Abstract
The aim of this study was to investigate the prognostic value of the lymphocyte-to-monocyte ratio (LMR) in patients undergoing hepatectomy and to compare it to established biomarkers including the neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR). Medical records were retrospectively analyzed for 652 HCC patients undergoing hepatectomy at the Affiliated Tumor Hospital of Guangxi Medical University and the First People’s Hospital of Changde between April 2004 to April 2012. The correlation between the LMR and clinical variables were analyzed in Kaplan-Meier log-rank survival analysis and then multivariate Cox regression models trying to find relation with disease-free survival (DFS) and overall survival (OS). The area under the ROC curve (AUC) of the LMR(AUC:0.627) for predicting long-term survival was greater than that of the NLR(AUC:0.600) and the PLR(AUC:0.520).Multivariate analysis showed LMR to be an independent risk factor for OS (P = 0.002), and the NLR and PLR were not independently significant. Subgroup analysis also showed that LMR was significantly associated with poor DFS and OS in patients positive for HBsAg or with cirrhosis (both P < 0.001).Elevated preoperative LMR is an independently associated with poor OS and DFS in HCC patients following curative resection and appears to be superior to NLR and PLR.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies in the world and the third leading cause of tumor death1,2,3,4. Although hepatectomy has achieved significant improvements, the prognosis of patients with liver cancer is far from satisfactory, due to distant metastasis and tumor recurrence5,6,7,8. Recently, the use of inflammatory and molecular biomarkers to improve the prognosis of HCC has received increasing attention. However, there is still a lack of reliable, low-cost tumor markers that can be easily applied to clinic to predict prognosis.
There is more and more consensus that inflammation is associated with the development of malignant tumors and that persistent systemic inflammatory responses is involved with poor prognosis in many cancers9,10,11,12,13. One widely studied inflammatory markers originated from full blood count are the lymphocyte-to-monocyte ratio (LMR), the neutrophil-to-lymphocyte ratio (NLR) and the platelet- to lymphocyte ratio (PLR), which have been identified as prognostic biomarker in HCC7,14,15,16.
However, there are few studies to compare the ability of the LMR, NLR and PLR to predict long-term survival among patients with HCC undergoing liver resection with curative intent. Although Yang YT et al. have shown that lymphocyte to monocyte ratio and neutrophil to lymphocyte ratio are superior inflammation-based predictors of recurrence in patients with hepatocellular carcinoma after hepatic resection, they did not conduct survival analysis of over survival(OS)16.
In light of these, the present study aimed to compare the relative prognostic value of the preoperative LMR, NLR and PLR in disease-free survival(DFS) and OS in HCC patients with an attempt to clarify the optimal use of these markers.
Materials and Methods
This research was approved by the Ethics Committee of the First People’s Hospital of Changde and the Tumor Hospital of Guangxi Medical University, and written informed consent was obtained from patients prior to surgery. All treatments were performed in accordance with relevant guidelines and regulations.
Patients
All HCC patients underwent hepatectomy with curative intent at the First People’s Hospital of Changde City and the Affiliated Tumor Hospital of Guangxi Medical University between April 2004 and April 2012 were included in our study. The inclusion criteria were: no treatment for HCC before hepatectomy; initial hepatectomy with curative intent performed at the authors’ center; no other simultaneous malignancies; no coexistent hematologic disorders and no preoperative fever, so that the preoperative platelet count, neutrophil, lymphocyte and monocyte reflected normal baseline values; and no renal, cerebral, or cardiopulmonary dysfunction before hepatectomy.
Diagnosis and definitions
Diagnose of HCC was based on the results of postoperative pathology. Hepatectomy with curative intent is defined as complete resection of all visible tumor and no residual tumor cells at surgical margins17. Preoperative NLR, LMR and PLR were determined within 7 d before surgery.
Follow-up visits
All patients were followed up one month after liver resection and followed by a three-month interval in the first year, and then every 3–6 months in subsequent years, as appropriate. At each follow-up, serum AFP assay, ultrasound, serum biochemistry, chest X-ray and abdominal CT or MRI were performed.
