Abstract
HIV-1 is characterized by high genetic variability, with implications for spread, and immune-escape selection. Here, the genetic modification of HIV-1 B subtype over time was evaluated on 3,328 pol and 1,152 V3 sequences belonging to B subtype and collected from individuals diagnosed in Italy between 2003 and 2016. Sequences were analyzed for genetic-distance from consensus-B (Tajima-Nei), non-synonymous and synonymous rates (dN and dS), CTL escapes, and intra-host evolution over four time-spans (2003–2006, 2007–2009, 2010–2012, 2013–2016). Genetic-distance increased over time for both pol and V3 sequences (P < 0.0001 and 0.0003). Similar results were obtained for dN and dS. Entropy-value significantly increased at 16 pol and two V3 amino acid positions. Seven of them were CTL escape positions (protease: 71; reverse-transcriptase: 35, 162, 177, 202, 207, 211). Sequences with ≥3 CTL escapes increased from 36.1% in 2003–2006 to 54.0% in 2013–2016 (P < 0.0001), and showed better intra-host adaptation than those containing ≤2 CTL escapes (intra-host evolution: 3.0 × 10−3 [2.9 × 10−3–3.1 × 10−3] vs. 4.3 × 10−3 [4.0 × 10−3–5.0 × 10−3], P[LRT] < 0.0001[21.09]). These data provide evidence of still ongoing modifications, involving CTL escape mutations, in circulating HIV-1 B subtype in Italy. These modifications might affect the process of HIV-1 adaptation to the host, as suggested by the slow intra-host evolution characterizing viruses with a high number of CTL escapes.
Similar content being viewed by others
Introduction
Human immunodeficiency virus type 1 (HIV-1) is characterized by a high genetic variability, mainly due to high rate of replication, mutation, and recombination1,2,3. Amino acid mutations that arise by chance can be thereafter selected by the pressure of the human immune system4,5 or combined antiretroviral therapy (cART)6,7. New selected amino acids may establish strong interactions among themselves, further modulating viral fitness, and development of drug resistance, but also immune escape process, thus enhancing pathogenic potential of the virus8,9.
Moreover, due to the continuum intent of HIV to find the best host adaptation, a constant selection of new viral species can occur at the intra-host level10. If these viral variants enhance viral competitive ability, they will rapidly spread at the epidemiological level becoming dominant variants characterized by selective advantage11,12.
To date, literature on HIV-1 evolutionary dynamics focused attention on the spread of drug resistance and on the potential that drug resistant mutations, together with compensatory mutations, had on increased fitness and virulence in patients never exposed to or starting cART13,14,15. Much has also been done in the field of CD8+ cytotoxic T-lymphocyte (CTL) related regions, their intra-host evolution and their relationship to clinical outcome16,17,18.
On the other hand, little is known regarding the extent of HIV-1 genetic modification over time, and regarding the role that CTL-mediated selection pressure has in inter-host HIV-1 evolution, even if some evidence has recently emerged19,20. Moreover, if and how fixation of CTL escapes may influence viral load and immunological parameters in the first phases of infection is still largely unknown.
Thus, in the present study, we investigated the extent of genetic divergence, CTL escape prevalence and intra-host evolution of the most prevalent HIV-1 subtype, the B form, in a cohort of HIV-1 infected patients diagnosed in Italy between 2003 and 2016.
Results
Study population
A total of 3,328 HIV-1 B subtype infected individuals with at least one polymerase (pol) sequence at HIV-1 diagnosis (range of weeks between HIV-1 diagnosis and pol sequencing: 0.8–5.0) were retrieved for this study. V3 sequences collected at the same time point of pol were also available for a subgroup of patients (N = 1,152).
By dividing the population in accordance with year of HIV-1 diagnosis, 554 individuals belonged to the time frame 2003–2006, 826 to 2007–2009, 1,003 to 2010–2012, and 945 to 2013–2016 (Table 1).
Looking at the overall population, the majority of individuals were male (2,814, 84.6%), and Italian (2,603, 78.2%) with a median (Interquartile-range, IQR) age of 38 (31–46) years. Among the risk factors, homosexual and heterosexual contacts were the most prevalent infection routes (1,654 [49.8%] and 940 [28.2%], respectively). Median (IQR) plasma viral load (copies/mL) was 76,619 (21,216–258,222), median (IQR) CD4+T and CD8+T cell counts were 333 (130–521) and 725 (460–1,085) (cell/mm3), respectively (Table 1). Recent infections accounted for 21.1% (N = 210) of the individuals for whom information regarding the chronic or recent phase of infection was available. The majority of these individuals with recent infection were male (180, 85.7%) and Italian (178, 84.8%) with a median (Interquartile-range, IQR) age of 36 (30–43) years. Homosexual and heterosexual contacts were the most prevalent infection routes (144 [68.6%] and 45 [21.4%], respectively). Median (IQR) plasma viral load (copies/mL) was 54,288 (13,077–189,192), median (IQR) CD4+T and CD8+T cell counts were 535 (405–721) and 780 (582–1,237) (cell/mm3), respectively.
By looking at the four time spans, no statistically significant differences were observed with respect to demographic characteristics, with the exception of a slight increase in males, occurring in 2007–2009, and a slight decrease in Italians, in 2013–2016, and in heterosexuals, since 2010–2012 (Table 1). CD8+T cell count significantly decreased in 2010–2012 and remained stable in 2013–2016 (Table 1).
Genetic distance evaluation over time
In the overall population, the mean value of genetic distance (mean ± standard error, SE) compared with consensus B was 0.043 ± 0.012 for pol and 0.100 ± 0.001 for V3. A progressive and significant increase in genetic divergence from consensus B was observed over time for both pol and V3 sequences (pol: from 0.037 ± 0.008 in 2003–2006 to 0.048 ± 0.010 in 2013–2016, P < 0.0001; V3: from 0.090 ± 0.005 in 2007–2009 to 0.111 ± 0.003 in 2013–2016, P < 0.0001) (Figs 1A and 2A). Comparable results were obtained considering only the recent infections with available 210 pol and 66 V3 sequences, even if the statistical significance was obtained only for pol (pol: from 0.039 ± 0.008 in 2003–2006 to 0.049 ± 0.010 in 2013–2016, P = 0.0003; V3: from 0.070 ± 0.010 in 2007–2009 to 0.090 ± 0.024 in 2013–2016, P = 0.315) (Figs 1B and 2B).
