Abstract
Highly pathogenic avian influenza virus (HPAIV) is a serious threat not only to domestic fowls but also to humans. Vaccines inducing long-lasting immunity against HPAIV are required. In the present study, we generated recombinant measles virus (MV) expressing the hemagglutinin protein of HPAIV without the multibasic site necessary for its pathogenicity in chickens using the backbone of an MV vaccine strain (rMV-Ed-H5HA) or a wild-type MV-derived mutant (rMV-HL-Vko-H5HA). We examined protective efficacy of the candidate vaccines in the monkey infection model by the challenge with a HPAIV (H5N1). Cynomolgus monkeys inoculated with the candidate vaccines produced both anti-H5 HA and anti-MV antibodies. They recovered earlier from influenza symptoms than unvaccinated monkeys after the challenge with the HPAIV strain. Chest radiography and histopathological analyses confirmed less severe pneumonia in the vaccinated monkeys. Vaccination tended to suppress viral shedding and reduced the interleukin-6 levels in the lungs. Furthermore, the vaccination with rMV-Ed-H5HA of monkeys with pre-existing anti-MV immunity induced the production of anti-H5 HA antibodies. These results suggest that both candidate vaccines effectively reduce disease severity in naïve hosts, and that rMV-Ed-H5HA is a particularly good candidate vaccine against HPAIV infection.
Similar content being viewed by others
Introduction
Highly pathogenic avian influenza virus (HPAIV) has continued to threaten human health since H5N1 infection was first recognized in humans in 19971. Although not as prevalent as seasonal influenza, it is considered a serious pathogen because its mortality rate in humans is high2. Recent studies have also demonstrated that several mutations in HPAIV confer transmissibility among mammalian hosts3,4. Therefore, the development of an effective vaccine against HPAIV is urgently required.
Various types of vaccines for HPAIV are being developed in several countries, including inactivated vaccines, live attenuated vaccines, and DNA vaccines5. Inactivated vaccines do not induce long-lasting immunity, and require frequent administration. Therefore, attenuated live vaccines are preferable, based on the strength and duration of their immunostimulation. However, vaccines derived from attenuated HPAIV entail safety issues with the potential occurrence of revertant and reassortant viruses6.
Utilization of the measles virus (MV) vector has been proposed to develop live vaccines for infectious diseases7,8,9,10. Attenuated MV strains had been established for the vaccination of humans, and have excellent characteristics as vectors: (1) the safety of MV vaccines is well known from the history of vaccination; (2) MV vaccines induce cellular immunity and long lasting immunity; and (3) the reverse genetics of MV have been established, and allow foreign genes encoding the antigens of other pathogens to be inserted into the MV genome. We have previously developed several types of recombinant MV (rMV) expressing foreign antigen11,12. For example, we used this technique to develop a candidate vaccine against Nipah virus infection and showed that vaccination with the recombinant MV completely protected African green monkeys from a Nipah virus challenge. Therefore, we expect that bivalent vaccine based on MV vaccine vector is useful to develop new vaccines against various emerging infectious diseases.
In this study, we developed a candidate HPAIV vaccine based on the MV vector. We generated rMV expressing an HPAIV antigen and evaluated its efficacy on the challenge with a wild HPAIV (H5N1) strain in a previously established model of HPAIV infection in non-human primate13.
Results
Generation of recombinant MV expressing H5 hemagglutinin (HA)
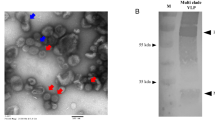
To generate rMV expressing H5 HA, we used a MV vaccine strain (Edmonston) and an attenuated HL strain as the backbone. The attenuated rMV-HL strain was previously generated by genetical modification to induce the deficient expression of the V protein14. The H5 HA gene (A/Anhui/1/2005, clade 2.3.4) was synthesized and inserted between the N and P genes of the full-genome cDNA of MV (Fig. 1a). To reduce the possibility that HA will function in cells infected with rMV, which could change the virus’ tropism, the multi basic site of HA necessary for its cleavage was removed. HEK 293 cells were transfected with the resultant plasmid and supporting plasmids and then overlain with B95a cells, and the recombinant viruses (rMV-Ed-H5HA or rMV-HL-Vko-H5HA) were rescued. Each recombinant virus grew in the appropriate permissive cell line (Vero cells for rMV-Ed-H5HA and B95a for rMV-HA-Vko-H5HA), although growth was slower and the maximum titer was lower than those of the corresponding parental viruses (Fig. 1b). An immunofluorescence assay and western blotting analysis demonstrated that H5 HA protein was expressed in the recombinant-virus-infected cells (Fig. 1c,d). Moreover, the expressed HA was not cleaved, unlike that in H5N1-infected cells (Fig. 1d), which is consistent with the design of the candidate vaccines. Therefore, infection with either recombinant virus (rMV-Ed-H5HA or rMV-HL-Vko-H5HA) caused the expression of H5 HA protein in vitro. In this paper, rMV-Ed-H5HA and rMV-HL-Vko-H5HA are collectively called ‘rMV-H5HA’.
