Abstract
The Up-to-seven (UTS) criteria (sum of tumor size and number not exceeding 7) for indicating liver transplantation (LT) in hepatocellular carcinoma (HCC) were originally based on explant pathology features and absence of microvascular invasion (MVI). 18F-fludeoxyglucose (18F-FDG) positron emission tomography (PET) was shown to indicate the risk of MVI and tumor recurrence. The aim of this study was to analyze the prognostic significance of the clinical UTS criteria when being combined with PET-status of the tumor. Data of 116 liver transplant patients were subject to retrospective analysis. Five-year recurrence-free survival (RFS) rates in patients meeting (n = 85) and exceeding (n = 21) the radiographic UTS criteria were 81% and 55.1%, respectively (p = 0.014). In the UTS In subset, RFS was significantly better in PET-negative (94.9%) than in PET-positive patients (48.3%; p < 0.001). In the UTS Out subset, 5-year RFS rates were 87.1% and 19% in patients with non- 18F-FDG-avid and 18F-FDG-avid tumors (p < 0.001), respectively. Positive PET-status was identified as the only independent clinical predictor of tumor recurrence in beyond UTS patients (Hazard ratio [HR] 19.25; p < 0.001). Combining radiographic UTS criteria with FDG-PET may safely expand the HCC selection criteria for LT.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is currently the fifth most common cancer and the third most common reason of cancer-related death worldwide1,2. Surgical resection is the treatment of choice. However, due to underlying cirrhosis with related liver dysfunction, major hepatectomy is often not practicable3,4. From an oncological point of view, liver transplantation (LT) is the best treatment option, since it removes the tumor and the tumor-generating cirrhosis5,6. Early experiences with LT for HCC were limited by high recurrence rates and poor survival7,8. In a landmark study of 1996, Mazzaferro et al. were able to demonstrate that LT in early stage HCC leads to excellent long-term outcome that was not different from patients with non-malignant diseases. Overall (OS) and recurrence-free survival (RFS) rates at 4 years post-LT were 85% and 92% for patients meeting the so-called Milan criteria (MC; one single HCC nodule of up to 5 cm, or a maximum of 3 tumor nodules, each not exceeding 3 cm and absence of macrovascular invasion), but only 50% and 59% for those exceeding them9,10. Consequently, the MC were implemented as standard for selecting suitable liver transplant recipients in the major allocation areas around the world.
In recent years, there is a growing concern that the MC may be too restrictive and inappropriate to satisfy continuously growing waiting list demands11,12. Several studies have shown that a subset of patients with HCC exceeding standard criteria may benefit from LT. Accordingly, numerous expanded criteria sets were proposed in the last two decades, such as the University of California (UCSF)13, Toronto14, Valencia15 and Hangzhou criteria16, to name just a few of them.
In 2009, Mazaferro et al. introduced the so-called Up-to-seven (UTS) criteria by simply combining the largest tumor nodule size and the number of HCC nodules, which should not exceed 7 in sum. In a large European multicenter trial including 1556 liver transplant recipients, they demonstrated that patients with HCC exceeding the MC but still meeting the UTS criteria have an excellent prognosis that was not different from patients meeting standard criteria HCC17. However, the authors have used post-LT generated histopathologic and not pre-LT radiographic features for their investigation18. Apart from that, beneficial outcome of the expanded HCC subset was related to lack of microvascular tumor invasion (MVI)17.
Tumor invasion into microscopic vessels is recognized as a major indicator of aggressive tumor behaviour and poor outcome19,20. However, it may reliably be assessed only on explant pathology and not by conventional radiographic imaging21. Therefore, for a safe application of the UTS criteria, the implementation of appropriate clinical biomarkers of tumor aggressiveness seems to be mandatory20.
In recent years, several transplant groups were able to demonstrate that 18F-fludeoxyglucose (18F-FDG) positron emission tomography (PET) provides useful information on metabolic tumor viability and posttransplant outcome22,23,24. PET-positivity was shown to correlate with presence of unfavourable histopathologic features, like MVI and poor grading23,25,26.