Statistical analysis
Statistical analysis was carried out with SPSS 19.0 (IBM, USA). Intergroup differences in continuous variables were compared by t-test or Mann–Whitney U test, as appropriate. While intergroup differences in categorical data were analyzed by two-sided χ2 test, Mann–Whitney U test or Fisher’s exact test, as appropriate. The area under the receiver operating characteristic (ROC) curve was calculated to measure the discriminatory power of the LMR, NLR and PLR as predictors of overall survival(OS). And an optimal cutoff value of 4.01, 2.78 and 99.5 corresponded to the maximum joint sensitivity and specificity on the ROC plot for LMR, NLR and PLR. Survival analysis was conducted to compare the over survival(OS) and disease free survival(DFS) rates using Kaplan-Meier survival curves with log-rank tests and Cox proportional hazard regression analyses, and p < 0.05 was considered statistically significant.
Data sharing statement
Technical appendix, statistical code, and dataset are available from the corresponding author at cdsdyrmyy01@163.com. Participants gave informed consent for data sharing.
Results
Baseline characteristics of all patients
Of 854 consecutive patients who underwent hepatic resection with curative intent from April 2004 to April 2012 inclusive, 145 patients (16⋅9%) experienced other treatments before hepatectomy; 20 patients (2⋅3%) had other malignant tumors simultaneously; 25 patients (2⋅9%) had preoperative fever and coexistent hematologic disorders, and 12 patients (1⋅4%) had cardiopulmonary, cerebral or renal dysfunction before hepatectomy. After exclusion, 652 patients (76⋅3%) were enrolled in our study.
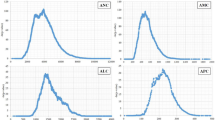
Our study were consisted of 566 males and 86 females. Details of baseline characteristics of all HCC patients and separately in the low and high LMR groups can be seen in Table 1. ROC analysis found the optimal cutpoint for the LMR, NLR, and PLR were 4.01, 2.78 and 99.5, respectively (Fig. 1). The area under the ROC curve (AUC) of the LMR (AUC:0.627) for predicting long-term survival was greater than that of the NLR (AUC:0.600) and the PLR(AUC:0.520).
Receiver operating curve (ROC) for the preoperative LMR, NLR and PLR in predicting long-term survival with an optimal cutoff value of 4.01 (sensitivity:62.1 percent,specifiity:59.2 percent, AUC:0.627) for LMR, 2.78 (sensitivity:30.9 percent,specifiity:81.6 percent, AUC:0.600) for NLR, and 99.5 (sensitivity:47.9 percent, specifiity:57.9 percent, AUC:0.520) for PLR. AUC: (LMR, 0.656 vs. PLR, 0.600 P < 0.001).
A lower LMR was significantly associated with higher values of AFP, tumor number, tumor size, PLT and AST (all P < 0.05). On the other hand, A lower LMR was significantly associated with lower values of albumin (P < 0.05). The lower LMR was also strongly associated with both higher NLR (P < 0.001) and higher PLR (P < 0.001). Especially, high NLR was more likely in the low LMR group (40.5%) compared to both the overall cohort (25.6%) and those with high LMR (9.3%).
Cox analyses of survival associated with LMR
Univariate analysis and cox proportional hazards regression were used to identify factors associated with OS and DFS and the detailed results were shown in Table 2.
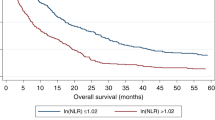
Univariate analysis identified the following factors significantly associated with poor OS: LMR < 4.01, AFP ≥ 400 ng/mL, BCLC stage B or C, multiple tumors, tumor size ≥ 5 cm, incomplete tumor capsule, AST ≥ 80 U/L, NLR ≥ 2.78 and PLR ≥ 99.5. LMR < 4.01, AFP ≥ 400 ng/mL, BCLC stage B or C, multiple tumors, tumor size ≥ 5 cm, incomplete tumor capsule, NLR ≥ 2.78 and PLR ≥ 99.5 were also found to be significantly associated with poor DFS (Table 2, Fig. 2).