Generation of rMV-H5HA. (a) Structure of the full-genome cDNA of rMV-H5HA. (b) Comparison of growth curves for rMV-H5HA and the parental rMVs in the corresponding cell lines. Data are averages ± SEM (n = 3). Closed or open dots indicate rMV-H5HA or the parental virus, respectively. Expression of H5 HA protein in cells infected with rMV-H5HA was examined with immunofluorescent microscopy (c) and western blotting (d) Full-length blots of each protein are shown in Supplemental Figure S1) (c) H5 HA was detected with anti-H5 HA antibody (rabbit) and anti-rabbit IgG antibody conjugated with Alexa Fluor 568, and MV N was detected with an anti-CDV N monoclonal antibody (mouse) and anti-mouse IgG antibody conjugated with Alexa Fluor 488, respectively.
Vaccination of cynomolgus monkeys with rMV-H5HA
To examine whether inoculation with rMV-H5HA induces immunity against H5N1 and MV, we inoculated cynomolgus monkeys with rMV-Ed-H5HA or rMV-HL-Vko-H5HA, because these nonhuman primates are susceptive to both MV and H5N1. We measured the antibody titers against MV and H5 with enzyme-linked immunosorbent assays (ELISA) (Table 1). The anti-MV antibody titers increased at 2 weeks post vaccination (wpv) in all three monkeys vaccinated with rMV-Ed-H5HA (#52, #53, and #54). After vaccination with rMV-HL-Vko-H5HA, the anti-MV antibody titers increased at 2 wpv in two of the three monkeys vaccinated (#57 and #58), and at 5 wpv in the third monkey (#56) after boosting. Anti-H5 HA antibodies were induced by rMV-Ed-H5HA in two of the three monkeys (#52 and #53) at 2 wpv, and in the third monkey (#54) at 5 wpv after boosting. Vaccination with rMV-HL-Vko-H5HA also increased the antibody titer against H5 HA (#57 and #58), whereas one monkey needed to be boosted twice (#56). Finally, all the vaccinated monkeys displayed similar antibody titers against MV and H5 HA. Therefore, inoculation with either candidate vaccines induced the production of antibodies against both MV and H5 HA. All the vaccinated monkeys appeared healthy and showed no leukopenia (data not shown), suggesting that H5 HA expression did not affect the safety of rMV.
Efficacy of rMV-HA in protecting monkeys from the challenge with a HPAIV (H5N1) strain
To examine the protective effects of rMV-Ed-H5HA or rMV-HL-Vko-H5HA against H5N1 infection, we challenged the vaccinated monkeys with H5N1 (A/whooper swan/Hokkaido/1/2008 clade 2.3.2.1) as previously described13. We monitored their body temperature, respiratory rate, heart rate, bodyweight, and appetite. All of the challenged monkeys had fever on the night after the day of challenge (Fig. 2a). Their high temperature persisted during the night, and a second bout of fever occurred in the unvaccinated monkeys (#45, #50, and #51). In contrast, the vaccinated monkeys recovered earlier, their body temperatures showed a circadian rhythm and no second bout of fever occurred (#52, #53, #54, #56, #57, and #58), indicating that fever, especially biphasic fever, was suppressed in the vaccinated monkeys. Tachycardia also persisted longer in the control monkeys than in the vaccinated monkeys (Supplemental Table 1). The unvaccinated monkeys also tended to show a loss of bodyweight, whereas the vaccinated monkeys maintained their bodyweight (Fig. 2b). All the unvaccinated monkeys showed tachypnea, which was more than twice as many as that before the challenge, whereas the vaccinated monkeys, except #58 for rMV-HL-Vko-H5HA, did not (Fig. 2c). When each symptom was scored (Supplemental Table 1), the clinical scores were lower in the vaccinated monkeys than in the unvaccinated monkeys (Fig. 2d). The difference between the control group and the vaccinated groups was significant (one-way repeated-measures ANOVA, p = 0.018), whereas the difference between the monkeys vaccinated with rMV-Ed-H5HA or rMV-HL-Vko-H5HA was not significant. Thus, the clinical symptoms were less severe in the vaccinated monkeys.
Clinical symptoms in monkeys after HPAIV challenge. (a) The vaccinated and unvaccinated monkeys were challenged with HPAIV (arrow). Fever onset was observed on the night of the day of challenge (black arrow heads). A second bout of fever was observed in the unvaccinated monkeys (gray arrow heads). Bodyweight (b) and respiratory rate (c) were monitored daily after the challenge. (d) Clinical symptoms were scored based on Supplemental Table 1. *p < 0.05, **p < 0.01, compared with the unvaccinated control on Dunnett’s test.