The primary aim of this retrospective study was to analyze the prognostic value of the UTS criteria when being based on pretransplant imaging. Apart from that, we investigated whether the combination of the radiographic UTS criteria with 18F-FDG PET may be useful for predicting posttransplant tumor recurrence and, thus, for safely expanding the pool of suitable liver transplant patients.
Methods
Subjects
The study protocol was approved by the local Ethics Committee (Ethical committee of the Medical School, Technical University Munich, Nr. 217/15). Patients’ registration, waiting list management and transplant procedures were performed according to national law and re-gulations. Prior to LT, all patients gave informed consent that follow-up data may be used for study purpose and respective publication. This work was supported by the German research Foundation (DFG) and the Technische Universität München within the funding programme Open Access Publishing.
From a prospectively updated data base (1996 to 2012; two-center study under same personal responsibilities and conditions), 116 patients that underwent LT for HCC were identified. Tumor diagnosis was established by clinical staging (radiographic imaging by computed tomography [CT] and/or magnetic resonance tomography [MRI] + alpha-fetoprotein level [AFP] measurement) without tumor biopsy. The minimum cut-off tumor nodule size for diagnostic purpose was 1 cm. The MC were primarily used for justifying patients’ listing.
Since December 2007, patients with HCC meeting the MC received exceptional priority status according to the model of end-stage liver disease (MELD) score. Based on HCC topography and remaining liver function, transarterial chemotherapy (TACE) as bridging to LT has been performed. Pretransplant tumor surveillance consisted of liver ultrasound and AFP level determination every 6 weeks, and CT/MRI scan minimum biannually. Additional radiographic imaging was performed when required, such as post-TACE, prior to MELD score upgrading and in the case of tumor-related symptoms.
Progression of tumor load beyond the MC resulted in loss of MELD exceptional priority status. Apart from that, a concise re-evaluation by computed tomography (CT) and/or magnetic resonance tomography (MRI) and AFP level determination every 3 months was initiated. According to an individual decision making process, these patients were primarily scheduled for center-based liver allocation, unless macrovascular tumor infiltration, lymph node infiltration or extrahepatic tumor spread (biological tumor progression) became evident.
18F-FDG PET was performed in all patients with liver malignancy in order to exclude extrahepatic tumor manifestation. The prospectively collected data were retrospectively used for the assessment of metabolic tumor properties.
As previously described, we distinguished between PET-positive (PET+ status; 18F-FDG-avid) and PET-negative (PET– status; non- 18F-FDG-avid) tumors. This classification was based on concise visual FDG-uptake assessment of each tumor nodule in very close morphological demarcation to the surrounding non-tumorous liver regions. Any significantly enhanced 18F-FDG uptake pattern compared to normal adjacent liver tissue (tumor to non-tumor maximum standard uptake value > 1) was indicating PET+ status of HCC22,23.
Based on final pretransplant radiographic staging, patients were classified as Milan In (HCC meeting the MC; Milan In) or Milan Out (HCC exceeding the MC; Milan Out), and UTS In (HCC meeting the UTS criteria; UTS In) and UTS Out (HCC exceeding the UTS criteria; UTS Out), respectively.
Transplant procedure and posttransplant follow-up
ABO-compatible deceased donor liver grafts were used for transplant procedure in all study patients. Venous reconstruction was performed by using the piggy back technique without veno-venous bypass. In order to avoid the theoretical risk of systemic tumor cell spread, we have not used intraoperative blood salvage autotransfusion. Posttransplant immunosuppression consisted of a calcineurin inhibitor based regimen either by cyclosporine A or tacrolimus augmented by azathioprine or mycophenolate mofetil. Prednisone was withdrawn latest 3 months post-LT with exception of pre-existing autoimmune hepatitis. Tumor surveillance post-LT consisted of AFP-level determination and liver ultrasound at least every three months. Apart from that, CT scans of the chest and abdomen were performed every 6 months during the first posttransplant year and minimum thereafter or in case of suspected HCC relapse.