Genetic distance of 3,328 (A) and 210 (B) HIV-1 B subtype pol sequences, belonging to newly diagnosed and recently infected patients, respectively, divided into four time frames in accordance with year of diagnosis. aGenetic distance was calculated by comparing sequences with HIV-1 consensus B using Tajima Nei model, MEGA 6. bBy Kruskal-Wallis test, corrected for Benjamini-Hochberg method. SE: standard error.
Genetic distance of 1,152 (A) and 66 (B) HIV-1 B subtype V3 sequences, belonging to newly diagnosed and recently infected patients, respectively, divided into three time frames. aGenetic distance was calculated by comparing HIV-1 sequences with HIV-1 consensus B using Tajima Nei model, MEGA 6. bBy Kruskal-Wallis test, corrected for Benjamini-Hochberg method. SE: standard error.
Similar results were also obtained for dN and dS values (overall dN and dS, mean ± SE for pol: 0.019 ± 0.006 and 0.130 ± 0.043; overall dN and dS, mean ± SE for V3: 0.078 ± 0.001 and 0.129 ± 0.003). In particular, both dN and dS progressively increased over time in both pol and V3 sequences (pol: from 0.017 ± 0.005 and 0.109 ± 0.029 in 2003–2006 to 0.021 ± 0.006 and 0.146 ± 0.037 in 2013–2016, P = 0.023 and 0.0001; V3: from 0.070 ± 0.004 and 0.117 ± 0.008 in 2007–2009 to 0.086 ± 0.002 and 0.139 ± 0.005 in 2013–2016, P = 0.0006 and 0.056) (Table 2 and Supplementary Material 1). Comparable results were again obtained considering only the recent infections (Table 2 and Supplementary Material 1).
Trend of amino acid variability over time
In order to measure the variation in pol and V3 amino acids over time, the first 369 amino acids of pol (99 PR amino acids and 270 reverse transcriptase [RT] amino acids) and the 35 amino acids defining the V3 were analysed for the entropy value. In particular, pol amino acid sequences obtained in the period 2003–2006 were compared with those obtained in the period 2013–2016. The same analysis was performed for V3 amino acid sequences obtained in the period 2007–2009 and in the period 2013–2016.
Significant increases in entropy values were found at 18 positions (16 in pol and two in V3).
In particular, by comparing pol amino acid sequences, entropy increased at five amino acid positions in protease (PR: 19, 33, 71, 72, 79), and at 11 positions in RT (35, 162, 173, 174, 177, 196, 200, 202, 207, 211, 214) (Fig. 3). Interestingly, CTL escape variants occur at seven of these positions, such as the PR position 71 (escape variant: A71V), and the RT positions 35 (escape variant: V35I), 162 (escape variant: S162ACQR), 177 (escape variant: D177E), 202 (escape variant: I202V), 207 (escape variant: Q207GE) and 211 (escape variant: R211K). By comparing V3 amino acid sequences, entropy increased at positions 2 and 19 (Fig. 3).
Amino acid positions characterized by an increased entropy value in the last time frame. Pol sequences obtained in the period 2003–2006 and those obtained in the period 2013–2016 were submitted for entropy analysis at HIV Los Alamos National Laboratory Entropy-Two tool (https://www.hiv.lanl.gov/content/sequence/ENTROPY/entropy.html) in order to obtain delta entropy values. The same analysis was performed by comparing V3 sequences obtained in the period 2007–2009 and in the period 2013–2016. Only delta values ≤0.10 and >0.10 followed by a P ≤ 0.05 after Benjamini-Hockberg correction were considered statistically significant.
Entropy significantly decreased only at RT amino acid position 11 (delta entropy value: −0.122, P = 0.0001).
Trend of CTL escapes over time
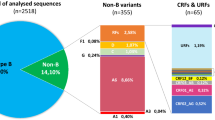
By analysing the prevalence of CTL escape mutations in pol, we found that 8.7% of sequences (N = 288) did not contain escape mutations, 19.0% (N = 632) contained one escape, 26.2% (N = 872) contained two escapes, 23.0% (N = 767) contained three escapes, 13.9% (N = 462) contained four escapes, and 9.2% (N = 307) contained ≥5 escapes. Among recent infections, 8.6% of sequences (N = 18) did not contain escape mutations, 21.4% (N = 45) contained one escape, 30.0% (N = 63) contained two escapes, and 40.0% (N = 84) contained ≥3 escapes. Looking at the CTL escape prevalence over time, pol sequences with ≥3 CTL escapes rose from 36.1% in 2003–2006 to 54.0% in 2013–2016 (P < 0.0001). In particular, pol sequences with 3, 4 and ≥5 CTL escapes increased from 18.9%, 11.4%, and 5.8% in 2003–2006 to 25.3%, 16.5% and 12.2% in 2013–2016, P = 0.008, 0.004, and <0.0001, respectively (Table 3). This increase was mainly due to PR escape mutation A71V, and RT escape mutations S162ACQR, D177E, I202V, and R211K (Supplementary Material 2). Limiting the analysis to recent infections, pol sequences with ≥3 CTL escapes were more frequently found in 2013–2016 compared with 2003–2006 (56.2% vs. 31.4%), even if this increase did not reach statistical significance (P = 0.139) (Table 4).
By analysing significant patterns of pairwise correlations among pol CTL escape mutations, a positive significant correlation was found between the CTL escapes at position 162 (S162ACQR) and the escape at position 177 (D177E) (number of sequences showing the correlated pair = 169; covariation frequency: 35.1%; phi = 0.11, P < 0.0001).
By analysing V3 loop, only 8 sequences in 1,152 (0.7%) contained CTL escapes. All these sequences belonged to the time frames 2010–2012 and 2013–2016 (2 [0.3%] and 6 [1.7%], respectively).
Role of epidemiological confounders in influencing HIV-1 B subtype variability and CTL escapes
We next sought to investigate whether changes in risk factors, in patients’ origin, and in sequences involved in transmission clusters (TCs) across time might interfere with HIV-1 B subtype increased variability.