We also examined the progression of pneumonia with chest radiography. In the control monkeys, abnormal density was detected in both the right and left lungs, especially in #50, at 4 days post infection (dpi), and remained until 8 dpi (Fig. 3a). In contrast, among the monkeys vaccinated with rMV-Ed-H5HA, #52 showed slightly abnormal density only in the right lung at 4 dpi; #53 showed abnormal density in both the right and left lungs, but it had decreased at 8 dpi; and #54 showed obvious abnormal density in the right lung, but it had decreased at 8 dpi. In the monkeys vaccinated with rMV-HL-Vko-H5HA, the three monkeys (#56, #57, and #58) showed slightly abnormal density in the right lung, especially in the lower lobes of #57 and #58, at 4 dpi, and it was decreased at 8 dpi. Therefore, the pulmonary density was lower or declined more rapidly in the vaccinated monkeys than in the control monkeys, suggesting that the inflammation in the lungs was less severe in the vaccinated monkeys than in the unvaccinated monkeys.
Inflammation of the lungs of HPAIV-challenged monkeys. (a) Chest X-rays taken at 4 and 8 dpi are shown. (b) Hematoxylin and eosin staining of the lower lobe of the right lung of the monkeys. Original maginifcation, 4× objective lens. (c) Histopathology of each lung lobe was scored as: 0, area of pulmonary alveoli was >60% of the observed section; 1, area of pulmonary alveoli was 40–60% of the observed section; 2, area of pulmonary alveoli was 30–40% of the observed section; 3, area of pulmonary alveoli was 20–30% of the observed section; 4, area of pulmonary alveoli was <20% of the observed section. The total score for each individual monkey was used in the analysis. *p < 0.05 compared with the unvaccinated control on Dunnett’s test.
The monkeys were euthanized at 8 dpi and a histopathological analysis was performed. In the control monkeys, the lung showed severe inflammation (Fig. 3b). There were smaller regions of severe inflammation in the monkeys vaccinated with either candidate vaccine than in the control monkeys (Fig. 3b). To evaluate the severity of inflammation, histopathological scores based on the areas of pulmonary alveoli were compared. Interstitial inflammation was less severe in the vaccinated monkeys than in the unvaccinated monkeys (Fig. 3c). We also compared interleukin-6 (IL-6) levels in the lungs of the control and vaccinated monkeys, because IL-6 levels are known to correlate with influenza severity15,16. The levels of IL-6 were lower in the vaccinated group than in the unvaccinated group (Fig. 4).
To further evaluate the effect of vaccination on the progress of HPAIV infection, viral shedding was examined. A reverse transcription (RT)-PCR analysis was used to detect viral RNA in nasal swabs. Viral RNA was detected after several days in the control monkeys, but none was detected or was detected only in one day in the vaccinated monkeys (Table 2), suggesting that vaccination with rMV-H5HA suppressed viral shedding after H5N1 challenge.
It is known that MV induces strong cellular immunity. To examine whether the vaccination with rMV-H5HA promotes induction of cellular immunity after H5N1 challenge, we examined interferon-gamma (IFN-γ) levels as an indicator of cellular immune response (Fig. 5). In control monkeys, IFN-γ increased in a biphasic pattern, in a lower level at around 1 dpi and then in a higher level at around 6 dpi. In the monkeys vaccinated with either rMV-Ed-H5HA or rMV-HL-Vko-H5HA, the maximum peak position shifted to 1–2 dpi. This suggests that the vaccination of rMV-H5HA promoted cellular immunity.
Together, these results suggest that vaccination with rMV-Ed-H5HA or rMV-HL-Vko-H5HA reduced the symptoms of influenza after H5N1 infection.
Influence of pre-existing immunity against MV on vaccination with rMV-H5HA
People are commonly vaccinated with an MV vaccine in childhood, particularly since the initiation of a global MV eradication campaign by the World Health Organization. To examine whether the presence of neutralizing antibodies inhibits the efficacy of the rMV-H5HA vaccines, we vaccinated two monkeys that had previously been vaccinated with an MV vaccine strain with rMV-Ed-H5HA (Table 3). The anti-MV antibody titers were similar in the two monkeys before vaccination with rMV-H5HA (Table 3; 0 wpv). The anti-MV antibody titers clearly increased after one dose rMV-Ed-H5HA (#46 and #47). No anti-H5 HA antibodies were detected in any monkeys after one dose, but the titer increased after the second dose. Therefore, repeated vaccination with rMV-Ed-H5HA induced the production of anti-H5 HA antibodies, even when the host animal displayed pre-existing immunity to MV.
Discussion
In this study, we generated recombinant MVs expressing the H5 HA of a HPAIV strain by inserting H5 HA gene between the N and P genes of a vaccine strain or a wild-type-derived attenuated strain of MV. Both candidate vaccines conferred protection against HPAIV challenge in non-human primates.