Statistical analysis
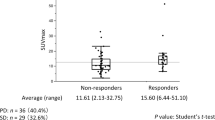
Categorical variables were compared using the χ2 test. Continuous variables were recorded by median and range, and compared using the Student’s t test.
The Kaplan-Meier method was performed to determine overall survival (OS) and recurrence-free survival (RFS) rates. Variables being significant for predicting HCC relapse in univariate analysis (p < 0.05) were entered into a stepwise multivariate logistic Cox regression model in order to identify independent prognostic factors (p < 0.05). Only pretransplant available clinical features were included in the analysis. All statistical analyses were performed by using the software SPSS 23.0 (IBM Inc., Munich, Germany).
Results
Clinicopathologic characteristics
The baseline clinicopathologic characteristics are summarized in Table 1.
Preoperative PET imaging demonstrated 41 PET-positive (35.3%) and 75 PET-negative tumors (64.7%).
Based on clinical staging, 66 patients were classified as Milan In (56.9%) and 50 patients as Milan Out (43.1%), whereas tumors were meeting and exceeding the UTS criteria in 85 (73.3%) and 21 (26.7%) patients, respectively. UTS In and UTS Out patients did not significantly differ with regard to gender, age, liver diseases, Child classification, MELD score, AFP level, TACE and PET status. Explant histopathological studies revealed more tumors demonstrating with MVI in the UTS Out subset (Table 1).
Overall survival and tumor recurrence
Posttransplant follow-up was ranging between 5 and 184 months (median: 74). OS rates were 82.7% and 75.6% at 3 and 5 years post-LT. Posttransplant HCC relapse was confirmed in 29 patients (25%) after a median of 11 months (range: 4–55).
Corresponding RFS rates were 77.2% and 74.4% at 3 and 5 years, respectively.
In univariate analysis, AFP level, multiple tumor nodules, maximum tumor diameter, number of HCC nodules, UTS criteria and PET-status were significantly associated with risk of HCC recurrence. Only positive PET-status, AFP level > 400 ng/nl and manifestation of multiple HCC nodules were identified as significant and independent predictors of HCC recurrence on multivariate analysis (Table 2).
Outcome according to the Milan and UTS criteria
OS rates among Milan In and Milan Out patients were 89.4% and 81.7%, and 74% and 62.7% at 3 and 5 years post-LT (Fig. 1; p < 0.001). There were 9 HCC recurrences in the Milan In subset (13.6%), whereas 20 Milan Out patients (40%) developed tumor relapse (p = 0.001). RFS rates were 86.2% and 86.2% among Milan In patients, but only 65.4% and 58.4% in patients with Milan Out HCC (Fig. 2; p = 0.001).
We found significantly better OS in patients meeting (85.9%, 77.4%) than in those exceeding the UTS criteria (74.2%, 63.2%; p = 0.034; Fig. 3).
Sixteen UTS In (18.8%) and 13 beyond UTS patients (41.9%; p = 0.011) developed HCC recurrence.
Thus, RFS rates at 3- and 5-years post-LT were 81% and 81% in patients meeting, but only 66.7% and 55.1% in those exceeding the UTS criteria (p = 0.014; Fig. 4), respectively.
PET-positivity and presence of more than 3 tumor nodules were identified as the only significant and independent clinical predictors of HCC recurrence among UTS In patients (Table 3). In this subset, RFS was significantly better in PET-negative (94.9%; 94.9%) than in PET-positive patients (48.3%; 48.3%; p < 0.001; Fig. 5).
Only PET-positivity remained as significant and independent predictor of HCC recurrence in beyond UTS patients (Table 4). In this subgroup, we recorded 3- and 5-year RFS rates of 93.8% and 87.1% in non- 18F-FDG-avid, but only 35.7% and 19% in 18F-FDG-avid patients (p < 0.001; Fig. 6), respectively. RFS was comparable between UTS In and PET-negative beyond UTS patients (p = 0.534; Fig. 7).
