Abstract
Overlapping idiopathic membranous nephropathy (IMN) and immunoglobulin A nephropathy (IgAN) is rare. This study aims to investigate the unique prognostic, clinical, and renal histopathological characteristics of IMN+IgAN. This retrospective observational study included 73 consecutive cases of IMN+IgAN and 425 cases of IMN treated between September 2006 and November 2015. Prognostic and baseline clinical and histopathological data were compared between the two patient groups. Poor prognostic events included a permanent 50% reduction in eGFR, end-stage renal disease, and all-cause mortality. Renal histopathology demonstrated that the patients with IMN+IgAN presented with significantly increased mesangial cell proliferation and matrix expansion, increased inflammatory cell infiltration, and higher proportions of arteriole hyalinosis and lesions than the patients with IMN (all P < 0.05). Kaplan–Meier analysis showed that the patients with IMN+IgAN had significantly higher cumulative incidence rates of partial or complete remission (PR or CR, P = 0.0085). Multivariate Cox model analysis revealed that old age at biopsy and high baseline serum creatinine and uric acid levels were significantly associated with poor prognosis (all P < 0.05), and increased IgA expression correlated significantly with PR or CR (P < 0.05). The present study found that overlapping IMN and IgAN presents with unique renal histopathology and appears not to cause a poorer prognosis than IMN.
Similar content being viewed by others
Introduction
Membranous nephropathy (MN), an autoimmune glomerular disease with a characteristic renal histopathology of immunoglobulin deposition along the extracapillary side of the glomerular basement membrane, is one of the most common causes for nephrotic syndrome in adults1,2,3,4,5,6. Approximately 75% of patients with MN have idiopathic or primary membranous nephropathy (IMN), and the remaining 25% of cases are associated with various secondary causes3, 6. The incidence of MN peaks in the fourth and fifth decades of life and appears higher in men than in women (men: women = 2-3:1)3,4,5. The exact etiology of MN remains unclear, and the disease course varies substantially. Approximately one-third of patients with MN experience spontaneous remission of proteinuria; another one-third develop persistent proteinuria; and the remaining one-third progress to end-stage renal disease (ESRD)7,8,9.
Immunoglobulin A nephropathy (IgAN), also known as Berger’s disease, is the most common primary glomerulonephritis, which is characterized by dominant or codominant IgA mesangial deposition10, 11. Although both IMN and IgAN are common primary glomerular diseases, coexisting MN and IgAN in adults is very rare12,13,14. Because of the low incidence, reports on overlapping MN and IgAN are limited to sparse case reports focusing on histopathological features12,13,14,15. In this study, we retrospectively reviewed 73 cases of overlapping IMN and IgAN and compared the renal histopathology of IMN only versus overlapping IMN and IgAN. In addition, we further examined the follow-up clinical data and compared the prognosis and outcomes of overlapping IMN and IgAN versus IMN only.
Materials and Methods
Ethics statement
The study was carried out in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of The First Affiliated Hospital of Wenzhou Medical University (Approval No: 2016151). All the study participants signed the informed consent form.
Patient selection
A total of 523 patients with IMN were identified from 4694 consecutive patients who underwent renal biopsies and were treated in the Department of Nephrology of The First Affiliated Hospital of Wenzhou Medical University between September 11, 2006 and November 25, 2015. The diagnosis of IMN followed the 2012 KDIGO Clinical Practice Guideline for Glomerulonephritis16 and was determined by a careful examination of kidney biopsies using light, immunofluorescence, and electron microscopy and an exclusion of secondary causes for MN. The pathology of the patients’ renal biopsies was characterized by (1) thickened glomerular capillary walls revealed by hematoxylin and eosin (H&E), periodic acid-Schiff (PAS), periodic acid silver methenamine (PASM), and Masson trichrome (Masson) staining; (2) positive IgG and C3 immunofluorescence staining along the capillary walls; and (3) subepithelial deposits and fusion in podocyte structure revealed by electron microscopy16. At the initial diagnosis, 523 patients with MN did not present with secondary causes for MN, such as malignancy, systemic lupus erythematosus, hepatitis B or C, diabetic glomerulosclerosis, adverse responses to medications, or renal damage from toxic agents. The authors had access to information that could identify individual participants during or after data collection. However, during follow-up examinations, 17 of the 523 patients were found to have a secondary cause for MN, including 9 cases of cancer and 8 cases of systemic lupus erythematosus. Thus, 506 patients with IMN were analyzed. The flow chart of patient selection is displayed in Fig. 1. Information on patients’ demographics (age and sex), body mass index (BMI, kg/m2), course of disease, and comorbidities such as diabetes, hypertension, infections, embolism, edema, nephrotic syndrome, and microscopic hematuria were collected.