In our previous studies in which we generated rMV expressing a foreign antigen, the foreign gene was inserted between the N and P genes, the rMV was successfully rescued, and the foreign protein was expressed after infection11,12. In this study, rMV-H5HA was also successfully rescued, although the growth of rMV-Ed-H5HA and rMV-HL-Vko-H5HA was slower than that of the parental viruses. Vaccination with rMV-Ed-H5HA or rMV-HL-Vko-H5HA induced the production of anti-H5HA antibodies in cynomolgus monkeys, suggesting that infection with either rMV-H5HA induced an immune response against MV and H5 HA. Vaccination also effectively protected the host animals from severe influenza after H5N1 infection.
When we compared the two candidate vaccines, the protection efficacy based on clinical scores did not differ between rMV-Ed-H5HA and rMV-HL-Vko-H5HA. Therefore, both rMV-Ed-H5HA and rMV-HL-Vko-H5HA are candidate vaccines against HPAIV infection in naïve hosts. Pre-existing immunity against MV must be considered, because most people possess neutralizing antibodies against MV owing to either natural infection or vaccination. Therefore, we examined the effects of prevaccination with MV and demonstrated that rMV-Ed-H5HA induced antibody production against H5 HA even when the monkeys possess MV-neutralizing antibodies, although antibody production was delayed compared with that in MV-naïve monkeys. This suggests that rMV-Ed-H5HA is even effective in the presence of MV-neutralizing antibodies. Similarly, pre-existing immunity against parainfluenza virus 5 (PIV5) did not inhibit the antibody production induced by a bivalent PVI5-based vaccine17.
H5 HA used as a vaccine antigen in this study belongs to clade 2.3.4 and the challenge virus belongs to clade 2.3.2.1, thus rMV-H5HA showed heterologous protection. Antigenic variation of HA often affect vaccine efficacy. However, ELISA titers obtained by using recombinant H5 HA of the vaccine antigen and the challenge virus were comparable (200, 400, and 200 for #52, #53, and #54 at 8 wpv). In addition, Yasui et al. previously demonstrated that vaccination of a recombinant vaccinia virus expressing the same H5 HA protein as this study induced production of neutralizing antibodies in one of three monkeys tested against the same challenge virus strain (A/whooper swan/Hokkaido/1/2008), and challenge induced the neutralizing antibodies in all of the three monkeys18. Also in our case, production of antibodies against H5 HA was boosted by the challenge (Supplemental Table 2), further supporting that immunity induced by vaccination with rMV-H5HA reacts to the challenge virus strain belonging to the different clade.
As for cross-clade protection, Shi et al.19 reported that antibodies against H5 HA (clade 2.3.4) protect chickens from the challenge of H5N1 (clade 2.3.2.1). Before that report, whereas Zhou et al.20 reported that neutralizing antibodies against H5 HA of clade 2.3.4 do not neutralize H5 HA of clade 2.3.2.1. The discrepancy may be due to different strains of H5N1 they used. Therefore, possibility of cross-protection may differ dependently on combination of virus strains for antigen and challenge.
Cellular immunity is also believed to contribute to recovery from influenza, by involving cytotoxic T lymphocytes and natural killer cells21,22,23. In this study, increase of IFN-γ in a biphasic patter was observed in the control monkeys, similarly to another monkey infection model of H5N124, whereas the early induction of IFN-γ was observed in the vaccinated monkeys. This suggests that the vaccination with rMV-H5HA helped to prompt cellular immune response against H5N1 infection. We infer that the cellular immune response contributed to remove the H5N1-infected cells from the vaccinated monkeys, resulting in less-severe symptoms.
Existing influenza vaccines are generally inactivated vaccines, thus the effective dose does not confer long-lasting immunity. In contrast, there are many literatures describing that live MV induces long-lasting immunity25,26,27. In addition, it was reported that measles vaccination was successful in protecting people who had no detectable antibodies at exposure28, and thus loss of antibody does not necessarily indicate loss of immunity. Thus, it is considered that cellular immunity induced by live MV vaccine is more important than humoral immunity. It remains to be determined whether the immunity induced against the foreign antigen expressed by MV vector-based vaccine is also maintained for a long time.
So far, Newcastle disease virus and PIV5 have been used as paramyxovirus-based vectors for developing a vaccine against H5N1, but their safety and efficacy have not yet been demonstrated in a non-human primate model29,30,31. The MV vector has the advantage that its safety is well known from its long history of vaccination in humans. We have also shown that rMV-Ed-H5HA induced immunity against H5 HA in the host animals even when they were sero-positive for MV. We anticipate that the MV vector can be generally used to develop vaccines against newly emerging infectious diseases.
Methods
Ethics statement
All animal experiments were in accordance with the Regulations for Animal Care and Use of The University of Tokyo and were approved by the Animal Experiment Committee at the Institute of Medical Science at The University of Tokyo (approval number: PA10-54).