Clinicopathologic differences between Milan In (n = 66), Milan Out/UTS In (n = 19), and beyond UTS patients (n = 31) are listed in Table 5.
Tumor recurrence rate was significantly lower, OS and RFS were both significantly better in Milan In patients as compared to the other two subsets. In contrast, there were no significant outcome differences between Milan Out/UTS In patients and patients with beyond UTS tumors (Table 5).
In the Milan Out/UTS In subgroup, 5-year RFS rates were 80% in PET-positive and 44.4% PET-negative patients (p = 0.078; Fig. 8). There was no significant difference in tumor-specific outcome between Milan In patients and patients with PET-negative Milan Out/UTS In tumors (p = 0.639; Fig. 9).
PET correlations with tumor characteristics and outcome
Table 6 describes the correlations of PET-status with clinicopathologic tumor variables and posttransplant outcome.
Positive PET-status correlated significantly with tumor nodule size and total tumor diameter, whereas it tended to be associated with elevated AFP levels. Apart from that, enhanced 18F-FDG uptake on PET was significantly correlated with presence of aggressive histopathologic features (Table 6).
Among PET-negative patients, OS and RFS rates were 97.3% and 88.7%, and 94.6% and 93.3% at 3- and 5-years, which was significantly higher than in PET+ patients (63.4% and 46.3%; 43.8% and 38.1%; p < 0.001). Tumor recurrence rate was 6.7% in non- 18F-FDG-avid patients, but 58.5% in those with PET+ tumors (p < 0.001; Table 6).
Discussion
At first sight, our data seem to implicate that expansion to the clinical UTS criteria does not dramatically increase the risk of tumor recurrence. We found considerable 5year RFS rates in patients meeting the radiographic UTS criteria (81%), which was only slightly inferior to the Milan In cohort (86.2%). Apart from that, an additional of 19 patients beyond the MC could, thereby, be declared as being suitable for LT (Table 5), which corresponds to an increase of 19.6%. Insofar, our study seems to validate the UTS criteria on basis of clinical staging. However, in the additionally recruited patients with tumors exceeding the MC but still meeting the UTS criteria (n = 19), the tumor recurrence rate was significantly higher (36.8% versus 13.6%; p = 0.023), and OS (62.2% versus 81.7%; p = 0.001) and RFS rates (63.2% versus 86.2%; p = 0.017) were both significantly lower compared to the Milan In subset (Table 5). Probably, just because of the small sample size, this has not yet become noticeable in the overall survival. Therefore, on closer examination, our data rather indicate that the undifferentiated application of the UTS criteria enhances the oncological risk.
Whether our results finally justify the implementation of the UTS criteria is a matter of critical discussion. Liberalizing the transplant criteria without expanding the pool of available donor organs results in growing waiting lists and prolongation of pre-LT waiting times. This may in turn enhance the drop out risk following tumor progression. Recently, Volk et al. identified a threshold survival of 61% at 5 years to be required for balancing benefit and harm of LT in advanced HCC patients, at least in the US27. In our Milan Out/UTS In cohort, 5-year OS and RFS rates were 61% and 63.2% (Table 5), respectively, which exceeded this cut-off value. However, a tumor relapse risk about 40% in an additionally selected expanded criteria HCC subset may be unacceptable, particularly in view of an escalating donor organ shortage28.
In recent years, several trials emphasized on the predictive power of the UTS criteria17,29,30,31. Nevertheless, they have not yet been implemented as standard for patients’ selection. It was a major limitation of these studies that pathomorphometric and not radiographic UTS features were used. Well-known discrepancies between pre- and posttransplant tumor staging may have limited clinical applicability32. Apart from that, absence of MVI contributed substantially to the prognostic value of the UTS criteria, which additionally hampered their implementation into clinical routine17,29,30,31. In order to create a realistic clinical scenario, we were using only pretransplant available variables in our analysis. Nevertheless, our data indirectly confirmed the specific significance of MVI in this setting, as tumor recurrence rate was significantly higher in the Milan Out/UTS In patients compared to the Milan In subset when MVI was not considered (Table 5).