Firstly, we investigated whether TCs frequency correlates with HIV-1 increased variability by comparing the subgroup of 1,119 pol sequences involved in TCs with the subgroup of 2,209 pol sequences out of TCs. The progressive and significant increase in genetic divergence from consensus B over time was confirmed both for sequences in TCs and for sequences out of TCs (TCs: from 0.038 ± 0.001 in 2003–2006 to 0.047 ± 0.00001 in 2013–2016, P < 0.0001; out of TCs: from 0.037 ± 0.00001 in 2003–2006 to 0.048 ± 0.00001 in 2013–2016, P < 0.0001). Similar results were also obtained for dN and dS values (TCs: from 0.016 ± 0.0004 and 0.113 ± 0.003 in 2003–2006 to 0.020 ± 0.0003 and 0.143 ± 0.002 in 2013–2016, P < 0.0001 and <0.0001; out of TCs: from 0.017 ± 0.0003 and 0.107 ± 0.001 in 2003–2006 to 0.021 ± 0.0002 and 0.147 ± 0.002 in 2013–2016, P < 0.0001 and <0.0001).
Looking at the CTL escape prevalence over time, pol sequences with 3, 4 and ≥5 CTL escapes increased both in TCs and out of TCs, although not always significantly (in TCs: from 24.0%, 8.3%, and 5.5% in 2003–2006 to 28.1%, 14.7% and 14.4% in 2013–2016, P = 0.209; P = 0.060; P = 0.012; out TCs: from 17.5%, 12.1%, and 5.8% in 2003–2006 to 23.7%, 17.5% and 11.0% in 2013–2016, P = 0.075; P = 0.020; P = 0.030).
In line with these results, the presence of TCs did not significantly affect either the number of circulating CTL escapes (Pearson’s phi = 0.015; P = 0.118) or the spread of single CTL escape (RT S162ACQR: phi = −0.25; P = 0.152; RT D177E: phi = 0.008; P = 0.641; RT I202V: phi = −0.051; P = 0.184; RT R211K; phi = −0.21; P = 0.221), with the exception of PR A71V (phi = 0.105; P < 0.0001).
Overall results suggest that the HIV-1 B subtype increased variability and the spread of CTL escapes are not predominantly correlated with expanding clades over time.
We next investigated whether variation in the proportion of risk factors, and patients’ origin across time might influence the HIV-1 B subtype increased variability. To do so, we restricted the analysis to a more homogenous population, composed of pol (N = 1,308) and V3 (N = 449) sequences belonging to MSM of Italian origin. The results confirmed the progressive and significant increase in genetic divergence from consensus B over time for pol, and like a trend for V3 (pol: from 0.038 ± 0.001 in 2003–2006 to 0.047 ± 0.001 in 2013–2016, P < 0.0001; V3: from 0.085 ± 0.007 in 2007–2009 to 0.098 ± 0.005 in 2013–2016, P = 0.348). Similar results were also obtained for dN and dS values (pol: from 0.017 ± 0.0004 and 0.110 ± 0.002 in 2003–2006 to 0.020 ± 0.0003 and 0.143 ± 0.002 in 2013–2016, P < 0.0001 and <0.0001; V3: from 0.072 ± 0.007 and 0.093 ± 0.012 in 2007–2009 to 0.077 ± 0.004 and 0.126 ± 0.010 in 2013–2016, P = 0.635 and 0.072). Looking at the CTL escape prevalence, pol sequences with 3, 4 and ≥5 CTL escapes were more frequently found in 2013–2016 compared with 2003–2006, even if this increase was not always significant (3 CTL escapes: from 20.8% in 2003–2006 to 26.6% in 2013–2016, P = 0.394; 4 CTL escapes: from 11.6% to 14.6%, P = 0.224; ≥5 CTL escapes: from 5.8% to 14%, P = 0.018). Again, these results suggest that changes in risk factors and patients’ origin are not predominantly responsible for HIV-1 B subtype variability.
Impact of CTL escapes and year of diagnosis on HIV-1 pol evolution
A subgroup of 153 individuals with two pol sequences available before therapy start (time-window between sequences within 70 weeks) was analysed to define if the evolutionary rate of HIV-1 per site per year may be affected by the time of diagnosis and number of CTL escapes. The evolutionary rate of HIV-1 per site per year in the 153 pairs of sequences was 3.9 × 10−3 (3.3 × 10−3–4.5 × 10−3).
Among these pairs, 73 carried ≥3 CTL escapes (time-window between sequences, median weeks [IQR] 59 [44–83]), while 80 carried ≤2 CTL escapes (time-window between sequences, median weeks [IQR] 62 [41–77]). Stratifying the pairs based on year of diagnosis, 28 pairs carrying ≥3 CTL escapes belonged to patients diagnosed after 2009 (time-window between sequences, median weeks [IQR] 58 [45–90]), while 57 carrying ≤2 CTL escapes belonged to patients diagnosed before 2009 (time-window between sequences, median weeks [IQR] 66 [51–78]).
Rates of HIV-1 intra-host evolution (95% confidence interval, CI) were consistently lower in pairs containing ≥3 CTL escapes than in those containing ≤2 CTL escapes (3.0 × 10−3 [2.9 × 10−3−3.1 × 10−3] vs. 4.3 × 10−3 [4.0 × 10−3–5.0 × 10−3], P [likelihood-ratio test, LRT] < 0.0001[21.09]). Consistent with these data, the selective pressure was lower in pol containing ≥3 CTL escapes than in pol containing ≤2 CTL escapes (dN/dS, 95% CI: 0.28 [0.24–0.34] vs. 0.25 [0.22–0.29]).
Stratifying the pairs based on year of diagnosis, the rates of HIV-1 intra-host evolution (95% CI) were significantly lower in pairs containing ≥3 CTL escapes and belonging to patients diagnosed after 2009 than in those with ≤2 CTL escapes and belonging to patients diagnosed before 2009 (3.2 × 10−3 [3.0 × 10−3–4.0 × 10−3] vs. 4.5 × 10−3 [4.0 × 10−3–5.0 × 10−3], P [LRT] < 0.001[12.76]). Again the selective pressure was confirmed to be lower in sequences circulating after 2009 and with ≥3 CTL escapes than in those circulating before 2009 and with ≤2 CTL escapes (dN/dS, 95% CI: 0.21 [0.15–0.27] vs. 0.27 [0.23–0.32]).
These findings might suggest a better HIV-1 intra-host adaptation for most recent viruses driving a higher number of CTL escapes.
Correlation between pol CTL escape mutants and viro-immunological parameters
By analysing a subgroup of 781 individuals characterized by recent infection or plasma viral load >10,000 copies/ml and CD4+T cells >500 cells/mm3, no significant correlations were found between CTL escapes and plasma viral load or CD4+T cell counts.
