcinoma in situ; IDC, invasive ductal carcinoma; IDC + DCIS, invasive ductal carcinoma with ductal carcinoma in situ.
The association of OS with IDC + DCIS versus IDC alone was also tested in our multivariable survival model when categorizing patients based on clinical node status (N0, N1, N2, or N3). Figure 3b shows that OS was improved with IDC + DCIS for patients with N0 disease (HR, 0.88; 95% CI, 0.86–0.90; p < 0.001), but not for patients with node positive (N1–N3) disease.
Association of survival with extent of DCIS and biologic subtype
Finally, we examined whether the extent of the DCIS component or biologic subtype influenced survival outcomes. Patients with IDC + DCIS with either a low (<25%) or extensive (≥25%) DCIS component were compared to patients with IDC alone. As local recurrence rates have been observed to be higher with an extensive intraductal component (EIC) unless appropriate resection with negative margins is achieved10,12,13, it is important to note that all patients had negative margins. Characteristics of the extent of DCIS are presented in Supplementary Table 3. Indeed, OS was better for patients who had a higher proportion of DCIS (Fig. 4), with 5-year OS rates of 85.5%, 88.5%, and 90.0% for IDC alone, low DCIS, and extensive DCIS, respectively (p < 0.001 for all comparisons). Supplementary Table 4 shows the biologic subtype among those patients for which ER, PR, and Her2 status are known. Interestingly, while IDC + DCIS was associated with improved survival for patients who were (1) ER or PR positive and Her2 negative or (2) Her2 positive, this was not seen for patients with triple negative disease (Supplementary Fig. 1).
Discussion
In this study we show that for patients with IDC, the presence of an accompanying DCIS component is associated with favorable prognostic features and confers a statistically significant improvement in OS. Our finding that IDC + DCIS is associated with lower clinical stage, lower tumor grade, and greater ER and PR positivity is consistent with prior studies5,6,7,8. Despite these observed differences in tumor characteristics, however, prior studies failed to demonstrate a significant improvement in OS for patients with IDC + DCIS versus IDC alone, likely due to limited statistical power. The large size of our study, with nearly 500,000 patients, allowed us to identify a significant OS difference, and to also examine whether factors such as invasive tumor size and nodal status influence survival outcomes. We find that the association of IDC + DCIS with improved OS dissipates upon reaching 4 cm of invasive disease or node positivity, suggesting that at a given threshold of disease burden, a DCIS component is no longer predictive of improved survival.
The presence of an extensive intraductal component has traditionally been viewed as a negative prognostic factor for local recurrence in the setting of breast conservation14,15,16, likely due to the burden of residual DCIS in the breast11. In the setting of appropriate surgery with negative margins, however, the local recurrence risk with EIC is similar to that of non-EIC patients10,12,13. In our analysis of patients with negative margins, we find that OS rates are actually better when an extensive intraductal component (≥25% DCIS) is present compared to patients with a low (<25%) intraductal component. Patients with either extensive or low intraductal components had higher OS than those with IDC alone. These observations suggest that tumors with larger proportions of DCIS may indeed be less biologically aggressive.
Existing evidence suggests that biological differences may exist between breast cancers which present as IDC + DCIS versus IDC alone6. Extensive analyses of breast cancer genomics by The Cancer Genome Atlas (TCGA) Network and others have identified distinct molecular subtypes of breast cancer, but these have focused on IDC and have not explicitly evaluated situations when IDC is accompanied by DCIS17,18,19. The presence of appreciable in situ disease may indicate that a tumor underwent many cell divisions before a subclone evolved to acquire an invasive phenotype. One might speculate that slower evolution to invasiveness could be a mark of reduced genomic instability, which is known to portend a more favorable prognosis20,21,22. While our data are consistent with the hypothesis that IDC + DCIS may be inherently less biologically aggressive, the molecular underpinnings for these findings remain unknown. In fact, while our findings appear most applicable to patients with hormone receptor or Her2 positive disease, triple negative tumors may exhibit different behavior.
Can our findings prove useful in clinical practice? There is a growing interest to identify patient populations for which breast cancer treatment can be de-intensified. Among patients with DCIS alone, recent studies have identified patients at highest risk for progression to invasive disease23,24,25. For example, after publication of CALGB 9343, the National Comprehensive Cancer Network (NCCN) changed guidelines to support the omission of adjuvant RT in elderly patients with favorable disease26,27. Modern studies, such as the IDEA Study (Individualized Decisions for Endocrine Therapy Alone) and TAILORx (Trial Assigning Individualized Options for Treatment), have explored whether patients may omit adjuvant RT or adjuvant chemotherapy, respectively, in the context of favorable gene-expression molecular profiles28,29. Although the survival difference we observe between IDC and IDC + DCIS is small, the presence of accompanying DCIS could be considered for incorporation as an additional factor in predictive models to further refine the selection of patients eligible for treatment de-escalation.