In fact, vascular tumor invasion is one of the most important prognostic features in LT for HCC19,20. While macrovascular infiltration may be appropriately detected by modern radiographic imaging and generally excludes patients from LT, MVI may reliably be confirmed only post-LT33,34. Pretransplant tumor biopsy is inappropriate due to high risk of sample errors caused by intratumoral heterogeneity21. Apart from that, there is a theoretical risk of tumor cell seeding that might affect posttransplant prognosis35.
Since tumor load correlates with risk of MVI and poor grading36,37, clinical surrogate markers of tumor aggressiveness are essential for safely expanding macromorphometric selection limits. In the past, response to TACE38, AFP-level39, C-reactive protein40, PIVKA II41, yglutamyltransferase42 and 18F-FDG PET22,24 were applied for biological tumor evaluation. Among them, increased 18F-FDG uptake on PET was shown to be highly associated with unfavorable histopathology and risk of tumor recurrence43,44,45.
18F-FDG PET is a well-established non-invasive tool for metabolic imaging of different malignancies46. Like glucose, 18F-FDG is uploaded by the tumor cells via several overexpressed glucose transporters. Well differentiated HCC nodules exhibit an enzyme activity that is not different to that of normal liver tissue, resulting in a similar FDG uptake pattern. On contrary, poorly differentiated HCCs are characterized by enhanced FDG uptake pattern as compared to the surrounding healthy liver regions. In contrast to several other cancers, 18F-FDG-PET is therefore not appropriate for detection of HCC, but rather for evaluation of metabolic tumor viability47.
In fact, the application of 18F-FDG PET was recently demonstrated to select suitable liver transplant patients with HCC beyond MC and UCSF criteria48,49,50,51. Although MVI plays an essential role for the prognostic reliability of the UTS criteria17,29,30,31, the are no comparable investigations in this context.
Our study impressively confirmed that enhanced 18F-FDG uptake on pretransplant PET is a valuable indicator of biological tumor aggressiveness and poor outcome (Table 6). Positive PET-status was even identified as most powerful independent clinical predictor of HCC recurrence in our series (Table 2). Apart from that, we were able to demonstrate that combining the clinical UTS criteria with FDG-PET leads to an extremely low tumor relapse risk (Fig. 5). Only 3 of 59 non- 18F-FDG-avid (5.1%), but 13 of 26 PET-positive (50%) patients meeting the UTS criteria developed tumor recurrence (p < 0.001).
However, by strictly adhering to this selection concept, more than 30% of our UTS In patients would have been excluded from LT, with almost half of them still being tumor-free alive after 5 years (Fig. 5). The number of liver transplants had thereby been reduced from originally 66 meeting standard criteria (Milan In) to 59 fulfilling the novel hybrid criteria set (UTS In + PET-negative). Rather, our data pointed out that the MC are excellent for selecting suitable liver transplant patients (Figs 1 and 2), whereas further biological tumor evaluation is necessary beyond the Milan boundaries (Table 5).
As shown in Fig. 8, 18F-FDG PET identifies those Milan Out/UTS In tumors that have an aggressive biological potential. Probably due to the small sample size (n = 19), the survival difference between PET-positive and PET-negative patients was just not significant (Fig. 8). However, non-18F-FDG-avid Milan Out/UTS In patients were able to achieve a 5-year RFS rate of 80%, which was comparable to Milan In patients (86.2%, Fig. 9). This needs to be validated in a larger study cohort.