Multivariate analysis (Table 2) identified the following prognostic independent predictors of poor OS: LMR < 4.01, BCLC stage B or C, multiple tumors, tumor size ≥ 5 cm and incomplete tumor capsule. LMR < 4.01, AFP ≥ 400 ng/mL, B multiple tumors, tumor size ≥ 5 cm, incomplete tumor capsule and NLR ≥ 2.78 were also found to be significantly associated with poor DFS.
Subgroup analyses associated with LMR
To clarify the subgroups of patients influenced by preoperative LMR, we grouped the patients according to HBV infection and liver cirrhosis, we discovered LMR was significantly associated with poor OS and DFS for patients with or without HBV infection (all P < 0.01; Fig. 3). LMR was also significantly associated with poor OS and DFS for patients with liver cirrhosis (both P < 0.001; Fig. 4B,D) but not for patients without cirrhosis (P = 0.466; Fig. 4C).
Discussion
Our research implies that the preoperative LMR is an independent indicator of poor OS and DFS in HCC patients suffered curative resection. Furthermore, in the subgroup of patients positive for HBsAg or with cirrhosis, we found that the LMR was also significantly associated with OS and DFS.
We have also defined optimal cutpoints for LMR, NLR and PLR in the ROC analysis, with values of 4.01, 2.78 and 99.5, respectively. And we have found the area under the ROC curve (AUC) of the LMR (AUC:0.627) for predicting long-term survival was greater than that of the NLR (AUC:0.600) and the PLR(AUC:0.520). Furthermore, we have also found the LMR is a better indicator for long-term survival compared to NLR and PLR, both publicly known independent indicators of OS and DFS7,14,18,19. Before this research, studies had usually reported the NLR is superior to the PLR16,20,21. However, when studied with LMR, we found both NLR and PLR were not independent indicator for OS. What’s more, the cutpoints applied in my study for NLR and PLR of 2.78 and 99.5, respectively were consistent with previous researches19,22.
The mechanism of why decreased LMR should indicate poor survival remains unclear, but some researches have given some explanations. As far as we know, as early as the 1970s, these markers of lymphocyte components have been fully confirmed in the study in which lymphocytopenia were observed in patients with advanced tumor23. This has been one of the foundations of other established inflammatory markers, such as PLR and NLR. Although the correlation between monocytes and prognosis have been evaluated recently, only preliminary hypotheses have been made to explain why monocytes may indicate prognostic information. Here we put forward several possible mechanisms. First, previous study have found circulating monocytes may promote tumor growth and help tumor cells escape immune surveillance24,25. Second, derived from circulating monocytes, tumor-associated macrophages (TAMs) have been reported to be able to infiltrate into the HCC matrix, exerting activity including promotion of proliferation, metastasis, angiogenesis and immunosuppression26,27,28,29.
Although offering some new findings, this study has several limitations that need to be addressed. On one hand, since the value of LMR is dynamic during follow-up, we use only baseline values to predict future results, so we may miss a lot of information. On the other hand, due to the nature of the retrospective study, the potential choice bias exists.
In summary, our study suggests that the LMR is superior to the NLR and PLR, both established independent indicators of OS. However, a larger prospective study are needed to prove our researches.
References
Alkozai, E. M. et al. Immediate Postoperative Low Platelet Count is Associated with Delayed Liver Function Recovery After Partial Liver Resection. Ann Surg. 251, 300–306 (2010).
Nguyen, V. T., Law, M. G. & Dore, G. J. Hepatitis B-Related Hepatocellular Carcinoma: Epidemiological Characteristics and Disease Burden. J Viral Hepat. 16, 453–463 (2009).
Yang, H. et al. Cyclooxygenase-2 Expression is Associated with Initiation of Hepatocellular Carcinoma, while Prostaglandin Receptor-1 Expression Predicts Survival. World J Gastroentero. 22, 8798 (2016).