Animals and housing
Thirteen cynomolgus monkeys (Macaca fascicularis, 5–6 years old, weighing 2.6–3.8 kg, seronegative for MV and H5N1) were imported from the Philippines. Before importation, the sera of the monkeys were imported and their antibody titers against MV and H5N1 were tested with ELISA, as described below, to select individuals lacking the corresponding antibodies. The imported monkeys were maintained at the Amami Laboratory of Injurious Animals at the Institute of Medical Science, The University of Tokyo, as described previously13. Transplant of telemetry (TA10CTA-D70, Data Sciences International) was performed after vaccination, and the body temperatures and heart rates of the monkeys were monitored as described previously13. The monkeys were euthanized under anesthesia at the end of the experimental period.
Cells and viruses
HEK 293 cells and Vero cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM) containing 5% fetal calf serum (FCS). B95a cells were maintained in RPMI-1640 containing 5% FCS. Measles virus Edmonston strain (MV-Ed) was propagated in Vero cells in DMEM supplemented with 2% FCS. Viruses were titrated by assessing the 50% tissue culture infectious dose (TCID50) in 96-well plates. A/whooper swan/Hokkaido/1/2008 (H5N1 clade 2.3.2.1), originally isolated from a dead wild water bird in Japan was used as described previously13,32. All infectious work with H5N1 was performed in P3 laboratories at the Institute of Medical Science, The University of Tokyo.
Plasmid construction and recombinant virus rescue
To generate an rMV expressing the H5N1 HA protein, we used replication-competent MV-based vectors: pMV-Ed for the Edmonston B strain and pMV-HL-Vko for a previously generated attenuated strain derived from the HL strain11,14. An HA cDNA of HPAIV (A/Anhui/1/2005 [H5N1, clade 2.3.4]) whose multi-basic site was deleted, was artificially synthesized18. The cDNA was re-amplified with PCR using the following primers: 5′- TGA CGC GTA TGG AGA AAA ATA GTG CTT CTT C -3′ (MluI site in italics) and 5′- GCA GGC CGG CCA CCT AAA TGC AAA T -3′ (FseI site in italics). The intergenic region between the N and P junction was amplified from pMV-Ed or pMV-HL-Vko by using the following primers: 5′- AGG GCC GGC CTG CCG AGG ACC AGA ACA A -3′ (FseI site in italics) and 5′- ATA CGC GTC ATC TGC TCC AAT CGT GGG AG -3′ for pMV-Ed, and 5′- ATA CGC GTC ATT GGC TCC AGT CGT GGG AG -3′ for rMV-HL-Vko(MluI site in italics). The corresponding PCR products were cloned into pGEM-T Easy (Promega). The plasmid was amplified in Escherichia coli DH5α and isolated with the Wizard Plus SV Miniprep DNA purification system (Promega), according to the manufacturer’s protocol. After digestion with MluI and NcoI, the N-P intergenic region was inserted into the plasmid containing H5 HA. The fragment of H5 HA connected to the N-P intergenic region was cloned into the FseI site of pMV-Ed or pMV-HL-Vko, and the resulting clones were used to rescue the recombinant MV expressing the H5 HA protein (rMV-Ed-H5HA or rMV-HL-Vko-H5HA), as describe previously33.
Virus characterization
Growth curve of rMV-Ed-H5HA and rMV-HL-Vko-H5HA were generated by infecting Vero and B95a cells, respectively, with the virus at a multiplicity of infection (moi) of 0.01. The virus was allowed to absorb to the cells for 1 h, and the inocula were removed. After medium was added, the cells were incubated at 37 °C. The cells and the supernatants were harvested at 12, 24, 48, 72, and 96 h post infection, and stored at −80 °C. The cells was frozen and thawed three times. The viral titers were determined by calculating the TCID50 values with the standard method.
Immunofluorescence assay
Vero cells were infected with either rMV-Ed-H5HA or the parental rMV-Ed at an moi of 0.01, and B95a cells were similarly infected either rMV-HL-Vko-H5HA or the parental rMV-HL-Vko. The cells were incubated until cytopathic effect (CPE) appeared, were fixed with 4% paraformaldehyde for >20 min at room temperature, and then permeabilized in 0.5% Triton X-100 in phosphate-buffered saline (PBS). The cells were then stained with rabbit polyclonal anti-H5 HA peptide antiserum or mouse polyclonal anti-canine distemper virus N serum34 in 10% Block Ace (DS Pharma Biomedical)/PBS solution, and then with goat anti-mouse IgG antibody conjugated with Alexa Fluor 488 (Invitrogen) or anti-rabbit IgG antibody conjugated with Alexa Fluor 568 (Molecular Probes). An imaging analysis was performed with the Fluoview FV1000 system (Olympus).