Noteworthy, we did not find significant outcome differences between Milan Out/UTS In and beyond UTS patients, although tumor load was significantly higher in the UTS Out cohort. One explanation might be that both subgroups did not differ regarding aggressive histopathologic variables (Table 5). According to this finding, the prognostic significance of tumor load may reach a plateau beyond the UTS limit. In fact, none of macromorphometric features but only positive PET-status was identified as an independent clinical promoter of HCC relapse in beyond UTS patients (Table 4).
Furthermore, outcome was not significantly different between patients meeting the UTS criteria and PET-negative patients exceeding them (Fig. 7). This interesting result indicates that biological tumor activity is the major prognostic determinant in advanced HCC stages. D’Amico et al. recently identified poor grading and MVI as the only independent predictors of tumor relapse in a series of 124 liver recipients with HCC beyond the UTS criteria, which supports this assumption on a histopathologic basis31. If being confirmed in large prospective trials, our data support the implementation of a purely tumor-biology based selection approach, as was already favored by others52.
There are several limitations of our study. First, it was a retrospective investigation with all the possible disadvantages of this study design. Second, the number of HCC patients beyond MC but still meeting the UTS criteria was rather low. Another critical point is that we have stratified our data according to semiquantitative and not quantitative PET results, which did not allow for further risk stratification in the 18F-FDG-avid subset. In contrast, our study was powered by a large PET data collection and a well-documented long-term follow-up. Apart from that, only preoperatively available tumor characteristics were used for risk analysis.
In conclusion, our study demonstrated that expansion to the clinical UTS criteria carries a considerable risk of selecting tumors with aggressive potential. The implementation of 18F-FDG PET improves the prognostic power of the UTS criteria, since it identifies patients with beneficial tumor biology. Expansion to the UTS criteria may, thereby, be safely realized.
References
Schütte, K. et al. Prevention of Hepatocellular Carcinoma. Gastrointest Tumors. 3, 37–43 (2016).
Bosetti, C. et al. Hepatocellular carcinoma epidemiology. Best Pract Res Clin Gastroenterol. 28, 753–770 (2014).
Pang, T. C. et al. Surgical management of hepatocellular carcinoma. World J Hepatol. 7, 245–252 (2015).
Fonseca, A. L. et al. Hepatocellular carcinoma: a comprehensive overview of surgical therapy. J Surg Oncol. 110, 712–719 (2014).
Sawada, T. et al. Liver transplantation for hepatocellular carcinoma. Dig Surg. 24, 126–130 (2007).
Sapisochin, G. et al. Liver transplantation for hepatocellular carcinoma: outcome and novel surgical approaches. Nat Rev Gastroenterol Hepatol. 14, 203–2017 (2017).
Ringe, B. et al. Surgical treatment of hepatocellular carcinoma: experience with liver resection and transplantation in 198 patients. World J Surg. 15, 270–285 (1991).
Iwatsuki, S. et al. Hepatic resection versus transplantation for hepatocellular carcinoma. Ann Surg. 214, 221–228 (1991).
Mazzaferro, V. et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. NEJM 334, 693–699 (1996).
Mazzaferro, V. et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl. 17(Suppl. 2), 44–57 (2011).
X. U, D. W. et al. Liver transplantation for hepatocellular carcinoma beyond the Milan criteria: A review. World J Gastroenterol. 28, 3325–3334 (2016).
Parikh, N. D. et al. Controversies in criteria for liver transplantation in hepatocellular carcinoma. Curr Opin Gastroenterol. 32, 182–188 (2016).
Yao, F. J. et al. Liver transplantation for hepatocellular carcinoma: validation of the UCSF-expanded criteria based on preoperative imaging. Am J Transplant. 7, 2587–2596 (2007).
Sapisochin, G. et al. The extended Toronto criteria for liver transplantation in patients with hepatocellular carcinoma: A prospective validation study. Hepatology. 64, 2077–2088 (2016).
Silva, M. et al. Expanded criteria for liver transplantation in patients with cirrhosis and hepatocellular carcinoma. Liver Transpl. 14, 1449–1460 (2008).
Zheng, S. S. et al. Liver transplantation for hepatocellular carcinoma: Hangzhou experiences. Transplantation. 85, 1726–1732 (2008).
