Abstract
Few studies have examined the association between ambient temperature and years of life lost (YLL). We aim to explore the burden of cardiovascular disease attributed to non-optimum temperature in China. YLL provides a complementary measure for examining the burden of disease due to ambient temperature. Non-optimal temperature leads to the increase of YLL. The mortality of fourteen cities in China during 2008–2013 was included in this study. We used the Distributed Lag Non-linear Model (DLNM) to estimate the association between daily mean temperature and YLL, controlling for long term trends, day of the week, seasonality and relative humidity. The daily YLL varied from 807 in Changchun to 2751 in Chengdu, with males higher than females. Extreme high and low temperatures were associated with higher YLL. The attributable fraction (AF) to cold effect is from 2.67 (95%CI: −1.63, 6.70) to 8.55 (95%CI: 5.05, 11.90), while the AF to heat effect is from 0.16 (95%CI: 0.06, 0.26) to 2.29 (95%CI: 1.29, 3.19). Cold effect was significantly higher than heat effect on cardiovascular disease in both men and women and for different age groups.
Similar content being viewed by others
Introduction
As the frequency of extreme temperature increases, numerous researchers have investigated the effects of high or low temperature on mortality1,2,3,4, especially in cardiovascular diseases5,6. The temperature-mortality relationship was usually depicted as U, J or V-shaped with delay effect7,8. The curve of the association between temperature and mortality shows that there exists the minimum mortality temperature, higher or lower than the optimum temperature could increase the excess deaths. Lag days of high temperature were one or two days, but the effects of low temperature lasted several days or even weeks3,7.
Although most of the previous studies have examined the association between extreme temperature and mortality and assessed whether there was evidence of excess mortality during extreme weather, few of them focused on the burden of disease associated with temperature9,10. Mortality only considered the number of deaths, and failed to take the death age into account. However, the short-term mortality displacement could heavily affect the relative risks of temperature on mortality. It would be more rational to assess the effect of ambient temperature exposure using the estimates of years of life lost (YLL), which takes into account the life expectancy11.
YLL, as an important part of Disability Adjusted Life Years (DALY), is a measure of disease burden that uses the life expectancy12. Compared with the traditional measure of mortality, YLL gives more weight to deaths among younger people. We should pay more attention to the effects of extreme temperature on young people who have a longer life expectancy than the elderly. At present, YLL is regarded as a more precise indicator to evaluate the burden of disease12 and some new studies10,13 have used YLL as outcome to evaluate the effect of ambient temperature around the world.
Cardiovascular disease is a major chronic non-communicable disease, accounting for about 40% of total deaths in China. About 3.7 million people died of cardiovascular disease each year, resulting in a serious increase on the burden of disease14. The change of ambient temperature was associated with human blood vessels’ contraction and may cause fluctuation of blood pressure. Literature has shown the rapid changes of blood pressure are likely to cause cardiovascular disease15. The evidence of the association between ambient temperature and the burden of cardiovascular disease is scarce in China. We collected data from Chinese national mortality surveillance system and investigated the association between extreme temperature and YLL in fourteen major Chinese cities during 2008–2013.
Results
Table 1 shows summary statistics of daily YLL and weather for the fourteen Chinese provincial capital cities during the study period. The daily number of deaths was highest in Beijing (214) and lowest in Changchun (52). Descriptive statistics on population in fourteen Chinese cities by gender and age are showed (Supplementary Table S1). The Daily YLL was highest in Chengdu (2751) and lowest in Changchun (807). The mean temperatures varied significantly in different cities, ranging from 5.1 °C in Harbin to 21.6 °C in Guangzhou.
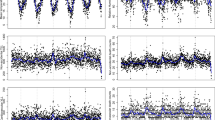
Figure 1 shows the city-specific distribution of YLL by gender. YLL of cardiovascular disease was significantly higher in males than in females in all the fourteen cities, especially in Harbin and Chengdu.
Figure 2 shows the city-specific distribution of YLL by age. YLL due to cardiovascular disease among those under the age of 65 years was higher than that in people aged greater than 65 years. The difference was two folds or more in cities like Harbin and Chengdu.