Yang, H. et al. Stratified Aspartate Aminotransferase-to-Platelet Ratio Index Accurately Predicts Survival in Hepatocellular Carcinoma Patients Undergoing Curative Liver Resection. Tumor Biol. 39, 568836102 (2017).
Forner, A., Llovet, J. M. & Bruix, J. Hepatocellular Carcinoma. Lancet. 379, 1245–1255 (2012).
Guo, Z. et al. Comparison of Survival of Patients with Bclc Stage a Hepatocellular Carcinoma After Hepatic Resection Or Transarterial Chemoembolization: A Propensity Score-Based Analysis. Ann Surg Oncol. 21, 3069–3076 (2014).
Yang, H. et al. Blood Neutrophil-Lymphocyte Ratio Predicts Survival After Hepatectomy for Hepatocellular Carcinoma: A Propensity Score-Based Analysis. World J Gastroentero. 22, 5088 (2016).
Zhong, J. et al. Hepatic Resection Associated with Good Survival for Selected Patients with Intermediate and Advanced-Stage Hepatocellular Carcinoma. Ann Surg. 260, 329–340 (2014).
Berardi, R. et al. Prognostic Models to Predict Survival in Patients with Advanced Non-Small Cell Lung Cancer Treated with First-Line Chemo- Or Targeted Therapy. Oncotarget. (2016).
Chan, A. W. H. et al. Prognostic Nutritional Index (Pni) Predicts Tumor Recurrence of Very Early/Early Stage Hepatocellular Carcinoma After Surgical Resection. Ann Surg Oncol. 22, 4138–4148 (2015).
Cummings, M. et al. Preoperative Neutrophil:Lymphocyte and Platelet:Lymphocyte Ratios Predict Endometrial Cancer Survival. Brit J Cancer. 113, 311–320 (2015).
Diakos, C. I., Charles, K. A., McMillan, D. C. & Clarke, S. J. Cancer-Related Inflammation and Treatment Effectiveness. Lancet Oncol. 15, e493–e503 (2014).
Neofytou, K. et al. The Preoperative Lymphocyte-to-Monocyte Ratio is Prognostic of Clinical Outcomes for Patients with Liver-Only Colorectal Metastases in the Neoadjuvant Setting. Ann Surg Oncol. 22, 4353–4362 (2015).
Li, X. et al. Platelet-to-Lymphocyte Ratio Acts as a Prognostic Factor for Patients with Advanced Hepatocellular Carcinoma. Tumor Biol. 36, 2263–2269 (2015).
Song, W. et al. Clinicopathological and Prognostic Significance of Platelet-to-Lymphocyte Ratio in Patients with Hepatocellular Carcinoma. Oncotarget. (2016).
Yang, T. et al. Lymphocyte to Monocyte Ratio and Neutrophil to Lymphocyte Ratio are Superior Inflammation-Based Predictors of Recurrence in Patients with Hepatocellular Carcinoma After Hepatic Resection. J Surg Oncol. (2017).
Hermanek, P. & Wittekind, C. The Pathologist and the Residual Tumor (R) Classification. Pathol Res Pract. 190, 115–123 (1994).
Mano, Y. et al. Preoperative Neutrophil-to-Lymphocyte Ratio is a Predictor of Survival After Hepatectomy for Hepatocellular Carcinoma. Ann Surg. 258, 301–305 (2013).
Okamura, Y. et al. Neutrophil to Lymphocyte Ratio as an Indicator of the Malignant Behaviour of Hepatocellular Carcinoma. Br J Surg. (2016).
Ji, F. et al. A Novel and Accurate Predictor of Survival for Patients with Hepatocellular Carcinoma After Surgical Resection: The Neutrophil to Lymphocyte Ratio (Nlr) Combined with the Aspartate Aminotransferase/Platelet Count Ratio Index (Apri). Bmc Cancer. 16 (2016).