Mazzaferro, V. et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 10, 35–43 (2009).
Sotiropoulos, G. C. et al. Liver transplantation for hepatocellular carcinoma in cirrhosis: is clinical classification before transplantation realistic? Transplantation. 79, 483–487 (2005).
Jonas, S. et al. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology. 33, 1080–1086 (2001).
Cillo, U. et al. Prediction of hepatocellular carcinoma biological behavior in patient selection for liver transplantation. World J Gastroenterol. 22, 232–252 (2016).
Pawlik, T. M. et al. Preoperative assessment of hepatocellular carcinoma tumor grade using needle biopsy: implications for transplant eligibility. Ann Surg. 245, 435–442 (2007).
Yang, S. H. et al. The role of (18)F-FDG-PET imaging for the selection of liver transplantation candidates among hepatocellular carcinoma patients. Liver Transpl. 12, 1655–1660 (2006).
Kornberg, A. et al. 18F-FDG-uptake of hepatocellular carcinoma on PET predicts microvascular tumor invasion in liver transplant patients. American J Transplant. 9, 592–600 (2009).
Lee, J. W. et al. Prediction of tumor recurrence by 18F-FDG PET in liver transplantation for hepatocellular carcinoma. J Nucl Med. 50, 682–687 (2009).
Lin, C. Y. et al. Predictive value of 18F-FDG PET/CT for vascular invasion in patients with hepatocellular carcinoma before liver transplantation. Clin Nuc Med. 42, 183–187 (2017).
Bailly, M. et al. 18F-FDG PET in liver transplantation setting of hepatocellular carcinoma: predicting histology? Clin Nucl Med. 41, 126–129 (2016).
Volk, M. L. et al. A novel model measuring the harm of transplanting hepatocellular carcinoma exceeding Milan criteria. Am J Transplant. 8, 839–846 (2008).
Settmacher, U. et al. Liver transplantation – current aspects of allocation, indication and donor pool expansion. Zentralbl Chir. 138, 604–610 (2013).
Gugenheim, J. et al. Recurrence after liver transplantation for hepatocellular carcinoma according to up-to-seven criteria. Hepatogastroenterology. 60, 799–806 (2013).
Lei, Y. et al. Up-to-seven criteria for hepatocellular carcinoma liver transplantation: a single center analysis. World J Gastroenterol. 19, 6077–6083 (2013).
D’Amico, F. et al. Predicting recurrence after liver transplantation in patients with hepatocellular carcinoma exceeding the up-to-seven criteria. Liver Transpl. 15, 1278–1287 (2009).
Freemann, R. B. et al. Optimizing staging for hepatocellular before liver transplantation: A retrospective analysisof the UNOS/OPTN database. Liver Transpl. 12, 1504–1511 (2006).
Zhao, W. C. et al. Preoperative predictors of microvascular invasion in multinodular hepatocellular carcinoma. Eur J Surg Oncol. 39, 858–864 (2013).
Grat, M. et al. Limitations of predicting microvascular invasion in patients with hepatocellular cancer prior to liver transplantation. Sci Rep. 7, 39881, https://doi.org/10.1038/srep39881. (2017).
Llovet, J. M. et al. Increased risk of tumor seeding after percutaneous radiofrequency ablation for single hepatocellular carcinoma. Hepatology 33, 1124–1129 (2001).
Cho, C. T. et al. Prediction of microvascular invasion of hepatocellular carcinoma: preoperative CT and histopathologic correlation. Am J Roengenol. 203, 253–259 (2014).
Pawlik, T. M. et al. Tumor size predicts vascular invasion and histologic grade: Implications for selection of surgical treatment for hepatocellular carcinoma. Liver Transpl. 11, 1086–1092 (2005).
Otto, G. et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 12, 1260–1267 (2006).