Hematoxylin and eosin (H&E), periodic acid-Schiff (PAS), periodic acid silver methenamine (PASM), and Masson trichrome (Masson) staining
Formalin-fixed paraffin-embedded biopsy tissue specimens were sectioned into 3-μm-thick sections. The tissue sections were stained with H&E, PAS, PASM, and Masson according to the standard protocols. Based on these stains, the extent of mesangial cell proliferation and matrix expansion was graded as 0, 1, 2, and 3, representing negative, mild, moderate, or strong, respectively. In addition, the extent of inflammatory cell infiltration, interstitial fibrosis, tubular atrophy, and renal interstitial lesions were evaluated semi-quantitatively according to a scale 0 to 3, representing very small (scale 0: 0–4%), small (scale 1: 5–24%), medium (scale 2: 25–49%), and large affected area (scale 3: ≥50%). Two pathologists scored the stained sections, and the average score was used. Other histopathological characteristics, including segmental sclerosis, crescent, arteriole hyperplasia, arteriole hyalinosis, and arteriole lesions, were also evaluated.
Fluorescence immunohistochemical staining for immunoglobulins, complement components, and matrix proteins
The expression of IgG, IgA, IgM, C3, C4, C1q, and fibrinogen was determined by fluorescence immunohistochemical (IHC) staining. Frozen tissue sections (5 μm) were incubated with the following primary antibodies: anti-human IgG (1:50), IgA (1:50), IgM (1:50), C3 (1:50), C4 (1:50), C1q (1:90), and fibrinogen (1:90) at 4 °C overnight. All the antibodies were purchased from Gene Tech Company (Shanghai, China). The tissue sections were washed with PBS buffer and then incubated with FITC-labeled secondary antibodies (1:50, Gene Tech Company, Shanghai, China) at room temperature for 45 minutes. The stained slides were observed under an Olympus BX41 fluorescence microscope (Olympus, Center Valley, PA, USA). Images (200x magnification) were captured using the digital camera attached to the microscope. The intensity of the staining signals was scored as 0, 1, 2, 3, and 4, representing very weak, weak, moderate, strong, and very strong, respectively. IgA positive staining was defined as an intensity score ≥2. The staining intensity was scored by two pathologists, and the average score was used.
Laboratory test
Urine protein quantification was determined using a 24-hour collection. Nephrotic syndrome was defined as proteinuria ≥3.5 g/d and hypoalbuminemia <30 g/L. Subnephrotic status was defined as >0.5 g proteinuria and <3.5 g per day. Proteinuria was graded as stage 1, 2, 3, and 4 when proteinuria was <3.5 g/d, 3.5–8 g/d, 8–15 g/d, and 15 g/d, respectively. Proteinuria and microscopic hematuria were evaluated by urinary sediment examination. The severity of proteinuria and microscopic hematuria was graded 0–4 with 0 representing the mildest and 4 representing the most severe stage. The estimated glomerular filtration rate (eGFR) was calculated according to the abbreviated Modification of Diet in Renal Disease (MDRD) study formula and serum creatinine levels17.
Electron microscopy
Epon-embedded biopsy tissue specimens were cut into ultrathin sections. The sections were fixed in 2.5% glutaraldehyde and then in 1% osmium tetroxide. The tissue sections were stained with uranyl acetate and lead citrate and examined under a Hitachi H7500 electron microscope (Tokyo, Japan). The ultrastructural stage of MN was determined according to the Ehrenreich and Churg four-stage classification.