Several limitations of our study should be noted. First, while the NCDB provides data regarding overall survival, cancer-specific outcomes such as local control, metastasis-free survival, and breast cancer-specific survival are unavailable. Second, while we quantitatively examined the effect of invasive tumor size on OS, the NCDB only records DCIS extent as a dichotomized variable (<25% or ≥25%). Thus, the minimum amount of DCIS that is necessary to observe an association with improved OS remains unclear. Third, because central pathologic review is not a requirement for NCDB data inclusion, inconsistencies in pathologic assessment across participating institutions could not be accounted for in this analysis. Fourth, biases inherent to the retrospective nature of our study may have been introduced. For example, selection bias is a frequent limitation in NCDB studies and could effect survival outcomes between study groups. However, it is likely that our study is less subject to selection bias as two groups are compared only based on a pathologic variable (presence or absence of a DCIS component) that should not significantly impact treatment decisions. Finally, the NCDB is not a population-based database30, thus patients presenting to NCDB-participating hospitals may not accurately represent the greater US population.
Conclusion
We find that breast cancer survival is improved when DCIS accompanies IDC, particularly for patients with invasive disease measuring less than 4 cm or node-negative disease. These findings suggest that the presence of DCIS with IDC may be a marker of reduced aggressiveness, and could be incorporated as a prognostic feature in future treatment algorithms.
References
Burstein, H. J., Polyak, K., Wong, J. S., Lester, S. C. & Kaelin, C. M. Ductal carcinoma in situ of the breast. The New England journal of medicine 350, 1430–1441, https://doi.org/10.1056/NEJMra031301 (2004).
Sgroi, D. C. Preinvasive breast cancer. Annu Rev Pathol 5, 193–221, https://doi.org/10.1146/annurev.pathol.4.110807.092306 (2010).
Espina, V. & Liotta, L. A. What is the malignant nature of human ductal carcinoma in situ? Nat Rev Cancer 11, 68–75, https://doi.org/10.1038/nrc2950 (2011).
Gradishar, W. J. et al. Invasive Breast Cancer Version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 14, 324–354 (2016).
Chagpar, A. B., McMasters, K. M., Sahoo, S. & Edwards, M. J. Does ductal carcinoma in situ accompanying invasive carcinoma affect prognosis? Surgery 146, 561–567; discussion 567–568, https://doi.org/10.1016/j.surg.2009.06.039 (2009).
Wong, H., Lau, S., Yau, T., Cheung, P. & Epstein, R. J. Presence of an in situ component is associated with reduced biological aggressiveness of size-matched invasive breast cancer. British journal of cancer 102, 1391–1396, https://doi.org/10.1038/sj.bjc.6605655 (2010).
Wong, H. et al. Coexisting ductal carcinoma in situ independently predicts lower tumor aggressiveness in node-positive luminal breast cancer. Med Oncol 29, 1536–1542, https://doi.org/10.1007/s12032-011-0082-y (2012).
Dieterich, M. et al. Accompanying DCIS in breast cancer patients with invasive ductal carcinoma is predictive of improved local recurrence-free survival. Breast 23, 346–351, https://doi.org/10.1016/j.breast.2014.01.015 (2014).
Carabias-Meseguer, P. et al. Influence of the in situ component in 389 infiltrating ductal breast carcinomas. Breast Cancer 20, 213–217, https://doi.org/10.1007/s12282-011-0330-1 (2013).
Gage, I. et al. Pathologic margin involvement and the risk of recurrence in patients treated with breast-conserving therapy. Cancer 78, 1921–1928 (1996).
Holland, R. et al. The presence of an extensive intraductal component following a limited excision correlates with prominent residual disease in the remainder of the breast. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 8, 113–118, https://doi.org/10.1200/JCO.1990.8.1.113 (1990).
Schnitt, S. J. et al. The relationship between microscopic margins of resection and the risk of local recurrence in patients with breast cancer treated with breast-conserving surgery and radiation therapy. Cancer 74, 1746–1751 (1994).