Lai, Q. et al. Alpha-fetoprotein and modified response evaluation criteria in solid tumors progression after locoregional therapy as predictors of hepatocellular cancer recurrence and death after transplantation, European Hepatocellular Cancer Liver Transplant Study Group. Liver Transpl. 19, 1108–1118 (2013).
An, H. J. et al. Serum C-reactive protein is a useful biomarker for predicting outcomes after liver transplantation in patients with hepatocellular carcinoma. Liver Transpl. 18, 1406–1414 (2012).
Kamiyama, T. et al. Multiplication of alpha-fetoprotein and protein induced by vitamin K absence-II is a powerful predictor of prognosis and recurrence in hepatocellular carcinoma patients after a hepatectomy. Hepatol Res. 45, 21–31 (2015).
Fu, S. J. et al. Elevated Preoperative Serum Gamma-glutamyltranspeptidase Predicts Poor Prognosis for Hepatocellular Carcinoma after Liver Transplantation. Sci Rep. 6, 28835, https://doi.org/10.1038/srep28835 (2016).
Kornberg, A. et al. 18F-FDG-uptake of hepatocellular carcinoma on PET predicts microvascular tumor invasion in liver transplant patients. Am J Transplant. 9, 592–600 (2009).
Kornberg, A. et al. Increased 18F-FDG uptake of hepatocellular carcinoma on positron emission tomography independently predicts tumor recurrence in liver transplant patients. Transplant Proc. 41, 2561–2563 (2009).
Lin, C. Y. et al. Predictive value of 18F-FDG PET/CT for vascular invasion in patients with hepatocellular carcinoma before liver transplantation. Clin Nucl Med. 42, 183–187 (2017).
Gallamini, A. et al. Positron Emission Tomography (PET) in Oncology. Cancers (Basel) 6, 1821–1889 (2014).
Iwata, Y. et al. Clinical usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose in the diagnosis of liver tumors. Ann Nucl Med. 14, 121–126 (2000).
Kornberg, A. et al. Patients with non-[18 F]fludeoxyglucose-avid advanced hepatocellular carcinoma on clinical staging may achieve long-term recurrence-free survival after liver transplantation. Liver Transpl. 18, 53–61 (2012).
Hsu, C. C. et al. Combination of FDG-PET and UCSF Criteria for Predicting HCC Recurrence After Living Donor Liver Transplantation. Transplantation 100, 1925–1932 (2016).
Takada, Y. et al. Significance of preoperative fluorodeoxyglucose-positron emission tomography in prediction of tumor recurrence after liver transplantation for hepatocellular carcinoma patients: a Japanese multicenter study. J. Hepatobiliary Pancreat Sci. 24, 49–57 (2017).
Detry, O. et al. Prognostic value of (18)F-FDG PET/CT in liver transplantation for hepatocarcinoma. World J Gastroenterol. 21, 3049–3054 (2015).
Hong, G. et al. Alpha-fetoprotein and (18)F-FDG positron emission tomography predict tumor recurrence better than Milan criteria in living donor liver transplantation. J Hepatol. 64, 852–859 (2016).
Author information
Authors and Affiliations
Contributions
A.K. conceived the study. A.K., U.W., K.M., M.S. and K.T. collected data. A.K. and J.K. analyzed data A.K. wrote the manuscript. H.F. and G.C. critically reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kornberg, A., Witt, U., Schernhammer, M. et al. Combining 18F-FDG positron emission tomography with Up-to-seven criteria for selecting suitable liver transplant patients with advanced hepatocellular carcinoma. Sci Rep 7, 14176 (2017). https://doi.org/10.1038/s41598-017-14430-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-14430-9
This article is cited by
-
Impact of metabolic indices of 18F-fluorodeoxyglucose positron emission tomography/computed tomography on post transplantation recurrence of hepatocellular carcinoma
Journal of Cancer Research and Clinical Oncology (2023)
-
Composite criteria using clinical and FDG PET/CT factors for predicting recurrence of hepatocellular carcinoma after living donor liver transplantation
European Radiology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.