Outcome parameters
The following outcome and prognostic parameters were recorded and used for statistical analysis: development of end-stage renal disease (ESRD), all-cause mortality, a permanent 50% reduction in eGFR compared with the baseline value, complete remission (CR), and partial remission (PR). CR was defined as urinary protein excretion <0.3 g/d (uPCR <300 mg/g or <30 mg/mmol) accompanied by a normal serum albumin concentration and a normal serum creatinine. PR was defined as urinary protein excretion <3.5 g/d (uPCR <3500 mg/g or <350 mg/mmol), a ≥50% reduction from peak values, an improvement or normalization of the serum albumin concentration, and stable serum creatinine16, 18. ESRD was defined as a permanent drop in eGFR to <15 mL/min/1.73 m2 requiring dialysis or kidney transplantation.
Statistical analysis
Data are presented as the mean ± standard deviation (SD). Student’s t-test and the chi-square test were used for two-group comparisons of continuous variables and categorical variables, respectively. A poor event-free renal survival curve was prepared using the Kaplan-Meier method. Cumulative hazard curves were plotted for CR and PR. Poor event-free renal survival and incidence rates of CR or PR in different groups were compared using the log-rank test. Univariate and multivariate Cox regression analyses were performed to analyze the correlation between the clinical parameters and outcomes. For all variables, the proportional hazard assumption was tested and found to be fulfilled. The statistical analysis software Medcalc version 15.6 was used for the survival analysis, and SPSS version 23 was used for Cox regressions and all other statistical analyses. The P value was 2-sided, and P < 0.05 was considered statistically significant.
Results
A total of 506 patients with idiopathic MN identified from the consecutive renal biopsy cases from September 11, 2006 to November 25, 2015 at The First Affiliate Hospital of Wenzhou Medical University were included in this retrospective study. Most patients were treated with RAS receptor inhibitors: angiotensin-converting enzyme inhibitors (ACEis) or angiotensin receptor blockers (ARBs), glucocorticoids, cyclophosphamide, calcineurin inhibitors (CNIs) including tacrolimus and cyclosporine and other immunosuppressors. The usual doses of drugs were as follow: (1) RAS receptor inhibitors: double dosage given orally daily; (2) glucocorticoids plus cyclophosphamide: full oral dosage (1 mg/kg/d) of glucocorticoids per day and i.v. cyclophosphamide 1 g/month until reaching an accumulated dose of 6–8 g for 6 months; (3) CNI therapy (tacrolimus or cyclosporine): tacrolimus 0.05–0.075 mg/kg/d given orally in two divided doses 12 hours apart, without prednisone, for 6–12 months or cyclosporine 3.5–5.0 mg/kg/d given orally in two equally divided doses 12 hours apart, with prednisone 0.15 mg/kg/d, for 6 months.
Because of the use of glucocorticoids and immunosuppressors, 24 patients experienced infections during the follow-up period: 20 infections were respiratory tract infections, particularly pulmonary infections; 1 was a lower limb skin infection; 1 patient had both a respiratory and lower limb skin infection; 1 patient had tuberculotic hydrothorax; 1 patient had Hepatitis E virus infection; 1 patient was infected with neurosyphilis; and 2 patients died because of serious infections. Five patients had embolic events during the follow-up period including 4 cerebral infarctions and 1 mesenteric arterial embolism. One patient suffered a subarachnoid hemorrhage and 1 patient had an upper gastrointestinal hemorrhage secondary to a duodenal ulcer. Four patients had repetitive renal biopsies. One patient’s twin brother also had nephrotic syndrome. Two patients had renal biopsies done during pregnancy.
Patients with IgA+ nephropathy presented with higher mesangial cell proliferation and matrix expansion but lower segmental sclerosis than patients with IgA− nephropathy
Of the 506 patients with IMN, 8 were excluded because of missing fluorescent IHC data. There were 73 cases of IgA+ and 425 cases of IgA− in the remaining 498 patients. Overall, 18 patients in the IgA+ group and 138 patients in the IgA− group did not have a follow-up examination after 6 months. Thus, 55 cases of IgA+ and 287 cases of IgA− were included in the outcome and prognosis analyses. The patient selection flow chart is displayed in Fig. 1.