Immunoblotting
Vero cells were infected with either rMV-Ed-H5HA or the parental rMV-Ed strain, B95a cells were infected with either rMV-HL-Vko-H5HA or the parental rMV-HL-Vko, and MDCK cells were infected with HPAIV (A/duck/Hokkaido/vac-3/2007 [H5N1])35, at an moi of 0.01. After CPE appeared, the cells were harvested, washed with PBS, and lysed in SDS sample buffer (4.6% SDS, 10% 2-mercaptoethanol, 20% glycerol, and 0.01% bromophenol blue in 125 mM Tris–HCl, pH 6.8). Proteins were separated by 10% SDS-polyacrylamide gel electrophoresis and transferred to a polyvinylidene difluoride membrane (Merck Millipore). After the membrane were blocked with TBS containing 5% skim milk and 0.05% Tween 20, they were incubated with a 1:1000 dilution of rabbit polyclonal anti-H5 HA peptide antibody, rabbit polyclonal anti-MV N antibody36, or mouse monoclonal anti-glycelaldehyde 3-phospate dehydrogenase (GAPDH) antibody in Can Get Signal® solution (TOYOBO). The membranes were washed three times with TBS containing 0.05% Tween 20 and then incubated with a 1:2000 dilution of anti-rabbit IgG antibody or a 1:1000 dilution of anti-mouse IgG antibody conjugated with horseradish peroxidase (HRP, Dako). The proteins that bound the antibodies were detected with ECL Plus Western Blotting Detection Reagent (GE Healthcare). The reaction was visualized with the LAS1000 system (Fujifilm).
Immunization and challenge
Three cynomolgus monkeys were subcutaneously vaccinated with rMV-Ed-H5HA or rMV-HL-Vko-H5HA (2 × 104 TCID50/monkey). At 4 and 6 weeks post vaccination (wpv), they were inoculated with the same dose as in the primary vaccination. Serum was collected every week after vaccination. At 13 wpv for rMV-Ed-H5HA or 20 wpv for rMV-HL-Vko-H5HA, the monkeys were challenged with a HPAIV (H5N1) strain as described previously13. Briefly, a total of 1 × 107 plaque forming units (PFU) (3.3 × 106 PFU/ml) was inoculated to the monkeys intratracheally (2 ml by droplet exposure), intranasally (0.25 ml per nostril by droplet exposure), and orally (0.5 ml by pipette inoculation).
Measurement of antibody titers
The titer of the antibodies directed the MV and H5 HA protein in the monkey sera were determined with ELISA. Anti-MV antibodies were measured as described previously11. To measure the anti-H5 HA antibodies, recombinant H5 HA protein was produced. The H5 HA gene was ligated to the E. coli protein expression vector pET21b (Novagen), from which the recombinant protein was expressed as a fusion protein with a histidine tag. Competent BL21 cells were transformed with the plasmid to express the protein at high levels. A 100 mL culture of the transformed cells was induced to express the H5 HA protein in the mid-log growth phase (OD600 = 0.4) by the addition of 1 mM IPTG. After incubation for 2 h, the bacteria were collected, lysed with lysis buffer (50 mM Tris-HCl, 500 mM NaCl,20 mM Imidazol pH7.9), and freezed at −80 °C. Thawed protein solution was added with lysozyme at 50 mg/ml, sonicated for 20 sec for 5 times, and then centrifuged at 10,000 × g for 20 min at 4 °C. The recombinant H5 HA was collected in the insoluble fraction. Thus it was dissolved with 6 M urea. The H5 HA protein containing the N-terminal histidine tag in the supernatant was affinity purified with a Ni-Sepharose 6 Fast Flow resin column (GE Healthcare), according to the manufacturer’s protocol. Ninty-six-well microtiter plates were coated overnight with a 0.4 µg/ml solution of the recombinant H5 HA protein diluted in coating buffer (0.1 M carbonate hydrogen carbonate buffer, pH9.6). The wells were blocked with 200 µl of 2% Block Ace in PBS at room temperature for 3 h, and washed with PBS containing 0.05% Tween 20 (PBS-T). The monkey sera (50 µl) were serially diluted two-fold (1:100 to 1:12800) and added to wells. After incubation for 1 h at 37 °C, the wells were washed and incubated for 1 h at 37 °C with 50 µl of HRP-conjugated goat anti-monkey-IgG antibody (1:1000 dilution; Cappel). After the wells were washed again, 100 µl of peroxidase substrate (KPL) was added to each well and the absorbance at 655 nm was measured 30 min later (Bio-Rad).
Pathological examination
The animals were observed daily for clinical signs. At 1–8 dpi, their bodyweights and respiratory rates were recorded and chest radiography was performed under anesthesia. Nasal swabs were also collected and suspended for RNA extraction, and RT-PCR was performed as described previously13. Blood was collected and hematology performed as described previously13. At 8 dpi, the animals were euthanized and their lungs were collected. Part of the lungs was fixed in 10% phosphate-buffered formalin. Paraffin-embedded sections were stained with hematoxylin and eosin. Three fields of view were observed in six lobes from each monkey, and the areas of pulmonary alveoli were calculated with Adobe Photoshop CS6 (Adobe Systems). The severity of inflammation was scored as follows: 0, area of pulmonary alveoli was >60% of the observed section; 1, area of pulmonary alveoli was 40–60% of the observed section; 2, area of pulmonary alveoli was 30–40% of the observed section; 3, area of pulmonary alveoli was 20–30% of the observed section; 4, area of pulmonary alveoli was <20% of the observed section. The score for each lobe of an individual monkey were summed and the total score was used in the analysis.