On the other hand, CD4/CD8 ratio significantly decreased in relation to the increased number of CTL escapes (from 1.64 ± 0.68 in patients infected by a virus with 0 CTL escapes to 0.69 ± 0.05 in patients infected by a virus with ≥5 CTL escapes, ρ = −0.100, P = 0.027) (Table 5). The negative correlations between the number of CTL escapes in pol and lower CD4/CD8 ratio were confirmed also when only the recent infections were analysed (1.02 ± 0.18 for 0 CTL escapes vs. 0.74 ± 0.06 for ≥3 CTL escapes, ρ = −0.15, P = 0.067) (Table 6).
Discussion
Our analysis based on HIV-1 B subtype pol (N = 3,328) and V3 (N = 1,152) sequences collected from a large number of HIV-1 newly diagnosed individuals in Italy in the time frame 2003–2016 indicates a progressive and significant increase in genetic and amino acid distance over time (with 18 amino acid positions characterized by entropy increase) for the most disseminated HIV-1 subtype in the world. This finding is also confirmed when only the subgroup of recently infected individuals is taken into account, confirming the higher variability of the new circulating viral strains belonging to HIV-1 B subtype compared with the older.
Despite the short time since its emergence (dated in 1944), HIV-1 B has generated successful epidemics in many countries in five continents, and the spread continues21. Due to the global extension of the HIV-1 B epidemic22,23,24, and the high evolutionary rates characterizing HIV25, a progressive diversity over time for this subtype has been reported both in North America20 and, even if limited to protease and integrase, in Europe26,27. A recent paper comparing the historic (1979–1989) versus modern (post-2000) HIV-1 subtype B cohorts in North America showed that in the past 30 years HIV-1 diversity increased approximately twofold, and the average background frequencies of CTL escape mutations also doubled20.
In our dataset, seven out of the 18 positions characterized by entropy increase take part in CTL escape variants (PR 71; RT 35, 162, 177, 202, 207, 211).
Of note, prevalence of CTL escapes significantly increased in the last time frame at five of these seven positions (PR: A71V; RT: S162ACQR, D177E, I202V, and R211K). Whereas entropy at positions 35 and 207 increased, V35I and Q207GE escapes did not change their prevalence concomitantly (V35I and Q207G/E prevalence: 18.8% and 19.1% in 2003–2006 vs. 16.8% and 19.4% in 2013–2016, P = 0.672 and P = 0.119, respectively). The reason for the entropy increase at these 2 positions may thus reside in other amino acid mutations not involved in CTL escapes, such as V35LTM and Q207HNADRK, whose prevalence increased from 7.9% and 8.1% in 2003–2006 to 13.4% and 10.7% in 2013–2016, respectively (P = 0.034 and P = 0.048). The role of these amino acid mutations is not clearly demonstrated, and thus further studies might be necessary to define their impact on HIV-1 B evolution and pathogenesis.
Notwithstanding the increase in sequence diversity observed over time in our dataset, we have to consider that HIV variation and immune escape process are also limited by structural and functional constraints28,29. In particular, the virus would have fewer viable options to generate escape variants in conserved protein regions because of the fitness cost required30. However, HIV overcomes this problem thanks to specific mechanisms that compensate for the fitness costs. For example, studies on gag polyprotein demonstrated the selection of compensatory mutations, which can restore the viral fitness. These mutations can occur both within31 and outside the epitope, but nearby in the three-dimensional protein structure32,33.
In this respect, the increased prevalence of some amino acid variants in pol and their correlation in mutational pathways (such as for S162ACQR and D177E) may suggest a compensatory role played by these mutations, which can therefore explain their frequent occurrence, rather than by chance in the circulating viral population. Its effect may positively influence the fixation of a specific CTL escape at population level34. In line with this, the prevalence of sequences with ≥3CTL escapes progressively increased in both overall population and recent infections, reaching 54.0% and 56.2% in 2013–2016, respectively. This may represent an evolutionary advantage with consequences for disease progression, infectivity, transmissibility, and response to antiviral treatments35.
Moreover, the ability of HIV-1 immune escape mutations to accumulate rapidly could undermine host antiviral immunity36,37,38, and thus in turn have immunological consequences at population level. In this respect, our study found that the higher number of CTL escapes in pol frequently correlated with lower CD4/CD8 ratio (delta CD4/CD8 ratio = −0.95) at HIV-1 diagnosis, suggesting an increased pathogenic potential of these viral strains. However, these data need to be interpreted with caution, especially because of the lack of HLA information.
The impossibility to match CTL escape variants with HLA types of the host also represents a limitation for the estimation of the CTL escape prevalence. It is known that CTL escape prevalence may differ between HLA mismatched and HLA matched people39,40, and that the fixation of some HIV-1 polymorphisms at population level strongly depends on population characteristics41. To partially overcome the lack of HLA information, we have focused attention on those CTL escapes that significantly increased over time, such as the PR A71V and the RT D177E (related to HLA-B*1503), the RT S162ACQR (related to HLA-A*1101 –A*8601, -A*0301, -B*38 and B*0702), I202V (related to HLA-B4001), and R211K (related to HLA-A*2501). By matching these data with the prevalence of HLA in Italian population, we found that all the mentioned HLA are well represented in Italy. In particular, the HLA-A*1101, -A*2501 and -A*0301 represent 16% of the overall HLA-A locus, while the HLA- B*5101, -B*0702, -B*4001, and -B*03 16% of the overall HLA-B locus42. Thus, the spread of the previously mentioned CTL escape polymorphisms at the population level in Italy may be explained by the relative diffusion of matched HLA in the general Italian population.
However, the persistence of CTL escapes is not always dependent on matched HLA. Specific escape mutations persist upon transmission to HLA unmatched hosts, perhaps owing to a lack of fitness costs43,44. A recent mathematical model shows that the median time to escape in HLA matched individuals across the 26 epitopes considered is 8 years, and the reversion rates is a little slower (median time to reversion: 6.5 years) with no evidence of reversion in 56% of CTL epitopes, suggesting that CTL escapes are able to spread rapidly at population level independently of HLA45.
The role of CTL escapes in the process of HIV adaptation to the host was also confirmed by the estimation of the intra-host evolution. In particular, by analysing a subgroup of individuals with two pol sequences available, we found that the rate of intra-host evolution and the consequent selective pressure were significantly lower for most recent HIV-1 diagnoses carrying ≥3 CTL escapes than older diagnoses carrying fewer CTL escapes (3.2 × 10−3 vs. 4.5 × 10−3). In the context of the already known slow HIV-1 pol evolution46, the slower intra-host evolution found for most recent circulating viruses driving a higher number of CTL escapes may suggest that HIV-1 had improved its adaptation to the host in recent years compared with the past, even if the adaptation process is still occurring.
