Abstract
Fifth metacarpal neck fracture commonly requires open reduction and internal fixation. Locking plate was widely adopted in the treatment of fifth metacarpal neck fracture as first-line choice for fixation. Patients with fifth metacarpal neck fracture receiving locking plate fixation were included for analysis. Features of internal fixation including number of distal and proximal locking screws, diameter of the screws and usage of lag screws were recorded. Clinical and radiographic outcomes included final volar angulation, grip strength, Michigan Hand Outcomes Questionnaire (MHQ) and range of motion (ROM) of fifth metacarpophalangeal joint. Three-screw fixation was less frequently presented in the group with increased volar angulation (≥30 degrees). Consistently, three-screw fixation of distal fragment could improve the prognosis compared with two-screw fixation (MHQ 95.4 ± 5.1 versus 80.4 ± 12.3, ROM 83.5 ± 7.2 versus 69.6 ± 7.7). In conclusion, the metacarpal head should be fixed by three locking screws instead of two locking screws.
Similar content being viewed by others
Introduction
The fifth metacarpal neck fracture accounts for approximately 20% of all fractures in hand1. A biomechanical study showed that final volar angulation more than 30 degrees could lead to decreased ROM of fifth metacarpophalangeal joint and functional impairment2. A range of surgical techniques have been described for the treatment of fifth metacarpal neck fracture: intramedullary K-wires3, transverse K-wires4, tension band5, locked intramedullary nailing6, external fixation7, and locking plate fixation8,9. A meta-analysis of six studies recommended locking plate as first-line choice of operative fixation10.
The secondary displacement in volar angulation was frequently observed after locking plate fixation, highlighting the need for improvement. We therefore showed that locking plate in combination with two crossed K-wires could decrease the secondary displacement in volar angulation compared with fixation with locking plate alone in previous study11. However, percutaneous K-wire fixation could also lead to an increase in surficial infection and irrigation of skin12. In addition, pin tract infection was also a major complication after K-wire fixation13. Thus, it is valuable to find how to improve the locking plate fixation without insertion of K-wires.
Features of internal fixation including number of distal and proximal locking screws, diameter of the screws and usage of lag screws is associated with the strength of fixation and therefore may affect the secondary displacement and prognosis14. However, to the best of our knowledge, there was no previous analysis of the association between these features of locking plate fixation and clinical outcomes. As a result, the fixation patterns were mainly based on the surgeons’ experiences and preferences. We hypothesized that specific fixation patterns might have a better outcomes compared with the rest ones. We therefore conducted an observational investigation on previous cases to find the better patterns for locking plate fixation.
Materials and Methods
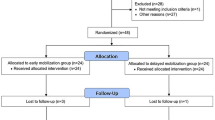
The study was approved by the Ethics Committee of Shanghai Jiaotong University Affiliated Sixth People’s Hospital. Informed consents were obtained from all participants and all methods in this study were in accordance with the Declaration of Helsinki. All patients with acute fifth metacarpal neck fractures (≤3 days) treated with open reduction and locking plate fixation from February 2014 to February 2016 were included for analysis. Patients with any of the following criteria were excluded initially: age below 20 or above 60, any injuries on tendons, ligaments, vessels and nerves on the upper limbs, fractures on the upper limbs in addition to fifth metacarpal neck, open fractures, immobilization after surgery. Fifty-nine patients were excluded from analysis due to incompletion of one-year follow-up.
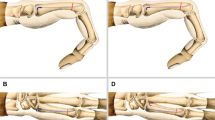
All patients were operated through a longitudinal dorsal approach facing the fifth metacarpal axis. T-shaped plates (three distal holes) or Y-shaped (two distal holes) plates were adopted based on the surgeon’s preferences to stabilize the fractures (Fig. 1). The plates in this study were provided by three manufacturers including Acumed (the U.S.), Guci (China) and Kangli (China). All surgeries in this study were conducted by 19 specialists of hand surgery with identical grade. There was no postoperative immobilization, and active mobilization was encouraged immediately after surgery. Patients were then regularly followed up. All patients received routine therapist-guided physical rehabilitation during the initial three months after surgery.