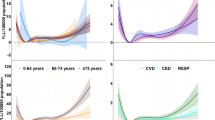
As showed in Fig. 3, YLL decreased first and then increased with the increase in mean temperature. Extreme high and low temperatures were associated with higher YLL. These dots concentrated between 20 and 30 degrees, in other words, the optimum temperature was within this range. The effect of high temperature on mortality seems to be immediate but persists less than a week (Supplementary Table S2). However, the lag effect of low temperature is significant and can last two or three weeks. The overall cumulative effect of low temperature is significantly higher than high temperature (Supplementary Table S3).
Table 2 shows the estimated attributable fraction calculated as a separate component caused by low and high temperatures in each city. Overall, the total fraction of YLL varied significantly in different cities, with the highest attributable fraction in Changsha (10.42), and the lowest estimates in Hefei (3.52). The confidence intervals (CI) for Changchun, Hefei and Kunming were not significant. Cold effect was responsible for most of the burden of cardiovascular disease, while the fraction attributable to heat effect was small.
Table 3 shows the cumulative cold and heat effects in different cities by gender and age. Cold effect was significantly higher than heat effect for all subgroups. The total extreme temperature effect (heat effect and cold effect) was higher in males than in females in Beijing, Shanghai, Jinan, Hefei and Tianjin, whilst in the other 9 cities, the effect was higher in females than in males. The estimates of cold and hot-related YLL were higher in people age greater than 65 years, with the highest attributable fraction in Changsha, and the lowest estimates in Hefei.
Discussion
In this study, we found that the association between ambient temperature and YLL was U-shaped curve, with a significant increase of YLL associated with low temperatures. The effect of low temperature on cardiovascular disease was higher than high temperature, and there exists the minimum value between ambient temperature and YLL of cardiovascular disease.
Current studies16,17 mainly focused on the impact of temperature on mortality, always biased by the fact that the abnormal temperatures have a greater impact on older people18. We used YLL as the outcome variable in this study, which fully takes into account the death weight of different age. It can be used to not only evaluate the disease burden of the temperature, but also to respond to the impact of health risk factors on the population. In measuring the health outcomes of extreme weather events, YLL representing the burden of specific diseases can act as a more concise and synthetic indicator than mortality, and therefore can convey more useful and straightforward information to decision makers.
In this paper, the effect of ambient temperature on the YLL of cardiovascular disease was analyzed by DLNM19. The results showed that the risk of temperature on YLL was nonlinear, high or low temperature could increase YLL. Unlike some studies13,16,20, the curves presented in this study were U-shaped (Supplementary Figure S1), instead of V or J-shaped. The difference was likely due to the discrepancy in population base and geographical region. Previous studies21,22 have shown that the impact of air temperature on the daily mortality of the population lagged behind, the lag time of high temperature and low temperature was different. The specific performance of high temperature effect was short, and the low temperature effect lasted for a long time, the relative risk of low temperature is significantly higher than high temperature. It was found that the association between temperature and YLL followed the same pattern, with no lag effect for high temperature and 7 days lag for the effect of low temperature, suggesting the high temperature warning should be early and responses should be rapid, while the low temperature should be paid attention to its longer effect and taking a relatively lasting response measures to reduce the adverse effects of low temperature.
As a part of the disability adjusted life years, YLL can be used to compare the burden of disease. The study shows that the temperature above or below the optimum temperature will cause the increase in YLL. The burden of disease caused by low temperature was significantly higher than that of high temperature, which was attributed to our definition. We define that the temperature below the optimum temperature belongs to low temperature and above the optimum temperature belongs to high temperature. At present, most of the studies23,24,25,26 are more concerned with extreme weather (heat waves and cold spell), because this kind of research can offer more intuitive understandings of the acute temperature influence on mortality, and to provide the basis for the formulation of policy, such as the definition of heat wave or cold spell and the high temperature allowance. Since there was only about one-fifth of AF caused by the extreme low and high temperature27, we should not only pay attention to the impact of extreme weather, but also the influence of non-optimum temperature.
The significantly higher YLL of cardiovascular disease in men found in the current study might be due to the poorer diet and lifestyle habits, more mental stress and other aspects of exposure in men compared with women28. There is no regular change in gender, which was inconsistent with the results of a study of the number of deaths29. Women’s life expectancy is higher than that of men, especially in the elderly. Therefore, the impact of temperature on women may be overestimated in the previous studies. With the age stratified analysis, it was found that the temperature impact on the people aged <65 years was lower than the people aged ≥65 years, namely, the elderly were more vulnerable populations of extreme temperatures, which were consistent with previous studies30,31. The main reason might be that the elderly people’s temperature regulation ability and the ability to adapt to the temperature become weak, and the elderly tend to have one or more common diseases at the same time.