Besides CTL escapes, further attention should be given to neutralizing epitope escapes, of which the V3 loop is rich. In our study, we found that while in pol entropy values increased also within CTL epitopes (such as PR position 71 and the RT positions 35, 162, 177, 202, 207 and 211), in V3 higher mutation rates occurred almost exclusively within previously described neutralizing epitopes47, and at residue 19 already associated with R5 tropism48. We are conscious that our analysis is limited to a very short region of env, and that further studies taking into account a longer env fragment encompassing at least all the variable loops and conserved regions of gp120 may be necessary. Similar studies will be of extreme interest in defining the tracing of amino acid modifications in HIV-1 domains involved in vaccine strategies and co-receptor affinity.
Looking at potential epidemiological confounders able to influence HIV-1 B subtype variability and CTL escapes over time, we found that neither risk factor nor patients’ origin, nor TCs strictly (and exclusively) impact HIV-1 B subtype variability over time. Doing these sub-studies yielded results mainly consistent with the overall analysis, suggesting that HIV-1 B subtype varied over time, regardless of these confounders.
Nevertheless, we cannot definitely exclude that the relevant epidemiological changes occurring in Italy in recent years, such as the migratory waves from low-middle income areas49, or the time-dependent influx of sequences from different risk groups might contribute (even if not predominantly) to HIV-1 B subtype variation in this country. For example, in our dataset individuals of “unknown” origin and “other or unknown” risk factors increased from 1.8% and 4.0% in 2003–2006 to 13.1% and 17.7% in 2013–2016, while Italians and heterosexuals decreased from 80.5% and 33.2% in 2003–2006 to 72.6% and 23.3% in 2013–2016. This geographic and epidemiological admixture combined with the documented high rate of post-immigration HIV-1 acquisition50 might also favour the diffusion of new HLAs at population level and the selection of new CTL escape mutations.
Finally, as the article is mainly focused on pol, the introduction of antiretroviral therapies merits attention (RT inhibitors were introduced in the late 1980s and PR inhibitors in the mid 1990s). Indeed, two out of the 18 positions characterized by entropy increase, the PR 33 and 71, are involved in drug resistance. The observed entropy increase was mainly due to the mutations L33F/I and A71VTIL, whose prevalence increased in the last two time frames (L33FI: 0.4% in 2003–2006 vs.1.2% in 2007–2009 vs. 3.9% in 2010–2012 vs. 3.0% in 2013–2016, P < 0.0001; A71VTIL: 15.0% in 2003–2006 vs. 13.7% in 2007–2009 vs. 18.5% in 2010–2012 vs. 21.2% in 2013–2016, P < 0.0001). Both L33F and A71VTIL are PI-selected accessory mutations, associated with a minimal or null reduced susceptibility to PIs51,52. Even if some of these mutations such as L33I and A71VT may also appear as natural polymorphisms or CTL escapes (such as A71V), we cannot exclude that their increased prevalence in the last two time frames may be an indicator of viral adaptation to PI drug exposure.
In conclusion, this study, based on HIV-1 B subtype sequences diagnosed in Italy, provides additional evidence that HIV-1 is still adapting to host, and that this adaptation may include CTL escape mutations. These findings can help in making accurate maps of escape pathways and in defining optimal induction CTLs strategies that may be effective in controlling HIV-1 replication, which may have implications for immunotherapeutic interventions. Moreover, this paper poses the bases for further studies involving viral evolution and viral adaptation focused on rapidly expanding epidemics such as those currently occurring in Africa and Asia, mainly driven by recombinant forms and non-B pure forms.
Materials and Methods
Study population
This study was conducted on 3,328 pol sequences (containing the full-length PR and the first 270 RT codons; nucleotides length: 1,107) and 1,152 V3 sequences (nucleotides length: 105; amino acid length: 35) obtained from HIV-1 B subtype newly diagnosed infected individuals (one sequence per patient) in Italy. All patients were naïve to cART and 210 of them were HIV-1 recently infected. Pol and V3 sequences were performed from plasma samples for routine clinical purposes from 2003 to 2016 and from 2007 to 2016, respectively, immediately after the diagnosis, and then collected in an anonymous database53,54. HIV-1 B subtype for pol and V3 sequences was firstly determined by Stanford DB (https://hivdb.stanford.edu/) and geno2pheno algorithm (https://coreceptor.geno2pheno.org/), respectively, and further confirmed by phylogenetic analysis based on pol, as described previously55.
Recent infections were determined by: (i) clinical/laboratory signs of primary HIV infection (HIV-1 plasma viral load levels >10,000 copies/mL and negative or indeterminate HIV-1 antibody test); (ii) a documented negative HIV-1 test performed within the 6 months prior to the HIV-1 diagnosis; and (iii) an antibody avidity index ≤0.80 (test performed only in clinically AIDS free individuals)56,57.
Ethic statement
This study was conducted on data collected for clinical purposes. All data used in the study were previously anonymized, according to the requirements set by Italian Data Protection Code (leg. decree 196/2003) and by the General authorizations issued by the Data Protection Authority. This study was approved by the ethics committee of Tor Vergata Hospital (Ethics Approval No. 238/16, 14 December 2016) and L. Spallanzani National Institute for Infectious Diseases, IRCCS (Ethics Approval No. 51, 18 December 2003).
Genetic distance and non-synonymous and synonymous substitution rate estimation
Genetic distance between each pol and V3 sequence and the HIV-1 subtype B consensus sequence was evaluated using MEGA 6 program based on the Tajima Nei model46,58.
The HIV-1 subtype B consensus sequence used for this analysis was published in 2002 by Los Alamos HIV Database. This consensus can be retrieved at https://www.hiv.lanl.gov/content/sequence/NEWALIGN/align.html site. The consensus sequence was calculated according to the default values on the Consensus Maker tools. Details can be retrieved at https://www.hiv.lanl.gov/content/sequence/NEWALIGN/align.html#consensus.
Mean number of synonymous (dS) and nonsynonymous (dN) substitutions per site were calculated by the method of Nei and Gojobori59, through the automatic tool SNAP (https://www.hiv.lanl.gov/content/sequence/SNAP/SNAP.html).