Demographics including gender distribution, age at disease onset, and BMI were similar in the IgA+ and IgA− groups (Table 1). The proportions of patients with comorbidities, such as edema, hypertension, diabetes, infection, embolism, nephrotic syndrome, and/or microscopic hematuria, were also similar in the two groups. Serum IgA levels were significantly higher in the IgA+ group than in the IgA− group (2.44 ± 0.95 g/L vs. 2.15 ± 0.89 g/L, P = 0.011, Table 1). All the other serum and urine test results were comparable in the two groups (Table 1).
Examination of the renal biopsies revealed that patients with IgA+ had significantly higher pathological stages compared with patients with IgA− (1.88 ± 0.73 vs. 1.65 ± 0.57, P = 0.003, Table 2). In particular, the IgA+ group had significantly increased mesangial cell proliferation, matrix expansion, and inflammatory cell infiltration than the IgA− group (All P < 0.05, Table 2). In contrast, the proportion of patients with segmental sclerosis was significantly lower in the IgA+ group than in the IgA− group (4.7% vs. 12.9%, P = 0.009, Table 2). In addition, significantly higher proportions of patients with IgA+ than patients with IgA− exhibited arteriole hyalinosis (41.1% vs. 25.4%, P = 0.006) and lesions (58.9% vs. 37.4%, P = 0.001, Table 2). Patients with IgA+ also appeared more likely to have arteriole hyperplasia than patients with IgA− (32.9% vs. 22.4%, P = 0.051, Table 2). Fluorescence IHC showed positive IgG for both groups and positive IgA for the IgA+ group. The staining intensity for IgM, C3, C4, C1q, and fibrinogen were weak, although the IgA+ group showed significantly stronger staining for IgM than the IgA− group (0.62 ± 0.90 vs. 0.32 ± 0.65, P = 0.008, Table 2).
Representative images of H&E, PAS, PASM, Masson, and fluorescence staining and representative images of electron microscopy for the IgA+ and IgA− groups are presented in Figs 2 and 3. Patients with IgA+ showed stiff capillary loops on H&E (Fig. 2a ) and PAS staining (Fig. 2b), spikes in the peripheral capillary wall on the PASM staining (Fig. 2c), and protein deposition (red colored area) on the peripheral capillary wall on the Masson staining (Fig. 2d). Electron microscopy showed global irregularities; capillary wall thickening; dense electron deposits in the sub-epithelium, intramembranous space, and mesangial areas; and epithelial foot process effacement (Figs. 2e and f). Patients at stages II-III had higher levels of mesangial cell proliferation and matrix expansion (Fig. 2), stronger staining for IgG (Fig. 2g), and more obvious epithelial foot process effacement (Fig. 2e and f) than patients at a lower pathological stage (stage I-II). Strong IgA staining was detected in patients in the IgA+ group at all pathological stages (Fig. 2). The staining signals of IgG appeared predominantly on the peripheral capillary walls, whereas the staining signals of IgA were mainly found in the mesangial area. The renal histopathology of patients with IgA− showed an absence of mesangial cell proliferation and matrix expansion (Fig. 3).
Representative images of the renal biopsy histopathology of patients with IgA+ at pathological stage II-III. (a) H&E staining (200x). (b) PAS staining (200x). (c) PASM staining (200x). (d) Masson staining (200x). (e and f). Electron microscopy. (g) Immunofluorescence staining for IgG (200x). (h) Immunofluorescence staining for C3 (200x). (i) Immunofluorescence staining for IgA (200x).
Representative images of the renal biopsy histopathology of patients with IgA− at pathological stage II-III. (a) H&E staining (200x). (b) PAS staining (200x). (c) PASM staining (200x). (d) Masson staining (400x). (e and f). Electron microscopy. (g) Immunofluorescence staining for IgG (200x). (h) Immunofluorescence staining for C3 (200x).
Patients with IgA+ showed significantly higher cumulative incidence rates of PR or CR than patients with IgA−
The follow-up duration ranged from 6 to 111 months. The IgA− group had a significantly longer follow-up duration than the IgA+ group (18.57 ± 16.32 months vs. 12.79 ± 12.03 months, P = 0.001, Table 3). At the latest follow-up examination, BUN, SCr, serum UA and albumin levels, proteinuria severity, and hematuria severity were similar in the two groups (Table 3).