Low temperature increased blood pressure and heart rate and exposure to low temperature in patients with cardiovascular disease may cause coronary spasms, chest pains, and even myocardial infarction. By contrast, exposure to high temperature leads to an increase in deprivation of body fluids and hypotension, and then increases the burden of heart. Cardiovascular disease has become the highest mortality chronic diseases, the burden of disease it caused has been gradually being acknowledged and emphasized. Environmental factors, especially ambient temperature and air pollution32, together with the lifestyle, exercise, diet and other risk factors33,34, play a vital role in the incidence and mortality of cardiovascular disease.
To our knowledge, this is the first study in China investigating the association between ambient temperature and the burden of cardiovascular disease measured by YLL. We utilized mortality surveillance data with proved good quality in a relatively large time span (2008~2013). We examined the association in fourteen major Chinese capital cities across different regions of China with significant temperature variations. Furthermore, we utilized YLL as an indicator of the burden of disease and explored the association between temperature and YLL.
We also have limitations. Firstly, the model does not control the effects of air pollution as confounding factors due to the lack of accurate matching of air pollution data for each day, such as PM2.5, NO2 or O3. We will investigate how to integrate air pollution measurements in subsequent versions of our model. The interaction between air pollution and temperature35, might have an impact on the results. Further studies should be undertaken ruling out the noise of air pollution. Secondly, we used the national life expectancy table rather than the city-specific life tables to calculate YLL because of the data availability. Although it may cause inaccuracy of YLL estimates, we believe it’s not likely to significantly change the results because the included capital cities have similar economic and development levels.
Conclusion
In summary, this study provides evidence that exposure to non-optimum ambient temperature increases the burden of cardiovascular disease in China. Low temperature has a more harmful influence than high temperature, and low and high temperatures-associated YLL were higher in the elderly. In order to reduce temperature-related YLL, the government should take measures to protect vulnerable people, especially patients with chronic diseases.
Material and Methods
Data sources
We collected daily cardiovascular mortality data of 14 Chinese cities (Fig. 4) during 2008–2013. The population of the cities ranged from 5.7 million in Hefei to 23 million in Shanghai (median 10 million in Shijiazhuang and 8.1 million in Shenyang). The mortality data of Guangzhou, Hefei, Shenyang and Shijiazhuang were from 2012 to 2013, Changchun’s mortality data were from 2008 to 2011, Shanghai’s data were from 2008 to 2012, Jinan’s data were from 2011 to 2013, and the other cities (Beijing, Changsha, Chengdu, Harbin, Kunming, Nanjing, Tianjin) were from 2008 to 2013. The code of underlying cause of death based on the 10th International Classification of Diseases (ICD-10) was used for deaths due to cardiovascular diseases(I00-I99). All data were classified by gender and age. The data were obtained from the China National Mortality Surveillance system36, which was administered by the Chinese Center for Disease Control and Prevention (China CDC). Detailed descriptions of the surveillance system and reporting procedures were published elsewhere37. In brief, all deaths occurred in the surveillance sites are required to be reported to the system. The underlying cause of death is coded by doctors and trained coders for death occurred in hospitals, while verbal autopsy is performed for deaths outside hospitals by village health workers or doctors at local hospitals38. Stringent quality control measurements are in place, including annual quality control meetings, staff training courses, development of regulations for death registration and regular site quality inspection.
The meteorological data for the same period were collected from the China Meteorological Data Sharing Service System (http://data.cma.cn/), which included daily mean temperature, minimum temperature, maximum temperature and relative humidity.
Measurements of YLL
We calculated the YLL for each death (YLLi) and each day (YLLt) by the following formulas13:
where A is the actual age at death for each individual, LEr is the remaining life expectancy at age A, ALB is the lower bound age from the life table. The national life table 2013 was obtained from the World Health Organization (WHO) (Supplementary Table S4). YLL was calculated by matching gender and age to the life table for each death. We calculated daily YLL by summing the YLL for all deaths on the same day. The sums were stratified by gender and age group (<65 and 65 + years).