CD8+ cytotoxic T-lymphocyte (CTL) escape mutations
Prevalence of CTL escape mutations in each pol and V3 sequence was evaluated considering all variants in the Los Alamos Immunology Database list defined as: documented escape, or non-susceptible form, or calculated escape, or inferred escape, or diminished response escape (https://www.hiv.lanl.gov/content/immunology/variants/ctl_variant.html, Data last updated at 2017-03-09, Supplementary Material 3).
To identify potential patterns of pairwise correlations between specific CTL escape mutations, a binomial correlation coefficient (phi) and its statistical significance for each pair of mutations were calculated. Average linkage hierarchical agglomerative cluster analysis was performed to investigate potential evolutionary pathways among CTL escape mutations60.
Shannon Entropy calculation
In order to evaluate the variability of each amino acid site in pol over time, the first 369 amino acids of pol (99 PR amino acids and 270 RT amino acids) were analysed for the entropy value. In particular, amino acid sequences obtained in the period 2003–2006 and those obtained in the period 2013–2016 were submitted to HIV Los Alamos National Laboratory (LANL) Entropy-Two tool (https://www.hiv.lanl.gov/content/sequence/ENTROPY/entropy.html)61. The same analysis was performed by comparing entropy values at the 35 amino acid positions of V3 sequences obtained in the period 2007–2009 and in the period 2013–2016. Only delta values ≤0.10 and >0.10 followed by a P ≤ 0.05 after Benjamini-Hochberg correction62 were considered statistically significant.
Statistical analysis
In order to estimate differences in demographic, virological and immunological parameters, genetic distance and CTL escape prevalence over time, pol sequences were divided into four time spans in accordance with the year of diagnosis (time spans: 2003–2006, 2007–2009, 2010–2012, 2013–2016). For the same purposes, V3 sequences, available from 2007, were divided into three time spans (time spans: 2007–2009, 2010–2012, 2013–2016).
CTL escapes were divided into 6 pre-defined categories (0, 1, 2, 3, 4, and ≥5 CTL escapes) for the overall population and into 4 pre-defined categories (0, 1, 2, and ≥3 CTL escapes) for recently infected individuals.
Genetic-distance, dN and dS values, and number of CTL escapes were also evaluated in 1) the subgroup of 1,308 pol and 449 V3 sequences belonging to MSM of Italian origin, 2) the subgroup of 1,119 pol sequences involved in TCs compared with the subgroup of 2,209 pol sequences out of TCs for the purpose of investigating whether risk factors, patients’ origin, and sequences in TCs across time might interfere with obtained results. Potential TCs (defined as clusters of ≥3 pol sequences) were identified by HIV-TRACE using a Tamura-Nei model, and a genetic distance cut-off ≤0.01563.
Kruskal-Wallis and Chi-squared test for trend were used to estimate significant changes over time periods, while Pearson’s Chi-squared test and Mann Whitney test were used to estimate significant changes between two different time periods.
Spearman correlation and Kruskal-Wallis test were also used to estimate significant correlations between viro-immunological parameters and number of CTL escapes. In order to ensure, wherever possible, exclusion of individuals with a late diagnosed chronic infection, these analyses were restricted to a subgroup of 781 individuals including the documented recent infections (N = 210) and individuals characterized by plasma viral load >10,000 copies/ml and CD4+T cells >500 cells/mm3 (N = 571). Viral load and CD4+T cells cut-offs were chosen in accordance with Pantazis N. et al. Lancet HIV 201464.
Again, only P ≤ 0.05 after Benjamini-Hochberg correction62 were considered statistically significant.
All the analyses were performed using the R open source statistical environment (version 3.3.1) and SPSS (version 23) for Windows (SPSS Inc., Chicago, Illinois).
Evolutionary rate estimation
To determine if year of diagnosis and number of CTL escapes may affect the intra-patient evolutionary rate of HIV-1, a subgroup of 153 patients with two pol sequences available before therapy initiation (time-window between sequences within 70 weeks) were analyzed by using HyPhy pol evolution package65. All sequences from each patient were arranged chronologically and the probability of evolving from the oldest to the newest sequence was estimated using maximum likelihood method. In particular, the pol sequences of individuals diagnosed after 2009 and with ≥3 CTL escapes were compared with pol sequences of individuals diagnosed before 2009 and with ≤2 CTL escapes. Branch lengths between the two sequences were assigned based on the difference between sampling dates. For each individual, we determined the nucleotide substitution rate by using a General Time Reversible (6 substitution rates, empirical frequencies) model, assuming strict molecular clock. Significance was assessed using the likelihood ratio test (LRT) with N-2 degrees of freedom. The evolutionary rate per site per year within host were tested for equality using the likelihood-ratio test (LRT)66. Sequence data are available in the Supplementary Dataset 1.
References
Mansky, L. M. & Temin, H. M. Lower in vivo mutation rate of human immunodeficiency virus type 1 than that predicted from the fidelity of purified reverse transcriptase. J. Virol. 69, 5087–5094 (1995).
Frost, S. D. et al. Neutralizing antibody responses drive the evolution of human immunodeficiency virus type 1 envelope during recent HIV infection. Proc. Natl. Acad. Sci. USA 102, 18514–18509 (2005).
Sanjuán, R. & Domingo-Calap, P. Mechanisms of viral mutation. Cell Mol. Life Sci. 73, 4433–4448 (2016).
Leslie, A. et al. Transmission and accumulation of CTL escape variants drive negative associations between HIV polymorphisms and HLA. J. Exp. Med. 201, 891–902 (2005).
Allen, T. M. et al. Selective escape from CD8+T-cell responses represents a major driving force of human immunodeficiency virus type 1 (HIV-1) sequence diversity and reveals constraints on HIV-1 evolution. J. Virol. 79, 13239–13249 (2005).
Nijhuis, M., van Maarseveen, N. M. & Boucher, C. A. HIV protease resistance and viral fitness. Curr. Opin. HIV AIDS 2, 108–115 (2008).
Chen, L., Perlina, A. & Lee, C. J. Positive selection detection in 40,000 human immunodeficiency virus (HIV) type 1 sequences automatically identifies drug resistance and positive fitness mutations in HIV protease and reverse transcriptase. J. Virol. 78, 3722–3732 (2004).
Martinez, J. P. et al. Fitness ranking of individual mutants drives patterns of epistatic interactions in HIV-1. PLoS One 6, e18375 (2011).