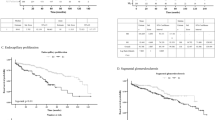
To compare the prognostic disease characteristics of the two patient groups, we performed Kaplan-Meier (K-M) analyses to investigate the cumulative poor event-free renal survival and cumulative incidence rates of PR or CR. Patients with longer than 6 months of follow-up duration, including 55 cases of IgA+ and 287 cases of IgA−, were included for the K-M analyses. A poor event was defined as an occurrence of a 50% reduction in eGFR, ESRD, or all-cause mortality. The one-year and 4-year cumulative poor event-free renal survival rates were 100.0% and 47.4%, respectively, in patients with IgA+, and they were 96.9% and 78%, respectively, in patients with IgA− (Fig. 4a). Although the 4-year survival rates were lower in the IgA+ group (47.4%) than in the IgA− group (78%), the differences were not statistically significant (odds ratio: 1.355; 95% CI: 0.3804–4.8234; P = 0.6744). Notably, the K-M analysis also revealed that the one, two, and three-year cumulative incidence rates of PR or CR were 25.6%, 67.7%, and 87.2%, respectively, in patients with IgA+, whereas the rates were 17.3%, 47.0%, and 66.4%, respectively in patients with IgA− (Fig. 4b). The patients with IgA+ had significantly higher cumulative incidence rates of PR or CR than patients with IgA− (odds ratio: 1.653; 95% CI: 1.0331–2.6441; P = 0.0085).
Kaplan-Meier analysis. (a) Cumulative poor event-free renal survival rate in all patients (including with treatment and without treatment) between the IgA+ and IgA− groups. (b) Cumulative incidence rates of PR or CR in all patients (including patients with and without treatment) between the IgA+ and IgA− groups.
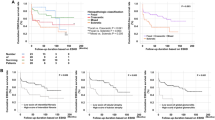
We next considered treatments; we performed K-M analysis to compare the prognosis with and without treatment. The with treatment group had a higher poor event-free renal survival rate than the without treatment group (P = 0.0002) (Fig. 5a). The different treatment groups had different poor prognoses (P = 0.0051), but good prognoses among the different treatment groups were negative (Fig. 5b).
Kaplan-Meier analysis. (a) Cumulative poor event-free renal survival rate and cumulative incidence rates of PR or CR in all patients with and without treatment. (b) Cumulative poor event-free renal survival rate and cumulative incidence rates of PR or CR in all patients receiving different treatments.
Next, we doubted that different treatments could influence IgA+ and IgA− groups. We classified similar cohorts into four groups as a whole, including (1) without treatment: general treatment without RAS inhibitors or glucocorticoids or immunosuppressors; (2) RAS receptor inhibitors; (3) glucocorticoids plus cyclophosphamide (GC + CTX); and (4) CNI therapy (tacrolimus or cyclosporine). There were no treatment differences between the IgA+ and IgA− groups (P = 0.517) as a whole: 3 (5.5%) versus 13 (4.5%) between the IgA+ and IgA− groups (P = 0.758) without treatment; 22 (40.0%) versus 96 (33.1%) between the IgA+ and IgA− groups with RAS receptor inhibitor treatment (P = 0.323); 13 (23.6%) versus 58 (20.0%) between the IgA+ and IgA− groups (P = 0.541) receiving treatment with GC + CTXt; and 14 (25.5%) versus 101 (34.8%) between the IgA+ and IgA− groups (P = 0.176) under CNI treatment (Table 4). Therefore, there was no statistical difference between treatments, including whole and partial; therefore, we can evaluate IgA’s deposition independent of the different treatments.
Association of baseline clinical parameters and disease prognosis
Of the 506 patients, 342 had a follow-up duration >6 months. We then focused on these 342 patients and carried out multivariate Cox regression analyses to identify factors that could be significantly associated with a poor prognosis or the incidence of PR or CR. Poor prognosis was defined as an occurrence of a 50% reduction in eGFR, ESRD, or all-cause mortality. Multivariate Cox analyses revealed that old age at biopsy, high baseline SCr and serum UA were significantly associated with a poor prognosis (Table 5). The multivariate Cox analysis also found that increased interstitial fibrosis and IgA expression, and reduced hypertension, BUN, and proteinuria were significantly associated with an incidence of PR or CR (Table 6). Additionally, the univariate Cox analysis revealed that the different treatments were not associated with either a good or a poor prognosis (Tables S1 and S2).