Measurement of IL-6 level in the lung
L-15 medium (2.5 volume) was added to frozen lung lobe tissues and a tissue homogenate was prepared. The homogenate was centrifuged at 3300 × g for 1 min and the supernatant was used for the assay. The IL-6 levels were measured with a BD Cytometric Bead Array Non Human Primate Th1/Th2 Cytokine Kit (BD Biosciences), according to the manufacturer’s protocol, and a FACSCalibur flow cytometry (BD Biosciences). The data were analyzed with the FCAP Array software (BD Biosciences). The average IL-6 level in the six lung lobes of an individual monkey was calculated, and the average values were used for further analysis.
Measurement of IFN-γ level
The sera or plasma collected from individual monkeys were heat inactivated, and then IFN-γ levels were measured with a commercial ELISA kit (Monkey IFN-γ ELISA kit, MABTECH), according to the manufacturer’s protocol.
Vaccination of monkeys with pre-existing immunity against MV
Two naïve monkeys were inoculated with MV Edmonston strain (2 × 104 TCID50/monkey). At 4 and 6 weeks postvaccination, they were inoculated with the same dose as the primary vaccination. Serum was collected several times after vaccination and ELISA were performed. After anti-MV antibodies were produced, the monkeys were vaccinated subcutaneously with rMV-Ed-H5HA subcutaneously.
Statistical analysis
All statistical analyses were performed with the JMP software (JMP Pro 10.0.2, SAS Institute Inc.).
References
Gambotto, A., Barratt-Boyes, S. M., de Jong, M. D., Neumann, G. & Kawaoka, Y. Human infection with highly pathogenic H5N1 influenza virus. Lancet 371, 1464–1475 (2008).
Adams, S. & Sandrock, C. Avian influenza: update. Medical Principles and Practice 19, 421–432 (2010).
Imai, M. et al. Transmission of influenza A/H5N1 viruses in mammals. Virus research 178, 15–20 (2013).
Linster, M. et al. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell 157, 329–339 (2014).
El Sahly, H. M. & Keitel, W. A. Pandemic H5N1 influenza vaccine development: an update. Expert review of vaccines 7, 241–247 (2008).
Luke, C. J. & Subbarao, K. Vaccines for pandemic influenza. Emerging infectious diseases 12, 66–72 (2006).
Brandler, S. & Tangy, F. Recombinant vector derived from live attenuated measles virus: potential for flavivirus vaccines. Comparative immunology, microbiology and infectious diseases 31, 271–291 (2008).
Naim, H. Y. Applications and challenges of multivalent recombinant vaccines. Human vaccines & immunotherapeutics 9, 457–461 (2013).
Naim, H. Y. Measles virus. Human vaccines & immunotherapeutics 11, 21–26 (2015).
Sato, H., Yoneda, M., Honda, T. & Kai, C. Morbillivirus receptors and tropism: multiple pathways for infection. Frontiers in microbiology 3, 75 (2012).
Satoh, M. et al. Evaluation of a recombinant measles virus expressing hepatitis C virus envelope proteins by infection of human PBL-NOD/Scid/Jak3null mouse. Comparative immunology, microbiology and infectious diseases 33, e81–88 (2010).
Yoneda, M. et al. Recombinant measles virus vaccine expressing the Nipah virus glycoprotein protects against lethal Nipah virus challenge. PLoS One 8, e58414 (2013).
Fujiyuki, T. et al. Experimental infection of macaques with a wild water bird-derived highly pathogenic avian influenza virus (H5N1). PLoS One 8, e83551 (2013).
Sato, H. et al. Measles virus induces cell-type specific changes in gene expression. Virology 375, 321–330 (2008).
Paquette, S. G. et al. Interleukin-6 is a potential biomarker for severe pandemic H1N1 influenza A infection. PLoS One 7, e38214 (2012).
Skoner, D. P., Gentile, D. A., Patel, A. & Doyle, W. J. Evidence for cytokine mediation of disease expression in adults experimentally infected with influenza A virus. The Journal of infectious diseases 180, 10–14 (1999).
Chen, Z. et al. Evaluating a parainfluenza virus 5-based vaccine in a host with pre-existing immunity against parainfluenza virus 5. PLoS One 7, e50144 (2012).
Yasui, F. et al. Sensitization with vaccinia virus encoding H5N1 hemagglutinin restores immune potential against H5N1 influenza virus. Scientific reports 6, 37915 (2016).
Shi, S. et al. Cross-clade protective immune responses of NS1-truncated live attenuated H5N1 avian influenza vaccines. Vaccine 34, 350–357 (2016).