Hinkley, T. et al. A systems analysis of mutational effects in HIV-1 protease and reverse transcriptase. Nat. Genet. 43, 487–489 (2011).
Maldarelli, F. et al. HIV populations are large and accumulate high genetic diversity in a nonlinear fashion. J. Virol. 87, 10313–10323 (2013).
Joseph, S. B., Swanstrom, R., Kashuba, A. D. & Cohen, M. S. Bottlenecks in HIV-1 transmission: insights from the study of founder viruses. Nat. Rev. Microbiol. 13, 414–425 (2015).
Alizon, S. & Fraser, C. Within-host and between-host evolutionary rates across the HIV-1 genome. Retrovirology 10, 49 (2013).
Mueller, S. M. et al. Influence of major HIV-1 protease inhibitor resistance mutations on CTL recognition. J. Acquir. Immune Defic. Syndr. 56, 109–117 (2011).
Theys, K. et al. Treatment-associated polymorphisms in protease are significantly associated with higher viral load and lower CD4 count in newly diagnosed drug- naïve HIV-1 infected patients. Retrovirology 9, 81 (2012).
Theys, K. et al. HIV-1 drug resistance: where do polymorphisms fit in? Future Microbiol. 8, 303–306 (2013).
Roberts, H. E. et al. Structured observations reveal slow HIV-1 CTL escape. PLoS Genet. 11, e1004914 (2015).
Zanini, F. et al. Population genomics of intrapatient HIV-1 evolution. Elife 11, 4 (2015).
Garcia-Knight, M. A. et al. Viral Evolution and Cytotoxic T Cell Restricted Selection in Acute Infant HIV-1 Infection. Sci. Rep. 6, 29536 (2016).
Li, G. et al. An integrated map of HIV genome-wide variation from a population perspective. Retrovirology 12, 18 (2015).
Kinloch, N. N. et al. Population-Level Immune-Mediated Adaptation in HIV-1 Polymerase during the North American Epidemic. J. Virol. 90, 1244–1258 (2015).
Gilbert, M. T. et al. The emergence of HIV/AIDS in the Americas and beyond. Proc. Natl. Acad. Sci. USA 104, 18566–18570 (2007).
Junqueira, D. M. & Almeida, S. E. HIV-1 subtype B: Traces of a pandemic. Virology 495, 173–184 (2016).
Abecasis, A. B. et al. HIV-1 subtype distribution and its demographic determinants in newly diagnosed patients in Europe suggest highly compartmentalized epidemics. Retrovirology 10, 7 (2013).
Paraskevis, D. et al. Tracing the HIV-1 subtype B mobility in Europe: a phylogeographic approach. Retrovirology 6, 49 (2009).
Rambaut, A., Posada, D., Crandall, K. A. & Holmes, E. C. The causes and consequences of HIV evolution. Nat. Rev. Genet. 5, 52–61 (2004).
Capel, E., Martrus, G., Parera, M., Clotet, B. & Martínez, M. A. Evolution of the human immunodeficiency virus type 1 protease: effects on viral replication capacity and protease robustness. J. Gen. Virol. 93, 2625–2634 (2012).
Meixenberger, K. et al. Molecular evolution of HIV-1 integrase during the 20 years prior to the first approval of integrase inhibitors. Virol. J. 14, 223 (2017).
Goulder, P. J. & Watkins, D. I. HIV and SIV CTL escape: implications for vaccine design. Nat. Rev. Immunol. 4, 630–640 (2004).
Woo, J., Robertson, D. L. & Lovell, S. C. Constraints on HIV-1 diversity from protein structure. J Virol. 84, 12995–3003 (2010).
Walker, B. D. & Korber, B. T. Immune control of HIV: the obstacles of HLA and viral diversity. Nat. Immunol. 2, 473–475 (2001).
Crawford, H. et al. Compensatory mutation partially restores fitness and delays reversion of escape mutation within the immunodominant HLA-B*5703-restricted Gag epitope in chronic human immunodeficiency virus type 1 infection. J. Virol. 81, 8346–8351 (2007).
Brockman, M. A. et al. Escape and compensation from early HLA-B57-mediated cytotoxic T-lymphocyte pressure on human immunodeficiency virus type 1 Gag alter capsid interactions with cyclophilin A. J. Virol. 81, 12608–12618 (2007).
Schneidewind, A. et al. Structural and functional constraints limit options for cytotoxic T-lymphocyte escape in the immunodominant HLA-B27-restricted epitope in human immunodeficiency virus type 1 capsid. J. Virol. 82, 5594–5605 (2008).
Barton, J. P. et al. Relative rate and location of intra-host HIV evolution to evade cellular immunity are predictable. Nat. Commun. 7, 11660 (2016).
Santoro, M. M. & Perno, C. F. HIV-1 Genetic Variability and Clinical Implications. ISRN Microbiol. 2013, 481314 (2013).
Goulder, P. J. et al. Evolution and transmission of stable CTL escape mutations in HIV infection. Nature 412, 334–338 (2001).
Kuhn, L. et al. Maternal versus paternal inheritance of HLA class I alleles among HIV-infected children: consequences for clinical disease progression. AIDS 18, 1281–1289 (2004).
Carlson, J. M. et al. HIV-1 adaptation to HLA: a window into virus-host immune interactions. Trends Microbiol. 23, 212–224 (2015).
Schellens, I. M. M. et al. Loss of HIV-1-derived cytotoxic T lymphocyte epitopes restricted by protective HLA-B alleles during the HIV-1 epidemic. AIDS 25, 1691–1700 (2011).
Dilernia, D. A. et al. HLA-driven convergence of HIV-1 viral subtypes B and F toward the adaptation to immune responses in human populations. PLoS One 3, e3429 (2008).
Kawashima, Y. et al. Adaptation of HIV-1 to human leukocyte antigen class I. Nature 458, 641–645 (2009).
Rendine, S. et al. Estimation of human leukocyte antigen class I and class II high-resolution allele and haplotype frequencies in the Italian population and comparison with other European populations. Hum. Immunol. 73, 399–404 (2012).
Yue, L. et al. Cumulative impact of host and viral factors on HIV-1 viral-load control during early infection. J. Virol. 87, 708–715 (2013).
Schneidewind, A. et al. Transmission and long-term stability of compensated CD8 escape mutations. J. Virol. 83, 3993–3997 (2009).