Statistical analysis
We applied the Distributed Lag Non-linear Model (DLNM) to estimate the impact of heat and cold temperature on YLL with the following formula:
where t is the day of observation; YLLt is the summing YLL at day t; α refers to the intercept; NS represents natural cubic spline; NS(Time) was used to control long-term trend and seasonality and the degrees of freedom (df) chooses 7, T is the time span; NS(Humidity) was used to control the confounding effects of humidity and the df is 3; Dow is day of the week and and Holiday is public holidays, both of them represented as categorical variables. Tempt refers to a two-dimensional natural spline for daily mean temperature with a lagged 14 days, considering the effect of low temperature on death and harvesting effect20,39. γ, η and β are coefficients for DOW, Holiday and Tempt. We modelled the exposure-response relationship with three internal knots placed at the 10th, 75th, and 90th percentiles of city-specific temperature distributions.
We used minimum mortality temperature (MMT) as the optimum temperature39,40. MMT was rooted in the best linear unbiased prediction of the overall cumulative exposure-response association in each city, which stands for a minimum mortality percentile between the 1st and the 99th percentiles. Exposure-response model needs MMT as the reference for calculating the attributable risk by re-centring the quadratic B-spline. We used the overall cumulative relative risk (RR) corresponding to each day’s temperature to calculate the attributable fraction (AF)27 of attributable YLL in the next 14 days for each day and each city. Confidence intervals (CIs) were calculated to assume a multivariate normal distribution of the best linear unbiased predictions of the reduced coefficients.
The heat and cold temperatures were defined as temperatures higher than the MMT and lower than the MMT, and then the attributable fraction to cold and heat effects on YLL due to cardiovascular was calculated.
Sensitivity analyses were conducted by changing df (6 and 10 per year) for time to control for season, df (4 and 6) for humidity and and the maximum lag days (7 days and 21 days) for daily mean temperature (Supplementary Table S5). All models were analyzed in R version 3.3.1.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Armstrong, B. G. et al. Association of mortality with high temperatures in a temperate climate: England and Wales. J Epidemiol Community Health 65, 340–345 (2011).
Baccini, M. et al. Impact of heat on mortality in 15 European cities: attributable deaths under different weather scenarios. J Epidemiol Community Health 65, 64–70 (2008).
Anderson, B. G. & Bell, M. L. Weather-related mortality: how heat, cold, andheat waves affect mortality in the United States. Epidemiology 20, 205–213 (2009).
Wang, C. et al. Temperature and daily mortality in Suzhou, China: a time series analysis. Sci Total Environ 466–467, 985–990 (2014).
Guo, Y. et al. Extremely cold and hot temperatures increase the risk of ischaemic heart disease mortality: epidemiological evidence from China. Heart 99, 195–203 (2013).
Braga, A. L., Zanobetti, A. & Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 US cities. Environ Health Perspect 110, 859–863 (2002).
Bao, J., Wang, Z., Yu, C. & Li, X. The influence of temperature on mortality and its Lag effect: a study in four Chinese cities with different latitudes. BMC Public Health 16, 375 (2016).
Fouillet, A. et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int. J. Epidemiol 37, 309–317 (2008).
Huang, C. et al. Effects of extreme temperatures on years of life lost for cardiovascular deaths: a time series study in Brisbane, Australia. Circ Cardiovasc Qual Outcomes 5, 609–614 (2012).
Yang, J. et al. 2015. The burden of ambient temperature on years of life lost in Guangzhou, China. Sci Rep 5, 12250 (2015).
Hajat, S., Armstrong, B. G., Gouveia, N. & Wilkinson, P. Mortality displacement of heat-related deaths: A comparison of Delhi, São Paulo, and London. Epidemiology 16, 613–620 (2005).
Donev D, et al. Measuring the Burden of Disease: Disability Adjusted Life Year (DALY). Available at: www.mf.uni-lj.Si/dokumenti/ (2014).
Egondi, T., Kyobutungi, C. & Rocklöv, J. Temperature Variation and Heat Wave and Cold Spell Impacts on Years of Life Lost Among the Urban Poor Population of Nairobi, Kenya. Int. J. Environ. Res. Public Health 12, 2735–2748 (2015).
Chen, W. China Cardiovascular disease report 2015. China Medical News 12, 11 (2016).
Muntner, P. et al. Visit-to-Visit Variability of Blood Pressure and Coronary Heart Disease, Stroke, Heart Failure, and Mortality: A Cohort Study. Ann Intern Med 163, 329–338 (2015).