Moran, M. S. et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 32, 1507–1515, https://doi.org/10.1200/JCO.2013.53.3935 (2014).
Schnitt, S. J., Connolly, J. L., Harris, J. R., Hellman, S. & Cohen, R. B. Pathologic predictors of early local recurrence in Stage I and II breast cancer treated by primary radiation therapy. Cancer 53, 1049–1057 (1984).
Harris, J. R. et al. The use of pathologic features in selecting the extent of surgical resection necessary for breast cancer patients treated by primary radiation therapy. Ann Surg 201, 164–169 (1985).
Osteen, R. T. et al. Identification of patients at high risk for local recurrence after conservative surgery and radiation therapy for stage I or II breast cancer. Arch Surg 122, 1248–1252 (1987).
Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406, 747–752, https://doi.org/10.1038/35021093 (2000).
Cancer Genome Atlas, N. Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70, https://doi.org/10.1038/nature11412 (2012).
Sorlie, T. et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98, 10869–10874, https://doi.org/10.1073/pnas.191367098 (2001).
Carter, S. L., Eklund, A. C., Kohane, I. S., Harris, L. N. & Szallasi, Z. A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat Genet 38, 1043–1048, https://doi.org/10.1038/ng1861 (2006).
Bakhoum, S. F. & Cantley, L. C. The Multifaceted Role of Chromosomal Instability in Cancer and Its Microenvironment. Cell 174, 1347–1360, https://doi.org/10.1016/j.cell.2018.08.027 (2018).
Negrini, S., Gorgoulis, V. G. & Halazonetis, T. D. Genomic instability–an evolving hallmark of cancer. Nat Rev Mol Cell Biol 11, 220–228, https://doi.org/10.1038/nrm2858 (2010).
Maxwell, A. J. et al. Risk factors for the development of invasive cancer in unresected ductal carcinoma in situ. Eur J Surg Oncol 44, 429–435, https://doi.org/10.1016/j.ejso.2017.12.007 (2018).
Ryser, M. D. et al. Cancer Outcomes in DCIS Patients Without Locoregional Treatment. J Natl Cancer Inst, https://doi.org/10.1093/jnci/djy220 (2019).
Visser, L. L. et al. Predictors of an Invasive Breast Cancer Recurrence after DCIS: A Systematic Review and Meta-analyses. Cancer Epidemiol Biomarkers Prev 28, 835–845, https://doi.org/10.1158/1055-9965.EPI-18-0976 (2019).
Hughes, K. S. et al. Lumpectomy plus tamoxifen with or without irradiation in women 70 years of age or older with early breast cancer. The New England journal of medicine 351, 971–977, https://doi.org/10.1056/NEJMoa040587 (2004).
Hughes, K. S. et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 31, 2382–2387, https://doi.org/10.1200/JCO.2012.45.2615 (2013).
Sparano, J. A. et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. The New England journal of medicine 379, 111–121, https://doi.org/10.1056/NEJMoa1804710 (2018).
The IDEA Study (Individualized Decisions for Endocrine Therapy Alone), https://clinicaltrials.gov/ct2/show/NCT02400190.
Palma, D. A. National Cancer Data Base: An Important Research Tool, but Not Population-Based. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, JCO2016692855 (2016).
Acknowledgements
AAP’s research efforts are supported in part by grant R01 CA197486 from the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
A.J.K., H.S.P. and A.A.P. conceptualized the project. J.R.K. obtained the data used for the study. All authors contributed to data analysis and editing of the article.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kole, A.J., Park, H.S., Johnson, S.B. et al. Overall survival is improved when DCIS accompanies invasive breast cancer. Sci Rep 9, 9934 (2019). https://doi.org/10.1038/s41598-019-46309-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-46309-2
This article is cited by
-
Functionalization of curcumin nanomedicines: a recent promising adaptation to maximize pharmacokinetic profile, specific cell internalization and anticancer efficacy against breast cancer
Journal of Nanobiotechnology (2023)
-
Spatial biology of cancer evolution
Nature Reviews Genetics (2023)
-
Pathologic complete response of ductal carcinoma in situ to neoadjuvant systemic therapy in HER2-positive invasive breast cancer patients: a nationwide analysis
Breast Cancer Research and Treatment (2023)
-
Clinicopathological characteristics and prognosis of triple-negative breast cancer invasive ductal carcinoma with ductal carcinoma in situ
Journal of Cancer Research and Clinical Oncology (2023)
-
Spatial genomics maps the structure, nature and evolution of cancer clones
Nature (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.