Fryer, H. R., Frater, J., Duda, A. & Roberts, M. G. Modelling the evolution and spread of HIV immune escape mutants. PLoS Pathog. 6, e1001196 (2010).
Hightower, G. K. et al. HIV-1 clade B pol evolution following primary infection. PLoS One 8, e68188 (2013).
Zolla-Pazner, S. Identifying epitopes of HIV-1 that induce protective antibodies. Nat. Rev. Immunol. 4, 199–210 (2004).
Svicher, V. et al. Identification and structural characterization of novel genetic elements in the HIV-1 V3 loop regulating coreceptor usage. Antivir Ther. 16, 1035–1045 (2015).
International Organization for Migration (IOM). IOM Releases Global Migration Statistics 2018, https://migrationdataportal.org/data?i=stock_abs_&t=2017&cm49=380, 07 August 2018.
Brännström, J., Sönnerborg, A., Svedhem, V., Neogi, U. & Marrone, G. A high rate of HIV-1 acquisition post immigration among migrants in Sweden determined by a CD4 T-cell decline trajectory model. HIV Med. 18, 677–684 (2017).
Rhee, S. Y. et al. Human immunodeficiency virus reverse transcriptase and protease sequence database. Nucleic Acids Res. 31, 298–303 (2003).
Shahriar, R. et al. Nonpolymorphic human immunodeficiency virus type 1 protease and reverse transcriptase treatment-selected mutations. Antimicrob. Agents Chemother. 53, 4869–4878 (2009).
Santoro, M. M. et al. Reliability and clinical relevance of the HIV-1 drug resistance test in patients with low viremia levels. Clin. Infect. Dis. 58, 1156–1164 (2014).
Svicher, V. et al. Performance of genotypic tropism testing in clinical practice using the enhanced sensitivity version of Trofile as reference assay: results from the OSCAR Study Group. New Microbiol. 33, 195–206 (2010).
Fabeni, L. et al. Dynamics and phylogenetic relationships of HIV-1 transmitted drug resistance according to subtype in Italy over the years 2000-14. J. Antimicrob. Chemother. 72, 2837–2845 (2017).
Suligoi, B. et al. Detection of recent HIV infections in African individuals infected by HIV-1 non-B subtypes using HIV antibody avidity. J. Clin. Virol. 41, 288–292 (2008).
Selleri, M. et al. Effective highly active antiretroviral therapy in patients with primary HIV-1 infection prevents the evolution of the avidity of HIV-1-specific antibodies. J. Acquir. Immune Defic. Syndr. 46, 145–150 (2007).
Tajima, F. & Nei, M. Estimation of evolutionary distance between nucleotide sequences. Mol. Biol. Evol. 1, 269–285 (1984).
Nei, M. & Gojobori, T. Simple methods for estimating the numbers of synonymous and nonsynonymous nucleotide substitutions. Mol. Biol. Evol. 3, 418–426 (1986).
Alteri, C. et al. Characterization of the patterns of drug-resistance mutations in newly diagnosed HIV-1 infected patients naïve to the antiretroviral drugs. BMC Infect. Dis. 9, 111 (2009).
Yang, O. O. Candidate vaccine sequences to represent intra- and inter-clade HIV-1 variation. PLoS One 4, e7388 (2009).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate-a practical and powerful approach to multiple testing. JR Stat Soc Ser 57, 289–300 (1995).
Kosakovsky Pond, S. L., Weaver, S., Leigh Brown, A. J. & Wertheim, J. O. HIV-TRACE (TRAnsmission Cluster Engine): a Tool for Large Scale Molecular Epidemiology of HIV-1 and Other Rapidly Evolving Pathogens. Mol. Biol. Evol. 35, 1812–1819 (2018).
Pantazis, N. et al. Temporal trends in prognostic markers of HIV-1 virulence and transmissibility: an observational cohort study. Lancet HIV 1, e119–126 (2014).
Pond, S. L., Frost, S. D. & Muse, S. V. HyPhy: hypothesis testing using phylogenies. Bioinformatics 21, 676–679 (2005).
Felsenstein, J. Evolutionary trees from gene frequencies and quantitative characters: finding maximum likelihood estimates. Evolution 35, 1229–1242 (1981).
Acknowledgements
This work was financially supported by the European Commission Framework 7 Programme (CHAIN, the Collaborative HIV and Anti-HIV Drug Resistance Network, Integrated Project no. 223131), the Italian Ministry of Health (Progetto Ricerca Corrente 2016, line n. 2, project n. 2, sub-project n. 2d), the Italian Ministry of Education, University and Research (MIUR) (Bandiera InterOmics Protocollo PB05 1°) and an unrestricted grant from AVIRALIA foundation. We gratefully thank A. Biddittu, M. Bruni, M. Romani for data management, and F. McDonald and D. Mandatori for English revision and editing.
Author information
Authors and Affiliations
Contributions
C.A. conceived the presented idea, developed and performed the analyses, and wrote the manuscript. L.F., R.S., G.B. and D.D.C. contributed to perform the statistical analyses. C.G., A.B., and G.B. determined the pol and V3 sequences. A.V., I.M., R.B., C.M., M.C., F.M., A.P., C.M.M., E.G., M.A. and A.A. provided samples. M.M.S. and L.F. contributed to the writing of the manuscript. M.M.S., V.S., F.C.S. and C.F.P. contributed to the interpretation of the results and revised the manuscript. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no financial and non-financial competing interests that might be perceived to influence the results and/or discussion reported in this paper. However, Francesca Ceccherini-Silberstein reports personal fees from Gilead Sciences, Bristol-Myers Squibb, Abbvie, Roche Diagnostics, Janssen-Cilag, Abbott Molecular, ViiV Healthcare; grants and personal fees from Merck Sharp & Dohme; grants from Italian Ministry of Education, University and Research (MIUR). Carlo Federico Perno reports grants from Italian Ministry of Instruction, University and Research (MIUR), and from Aviralia Foundation; personal fees from Gilead Sciences, Abbvie, Roche Diagnostics, Janssen-Cilag, Abbott Molecular; and grants and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, and ViiV Healthcare. All other authors have nothing to declare.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alteri, C., Fabeni, L., Scutari, R. et al. Genetic divergence of HIV-1 B subtype in Italy over the years 2003–2016 and impact on CTL escape prevalence. Sci Rep 8, 15739 (2018). https://doi.org/10.1038/s41598-018-34058-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34058-7
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.