Yamamura, K. et al. Comparison of Inflammation-Based Prognostic Scores as Predictors of Tumor Recurrence in Patients with Hepatocellular Carcinoma After Curative Resection. J Hepatobiliary Pancreat Sci. 21, 682–688 (2014).
Shen, S. et al. Preoperative Aspartate Aminotransferase to Platelet Ratio is an Independent Prognostic Factor for Hepatitis B-Induced Hepatocellular Carcinoma After Hepatic Resection. Ann Surg Oncol. 21, 3802–3809 (2014).
Kim, U. S. & Papatestas, A. E. Letter: Peripheral Lymphocyte Counts in Colonic Disease. Lancet. 2, 462–463 (1974).
Augier, S. et al. Inflammatory Blood Monocytes Contribute to Tumor Development and Represent a Privileged Target to Improve Host Immunosurveillance. J Immunol. 185, 7165–7173 (2010).
Hu, Y. C. et al. Overexpression of Rip140 Suppresses the Malignant Potential of Hepatocellular Carcinoma by Inhibiting Nfkappabmediated Alternative Polarization of Macrophages. Oncol Rep. 37, 2971–2979 (2017).
Galdiero, M. R. et al. Tumor Associated Macrophages and Neutrophils in Cancer. Immunobiology. 218, 1402–1410 (2013).
Jackaman, C. et al. Aging and Cancer: The Role of Macrophages and Neutrophils. Ageing Res Rev. 36, 105–116 (2017).
Yan, C., Yang, Q. & Gong, Z. Tumor-Associated Neutrophils and Macrophages Promote Gender Disparity in Hepatocellular Carcinoma in Zebrafish. Cancer Res. 77, 1395–1407 (2017).
Zhu, X. D. et al. High Expression of Macrophage Colony-Stimulating Factor in Peritumoral Liver Tissue is Associated with Poor Survival After Curative Resection of Hepatocellular Carcinoma. J Clin Oncol. 26, 2707–2716 (2008).
Acknowledgements
The study was reviewed and approved by the Tumor Hospital of Guangxi Medical University and the First People’s Hospital of Changde City Institutional Review Boards. All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Author information
Authors and Affiliations
Contributions
Yu-Ting Yang, Jing-Hang Jiang and Hao-Jie Yang contributed equally to this work. Bang-De Xiang and Ze-Min Xiao contributed equally to this work; Yu-Ting Yang, Bang-De Xiang and Ze-Min Xiao contributed to the study design and conception. Jing-Hang Jiang and Zhi-jun Wu collected the relative data. Hao-Jie Yang and Yu-Ting Yang analyzed and interpreted the data. Hao-Jie Yang, Yu-Ting Yang, and Bang-De Xiang contributed to editing of the article. Bang-De Xiang and Ze-Min Xiao contributed to quality control and review of the data and article.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, YT., Jiang, JH., Yang, HJ. et al. The lymphocyte-to-monocyte ratio is a superior predictor of overall survival compared to established biomarkers in HCC patients undergoing liver resection. Sci Rep 8, 2535 (2018). https://doi.org/10.1038/s41598-018-20199-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-20199-2
This article is cited by
-
Prognostic impact of osteosarcopenia in patients undergoing pancreatic resection for pancreatic ductal adenocarcinoma
Langenbeck's Archives of Surgery (2024)
-
Prognostic utility of systemic inflammatory markers and chronic hepatitis C virus infection status in hepatocellular carcinoma patients treated with local ablation
BMC Cancer (2022)
-
Clinical importance of the absolute count of neutrophils, lymphocytes, monocytes, and platelets in newly diagnosed hepatocellular carcinoma
Scientific Reports (2021)
-
Lymphocyte to monocyte ratio-based nomogram for predicting outcomes of hepatocellular carcinoma treated with sorafenib
Hepatology International (2020)
-
Transarterial chemoembolization combined with radiofrequency ablation for solitary large hepatocellular carcinoma ranging from 5 to 7 cm: an 8-year prospective study
Abdominal Radiology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.