Discussion
Overlapping MN and IgAN is considered to be a rare medical condition. The majority of previous studies on this rare condition were reports of a single case or a case series and focused on a description of the renal pathology12,13,14,15, 19. Notably, the current study included the largest patient cohort of overlapping IMN and IgAN (73 cases) and IMN alone (425 cases), which compared the prognostic, clinical, and histopathological characteristics of the two patient groups. Similar to the findings in the current study, the previous reports have also shown that IgG deposits are mainly in the capillary walls, while IgA deposits are predominantly in the mesangial area in the renal pathology of patients with overlapping MN and IgAN12,13,14,15, 19.
In the current study, we found similar baseline clinical features in the overlapping IMN and IgAN groups and the IMN only group. Although the current study showed a statistically significantly higher pathological stage in the IgA+ group than in the IgA− group, the increment was only approximately 14% (1.88 vs. 1.65) and therefore may represent a minimal clinical significance.
To the best of our knowledge, the current study is the first comprehensive comparison of the renal pathological features of overlapping IMN and IgAN versus IMN only and to define the unique renal histopathology associated with overlapping IMN and IgAN. Compared with the IMN only group, the renal histopathology of the overlapping IMN and IgAN groups not only exhibited significantly increased mesangial cell proliferation and matrix expansion, which are characteristic of the renal histopathology of IgAN but also showed increased inflammatory cell infiltration and higher proportions of arteriole hyalinosis and lesions. However, the proportion of segmental sclerosis was significantly lower in the overlapping IMN and IgAN group compared with the IMN alone group.
The lower chance of segmental sclerosis in the patients with overlapping IMN and IgAN may explain the high incidence of PR or CR in these patients. In the current study, we performed K-M analysis to discover that the one, two, and three-year cumulative incidence rates of PR or CR were significantly higher in the patients with overlapping IMN and IgAN than in the patients with IMN only. Consistently, the multivariate Cox model analysis also revealed that increased IgA expression was significantly associated with the incidence of PR or CR. PR and CR have been recommended as surrogate endpoints to evaluate the outcomes of patients with IMN20. Although the cumulative poor event-free renal survival rate was lower in the patients with overlapping IMN and IgAN than in the patients with IMN alone, the difference was not statistically significant. A previous case series study showed a similar renal prognosis in overlapping MN and IgAN versus MN only12. Stokes et al. also indicated that the combination of MN and IgAN may not lead to a poorer clinical outcome compared with MN alone12. Similarly, Nishida et al. reported a pediatric case of coexisting MN and IgAN and suggested that overlapping MN and IgAN might not lead to deleterious outcomes21. The physiological and cellular mechanisms underlying the overlapping IMN and IgAN-associated increase in disease remission remains unclear.
To avoid the effects of different treatments between overlapping IMN and IgAN and IMN only, we took treatment into account. We found that there was a better prognosis with drug treatment than without treatment, and the prognosis rank differed between different drug treatments.
However, despite the different drug treatments, poor prognosis displayed no significant statistical difference between overlapping IMN and IgAN and IMN only. We speculate that the reason there is no difference is because the different treatments in our research were chosen according to the clinical symptoms, such as persistent nephrotic syndrome, rather than pathological features such as the presence or absence of IgA deposition, which is also recommended by the KDIGO clinical practice guidelines for glomerulonephritis of IMN16. The proportions of patients with comorbidities, such as edema, hypertension, diabetes, infection, embolism, nephrotic syndrome, and/or microscopic hematuria, were similar between the IgA+ and IgA− groups. In other words, the clinical symptoms were comparable between the IgA+ and IgA− groups, and therefore the treatments were also comparable between the IgA+ and IgA− groups. Therefore, we can evaluate IgA’s deposition independent of the different treatments.
The etiology of overlapping IMN and IgAN is unlikely to be due to chance alone. IMN and IgAN could develop simultaneously, or either IgAN or IMN could be the primary event and subsequently stimulate the other nephropathy19. Miyazaki et al. reported a case of the development of IgAN 14 years after the diagnosis of MN22. Genetic factors may contribute to the development of overlapping IgAN and MN. Familial overlapping of IgAN and MN has been reported previously19, 23, 24.