Demographic parameters including age and gender were recorded for each group. Clinical assessments were conducted at 1 year after treatment. Clinical assessments included grip strength, Michigan Hand Outcomes Questionnaire (MHQ)15, range of motion (ROM) of fifth metacarpophalangeal joint. Grip strength was measured with the elbow flexed at 90 degree and the forearm in neutral rotation. Values are expressed as percentages of the values of the contralateral hand. The MHQ is a 37-item questionnaire, which is divided into the same distinct 6 subscales: overall hand function, activities of daily living, pain (reversed), work performance, aesthetics, and patient satisfaction. The MHQ total score is obtained by averaging the scores for all 6 subscales. The total score ranges from 0 to 100 with a higher score indicating better hand performance. The ROM of fifth metacarpophalangeal joint was also recorded using a finger goniometer. The volar angulation and axial shortening was measured by the plain radiograph based on methods introduced and advocated in previous reports16,17. For the measurement of volar angulation, the distal line was drawn from the mid-medullary point in the distal fragment to the most distal point of the metacarpal head, and the proximal line centrally through the shaft medullary canal, irrespective of where the line hit the basis of the metacarpal. Radiographic parameters were measured immediately and one year after surgery. Radiographic assessments were performed by two authors. Inter-observer correlation coefficients for volar angulation was 0.82. The values of volar angulation were averaged values from two observers. We randomly chose 50 patients from February 2014 to February 2016 with hand injury but no metacarpal fracture. The radiographs of these 50 patients were all taken for medical purposes.
Statistical analysis was performed using SPSS 22.0 software. A P value of <0.05 was considered to be statistically significant. Data were presented as mean ± standard deviation. Student’s t test and chi-square test were used to compare numeric and nonnumeric variables respectively.
Results
Total 234 patients were included for analysis in our study. All of the treating surgeons were specialists of hand surgery. In our series, 177 of 234 cases were male. The average age of this series was 35.9 ± 8.3 (20 to 59). The right hand was affected in 132, the left hand in 102 cases. Statistically, there was no significant difference of demographics between two groups. The average volar angulation immediate after surgery were 8.2 ± 3.1 degrees and increased to 25.8 ± 8.6 degrees one year after surgery. There was no tendon rupture, deep infection and neurological complications in all patients of this study. Superficial infection, tenosynovitis and malunion were the major complications observed in this study.
Since the volar angulation is highly relevant to the prognosis, we first divided patients into two groups based on the volar angulation one year after surgery. We then compared the volar angulation immediately after surgery and found the values were similar between two groups (8.2 ± 2.9 versus 8.1 ± 3.5, P = 0.79). We also measured the volar angulation in 50 patients without fifth metacarpal fractures. The average volar angulation in these patients was 7.8 ± 3.2 similar to the immediate value after surgery. We compared the features of internal fixation between two groups and found the number of distal locking screws were associated with the final angulation (Table 1). Three-screw fixation in distal fragment was less frequently presented in cases with increased final angulation. We also compared the clinical outcomes in patients with two or three distal locking screws (Table 2). The MHQ score and ROM in three-screw group were higher than that of two-screw group. The differences in rates of complications were insignificant.
Discussion
A previous meta-analysis based on six studies recommended locking plate as the first-line choice of operative fixation10. However, secondary displacement in volar angulation which limits the recovery of hand functions could be frequently observed after locking plate fixation, highlighting the need for the improvement of the locking plate fixation. In previous study, we showed that locking plate in combination with two crossed K-wires could decrease the secondary displacement in volar angulation compared with fixation with locking plate alone11. However, infection is the major challenge for percutaneous K-wire fixation. In this study, we focused on finding how to improve the locking plate fixation without insertion of K-wires.
There was no previous study, to the best of our knowledge, analyzing the association between features of locking plate fixation and clinical outcomes. As a result, the fixation patterns were mainly based on the surgeons’ experiences and preferences. Hence, we conducted an observational analysis of plate fixation features in this study. Our results revealed that the fixation with three distal locking screws could reduce the secondary displacement and improve clinical outcomes. Hence, we recommended that the distal fragment should be fixed by three locking screws in fifth metacarpal neck fracture. To achieve the three-screw fixation of distal fragment, T-shaped plates (three distal holes) should be adopted instead of Y-shaped (two distal holes) plates. Our study revealed that three-screw fixation of distal fragment was better than two-screw fixation. In addition, the efficacy of locking plate in fifth metacarpal neck fracture should be reassessed since the number of distal locking screws were mainly based on the surgeons’ experiences and preferences previously.
Previous study has indeed reported extensor tendon rupture as a severe complication after plate fixation18. However, we did not encounter any patients with tendon rupture in our series. One possibility was that the advances in locking plates including improved biomaterials and anatomically pre-contoured designs have tremendously decrease the rate of this complication14. A soft-tissue flap to separate the tendon and plate might also be effective in preventing this complication.