Zhou, F. et al. A triclade DNA vaccine designed on the basis of a comprehensive serologic study elicits neutralizing antibody responses against all clades and subclades of highly pathogenic avian influenza H5N1 viruses. Journal of virology 86, 6970–6978 (2012).
Grant, E. J., Quinones-Parra, S. M., Clemens, E. B. & Kedzierska, K. Human influenza viruses and CD8(+) T cell responses. Curr Opin Virol 16, 132–142 (2016).
Weiss, I. D. et al. IFN-gamma treatment at early stages of influenza virus infection protects mice from death in a NK cell-dependent manner. J Interferon Cytokine Res 30, 439–449 (2010).
Yap, K. L. & Ada, G. L. The recovery of mice from influenza A virus infection: adoptive transfer of immunity with influenza virus-specific cytotoxic T lymphocytes recognizing a common virion antigen. Scand J Immunol 8, 413–420 (1978).
Shinya, K. et al. Integrated clinical, pathologic, virologic, and transcriptomic analysis of H5N1 influenza virus-induced viral pneumonia in the rhesus macaque. Journal of virology 86, 6055–6066 (2012).
Markowitz, L. E., Preblud, S. R., Fine, P. E. & Orenstein, W. A. Duration of live measles vaccine-induced immunity. Pediatr Infect Dis J 9, 101–110 (1990).
Amanna, I. J., Carlson, N. E. & Slifka, M. K. Duration of humoral immunity to common viral and vaccine antigens. N Engl J Med 357, 1903–1915 (2007).
Naniche, D. Human immunology of measles virus infection. Curr Top Microbiol Immunol 330, 151–171 (2009).
Samb, B. et al. Serologic status and measles attack rates among vaccinated and unvaccinated children in rural Senegal. Pediatr Infect Dis J 14, 203–209 (1995).
Cornelissen, L. A. et al. Protective efficacy of Newcastle disease virus expressing soluble trimeric hemagglutinin against highly pathogenic H5N1 influenza in chickens and mice. PLoS One 7, e44447 (2012).
Ge, J. et al. Newcastle disease virus-based live attenuated vaccine completely protects chickens and mice from lethal challenge of homologous and heterologous H5N1 avian influenza viruses. Journal of virology 81, 150–158 (2007).
Li, Z. et al. Recombinant parainfluenza virus 5 expressing hemagglutinin of influenza A virus H5N1 protected mice against lethal highly pathogenic avian influenza virus H5N1 challenge. Journal of virology 87, 354–362 (2013).
Okamatsu, M. et al. Antigenic, genetic, and pathogenic characterization of H5N1 highly pathogenic avian influenza viruses isolated from dead whooper swans (Cygnus cygnus) found in northern Japan in 2008. Virus Genes 41, 351–357 (2010).
Terao-Muto, Y. et al. Heparin-like glycosaminoglycans prevent the infection of measles virus in SLAM-negative cell lines. Antiviral research 80, 370–376 (2008).
Masuda, M. et al. Characterization of monoclonal antibodies directed against the canine distemper virus nucleocapsid protein. Comparative immunology, microbiology and infectious diseases 29, 157–165 (2006).
Soda, K. et al. Development of vaccine strains of H5 and H7 influenza viruses. The Japanese journal of veterinary research 55, 93–98 (2008).
Hagiwara, K. et al. Phosphorylation of measles virus nucleoprotein upregulates the transcriptional activity of minigenomic RNA. Proteomics 8, 1871–1879 (2008).
Acknowledgements
The authors thank Fumihito Ohashi (Osaka Prefecture University) and Fumiko Ono (The Corporation for Production and Research of Laboratory Primates) for their technical support. This work was supported by Grants-in-Aid from the Ministry of Education, Science, Sports, and Culture of Japan, KAKENHI to C.K. and T.F.
Author information
Authors and Affiliations
Contributions
T.F., M.Y., and C.K. designed the study. T.F., R.H., M.Y., T.K., F.Y., H.J.K., K.M., F.I., M.H., Y.K., M.O., H.S., S.H., M.K., and C.K. performed experiments. T.F., R.H., M.Y., and H.J.K. analyzed the data. T.F., R.H., K.H., and C.K. wrote the manuscript. C.K. supervised the study.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fujiyuki, T., Horie, R., Yoneda, M. et al. Efficacy of recombinant measles virus expressing highly pathogenic avian influenza virus (HPAIV) antigen against HPAIV infection in monkeys. Sci Rep 7, 12017 (2017). https://doi.org/10.1038/s41598-017-08326-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-08326-x
This article is cited by
-
Self-replicating vehicles based on negative strand RNA viruses
Cancer Gene Therapy (2023)
-
A protective measles virus-derived vaccine inducing long-lasting immune responses against influenza A virus H7N9
npj Vaccines (2023)
-
Versatility of live-attenuated measles viruses as platform technology for recombinant vaccines
npj Vaccines (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.