The current study also found that increased age at biopsy and high baseline SCr and serum UA levels significantly increased the risk of a 50% reduction in eGFR, ESRD, or all-cause mortality. Similarly, recent studies have also demonstrated that persistent nephrotic range proteinuria and elevated creatinine levels are associated with poor outcomes in patients with IMN25, 26. The correlation between high interstitial fibrosis and the incidence of PR or CR may be explained by the interstitial fibrosis-mediated nonspecific reduction in urine secretion. We speculate that increased interstitial fibrosis may result in the blockage of capillary loops and the reduction in urinary protein excretion, therefore leading to a false sense of a better prognosis.
The main limitation of the current study is that the follow-up duration of patients varied greatly, which results in big variations in the renal survival analysis. We are currently continuing to follow up with the patients and will further investigate the prognostic features of overlapping IMN and IgAN. The M-type phospholipase A2 receptor (PLA2R) has mostly been studied in IMN since 2009. However, because our patient selection occurred between September 11, 2006 and November 25, 2015 in this research and the commercial detection of PLA2R in the clinic was not mature during this time in our district, PLA2R was not a consideration in our study.
Conclusions
This retrospective observational study found that, in addition to presenting the IgAN-characteristic renal histopathology, such as significantly increased mesangial cell proliferation and matrix expansion, patients with overlapping IMN and IgAN also exhibited unique features, such as increased inflammatory cell infiltration, higher proportions of arteriole hyalinosis and lesions, but lower proportions of segmental sclerosis compared with patients with IMN only. In addition, overlapping IMN and IgAN appears to correlate with an increased incidence of disease remission and thus may not lead to a poorer prognosis compared with IMN only.
References
Seitz-Polski, B. et al. Epitope Spreading of Autoantibody Response to PLA2R Associates with Poor Prognosis in Membranous Nephropathy. Journal of the American Society of Nephrology: JASN. 27, 1517–1533 (2016).
Lee, T. et al. Patients with primary membranous nephropathy are at high risk of cardiovascular events. Kidney international. 89, 1111–1118 (2016).
Radice, A. et al. Clinical usefulness of autoantibodies to M-type phospholipase A2 receptor (PLA2R) for monitoring disease activity in idiopathic membranous nephropathy (IMN). Autoimmunity reviews. 15, 146–154 (2016).
Ronco, P. & Debiec, H. Pathophysiological advances in membranous nephropathy: time for a shift in patient’s care. Lancet (London, England). 385, 1983–1992 (2015).
Bally, S. et al. Phospholipase A2 Receptor-Related Membranous Nephropathy and Mannan-Binding Lectin Deficiency. Journal of the American Society of Nephrology: JASN. 27, 3539–3544 (2016).
Hoxha, E. et al. Spontaneous remission of proteinuria is a frequent event in phospholipase A2 receptor antibody-negative patients with membranous nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 30, 1862–1869 (2015).
Fervenza, F. C., Sethi, S. & Specks, U. Idiopathic membranous nephropathy: diagnosis and treatment. Clinical journal of the American Society of Nephrology: CJASN. 3, 905–919 (2008).
Roccatello, D. et al. New insights into immune mechanisms underlying response to Rituximab in patients with membranous nephropathy: A prospective study and a review of the literature. Autoimmunity reviews. 15, 529–538 (2016).
Morita, M. et al. Glomerular endothelial cell injury and focal segmental glomerulosclerosis lesion in idiopathic membranous nephropathy. PloS one. 10, e0116700 (2015).
Roberts, I. S. et al. The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney international. 76, 546–556 (2009).
Cattran, D. C. et al. The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney international. 76, 534–545 (2009).
Stokes, M. B. & Alpers, C. E. Combined membranous nephropathy and IgA nephropathy. American journal of kidney diseases: the official journal of the National Kidney Foundation. 32, 649–656 (1998).
Koselj-Kajtna, M. et al. Recurrent immunoglobulin A nephropathy complicated with de novo membranous glomerulonephritis in renal allografts. Transplantation proceedings. 34, 3117–3118 (2002).