There were several limitations of this study. First, given the observational nature of this study, the number of distal locking screws was decided based on the surgeon’s preference instead of randomly. Second, although the clinical outcomes were blinded when the radiographic assessment was done, the blinding of internal fixation features was impossible. Since all treating surgeons are specialists in hand surgery, personal experiences in clinical practices might cause potential bias on the measurement.
References
Hunter, J. M. & Cowen, N. J. Fifth metacarpal fractures in a compensation clinic population. A report on one hundred and thirty-three cases. J Bone Joint Surg Am 52, 1159–65 (1970).
Ali, A., Hamman, J. & Mass, D. P. The biomechanical effects of angulated boxer’s fractures. J Hand Surg Am 24, 835–44 (1999).
Heo, Y. M., Kim, S. B., Yi, J. W., Kim, T. G. & Lim, B. G. Radiologic Changes by Early Motion in Neck Fractures of the Fifth Metacarpal Treated with Antegrade Intramedullary Fixation. J Hand Surg Asian Pac Vol 21, 30–6 (2016).
Potenza, V., Caterini, R., De Maio, F., Bisicchia, S. & Farsetti, P. Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning. Injury 43, 242–5 (2012).
Wong, K. P., Hay, R. A. & Tay, S. C. Surgical outcomes of fifth metacarpal neck fractures–a comparative analysis of dorsal plating versus tension band wiring. Hand Surg 20, 99–105 (2015).
Orbay, J. L. & Touhami, A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin 22, 279–86 (2006).
Margic, K. External fixation of closed metacarpal and phalangeal fractures of digits. A prospective study of one hundred consecutive patients. J Hand Surg Br 31, 30–40 (2006).
Zemirline, A. et al. The MetaHUS((R)) fixation system versus pinning and plating in 5th metacarpal neck fractures. Chir Main 33, 207–10 (2014).
Facca, S., Ramdhian, R., Pelissier, A., Diaconu, M. & Liverneaux, P. Fifth metacarpal neck fracture fixation: Locking plate versus K-wire? Orthop Traumatol Surg Res 96, 506–12 (2010).
Zong, S. L. et al. Treatments for the Fifth Metacarpal Neck Fractures: A Network Meta-analysis of Randomized Controlled Trials. Medicine (Baltimore) 95, e3059 (2016).
Zhu, H., Xu, Z., Wei, H. & Zheng, X. Locking Plate Alone versus in Combination with Two Crossed Kirschner Wires for Fifth Metacarpal Neck Fracture. Sci Rep 7, 46109 (2017).
Greeven, A. P., Bezstarosti, S., Krijnen, P. & Schipper, I. B. Open reduction and internal fixation versus percutaneous transverse Kirschner wire fixation for single, closed second to fifth metacarpal shaft fractures: a systematic review. Eur J Trauma Emerg Surg 42, 169–75 (2016).
Lu, D., Wang, T., Chen, H. & Sun, L.J. Management of pin tract infection in pediatric supracondylar humerus fractures: a comparative study of three methods. Eur J Pediatr (2017).
Ruchelsman, D. E., Mudgal, C. S. & Jupiter, J. B. The role of locking technology in the hand. Hand Clin 26, 307–19 (2010). ; v.
Shauver, M. J. & Chung, K. C. The Michigan hand outcomes questionnaire after 15 years of field trial. Plast Reconstr Surg 131, 779e–87e (2013).
Braakman, M. Are lateral X-rays useful in the treatment of fractures of the fourth and fifth metacarpals? Injury 29, 1–3 (1998).
Sletten, I. N. et al. Assessment of volar angulation and shortening in 5th metacarpal neck fractures: an inter- and intra-observer validity and reliability study. J Hand Surg Eur Vol 38, 658–66 (2013).
Page, S. M. & Stern, P. J. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am 23, 827–32 (1998).
Acknowledgements
This study was supported by National Natural Science Foundation of China (81371965), Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant (20161429), Shanghai Pujiang Program (16PJD035).
Author information
Authors and Affiliations
Contributions
Xianyou Zheng was responsible for study design and manuscript writing. Hongyi Zhu was responsible for data collection and analysis. Bingbo Bao was responsible for clinical outcome measurement. Hongyi Zhu and Bingbo Bao contributed equally to this work.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, H., Bao, B. & Zheng, X. Three-screw versus two-screw fixation of distal fragment in fifth metacarpal neck fractures stabilized with locking plate. Sci Rep 7, 12516 (2017). https://doi.org/10.1038/s41598-017-12771-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12771-z
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.