Guo, Y. et al. The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect 119, 1719–1725 (2011).
Yang, J. et al. Cardiovascular mortality risk attributable to ambient temperature in China. Heart 101, 1966–1972 (2015).
Yu, W. et al. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci Total Environ 408, 3513–3518 (2010).
Gasparrini, A., Armstrong, B. & Kenward, M. G. Distributed lag non-linear models. Stat Med 29, 2224–2234 (2010).
Group, T. E. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet 349, 1341–1346 (1997).
Braga, A. L., Zanobetti, A. & Schwartz, J. The time course of weather-related deaths. Epidemiology 12, 662–667 (2001).
Carder, M. et al. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup Environ Med 62, 702–710 (2005).
Barnett, A. G., Hajat, S., Gasparrini, A. & Rocklöv, J. Cold andheat waves in the United States. Environ Res 112, 218–224 (2011).
Carmona, R. et al. Mortality attributable to extreme temperatures in Spain: A comparative analysis by city. Environ Int 91, 22–28 (2016).
Montero, J. C. et al. Mortality from cold waves in Castile–La Mancha. Sci Total Environ 408, 5768–5774 (2010).
Huynen, M. M. et al. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect 109, 463–470 (2001).
Gasparrini, A. & Leone, M. Attributable risk from distributed lag models. BMC Med Res Methodol 14, 55–65 (2014).
Huang, C. et al. The impact of temperature on years of life lost in Brisbane, Australia. Nature. Clim Change 2, 265–270 (2012).
Almeida, S. P., Casimiro, E. & Calheiros, J. Effects of apparent temperature on daily mortality in Lisbon and Oporto, Portugal. Environ Health 9, 12–20 (2010).
Donaldson, G. C., Keatinge, W. R. & Saunders, R. D. Cardiovascular responses to heat stress and their adverse consequences in healthy and vulnerable human populations. Int J Hyperth 19, 225–235 (2003).
Chung, J. Y. et al. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci Total Environ 408, 390–396 (2009).
Pope, C. A. et al. Relationships between fine particulate air pollution, cardiometabolic disorders, and cardiovascular mortality. Circ Res 116, 108–115 (2015).
Li, Y. et al. Potential impact of time trend of life-style factors on cardiovascular disease burden in China. J Am Coll Cardiol 68, 818–833 (2016).
Maessen, M. F. et al. Lifelong exercise patterns and cardiovascular health. Mayo Clin Proc 91, 745–754 (2016).
Cheng, Y. & Kan, H. Effect of the interaction between outdoor air pollution and extreme temperature on daily mortality in Shanghai, China. J Epidemiol 22, 28–36 (2012).
Liu, S. et al. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ 94, 46–57 (2016).
Sun, Z. Cardiovascular responses to cold exposure. Front Biosci 2, 495–503 (2010).
Wang, L. et al. Evaluation of the quality of cause of death statistics in rural China using verbal autopsies. J Epidemiol Community Health 61, 519–526 (2007).
Daniel, O. A. et al. Evolution of Minimum Mortality Temperature in Stockholm, Sweden, 1901-2009. Environ Health Perspect 124, 740–745 (2016).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386, 369–375 (2015).
Author information
Authors and Affiliations
Contributions
Maigeng Zhou and Guijie Luan conceived and designed the experiments; Peng Yin and Lijun Wang collected the data; Guijie Luan analyzed the data and wrote the paper; Tiantian Li revised the methods and manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luan, G., Yin, P., Li, T. et al. The years of life lost on cardiovascular disease attributable to ambient temperature in China. Sci Rep 7, 13531 (2017). https://doi.org/10.1038/s41598-017-13225-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13225-2
This article is cited by
-
Short-term exposure to various ambient air pollutants and emergency department visits for cause-stable ischemic heart disease: a time-series study in Shanghai, China
Scientific Reports (2023)
-
Estimating the influence of high temperature on hand, foot, and mouth disease incidence in China
Environmental Science and Pollution Research (2023)
-
Summer heat waves and their mortality risk over a 14-year period in a western region of Iran
International Journal of Biometeorology (2023)
-
Temperature, cardiovascular mortality, and the role of hypertension and renin–angiotensin–aldosterone axis in seasonal adversity: a narrative review
Journal of Human Hypertension (2022)
-
Associations between air pollution exposure and birth defects: a time series analysis
Environmental Geochemistry and Health (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.