Kfoury, H. K., Alghonaim, M., AlSuwaida, A. K., Zaidi, S. N. & Arafah, M. Nasopharyngeal T-cell monomorphic posttransplant lymphoproliferative disorders and combined IgA nephropathy and membranous glomerulonephritis in a patient with renal transplantation: a case report with literature review. Transplantation proceedings. 42, 4653–4657 (2010).
Hu, R., Xing, G., Wu, H. & Zhang, Z. Clinicopathological features of idiopathic membranous nephropathy combined with IgA nephropathy: a retrospective analysis of 9 cases. 11, 86 (2016).
KDIGO clinical practice guideline for glomerulonephritis. Abstract. Kidney Int Suppl (2011). 2, 142 (2012).
Levey, A. S. et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Annals of internal medicine. 130, 461–470 (1999).
Qin, H. Z. et al. Combined Assessment of Phospholipase A2 Receptor Autoantibodies and Glomerular Deposits in Membranous Nephropathy. Journal of the American Society of Nephrology: JASN. 27, 3195–3203 (2016).
Jennette, J. C., Newman, W. J. & Diaz-Buxo, J. A. Overlapping IgA and membranous nephropathy. American journal of clinical pathology. 88, 74–78 (1987).
Thompson, A., Cattran, D. C., Blank, M. & Nachman, P. H. Complete and Partial Remission as Surrogate End Points in Membranous Nephropathy. Journal of the American Society of Nephrology: JASN. 26, 2930–2937 (2015).
Nishida, M., Kato, R. & Hamaoka, K. Coexisting Membranous Nephropathy and IgA Nephropathy. Fetal and pediatric pathology. 34, 351–354 (2015).
Miyazaki, K. et al. Development of IgA nephropathy 14 years after diagnosis of membranous nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 17, 140–143 (2002).
Ohzono, Y. et al. A case of familial IgA nephropathy. Nihon Jinzo Gakkai shi. 27, 533–540 (1985).
Guella, A., Akhtar, M. & Ronco, P. Idiopathic membranous nephropathy in identical twins. American journal of kidney diseases: the official journal of the National Kidney Foundation. 29, 115–118 (1997).
Kanigicherla, D. A. et al. Long-term outcomes of persistent disease and relapse in primary membranous nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association - European Renal Association. 31, 2108–2114 (2016).
Barbour, S. J., Cattran, D. C., Espino-Hernandez, G., Hladunewich, M. A. & Reich, H. N. Identifying the ideal metric of proteinuria as a predictor of renal outcome in idiopathic glomerulonephritis. Kidney international. 88, 1392–1401 (2015).
Acknowledgements
This study was supported by the Zhejiang Province Natural Science Foundation (Grant No: LY16H150007, Xinxin Chen), the Zhejiang Province Medicine and Health Science and Technology Program (Grant No: 2016KYB188, Xinxin Chen), the Wenzhou Science and Technology Program (Grant No: Y20160311, Xinxin Chen) and the Key Construction Academic Subject (Medical Innovation) of Zhejiang Province (11-CX26).
Author information
Authors and Affiliations
Contributions
Xinxin Chen was the main researcher; she planned the study, wrote the protocol, participated in the data analysis, and contributed to writing this manuscript. Yu Chen, Huan Tong and Guangju Zhao helped with data collection. Chaosheng Chen helped with clinical analysis. Keqing Shi helped with statistical analysis. Yinqiu Lv, Bo Chen and Duo Li helped with pathologic analysis. Zhongqiu Lu critically reviewed and revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, X., Chen, Y., Shi, K. et al. Comparison of prognostic, clinical, and renal histopathological characteristics of overlapping idiopathic membranous nephropathy and IgA nephropathy versus idiopathic membranous nephropathy. Sci Rep 7, 11468 (2017). https://doi.org/10.1038/s41598-017-11838-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-11838-1
This article is cited by
-
Diagnostic value of renal biopsy in anti-phospholipase A2 receptor antibody-positive patients with proteinuria in China
Scientific Reports (2024)
-
Serum complement factor B is associated with disease activity and progression of idiopathic membranous nephropathy concomitant with IgA nephropathy
International Urology and Nephrology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.